Introduction
The presentation of bladder cancer is rare (0.038%)
in the first two decades of an individual's life, particularly
until the age of 10 years (1,2). As
such, the literature on this topic is very limited, with only a
small number of cases having been previously described (3). Furthermore, to the best of our
knowledge, the majority of these previously reported cases have
been early-stage, low-grade carcinomas that were treated with
transurethral resection with a favorable outcome in patients <25
years-of-age (4,5). Transitional cell carcinomas in children
have been shown to have a less aggressive nature, as compared with
the same carcinomas in adults (4).
In adults, management of bladder carcinoma involves transurethral
resection for non-invasive lesions, and a cystectomy in cases of
muscle invasion. In addition, surgery is typically followed by
intravesical chemotherapy and/or immunotherapy in order to control
any microscopic residuals (6). Both
the American Urological Association and the International
Consultation on Bladder Cancer 2012 suggested that intravesical
mitomycin installation into the bladder should occur immediately
following the transurethral resection of papillary lesions.
Furthermore, for cases of high-grade disease, a cytoscopy and
re-resection of the resected areas should occur at 6 weeks
following the initial resection (7,8).
However, such recommendations do not seem justified for children,
who appear to have clinical features that differ from adult
patients and a better prognosis (4).
The present study reports a rare case of bladder cancer identified
in a 10-year-old female patient, which, apart from exhibiting
high-grade histological features, also presented sarcomatoid
differentiation with aggressive characteristics.
Case report
A 10-year-old female patient was referred to The
Second Xiangya Hospital of Central South University (Changsha,
China) presenting with painless hematuria and urinary frequency for
4 months. The patient had previously been diagnosed with urinary
tract infection at a local hospital, and antibiotics had been
prescribed. Physical examination revealed no abnormalities and a
blood test showed a normal white blood cell count. However, a
urinalysis detected white blood cells [1+/high power objective
(HP)], red blood cells (4+/HP) and bacteriuria (2+), which
suggested that the patient had severe hematuresis associated with
infection.
Chest X-ray and bone scan images were normal. An
abdominal computed tomography (CT) scan demonstrated a mass in the
posterior bladder wall with a rough edge; no lymphadenopathy was
found. Cystoscopy revealed a reddish, broccoli-like broad-based
tumor in the posterior bladder wall (Fig. 1). Biopsy indicated a high-grade
muscle-invasive urothelial carcinoma.
A traditional radical cystectomy was performed,
although, due to the age of the patient, the internal genitalia
were maintained in order to preserve the fertility of the patient.
Briefly, following a bilateral pelvic lymphadenectomy, the superior
vesical pedicles were ligated and divided on both sides. The blood
supply to both the ovaries and uterus was preserved, and a plane
was constructed between the uterus and bladder and later was
mobilized along with a small strip of anterior vaginal wall.
Subsequently, a cystectomy combined with a urethrectomy was
conducted, and an ileal conduit was made.
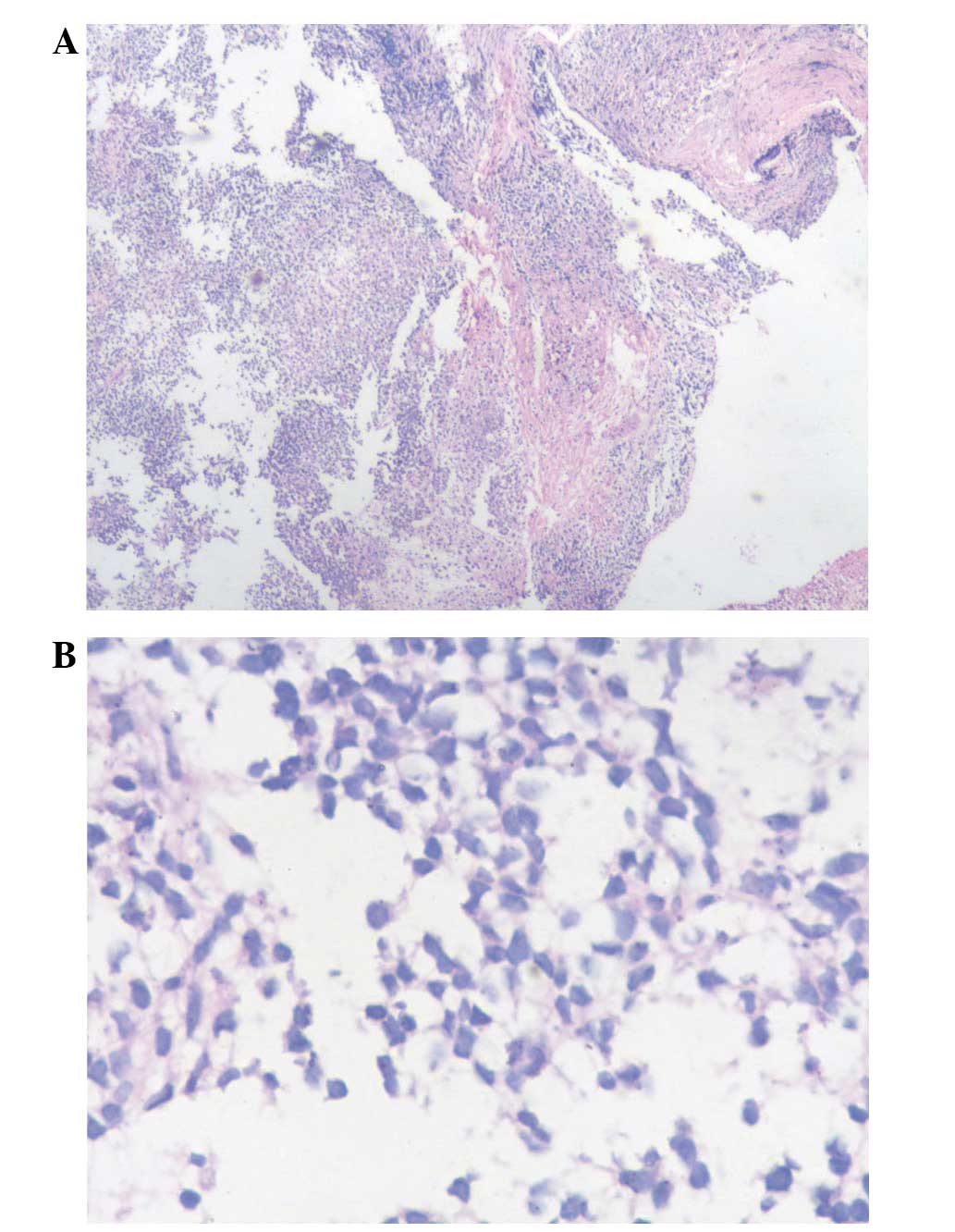
Upon gross examination, a 60×55 mm broad-based tumor
was found in the posterior bladder wall. Subsequently, the cancer
tissue was fixed in 10% formalin and dehydrated using an alcohol
gradient, after which it was made transparent using xylene and
embedded in paraffin (all: Sinopharm Chemical Reagent Co., Ltd.,
Shanghai, China). The paraffin-embedded tissue was then cut into
5–8 µm sections using the VIP 6-E2 Vacuum Infiltration Tissue
Processor (Sakura Finetek USA, Inc., Torrance, CA, USA), and
stained with hematoxylin and eosin (Beyotime Institute of
Biotechnology, Haimen, China). Subsequently, the tissue sections
were dehydrated using alcohol, made transparent with xylene and
mounted using Canada balsam (Qiyun Biotechnology Co., Ltd.,
Guangzhou, China), prior to visualization under an optical
microscope (Olympus BX41; Olympus Corporation, Tokyo, Japan). The
histopathological findings suggested that the tumor was a grade 3
muscle-invasive urothelial carcinoma with sarcomatoid
differentiation, according to the World Health Organization 1973
grading system (9). The TNM
classification of the tumor was T2bN0M0 (10). Both ureter edges were clear, and the
lymph nodes surrounding the iliac arteries and obtuator lymph nodes
were negative (Fig. 2). Adjuvant
chemotherapy, including methotrexate (Jiangsu Hengrui Medicine Co.,
Ltd., Lianyungang, China) vinblastine, adriamycin and cisplatin
(all Shenzhen Main Luck Pharmaceuticals Inc., Shenzen, China), was
administered 3 weeks after surgery; however, after receiving 4
cycles of chemotherapy, a CT scan of the abdomen identified disease
progression and the patient succumbed 2 months later. The patient
survived for only 6 months after surgery.
Discussion
The present case report describes a rare case of
aggressive bladder carcinoma in a pediatric patient. The most
important features of the case include the histopathological
findings of the tumor, which revealed divergent differentiation,
and fast disease progression following surgery. Despite the
immediate administration of chemotherapy following surgery, the
treatment was not beneficial for the patient.
The presentation of urothelial carcinoma of the
bladder is rare in pediatric patients, accounting for ~0.4% of
cases (11). To the best of our
knowledge, all reported bladder cancer cases in young people have
been of low grade and low malignancy potential, with favorable
outcomes (12,13), and the majority of them were treated
with transurethral resection of the bladder tumor without any kind
of adjuvant therapy (5). From a
histological point of view, mesenchymal components can sometimes be
found in high-grade bladder cancer, which usually indicates poor
prognosis (14). This was the case
in the present patient, for whom multiple mesenchymal components
were found in a high-grade urothelial carcinoma.
Gross hematuria is a common symptom of bladder
cancer in both pediatric and adult patients. In many cases, gross
hematuria leads to a misdiagnosis of urinary tract infection or
urinary stone disease (15,16), and thus, the underlying condition
remains unidentified. Risk factors for bladder cancer in pediatric
patients are not clear. A review in which multiple cases of bladder
cancer within families were analyzed suggested that there might be
a genetic predisposition for this disease; however, it remains
unclear whether multiple bladder cancer cases within families are a
result of genetic predisposition or due to shared environmental
exposure among family members (17).
There is no guideline available for the treatment
and follow-up of high-grade bladder cancer in pediatric patients.
The outcome of radical cystectomy is unpleasant, including a poor
quality of life, poor prognosis and reduced fertility in women
(18). However, radical cystectomy
combined with adjuvant therapy (chemotherapy and/or radiation
therapy) is currently the primary treatment option for invasive
high-grade bladder cancer (19).
Fertility-preserving radical cystectomy and chemotherapy have been
reported in young females (20) and
children (21). Lymph node
involvement has been reported to be the most important predictive
factor for cancer recurrence (22);
however, no evidence of lymph node involvement was identified in
the present case during surgery.
In conclusion, it is important to consider carefully
presentations of gross hematuria in pediatric patients. It is
recommended that the management of urothelial neoplasia in young
patients should largely depend on the tumor's grade and stage,
rather than on the age of the patient. The use of radical
cystectomy combined with adjuvant therapy in pediatric patients is
controversial due to a lack of guidelines for the management and
follow-up of these patients; however, it continues to be a viable
option for the treatment of high-grade muscle-invasive bladder
cancer in children.
References
|
1
|
Serrano-Durbá A, Domínguez-Hinarejos C,
Reig-Ruiz C, Fernández-Córdoba M and García-Ibarra F: Transitional
cell carcinoma of the bladder in children. Scand J Urol Nephrol.
33:73–76. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Thomas G, Gera P, Arbuckle S and Cohen R:
Transitional cell papilloma of the bladder in a child: A case
report and review of literature. J Pediatr Urol. 2:59–62. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bujons A, Caffaratti J, Garat JM and
Villavicencio H: Long-term follow-up of transitional cell carcinoma
of the bladder in childhood. J Pediatr Urol. 10:167–170. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yusim I, Lismer L, Greenberg G, Haomud K
and Kaneti J: Carcinoma of the bladder in patients under 25 years
of age. Scand J Urol Nephrol. 30:461–463. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hoenig DM, McRae S, Chen SC, Diamond DA,
Rabinowitz R and Caldamone AA: Transitional cell carcinoma of the
bladder in the pediatric patient. J Urol. 156:203–205. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Resnick MJ, Bassett JC and Clark PE:
Management of superficial and muscle-invasive urothelial cancers of
the bladder. Curr Opin Oncol. 25:281–288. 2013.PubMed/NCBI
|
|
7
|
Malmström PU, Sylvester RJ, Crawford DE,
Friedrich M, Krege S, Rintala E, Solsona E, Di Stasi SM and Witjes
JA: An individual patient data meta-analysis of the long-term
outcome of randomised studies comparing intravesical mitomycin C
versus bacillus Calmette-Guérin for non-muscle-invasive bladder
cancer. Eur Urol. 56:247–256. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fine SW, Humphrey PA, Dehner LP, Amin MB
and Epstein JI: Urothelial neoplasms in patients 20 years or
younger: A clinicopathological analysis using the world health
organisation 2004 bladder consensus classification. J Urol.
174:1976–1980. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
World Health Organization (WHO):
Histological typing of urinary bladder tumors. WHO (Geneva).
237–256. 1973.
|
|
10
|
International Union Against Cancer (UICC):
TNM classification of malignant tumors (7th). Genewa, Switzerland:
UICC. 262–265. 2009.
|
|
11
|
Poddevin F and Bayart M: Urothelial tumor
of the bladder in children. J Urol (Paris). 101:191–194. 1995.(In
French). PubMed/NCBI
|
|
12
|
Williamson SR, Lopez-Beltran A, MacLennan
GT, Montironi R and Cheng L: Unique clinicopathologic and molecular
characteristics of urinary bladder tumors in children and young
adults. Urol Oncol. 31:414–426. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fine SW, Humphrey PA, Dehner LP, Amin MB
and Epstein JI: Urothelial neoplasms in patients 20 years or
younger: A clinicopathological analysis using the World Health
Organization 2004 bladder consensus classification. J Urol.
174:1976–1980. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Patel R, Tery T and Ninan GK: Transitional
cell carcinoma of the bladder in first decade of life. Pediatr Surg
Int. 24:1265–1268. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ristiċ-Petroviċ A, Stojnev S,
Jankoviċ-Velickoviċ L and Marjanoviċ G: Malakoplakia mimics urinary
bladder cancer: A case report. Vojnosanit Pregl. 70:606–608. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gedikoğlu G, Sӧkmensüer C, Sӧylemezoğlu F
and Koçal C: Carcinosarcoma of the urinary bladder. Int Urol
Nephrol. 28:333–336. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mueller CM, Caporaso N and Greene MH:
Familial and genetic risk of transitional cell carcinoma of the
urinary tract. Urol Oncol. 26:451–464. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yossepowitch O and Dalbagni G:
Transitional cell carcinoma of the bladder in young adults:
Presentation, natural history and outcome. J Urol. 168:61–66. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
World Health Organization (WHO) Consensus
Conference on Bladder Cancer. Hautmann RE, Abol-Enein H, Hafez K,
Haro I, Mansson W, Mills RD, Montie JD, Sagalowsky AI, Stein JP,
Stenzl A, et al: Urinary diversion. Uro. 69(1 Suppl): 17–49. 2007.
View Article : Google Scholar
|
|
20
|
Gupta NP, Ansari MS, Khaitan A and Dawar
R: Fertility preserving radical cystectomy in a young female with
malignant mesenchymal tumour of urinary bladder. Int Urol Nephrol.
35:501–502. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Neogi S, Kariholu PL, Dhakre G, Gupta V,
Agarwal N and Bhadani P: Malignant urothelial carcinoma of urinary
bladder in a young child: A rare case report. Urology. 81:888–890.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Skinner DG, Daniels JR, Russell CA,
Lieskovsky G, Boyd SD, Nichols P, Kern W, Sakamoto J, Krailo M and
Groshen S: The role of adjuvant chemotherapy following cystectomy
for invasive bladder cancer: A prospective comparative trial. J
Urol. 145:459–467. 1991.PubMed/NCBI
|