Introduction
Tuberculosis (TB) remains a major cause of morbidity
and mortality in developing countries affecting millions of people
worldwide (1,2). Skeletal TB, constituting 10–20% of all
the extrapulmonary TB (ETB), is a well-recognized clinical
condition that is easily diagnosed and managed with an excellent
outcome (2). However, the occurrence
of multifocal skeletal involvement, which is defined as
osteoarticular lesions that occur simultaneously at two or more
locations in the skeletal system, is exceptional and constitutes
<5% of all skeletal TB cases, even in countries where TB is
endemic (3–6).
Radiological examinations, including conventional
roentgenography, magnetic resonance imaging (MRI) and computed
tomography (CT) scans, can be used to assist the diagnosis of
multifocal skeletal TB (4,5,7).
However, the diagnosis and treatment of multifocal skeletal TB are
frequently delayed due to the rarity and vague symptoms of the
disease, thus allowing progression to severe deformities and
functional deficits (3,5,6).
In the present study, a case of atypical
disseminated multifocal skeletal TB is presented. Unusual
radiological images were observed, which were more compatible with
a hematological malignancy or metastatic disease rather than an
infectious disease. Despite widespread osteoarticular involvement,
the outcome of the patient was favorable following anti-TB
treatment.
Case report
A 19-year-old male patient was admitted to Subei
People's Hospital of Jiangsu (Yangzhou, China) on 5th September
2011 with a 2 month history of recurrent fever and intermittent
thoracic back pain. The recurrent fever did not occur at specific
times and the temperature did not exceed 38.0°C. The patient also
reported limited mobility, decreased appetite and weight loss, but
did not experience chills or night sweats. There was no history of
exposure to TB or of a chronic cough. The patient presented a
normal general physical condition, with a body temperature of
37.3°C. A physical examination revealed slight tenderness over the
mid-thoracic spine, lumbar spine and left sacroiliac joint. No
paraspinal swelling or spasms were observed, while the sensation,
muscle strength and muscle tone of the lower extremities were
normal. Laboratory examinations showed a normal white blood cell
count [6.6×109/l; normal range (NR),
3.5–9.5×109/l] and normal levels of hemoglobin (120 g/l;
NR, 110–160 g/l), human leukocyte antigen-B27 (78; NR, 0–145) and
rheumatoid factor (5.0 IU/ml; NR, 0–14 IU/ml). In addition, tests
for autoantibodies, immunoglobulin, TB antibodies and
tumor-associated antigens were negative. The erythrocyte
sedimentation rate (ESR) was 75 mm/h, which was higher than the
normal range (0–15 mm/h), and the C-reactive protein level was
normal (10 mg/l; NR, 0–10 mg/l). Human immunodeficiency virus (HIV)
and purified protein derivative (PPD) tests were negative.
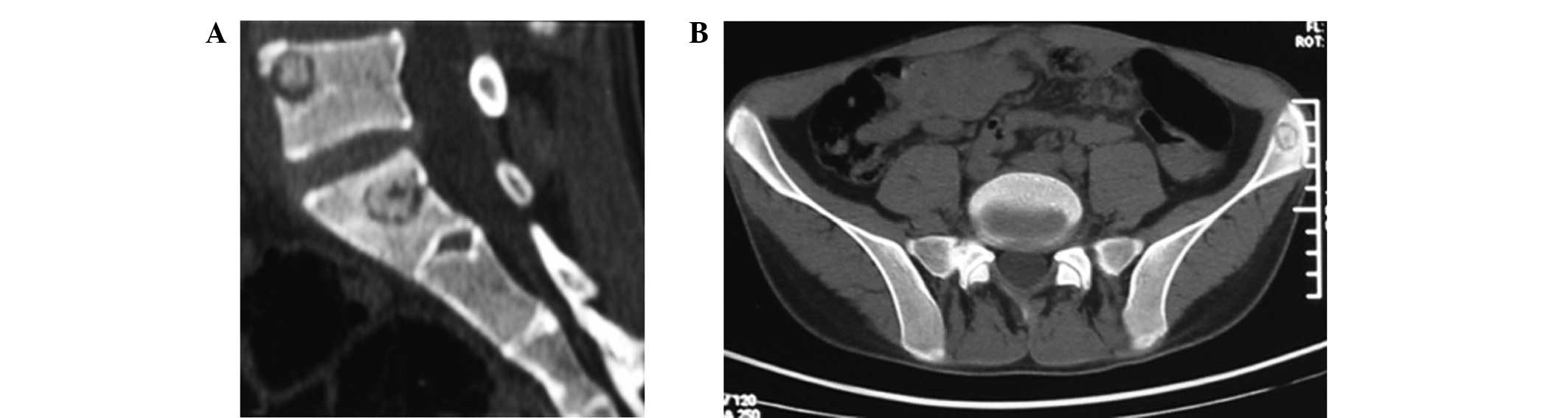
Further imaging analysis showed normal abdominal
ultrasound findings and X-rays of the chest, thorax, lumbosacral
region and pelvis. CT reconstruction of the sacroiliac joint
indicated multiple round hypodense lesions with a hyperdense
center, as well as some cortical destruction and soft tissue
swelling in the lumbar and sacral vertebrae, and the left ilium
regions (Fig. 1). A
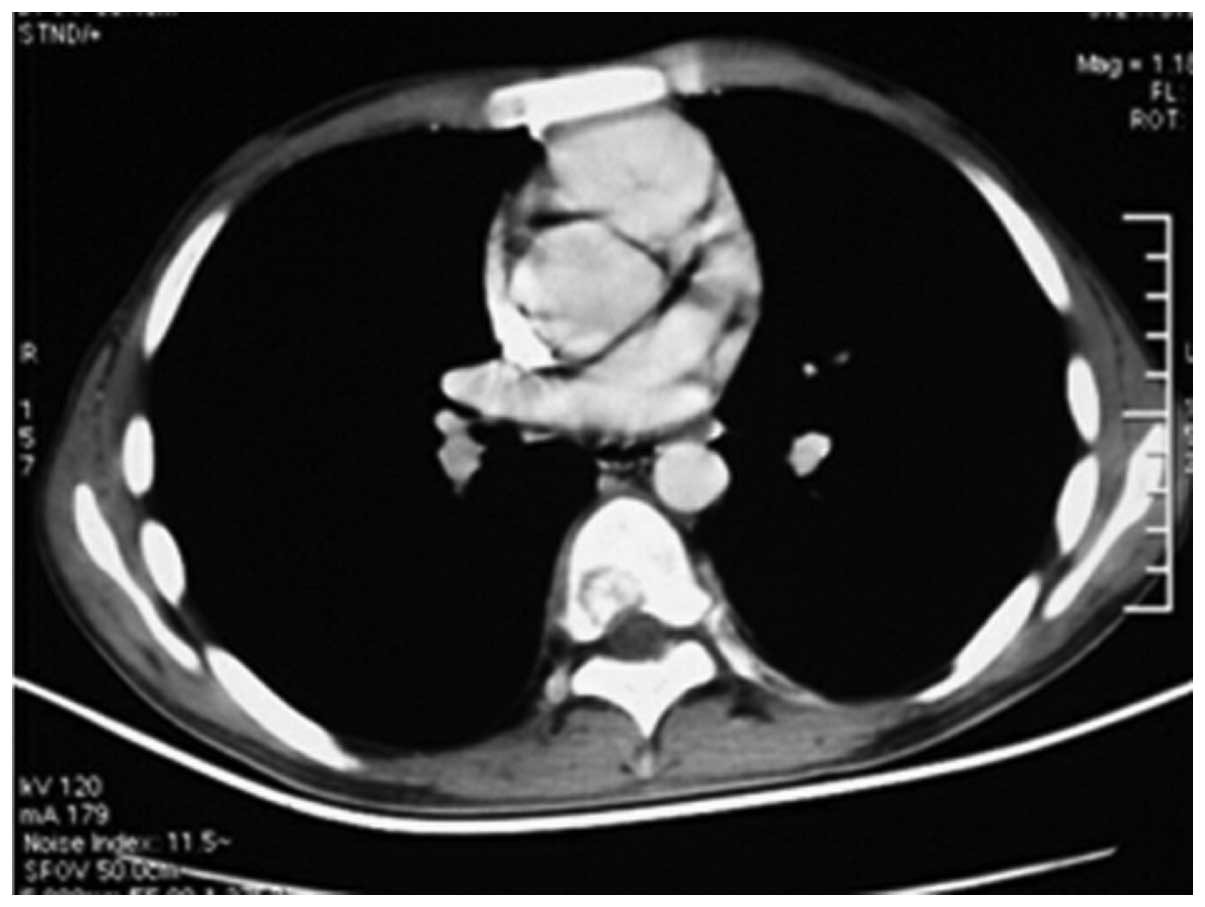
contrast-enhanced CT scan of the chest, with Omnipaque™ (1.5 ml/kg;
GE Healthcare Life Sciences, Shanghai, China) as the contrast
enhancement agent, demonstrated an irregular patchy hypodense
signal in the left lung lobe with a patchy translucent shadow
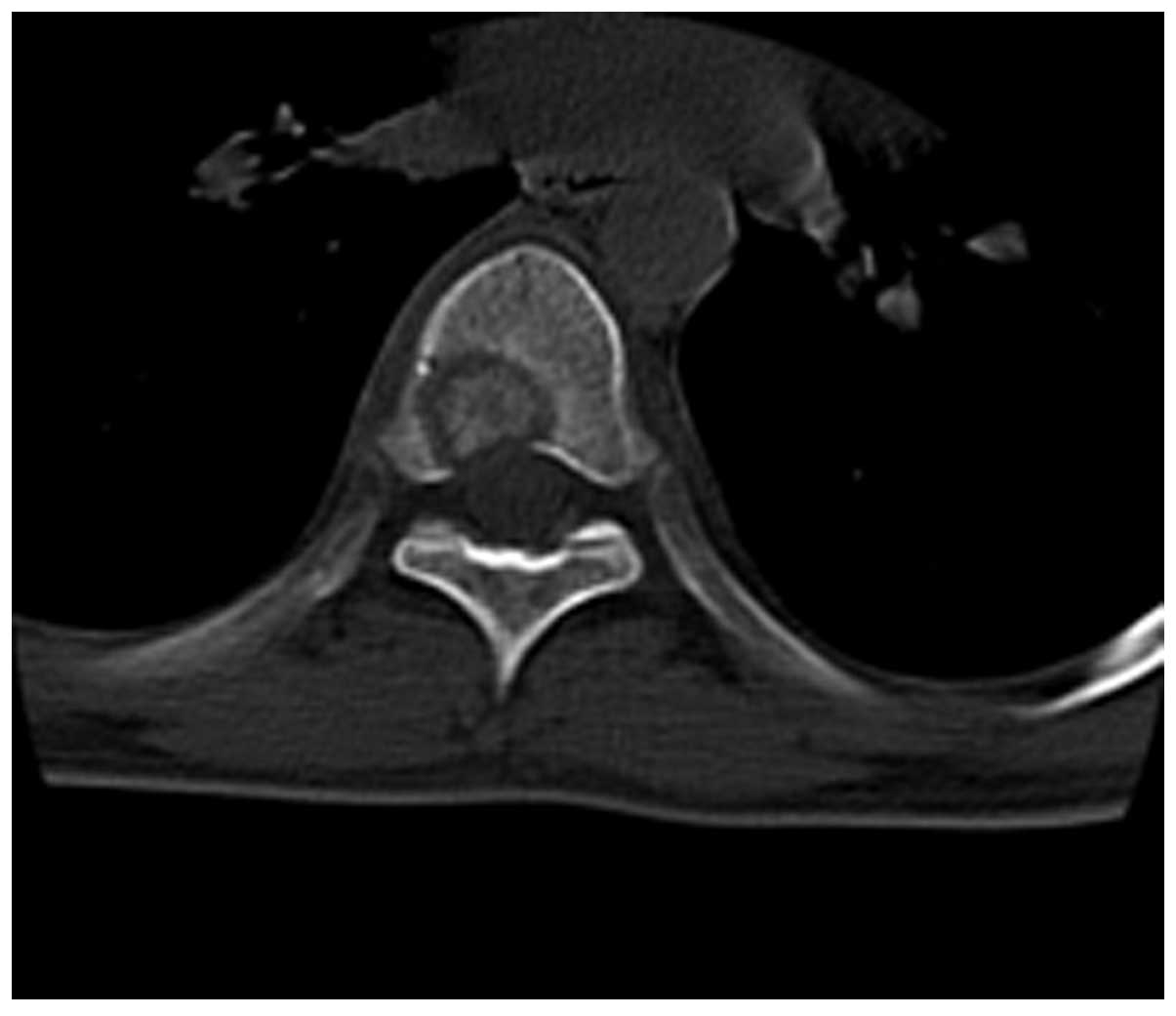
inside, which was enhanced heterogeneously (Fig. 2). A chest CT scan showed multiple
round hypodense lesions with higher central density in the thoracic
vertebrae, ribs and sternum (Fig.
3). Furthermore, a CT reconstruction of the thoracic spine
indicated bone destruction with partial cortical perforation
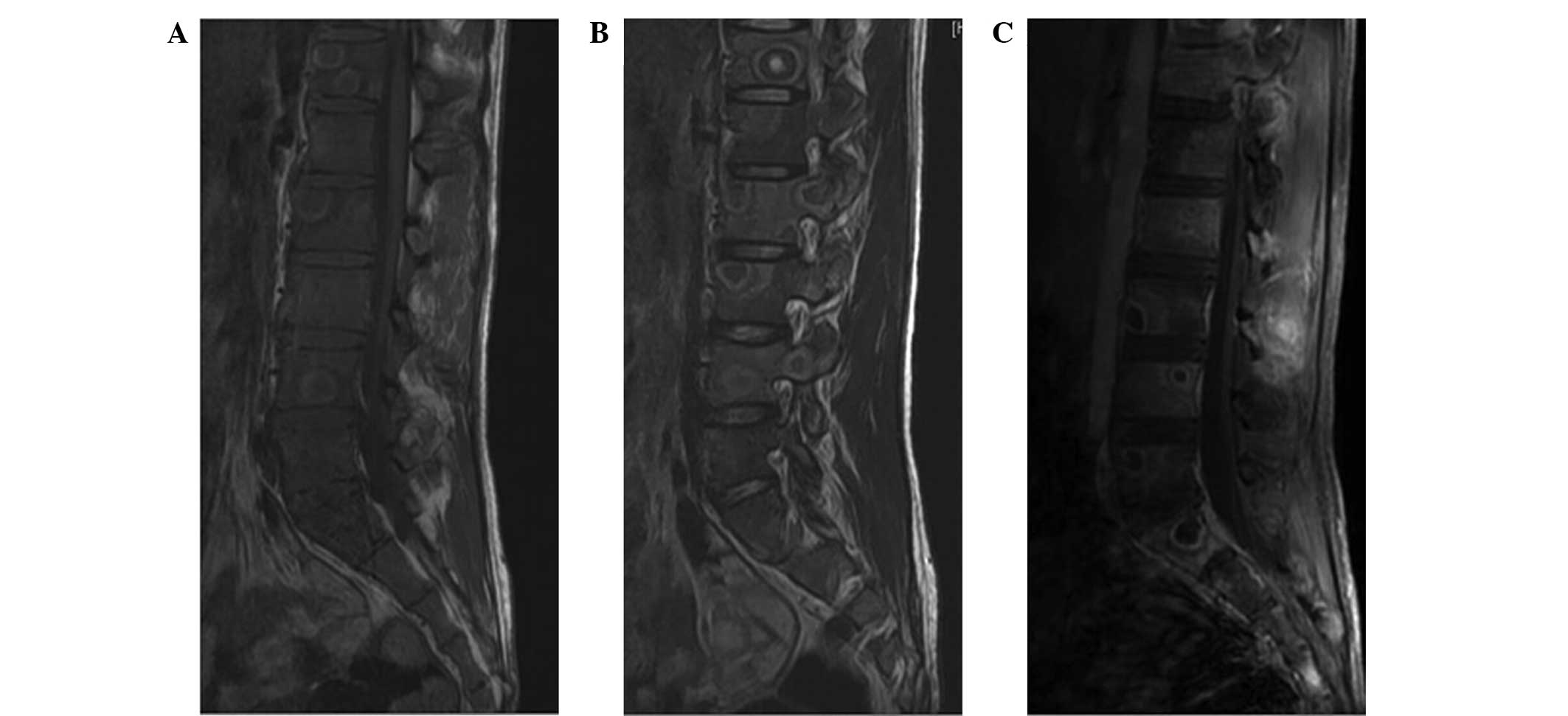
(Fig. 4). MRI scans revealed
multiple round ring signal shadows with a continuous finishing
border from Th12 to S4 in the anterior, central and posterior
elements, but not in the end plate. In addition, sagittal
T1-weighted and T2-weighted images revealed a hypodense signal in
the internal of the lesions and a slightly hypodense signal in the
peripheral region, which was accompanied by soft tissue swelling,
with visible ring enhancement and soft tissue enhancement following
intravenous administration of gadolinium (GE Healthcare Life
Sciences) (Fig. 5).
Based on the symptoms and all the aforementioned
examinations, lymphoma, metastatic disease or bone TB were
suspected. Since the CT and MRI findings did not allow for a final
diagnosis, a CT-guided biopsy from the lesions in the Th7
vertebral, left iliac and adjacent left lung using an 8-gauge
needle (Yangzhou City Jiangzhou Medical Instrument Co., Ltd.,
Yangzhou, China) was performed to confirm the diagnosis. However,
no evidence of granulomata, necrosis, lymphoma or other
malignancies was observed. Subsequently, an open biopsy was
performed in order to establish a pathological diagnosis, during
which fish-shaped soft tissue adhesion with surrounding tissues
under the lamina of Th7 and local sequestrum formation were
observed. Part of the surrounding soft tissues and bone lesions
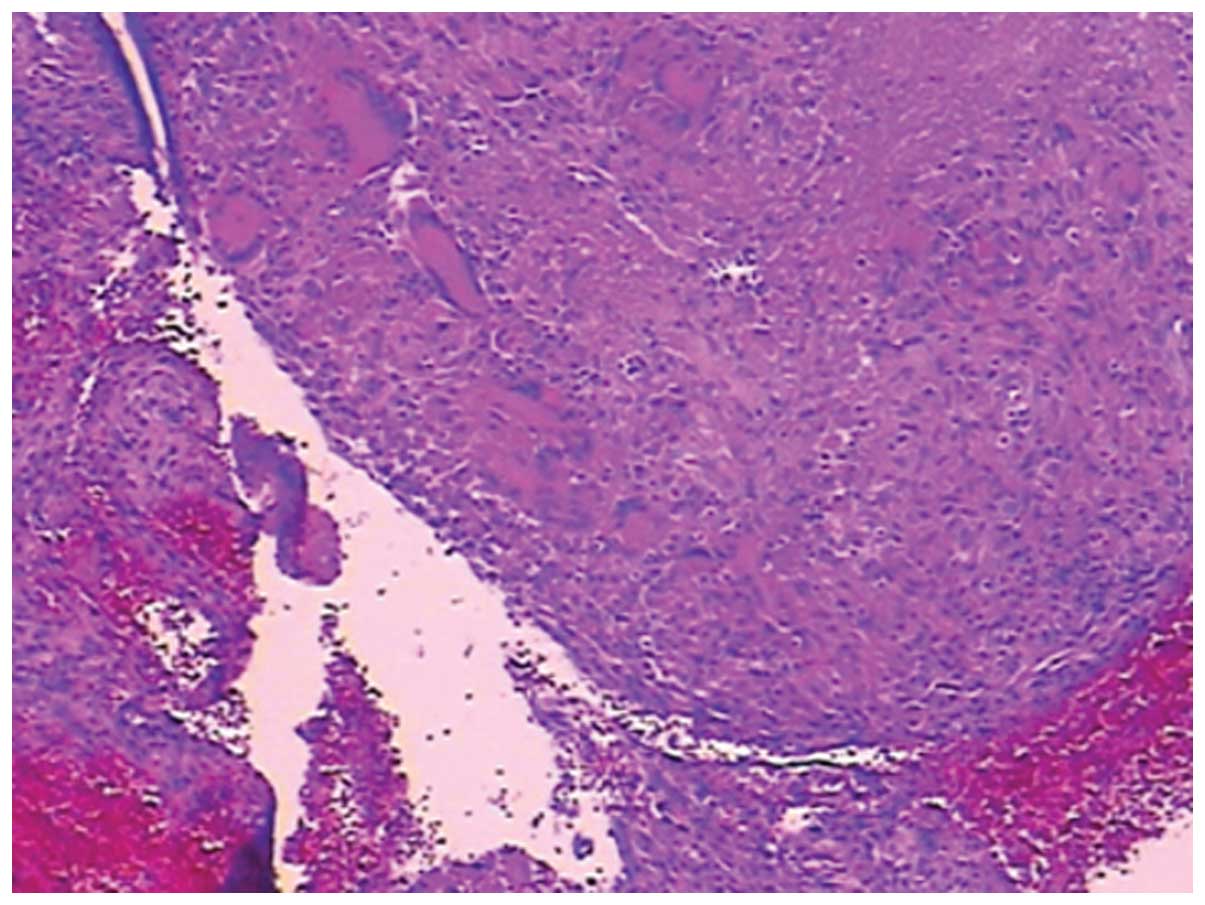
were removed for pathological examination and culturing. Upon
hematoxylin and eosin staining of the tissue and visualization
under the Olympus BX43 microscope (Olympus Corporation, Tokyo,
Japan), a large amount of necrosis, epithelioid cells, Langerhans
giant cells and dead bone were observed (Fig. 6), which are characteristics of TB
(2,5). The results of Acid-Fast Bacilli
culturing (Sinobest Biotech Co., Ltd., Shanghai, China) were
negative; however, a polymerase chain reaction performed by
Shanghai Genechem Co., Ltd. (Shanghai, China) was positive for TB.
Based on these observations, a diagnosis of multifocal skeletal TB
was established.
The patient was discharged from the hospital on 27th
September 2011. Postoperatively, the patient was administered a
common quartet anti-TB chemotherapy regimen (2,5),
including isoniazid (300 mg/day), rifampicin (600 mg/day),
pyrazinamide (750 mg/day) and ethambutol (750 mg/day; all Shanghai
Sine Pharmaceutical Co., Ltd., Shanghai, China) for 12 months. The
patient's symptoms greatly improved after 1 month of anti-TB
treatment and the ESR decreased to 65 mm/h. At the final follow-up
on 11th March 2013, the patient was free of symptoms and the ESR
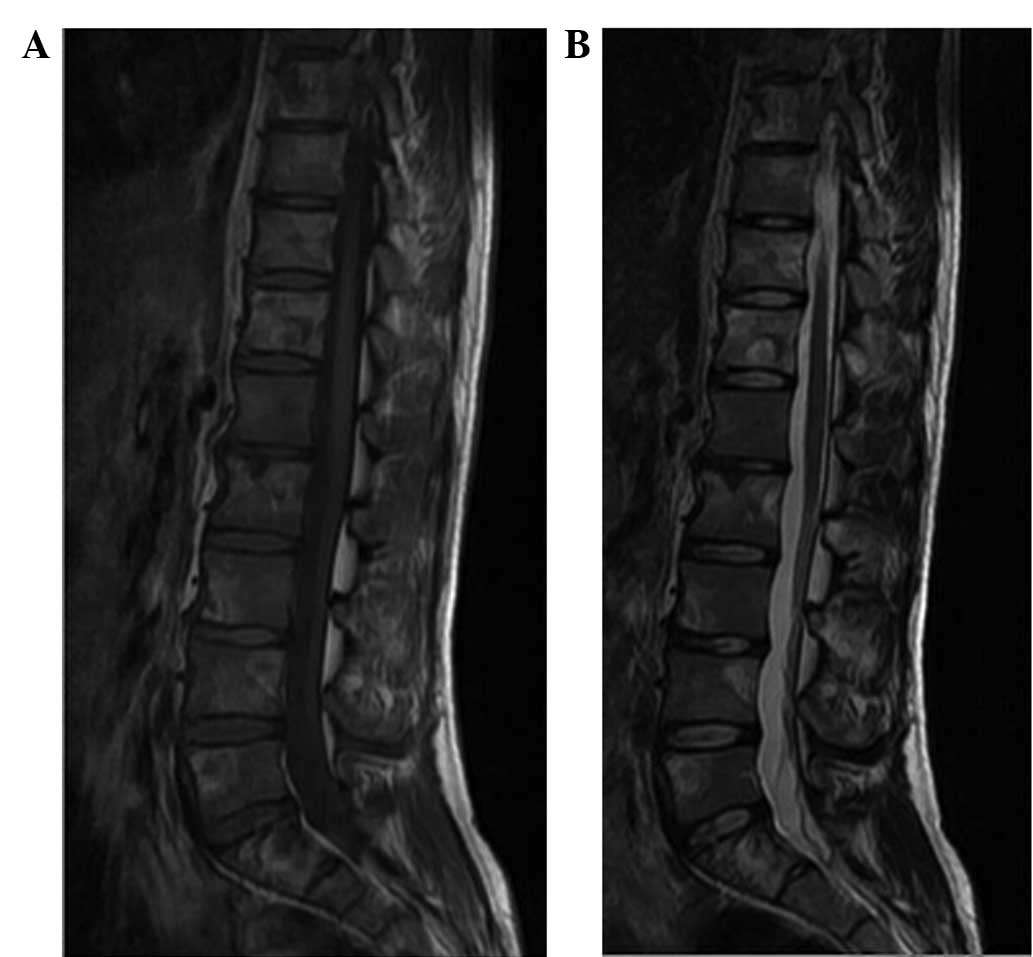
had decreased to the normal value. MRI scans obtained following 20
months of anti-TB therapy showed that the range of the extensive
abnormal signal intensity had become smaller, as compared with that
before anti-TB treatment was initiated (Fig. 7).
Informed consent was obtained from the patient's
family prior to the publication of the present case.
Discussion
TB remains a major cause of morbidity and mortality
worldwide, and is responsible for ~1.6 million deaths per year
(1,4). According to the World Health
Organization, ~8.8 million new cases of TB occur every year
worldwide (5,8). Multifocal skeletal TB has rarely been
reported in non-immunocompromised patients and in patients with
normal pulmonary findings, particularly in China (5,9). The
spine is the most commonly affected site, of which the upper lumbar
and lower thoracic regions are the most frequently involved,
comprising 50% of all multifocal skeletal TB cases (3–6). The
average number of vertebrae that are affected by multifocal TB, as
seen radiologically, is 3.0 in children and 2.5–3.8 in adults
(10). In the present case, there
were multiple round hypodense lesions in the ribs, sternum,
multi-segment thoracic, multi-segment lumbar and sacral vertebrae,
and ilium regions, accompanied by some adjacent soft tissue
swelling.
A positive PPD test is a fundamental finding in TB
patients; however, a negative test is not sufficient to exclude the
disease. Although radiological findings do not firmly establish the
diagnosis in the case of a negative PPD result, imaging remains the
most useful diagnostic tool in such cases (5,6,10). The characteristic findings of spinal
TB include destruction of two adjacent vertebral bodies,
destruction of the intervening disc, and the occurrence of
paravertebral and epidural abscesses (7,11).
Skeletal TB does not present any specific features
on radiological images in the early stages of the disease, thus
mimicking metastatic tumors or certain primary osseous lesions,
such as eosinophilic granuloma, particularly if multiple
destructive lesions are present (5,7,12). Plain radiography is of little help
unless the collapse of the disc margin or vertebra body appears
(4–7). In addition, CT scans are unable to show
the early alterations in the vertebral marrow and to differentiate
an infectious disease from neoplastic involvement (4–7). By
contrast, MRI has been shown to be a more sensitive and specific
imaging modality that may guide the diagnosis at early stages of
skeletal TB. The typical MRI patterns are abnormal signal
intensities appearing hypointense or isointense on a T1-weighted
image of the affected vertebral bodies and discs and hyperintense
on a T2-weighted image of the osseous, and soft-tissue changes with
heterogeneous enhancement of the vertebral body (4–7,11). Overall, the sensitivity and
specificity of MRI for TB may be 100 and 88.2%, respectively
(5,7). In the present case, the MRI features
included multiple round hypodense lesions with finishing borders in
the thoracic, lumbar and sacral vertebrae, which was not sufficient
evidence for the diagnosis of TB; on the contrary, these
observations were suggestive of hematological malignancies, such as
lymphoma or multiple myeloma, or metastatic diseases. The common
characteristics of end-plate disruption and high signal intensity
of the intervertebral disc were not demonstrated. Therefore, the
presentation of the TB case reported in the current study is
considered unusual.
To the best of our knowledge, the present study is
the first to report an extremely rare case of multifocal
osteoarticular TB with multiple round hypodense lesions and a
surprisingly negative PPD test result. The ETB and disseminated
forms of the disease are usually more frequent in certain patients,
such as those with a much older age, malnutrition and hemodialysis,
as well as immunocompromised and in particular HIV-infected
individuals (5,6). However, the current patient was a
healthy 19-year-old male with no signs of systemic involvement and
a negative HIV status. This demonstrated the diagnostic
difficulties of the atypical forms of TB.
In patients with skeletal TB, the onset of symptoms
is generally insidious, without general alarming signs, such as
fever, night sweats, toxicity or extreme weakness. This condition
may mimic malignant diseases, both clinically and radiographically.
Although CT and MRI are reliable techniques that help establish a
diagnosis, biopsy or CT-guided needle aspiration remain essential
for accurate diagnosis and adequate treatment. The advantage of
needle aspiration is that it is a less invasive technique; however,
only a small number of specimens can be obtained, particularly when
the lesions are sclerotic, and thus the diagnosis rate is only
81.0% in children (13) and 91.3% in
adults (14). Hao et al
(15) concluded that the diagnostic
accuracy of CT-guided thoracic spinal biopsy using a 16-gauge
needle was 90.5% overall, as the diagnostic accuracy was
significantly lower for the middle thoracic spine (90.0%) compared
with that for the lower spine (97.6%), as well as lower for
sclerotic lesions (81.3%) compared with that for lytic lesions
(96.4%). Similarly, in the present study, the CT-guided aspiration
using an 8-gauge needle was not able to confirm the diagnosis,
possibly due to the limited amount of tissue acquired and the
histological nature of the lesion itself, resulting in the use of
open biopsy to establish the diagnosis.
Multidrug anti-TB therapy including isoniazid,
rifampin, ethambutol and pyrazinamide advocated for an approximate
duration of 12–18 months usually leads to complete resolution of TB
(2,5). Medical treatment is highly effective
when administered appropriately, as performed in the present
study.
The mean time to diagnosis is reported to be 16–19
months after the presentation of symptoms (11). Ringshausen et al (12) described the fatal case of a patient
with spinal TB, who was mistakenly irradiated for suspected
metastatic lung cancer of the spine. The authors claimed that the
most common cause in delayed diagnosis is failure to consider this
disease (12). Thus, TB should be
considered in all patients with multiple round hypodense lytic
lesions of the skeletal system, especially in countries endemic for
TB, in order to avoid delays that may result in irreversible damage
and in a high mortality rate.
In conclusion, the diagnosis of multifocal skeletal
TB is difficult for various reasons, requiring careful
consideration and numerous examinations. A high index of suspicion
for the possibility of TB appearance has to be maintained in any
patient with multiple round hypodense lytic lesions of the skeletal
system in countries endemic for TB. In addition, MRI is
particularly valuable in the diagnostic and follow-up procedures.
However, confirmation of the diagnosis may only be possible
following biopsy.
References
|
1
|
Dye C, Scheele S, Dolin P, Pathania V and
Raviglione MC: Consensus statement. Global burden of tuberculosis:
Estimated incidence, prevalence and mortality by country. WHO
global surveillance and monitoring project. JAMA. 282:677–686.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Moon MS, Moon YW, Moon JL, Kim SS and Sun
DH: Conservative treatment of tuberculosis of the lumbar and
lumbosacral spine. Clin Orthop Relat Res. 40–49. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yilmaz MH, Kantarci F, Mihmanli I and
Kanberoglu K: Multifocal skeletal tuberculosis. South Med J.
97:785–787. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Agarwal A, Khan SA and Qureshi NA:
Multifocal osteoarticular tuberculosis in children. J Orthop Surg
(Hong Kong). 19:336–340. 2011.PubMed/NCBI
|
|
5
|
Hong L, Wu JG, Ding JG, Wang XY, Zheng MH,
Fu RQ, Li WB, Peng WX, He WF and Sun QF: Multifocal skeletal
tuberculosis: Experience in diagnosis and treatment. Med Mal
Infect. 40:6–11. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Marudanayagam A and Gnanadoss JJ:
Multifocal skeletal tuberculosis: A report of three cases. Iowa
Orthop J. 26:151–153. 2006.PubMed/NCBI
|
|
7
|
Danchaivijitr N, Temram S, Thepmongkhol K
and Chiewvit P: Diagnostic accuracy of MR imaging in tuberculous
spondylitis. J Med Assoc Thai. 90:1581–1589. 2007.PubMed/NCBI
|
|
8
|
Wright GD and Sutherland AD: New
strategies for combating multidrug-resistant bacteria. Trends Mol
Med. 13:260–267. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang Y, Zhang Y and Ma J: The prospect of
incidental detection of unsuspected skeletal tuberculosis by bone
scintigraphy should not be overlooked. Clin Nucl Med. 32:435–439.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
St Clair Strange FG: Current concepts
review. Tuberculosis of bones and joints (78-A:288-298, Feb. 1996)
by Watts and Lifeso. J Bone Joint Surg Am. 80:6041998.PubMed/NCBI
|
|
11
|
Moore SL and Rafii M: Imaging of
musculoskeletal and spinal tuberculosis. Radiol Clin North Am.
39:329–342. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ringshausen FC, Tannapfel A, Nicolas V,
Weber A, Duchna HW, Schultze-Werninghaus G and Rohde G: A fatal
case of spinal tuberculosis mistaken for metastatic lung cancer:
Recalling ancient Pott's disease. Ann Clin Microbiol Antimicrob.
8:322009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ballah D, Nijs E, Keller MS, Zhu X,
Krishnamurthy G and Cahill AM: Percutaneous CT-guided vertebral
bone biopsy in children. Pediatr Radiol. 43:582–588. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Poyanli O, Akan K, Unay K and Tangay C:
CT-guided percutaneous transpedicular biopsy for the diagnosis of
vertebral lesions. Acta Orthop Belg. 74:503–506. 2008.PubMed/NCBI
|
|
15
|
Hao DJ, Sun HH, He BR, Liu TJ, Jiang YH
and Zhao QP: Accuracy of CT-guided biopsies in 158 patients with
thoracic spinal lesions. Acta Radiol. 52:1015–1019. 2011.
View Article : Google Scholar : PubMed/NCBI
|