Introduction
Valvular heart disease (VHD) is a major health
problem afflicting the elderly in particular, with a prevalence of
2.5% in the United States. VHD occurs due to congenital defects or
because of acquired pathology (1).
Calcific aortic valve disease (CAVD) is initiated as aortic valve
sclerosis (AVSc), which is a mild thickening of the valve, to
aortic valve stenosis (AVS), which results in severe impairment of
the valve motion. CAVD is increasingly present in the aging
population, reaching epidemic proportions, with approximately one
third of individuals aged >65 years, showing sub-clinical
evidence of CAVD, in the form of aortic sclerosis (2). As a large proportion of the worldwide
population is becoming aged, the prevalence of acquired forms of
VHD is expected to rise (3). Age,
gender, tobacco use, hypercholesterolemia, rheumatic heart disease
and hypertension constitute significant risk factors of acquired
CAVD. Congenital CAVD primarily results from the disturbed
expression of genes that are involved in normal heart valve
development. Congenital valve abnormalities comprise almost 50% of
the cases of congenital heart defects (CHD) (4). Advances in the identification of these
defects and in the associated care for infants suffering from CHDs
is on the rise, thus increasing the net incidence and burden of
congenital valve diseases (4). Type
II diabetes is considered an important risk factor for native CAVD
(5). The pathogenesis of congenital
and acquired CAVD is likely due to the interplay of genetic and
environmental influences, even though the precise mechanisms are
not known.
Although the incidence of VHD is high, therapeutic
approaches for this disease are limited. The only available primary
clinical approach for valve repair or replacement is surgery as the
primary treatment (6,7). In fact, aortic valve replacement is the
second most frequent cardiac surgery following coronary artery
bypass grafting (8). CAVD advances
to calcific aortic stenosis (CAS), which is the most severe form of
the disease. It is extremely debilitating affecting as many as 2%
of individuals >60 years of age, requiring surgery to preclude
death, once the symptoms become evident (9). CAVD is mainly diagnosed by clinical
examination, echocardiography and cardiac catheterization. There
are also many potential biomarkers that provide clinically useful
information regarding the extent, severity, progression and
prognosis of CAVD (8).
Structure of cardiac valve and pathogenesis
of CAVD
The atrioventricular valves (mitral and tricuspid)
and the semilunar valves (aortic and pulmonic) are two types of
mature heart valves. These valves consist of an outer layer of
valve endothelial cells (VECs) surrounding three layers of
extracellular matrix each with specialized function and
interspersed with valve interstitial cells (VICs) (10). Changes in the functionality and
localization of matrix components potentially lead to VHD, since
the proper organization of extracellular matrix (ECM) is essential
in maintaining overall valve morphology and normal valve function.
The three layers of ECM, consisting of collagens, proteoglycans and
elastin, collectively contribute to the biomechanical support for
the valves and any derangements in these morphological units can
have detrimental effects on the complicated structures of valves
that open and close approximately 100,000 times daily in order to
maintain proper directionality of blood flow through the heart
chambers (11). The protective
endothelium over the surface of the valve leaflets is formed by the
VECs, which communicate with VICs in the underlying layer and
regulate their response to alterations in the blood flow (10). Genetic or acquired/environmental
causes that disrupt the normal organization and composition of the
ECM and communication between VECs and VICs alter valve mechanics
and interfere with the valve leaflet function, culminating in heart
failure (11).
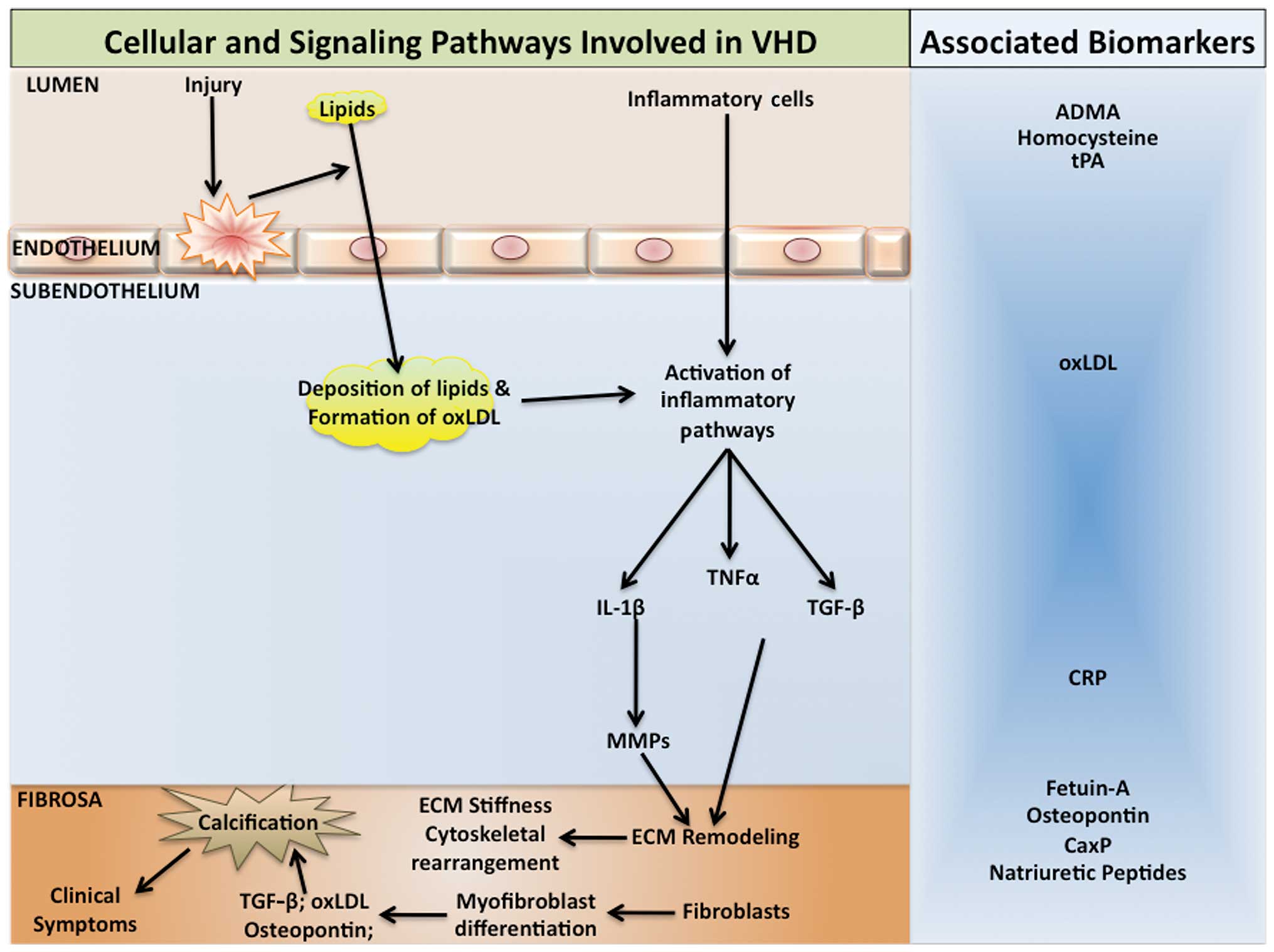
Histopathology of CAVD
The histopathologic heterogeneity of CAVD indicates
the involvement of diverse cell-dependent mechanisms that regulate
calcium load on the valve leaflets (12), as well as the participation of
different cell types, including interstitial cells, endothelial
cells and cardiac chondrocytes, in valve biomineralization
(13) (Fig. 1). Histopathologic studies (12) demonstrated the presence of calcified
nodules composed of amorphous calcium phosphate, without any
organization into specific histological structures. In these
affected valves, similar to atherosclerosis, there are signs of
inflammation and bone morphogenetic protein-2 expression (12). Additionally, woven and lamellar bone
with osteoblast matrix production and vascularization has been
identified in calcifying native aortic valves (14). During the pathogenesis of CAVD, one
of the earliest events following endothelial cell dysfunction is
the accumulation of lipids and subendothelial matrix at the
ventricular surface of the valve with downward displacement of the
subjacent elastic lamina while plaque-like subendothelial deposits
occur on the aortic surface of the valve. It has been suggested
that VECs via the endothelial-mesenchymal transition (EMT), can
contribute to calcifying vascular cell types, in response to
stimuli that promote arteriosclerotic calcification (15). Athough the contribution of acquired
immunity to the progression of CAVD remains to be determined,
recent data indicate that an adaptive immune response is likely
activated in CAVD as clonally expanded effector-memory T-cell
populations are observed in the valve and in the circulation of
patients with severe CAS (16)
(Fig. 1).
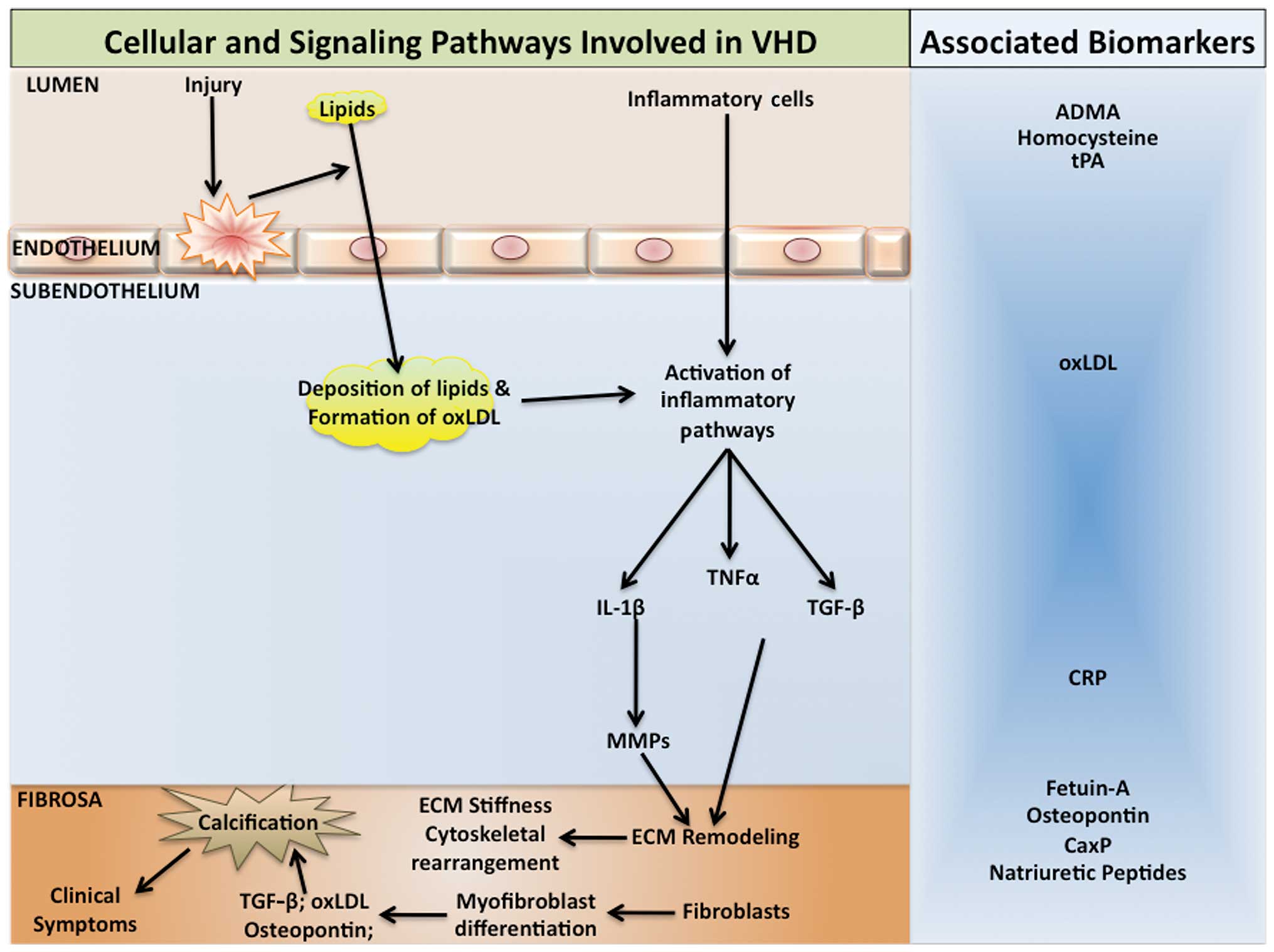 | Figure 1.Pathogenic pathways involved in
calcific aortic valve disease. Mechanical stress or injury on the
aortic valve along with other atherosclerotic risk factors causes
valvular endothelial dysfunction. This leads to lipid deposition in
the subendothelium where they are oxidized and factors such as
oxidized low-density lipoprotein (oxLDL) are formed. Inflammatory
cells such as monocytes, infiltrate the valve tissue and form foam
cells by phagocytosis of the lipids. Inflammatory cytokines are
released which promote remodeling of the extracellular matrix.
Fibroblasts transdifferentiate into valvular myofibroblasts with an
osteoblast-like phenotype, and cause calcification. Biomarkers are
associated with different stages of CAVD and can be useful in
following the pathogenesis of the disease. TNFα, tumor necrosis
factor α; TGF-β, transforming growth factor-β; IL-1β,
interleukin-1β; MMP, matrix metalloproteases; ECM, extracellular
matrix; ADMA, asymmetric dimethylaminoarginine; tPA, tissue
plasminogen activator; CRP, C-reactive protein; CaxP, calcium
phosphate product. |
The earliest amorphous calcium phosphate deposition
occurs in a stippled pattern on the fibrosal interface with the
fibro-fatty expansion of the valve spongiosa (17) and these calcium deposits form readily
via epitaxial mineral deposition on a number of nidi, including
cholesterol crystals (18), collagen
and fragmented elastin fibers (19).
Coexpression of collagen and alkaline phosphatase, which in the
elastin-rich environment can trigger mineralization, has been
demonstrated in CAVD by immunogold electron microscopy (20). Biomineralization also occurs in the
absence of alkaline phosphatase, as matrix vesicles contain
molecules such as annexin A5, annexin A6, and phosphatidylserine,
which readily bind calcium and nucleate mineral deposition
(21) while the absence of
inhibitors of mineralization such as pyrophosphate,
phosphoosteopontin, and fetuin can further promote the deposition
of calcium (22). However, following
the initiation of mineral deposition, circulating osteoprogenitors
(COPs) derived from myeloid cell lineage arrive to the site and
play an important role in the subsequent stages of disease
response. T These COP cells most likely originate from the bone
marrow. The presence of type I collagen (+) CD45 (+) COP cells in
valves has been detected at the fibroproliferative and
neovascularization phases of disease, whereas CD45 (+) cells are
observed in ossifying and non-ossifying valve segments (23). Circulating myeloid calcifying cells,
which are positive for alkaline phosphatase and osteocalcin are
elevated in type II diabetes patients, and may contribute to the
increased incidence of CAVD in these patients (24).
Inflammation and activation of CAVD
pathogenesis
Inflammation is known to play a significant role in
many types of macrovascular calcification, including CAVD (25). A number of the
inflammation-associated factors, including tumor necrosis factor,
interleukin 1-β, advanced glycosylation-end products, and oxidized
low-density lipoprotein (oxLDL) cholesterol, activate vascular
biomineralization and vascular osteogenic signaling processes
(26) (Fig. 1). Aggravated fibrocalcific responses
have been observed in CAVD in association with increased levels of
oxLDL (27). By employing
histological studies on human samples and mouse models, it has been
demonstrated that reactive oxygen species, specifically hydrogen
peroxide, has a pro-osteogenic and pathogenic role in CAVD and that
a number of the enzymatic mechanisms that counteract oxidative
stress are downregulated in valves during the pathogenesis of CAVD
(28). Specifically, hydrogen
peroxide has been shown to activate osteogenic Cbfa1/runt-related
transcription factor 2 (Runx2) and Msx2/Wnt signaling pathways to
promote mineralization and these pathways are activated in
calcifying human aortic valves (28).
Genetics of CAVD
Advances in genomic technologies have led to the
identification of several genes that contribute to the normal
development and function of the four heart valves and to the
identification of many genetic abnormalities in some of these genes
in congenital form of CAVD (29).
The most common congenital valve anomalies are bicuspid aortic
valve (BAV) and mitral valve prolapse (MVP). BAV is estimated to
have a prevalence of 1–2% (30).
Normal aortic valve develops until there are three cusps, whereas
in BAV disease there is a fusion of two of the leaflets during
development, leading to significant morbidity primarily through
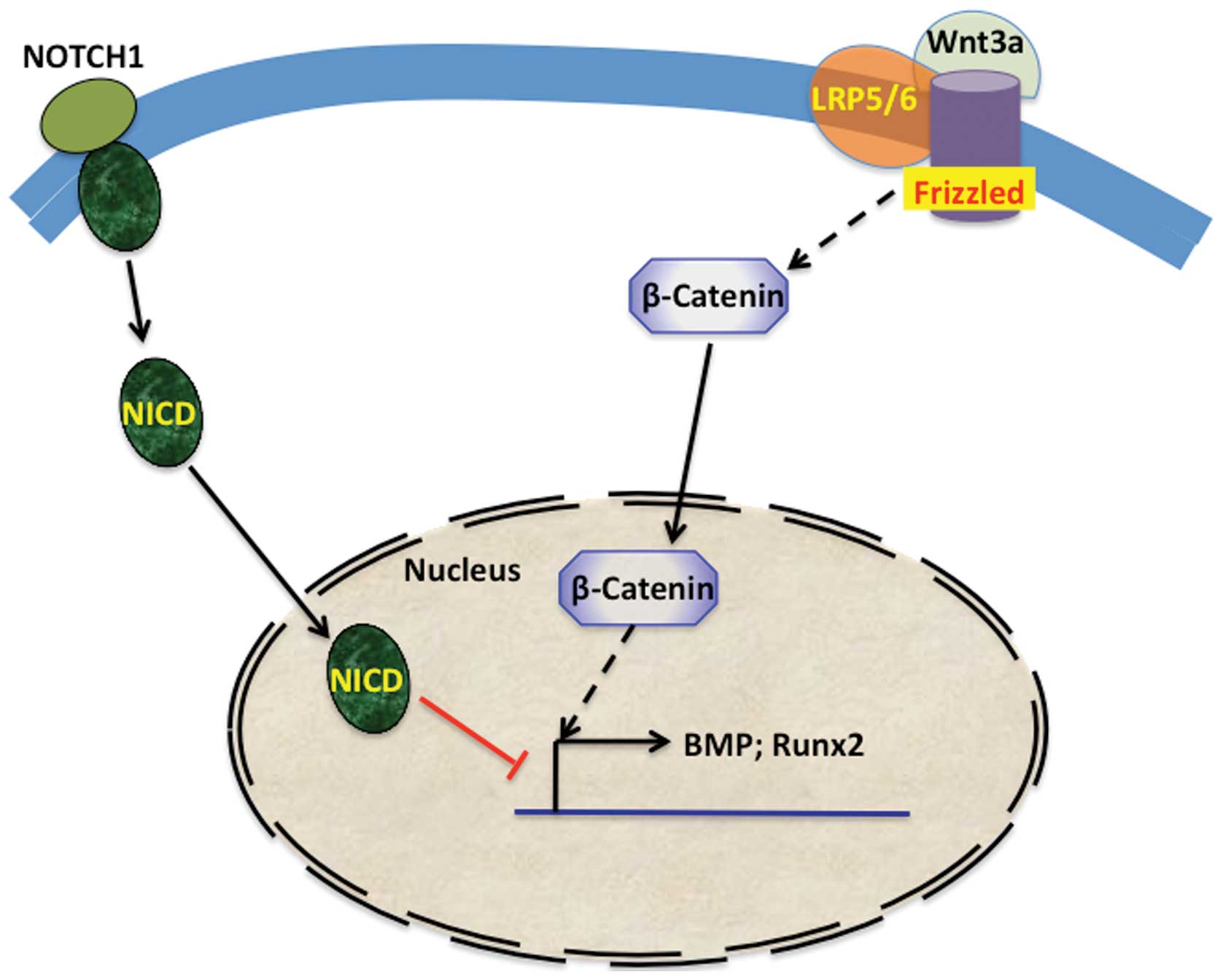
valve calcification. NOTCH1, a member of the Notch signaling
pathway, was one of the first mutated genes identified in BAV. The
Jagged/Notch signaling pathway, which plays an important role in
bone formation is also central to valve morphogenesis and CAVD.
Jagged1 signals from endothelial cells support the Notch1-mediated
EMT necessary for cardiac valve morphogenesis during the
development of heart (31).
Heterozygous loss-of-function NOTCH1 mutations segregate with the
disease in families with autosomal dominant BAV (32). Ex vivo, Notch can suppress
Runx2 signaling and mineralization (Fig.
2) in VICs (33).
MVP affects 2–3% of the population and is manifested
by systolic displacement of a thickened mitral valve leaflet into
the left atrium. This condition is normally observed in adults and
often associated with the fibromyxomatous degeneration of the
leaflets, valve regurgitation, congestive heart failure,
arrhythmias, and infective endocarditis (34). Involvement of transforming growth
factor-β (TGF-β), which is needed for remodeling and maintenance of
mitral valve, in MVP pathogenesis has been suggested (35). TGF-β, bone morphogenetic proteins,
and Wnt, which act via signaling through ALK- and LDL
receptor-related protein-receptor complexes to promote bone
formation, mineralization, and skeletal homeostasis (Fig. 2), also play an important role in the
earliest stages of aortic valve morphogenesis (36). A recent genome-wide association study
that included CAVD and mitral annular calcification patients
identified a single-nucleotide polymorphism (SNP) in the
lipoprotein (a) locus only in CAVD patients (37).
Treatment choices and biomarkers
As mentioned previously, surgical valve replacement
is the widely accepted treatment of choice for AVS, with either
mechanical or biological prostheses. Although there are other
treatment options, including balloon aortic valvuloplasty or
percutaneous valve replacement, they have many limitations. For
example, aortic valvuloplasty showed non-trivial complication
rates, but moderately high rates of aortic insufficiency with much
higher rates of recurrence (38).
Percutaneous aortic valve replacement is currently being examined
in several studies and appears to be suitable for select groups of
patients (39).
Numerous biomarkers have been suggested for
following the pathogenesis of aortic valve disease, but not all
biomarkers are clinically useful candidates. Presently, asymmetric
dimethylarginine, fetuin-A, calcium phosphate product, natriuretic
peptides and osteopontin are the most promising candidates. A
circulating level of asymmetric dimethylarginine, which is involved
in endothelial cell dysfunction, was found to correlate with the
extent of AVS (40). Fetuin-A, an
inhibitor of soft tissue calcification, also seems to be a good
candidate as its serum levels show strong inverse correlation with
the extent of valve degeneration and calcification (41). Osteopontin is directly associated
with the ectopic calcification process, which occurs during the
latter stages of CAVD making this protein a specific biomarker for
CAVD (42).
In conclusion, CAVD and other types of VHDs are
reaching epidemic status in their prevalence in many developed and
developing countries. CAVD ranges from AVSc, i.e., mild thickening
of the valve, to AVS, which is severe impairment of the valve
motion. Risk factors for acquired valve diseases include age,
gender, tobacco use, hypercholesterolemia, hypertension, and type
II diabetes mellitus. Diverse cell-dependent mechanisms and
signaling pathways orchestrate valve biomineralization with the
participation of different cell types including interstitial cells,
endothelial cells, cardiac chondrocytes, and COPs. In addition,
several genetic mutations that cause congenital valve diseases have
been identified along with specific SNPs associated with CAVD.
Despite the many advances, there is still a lack of pharmacological
treatments for the valve diseases and the most widely accepted
approach is surgery. Recent advances in the identification of
molecular mechanisms involved in the development and pathogenesis
of valvular disease are making a significant impact in our
understanding of the heart valve disease.
References
|
1
|
Go AS, Mozaffarian D, Roger VL, Benjamin
EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al:
American Heart Association Statistics Committee and Stroke
Statistics Subcommittee: Heart disease and stroke statistics-2013
update: a report from the American Heart Association. Circulation.
127:e6–e245. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rajamannan NM, Evans FJ, Aikawa E,
Grande-Allen KJ, Demer LL, Heistad DD, Simmons CA, Masters KS,
Mathieu P, O'Brien KD, et al: Calcific aortic valve disease: not
simply a degenerative process: a review and agenda for research
from the National Heart and Lung and Blood Institute Aortic
Stenosis Working Group. Executive summary: Calcific aortic valve
disease-2011 update. Circulation. 124:1783–1791. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
d'Arcy JL, Prendergast BD, Chambers JB,
Ray SG and Bridgewater B: Valvular heart disease: The next cardiac
epidemic. Heart. 97:91–93. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Le Gloan L, Mercier LA, Dore A, Marcotte
F, Ibrahim R, Mongeon FP, Asgar A, Miro J, Poirier N and Khairy P:
Recent advances in adult congenital heart disease. Circ J.
75:2287–2295. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Katz R, Wong ND, Kronmal R, Takasu J,
Shavelle DM, Probstfield JL, Bertoni AG, Budoff MJ and O'Brien KD:
Features of the metabolic syndrome and diabetes mellitus as
predictors of aortic valve calcification in the Multi-Ethnic Study
of Atherosclerosis. Circulation. 113:2113–2119. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Itagaki S, Adams DH and Anyanwu AC:
Triggers for surgical referral in degenerative mitral valve
regurgitation. Circ J. 77:28–34. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Maeda K, Kuratani T, Mizote I, Shimamura
K, Takeda Y, Torikai K, Nakatani S, Nanto S and Sawa Y: Early
experiences of transcatheter aortic valve replacement in Japan.
Circ J. 77:359–362. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Beckmann E, Grau JB, Sainger R, Poggio P
and Ferrari G: Insights into the use of biomarkers in calcific
aortic valve disease. J Heart Valve Dis. 19:441–452.
2010.PubMed/NCBI
|
|
9
|
Nightingale AK and Horowitz JD: Aortic
sclerosis: Not an innocent murmur but a marker of increased
cardiovascular risk. Heart. 91:1389–1393. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tao G, Kotick JD and Lincoln J: Heart
valve development, maintenance, and disease: The role of
endothelial cells. Curr Top Dev Biol. 100:203–232. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hinton RB Jr, Lincoln J, Deutsch GH,
Osinska H, Manning PB, Benson DW and Yutzey KE: Extracellular
matrix remodeling and organization in developing and diseased
aortic valves. Circ Res. 98:1431–1438. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mohler ER III, Gannon F, Reynolds C,
Zimmerman R, Keane MG and Kaplan FS: Bone formation and
inflammation in cardiac valves. Circulation. 103:1522–1528. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Boström KI, Jumabay M, Matveyenko A,
Nicholas SB and Yao Y: Activation of vascular bone morphogenetic
protein signaling in diabetes mellitus. Circ Res. 108:446–457.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Srivatsa SS, Harrity PJ, Maercklein PB,
Kleppe L, Veinot J, Edwards WD, Johnson CM and Fitzpatrick LA:
Increased cellular expression of matrix proteins that regulate
mineralization is associated with calcification of native human and
porcine xenograft bioprosthetic heart valves. J Clin Invest.
99:996–1009. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Balachandran K, Alford PW, Wylie-Sears J,
Goss JA, Grosberg A, Bischoff J, Aikawa E, Levine RA and Parker KK:
Cyclic strain induces dual-mode endothelial-mesenchymal
transformation of the cardiac valve. Proc Natl Acad Sci USA.
108:19943–19948. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Winchester R, Wiesendanger M, O'Brien W,
Zhang HZ, Maurer MS, Gillam LD, Schwartz A, Marboe C and Stewart
AS: Circulating activated and effector memory T cells are
associated with calcification and clonal expansions in bicuspid and
tricuspid valves of calcific aortic stenosis. J Immunol.
187:1006–1014. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Otto CM, Kuusisto J, Reichenbach DD, Gown
AM and O'Brien KD: Characterization of the early lesion of
‘degenerative’ valvular aortic stenosis. Histological and
immunohistochemical studies. Circulation. 90:844–853. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Laird DF, Mucalo MR and Yokogawa Y: Growth
of calcium hydroxyapatite (Ca-HAp) on cholesterol and cholestanol
crystals from a simulated body fluid: A possible insight into the
pathological calcifications associated with atherosclerosis. J
Colloid Interface Sci. 295:348–363. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schoen FJ and Levy RJ: Founder's Award,
25th Annual Meeting of the Society for Biomaterials, perspectives.
Providence, RI, April 28-May 2, 1999. Tissue heart valves: Current
challenges and future research perspectives. J Biomed Mater Res.
47:439–465. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rajamannan NM, Subramaniam M, Rickard D,
Stock SR, Donovan J, Springett M, Orszulak T, Fullerton DA, Tajik
AJ, Bonow RO, et al: Human aortic valve calcification is associated
with an osteoblast phenotype. Circulation. 107:2181–2184. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kapustin AN, Davies JD, Reynolds JL,
McNair R, Jones GT, Sidibe A, Schurgers LJ, Skepper JN, Proudfoot
D, Mayr M, et al: Calcium regulates key components of vascular
smooth muscle cell-derived matrix vesicles to enhance
mineralization. Circ Res. 109:e1–e12. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jahnen-Dechent W, Heiss A, Schäfer C and
Ketteler M: Fetuin-A regulation of calcified matrix metabolism.
Circ Res. 108:1494–1509. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Egan KP, Kim JH, Mohler ER III and Pignolo
RJ: Role for circulating osteogenic precursor cells in aortic
valvular disease. Arterioscler Thromb Vasc Biol. 31:2965–2971.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fadini GP, Albiero M, Menegazzo L, Boscaro
E, de Kreutzenberg Vigili S, Agostini C, Cabrelle A, Binotto G,
Rattazzi M, Bertacco E, et al: Widespread increase in myeloid
calcifying cells contributes to ectopic vascular calcification in
type 2 diabetes. Circ Res. 108:1112–1121. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wallby L, Janerot-Sjöberg B, Steffensen T
and Broqvist M: T lymphocyte infiltration in non-rheumatic aortic
stenosis: A comparative descriptive study between tricuspid and
bicuspid aortic valves. Heart. 88:348–351. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Towler DA: Molecular and cellular aspects
of calcific aortic valve disease. Circ Res. 113:198–208. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Stewart CR, Stuart LM, Wilkinson K, van
Gils JM, Deng J, Halle A, Rayner KJ, Boyer L, Zhong R, Frazier WA,
et al: CD36 ligands promote sterile inflammation through assembly
of a Toll-like receptor 4 and 6 heterodimer. Nat Immunol.
11:155–161. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
28
|
Miller JD, Chu Y, Brooks RM, Richenbacher
WE, Peña-Silva R and Heistad DD: Dysregulation of antioxidant
mechanisms contributes to increased oxidative stress in calcific
aortic valvular stenosis in humans. J Am Coll Cardiol. 52:843–850.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lincoln J and Garg V: Etiology of valvular
heart disease-genetic and developmental origins. Circ J.
78:1801–1807. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
McBride KL and Garg V: Heredity of
bicuspid aortic valve: Is family screening indicated? Heart.
97:1193–1195. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hofmann JJ, Briot A, Enciso J, Zovein AC,
Ren S, Zhang ZW, Radtke F, Simons M, Wang Y and Iruela-Arispe ML:
Endothelial deletion of murine Jag1 leads to valve calcification
and congenital heart defects associated with Alagille syndrome.
Development. 139:4449–4460. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Foffa I, Ait Alì L, Panesi P, Mariani M,
Festa P, Botto N, Vecoli C and Andreassi MG: Sequencing of NOTCH1,
GATA5, TGFBR1 and TGFBR2 genes in familial cases of bicuspid aortic
valve. BMC Med Genet. 14:442013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nus M, MacGrogan D, Martínez-Poveda B,
Benito Y, Casanova JC, Fernández-Avilés F, Bermejo J and de la
Pompa JL: Diet-induced aortic valve disease in mice
haploinsufficient for the Notch pathway effector RBPJK/CSL.
Arterioscler Thromb Vasc Biol. 31:1580–1588. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Freed LA, Levy D, Levine RA, Larson MG,
Evans JC, Fuller DL, Lehman B and Benjamin EJ: Prevalence and
clinical outcome of mitral-valve prolapse. N Engl J Med. 341:1–7.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lincoln J and Garg V: Etiology of valvular
heart disease-genetic and developmental origins. Circ J.
78:1801–1807. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Armstrong EJ and Bischoff J: Heart valve
development: Endothelial cell signaling and differentiation. Circ
Res. 95:459–470. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Thanassoulis G, Campbell CY, Owens DS,
Smith JG, Smith AV, Peloso GM, Kerr KF, Pechlivanis S, Budoff MJ,
Harris TB, et al: CHARGE Extracoronary Calcium Working Group:
Genetic associations with valvular calcification and aortic
stenosis. N Engl J Med. 368:503–512. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Balmer C, Beghetti M, Fasnacht M, Friedli
B and Arbenz U: Balloon aortic valvoplasty in paediatric patients:
Progressive aortic regurgitation is common. Heart. 90:77–81. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Webb JG, Chandavimol M, Thompson CR, Ricci
DR, Carere RG, Munt BI, Buller CE, Pasupati S and Lichtenstein S:
Percutaneous aortic valve implantation retrograde from the femoral
artery. Circulation. 113:842–850. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Vallance P, Leone A, Calver A, Collier J
and Moncada S: Accumulation of an endogenous inhibitor of nitric
oxide synthesis in chronic renal failure. Lancet. 339:572–575.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Koos R, Brandenburg V, Mahnken AH,
Mühlenbruch G, Stanzel S, Günther RW, Floege J, Jahnen-Dechent W,
Kelm M and Kühl HP: Association of fetuin-A levels with the
progression of aortic valve calcification in non-dialyzed patients.
Eur Heart J. 30:2054–2061. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Yu PJ, Skolnick A, Ferrari G, Heretis K,
Mignatti P, Pintucci G, Rosenzweig B, Diaz-Cartelle J, Kronzon I,
Perk G, et al: Correlation between plasma osteopontin levels and
aortic valve calcification: Potential insights into the
pathogenesis of aortic valve calcification and stenosis. J Thorac
Cardiovasc Surg. 138:196–199. 2009. View Article : Google Scholar : PubMed/NCBI
|