Introduction
Knee joint is one of the most vulnerable joints in
the human body. Its ligamentous injury incidence is relatively
high, at 15%. Due to its unique anatomical structure and anatomical
effect, the anterior cruciate ligament (ACL) is extremely
vulnerable to injuries, accounting for approximately 56% of all
knee joint ligaments (1). Femoral
intercondylar notch is an important anatomical structure in the
distal part of femur. ACL injury is closely associated with the
size of the femoral intercondylar notch, considered susceptible to
ACL injury. Therefore, it is critical to investigate the femoral
intercondylar notch (2).
Magnetic mesonance imaging (MRI) has a good soft
tissue imaging ability as well as a high soft tissue resolution and
differentiates various results precisely. Thus it is beneficial in
clinic application (3). In the
present study, we studied the association between ACL rupture and
anatomic morphologic changes of the intercondylar notch and
analyzed the correlation between the course of ACL and knee joint
motor function scoring, thus providing a reference for clinical
treatments of ACL rupture patients.
Materials and methods
General materials
Forty patients with unilateral ACL rupture treated
at the Xuzhou Third Hospital (Jiangsu, China) between July, 2013
and October, 2014, were enrolled in the current study. The patients
were from multiple professions and were confirmed without disease
history on the knee joint. Of the 40 cases, 22 cases were men and
18 were women, aged 20–62 years, with an average of 32.2±2.3 years.
The patients had a disease history of 2–28 months, with an average
of 20.4±1.3 months. Eighteen cases of ACL were identified on the
left knee while 23 cases were on the right knee.
Approval for the present study was obtained from the
Ethics Committee of Xuzhou Third Hospital. Informed consent was
obtained from the patients.
The inclusion criteria for the study were: i)
patients ≥18 years old; ii) patients whose affected knee joints had
different degrees of pain after movement, limited leg extension,
knee joint effusion or knee joint instability as well as other
clinical performances; iii) patients who accepted X-ray and nuclear
MRI (NMRI) examination on the affected side prior to treatment and
had complete materials; iv) patients who had no significant
degenerative changes on the affected knee joint under X-ray
examination; v) patients whose injury conditions on cruciate
ligaments, meniscus and cartilage on articular surface were
confirmed under the detection of laparoscopic surgery and who
accepted corresponding treatments on injury condition. The
exclusion criteria for the study were: i) patients with direct
contact injuries or high-energy violence injuries, such as car
accident and falling accidents; ii) patients with bilateral knee
joint injuries or whose affected knee joint had multiple ligament
injury; iii) patients with uneven density on the intercondylar
notch and articular surface under X-ray examination, with condyle
osteophyte formation on median and lateral femur as well as on
tibial intercondylar eminence or with obvious degeneration of the
knee joint; iv) patients with a past history of knee joint
tuberculosis, suppurative arthritis, rheumatism or rheumatoid
arthritis and other knee joint diseases; v) patients with knee
joint tumor or tumor-like lesion; vi) patients with a past history
of trauma or related operation on the affected knee joint; vii)
patients with severe hepatic renal dysfunction; viii) patients with
poor compliance and patients that declined participation in the
study.
Methods
The 40 patients were diagnosed by 4-limb joint image
diagnostic apparatus produced by Italian Esaote (Genova, Italy)
professional knee joint-phased array surface coil, and the magnetic
field intensity was 0.2 T. The scanning sequence performed were as
follows: coronal plane spin-echo (SE) sequence T2W1, TR2100 ms and
TE90 ms; vertical plane SE sequence T1W1, TE90 ms and TR2100 msl;
cross section GE sequence TE18 ms and TR540 ms, with deflecting
angle of 40°, a layer thickness of 3.5 mm, FOV 170×170 mm,
interlamellar spacing of 0.4 mm. The patients were maintained in a
supine position until the lower patella was located in the central
part of the coil. The knee joints of the patients were bent to 10°
until the border of the intercondylar notch was adjacent to the
anatomic landmark. The trailing edge was the initial image of the
trailing edge joint of the femoral condyle, while the leading edge
was the terminal image of the medial and lateral condyle which
maintained continuity. The trailing edge served as the line of
bilateral condylar joint surface.
Observation indications
The patients were divided into the observation group
(affected side) and the control group (healthy side). MRI
measurements were performed to determine whether on the NMRI
coronal plane SE sequence T2W1 image, the border of the
intercondylar notch was consistent with the anatomic landmark. The
anterior border was the initial clear and continuous image of
medial and lateral condyle. The posterior border was the terminal
clear image of medial and lateral condyle. The lower border was the
line between the lowest points of cartilage surface of the medial
and lateral condyle. The initial image showing continuity in the
medial and lateral condyle and which showed a clear notch shape and
popliteus tendon sulcus of the lateral condyle was considered the
standard. Line I was denoted as the line between the lowest points
of cartilage surface of medial and lateral condyle. A line parallel
to line I on the popliteus tendon sulcus was drawn, and designated
as line II. The distance between line II and the crossing point of
the medial and lateral walls of the femoral intercondylar notch as
intercondylar notch width (ICW) was measured. To determine the
distance between line II and the crossing point of the medial
condyle and lateral condyle of the femur as EW, a line
perpendicular to line I from the highest point of the intercondylar
notch was drawn and the height of this line was determined as
intercondylar notch height (ICH). The ratio of ICW and EW was the
notch as notch width index (NWI), and that of ICW and ICH as the
notch shape index (NSI). Lysholm and Tegner scoring on the affected
knee joints was performed and the differences of the aforementioned
indices were compared. The correlation between ICW and disease
progression as well as knee joint motor function scoring was
analyzed.
Statistical analysis
The SPSS 18.0 software package (SPSS, Inc., Chicago,
IL, USA) was applied to process the data. Measurement data were
presented as means ± standard deviation. The t-test was used to
determine comparisons between groups. Enumeration data were
presented by case or percentage. The χ2 test was used to
determine comparisons between groups. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparisons of ICW, ICH and EW between
the two groups
ICW in the observation group was significantly
smaller than that in the control group and differences were
statistically significant (17.3±2.1 mm vs. 22.5±2.6 mm; P<0.05).
Differences of ICH in the two groups was not statistically
significant (31.3±2.6 mm vs. 30.9±2.5 mm; P>0.05; Table I).
 | Table I.Comparisons of ICW, ICH and EW between
the two groups (mm). |
Table I.
Comparisons of ICW, ICH and EW between
the two groups (mm).
| Groups | ICW | ICH | EW |
|---|
| Observation | 17.3±2.1 | 31.3±2.6 | 77.5±3.8 |
| Control | 22.5±2.6 | 30.9±2.5 | 78.2±3.9 |
| T | 2.843 | 0.701 | 0.813 |
| P-value | 0.037 | 0.483 | 0.416 |
Comparisons of NWI and NSI between the
two groups
NWI and NSI in the observation group were
significantly less than those in the control group. Differences
were statistically significant (NWI: 0.201±0.03 vs. 0.253±0.04,
P<0.05; NSI: 0.521±0.003 vs. 0.564±0.005, P<0.05; Table II).
 | Table II.Comparisons of NWI and NSI between the
two groups. |
Table II.
Comparisons of NWI and NSI between the
two groups.
| Groups | NWI | NSI |
|---|
| Observation | 0.201±0.03 | 0.521±0.003 |
| Control | 0.253±0.04 | 0.564±0.005 |
| T | 2.572 | 2.643 |
| P-value | 0.035 | 0.029 |
Comparisons of knee joint function
scoring
Differences of Lysholm and Tegner scoring between
the two groups were not statistically significant (Lysholm scoring:
32.3±7.4 vs. 34.6±5.2, P>0.05; Tegner scoring: 5.2±1.1 vs.
5.3±1.3, P>0.05; Table
III).
 | Table III.Comparisons of knee joint function
scoring. |
Table III.
Comparisons of knee joint function
scoring.
| Groups | Lysholm scoring | Tegner scoring |
|---|
| Observation | 32.3±7.4 | 5.2±1.1 |
| Control | 34.6±5.2 | 5.3±1.3 |
| T | 0.363 | 0.275 |
| P-value | 0.715 | 0.624 |
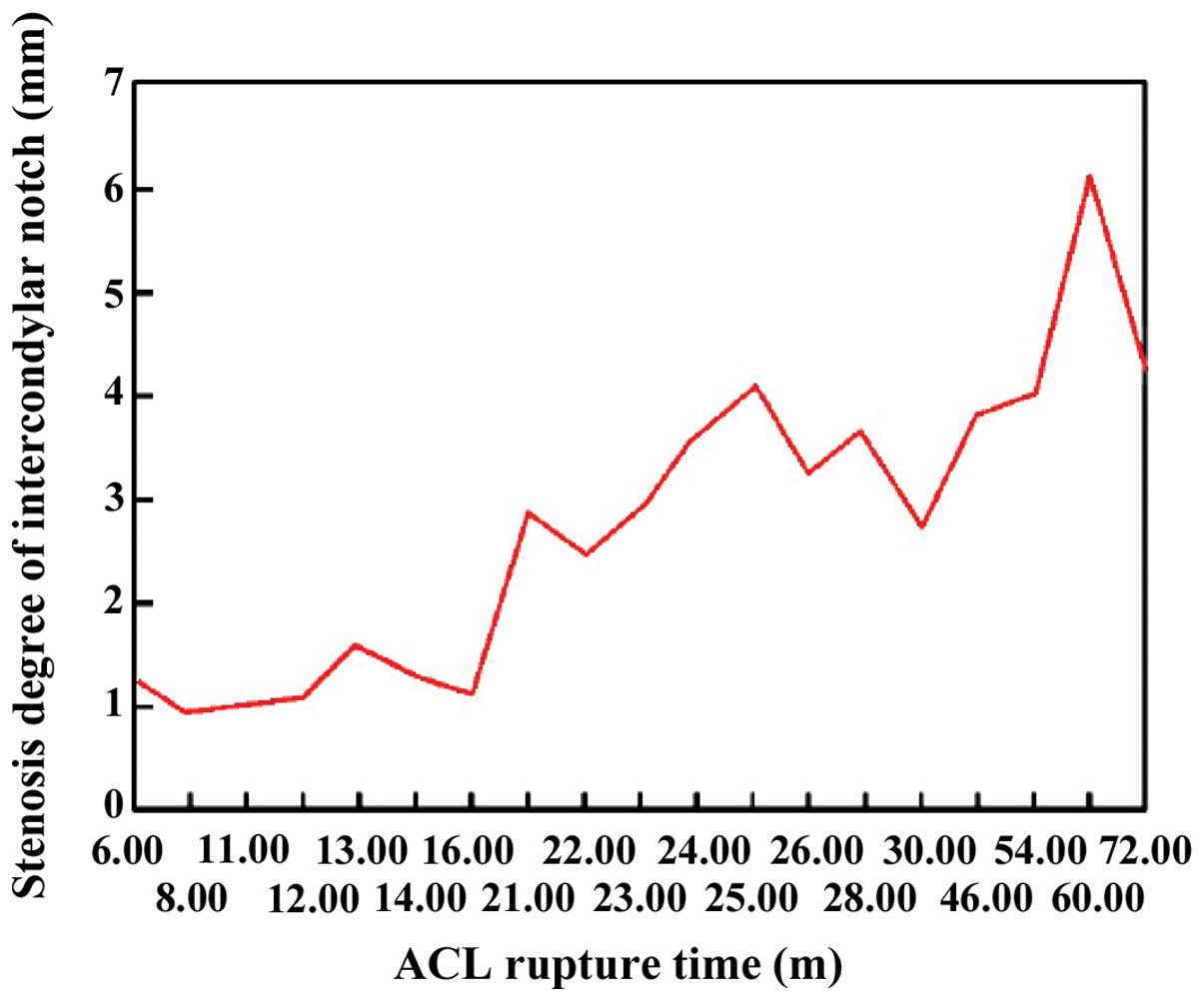
Analysis of the correlation between
ICW and disease progression as well as knee joint motor function
scoring
The differential value of ICW in the observation
group was 2.6±1.3 mm and the ACL rupture time of the affected knee
was 20.4±1.3 months on average. The correlation was statistically
significant (r=0.721, P<0.01; Fig.
1). Correlation of Lysholm scoring, Tegner scoring and
intercondylar notch stenosis degree on the affected knee were not
statistically significant (r=−0.236, P>0.05; r=−0.127,
P>0.05).
Discussion
Attention has been focused on the association
between ACP and intercondylar notch. The size of intercondylar
notch was closely associated with ACP rupture (2). Patients with narrow intercondylar notch
are considered more susceptible to ACP injury. Major factors
resulting in the narrowness of intercondylar notch included joint
degeneration, congenital malformation, long-term instability of the
knee joint and reconstruction failure of the ruptured ACL. The lump
between ACL and femoral intercondylar notch resulted in limited
straightening of the knee joint, pain and other symptoms (4). Therefore, investigation of
intercondylar notch and an analysis of their effects in the
treatment of patients with ACL rupture is crucial. MRI is commonly
used in the detection of orthopedic trauma and soft tissue lesions.
Different sequences of MRI have different application values in
varying tissue signals and quantitatively detect relevant
anatomical structures (5).
The results of the present study have shown that ICW
in the observation group was significantly smaller than that in the
control group and differences were statistically significant.
Differences of ICH and EW between the two groups were not
statistically significant. NWI and NSI in the observation group
were significantly less than those in the control group and
differences were statistically significant. By contrast,
differences of the Lysholm and Tegner scoring between the two
groups were not statistically significant. Additionally, the
differential value of ICW in the observation group and ACL rupture
time of the affected knee was positively correlated. By contrast,
the correlation between Lysholm scoring, Tegner scoring, and
intercondylar notch stenosis degree on the affected knee was not
statistically significant. NSI served as the ratio between ICW and
ICH. The greater the ratio, the more rounded the intercondylar
notch. While extending their knee joints, ACL on patients with a
relatively low ratio would become tight and most of the ligaments
would be in the anterior part of intercondylar notch. Thus, the
narrow intercondylar notch did not provide sufficient space,
resulting in dysfunctions of ACL (6). The greater the NSI, the more likely the
intercondylar notch was able to provide sufficient space for ACL,
when the patients extended their knee joints.
The abovementioned results have confirmed the
association between intercondylar notch stenosis and ACL rupture
and that intercondylar notch stenosis was one of the key factors
resulting in ACL rupture. These results are consistent with those
of previous reports (7). However,
the literature seldom mentions the association between ICH and ACL
rupture. A possible reason is that the measurement criteria of ICH
were uncertain, and due to the measurement having a certain degree
of difficulty, exact data could not be obtained (8). The results of the present study have
shown that differences of ICH and EW between the two groups were
not statistically significant. By contrast, the differences of ICW
between the two groups were statistically significant, indicating
that ICW was important to ACL rupture. Additionally, the shape and
width of the femoral intercondylar notch were important factors
that affect ACL rupture.
Direct indications of ACL rupture under MRI
examination included (9): ACL
disappearance or shrinking, discontinuity, abnormal contour, edema
and thickening. Indirect indications of ACL rupture included
lateral and posterior tibia contusion, femur lateral condyle
contusion, kissing bone contusion, lateral meniscus posterior horn
exposure, anterior disc displacement of tibia, PCL curvature,
posterior PCL line and patellar tendon tortuosity, decrescent angle
between ACL and tibial plateau, Segond fracture, trigonum effusion
and medial collateral ligament injury (10). Use of MRI in the diagnosis of
complete ACL rupture is common with the sensibility and specificity
of MRI in diagnosing ACL rupture reaching 89 and 84%, respectively
(11). However, there was still a
certain degree of false-positive and -negative results. Common
reasons for false-positive results included hypertrophic synovium
in intercondylar notch, scar healing degeneration of ACL,
structural artifacts on tissues and organs between joint capsule
and ACL, including tendon, synovial membrane, fat and blood vessel.
Common reasons for false-negative results included the separation
of integrated end of ligament under incomplete ACL fracture,
formation of edema and scar under long-term injury and
disappearance of localized high signal (12,13).
Therefore, MRI examination prior to arthroscopic surgery is crucial
as it may effectively reduce or avoid the implementation of
arthroscopic surgery. MRI showed images on sagittal, coronal and
transverse sections and does not result in artifacts. In addition,
there was no need to use any contrast agents, thus preventing any
adverse effects on the body. MRI had a relatively higher display
rate of injuries on joint, tendon and ligament in the
musculoskeletal system (14,15). In the present study, all 40 patients
accepted MRI examination and obtained clear images as well as exact
parameters associated with the intercondylar notch.
In conclusion, following ACL rupture, ICW on the
affected knee indicated significant stenosis. NSI and NWI were
significantly reduced and the stenosis degree was further
aggravated with disease progression. No correlation was found for
Lysholm and Tegner scoring of patients with different degrees of
stenosis. However, additional studies should be conducted using
larger samples for the results to be confirmed.
References
|
1
|
Hunter DJ, Niu J, Zhang Y, Totterman S,
Tamez J, Dabrowski C, Davies R, Le Graverand MP, Luchi M,
Tymofyeyev Y and Beals CR: OAI Investigators: Change in cartilage
morphomerty: a sample of the progression cohort of the
Osteoarthritis Initiative. Ann Rheum Dis. 68:349–356. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cha JH, Lee SH, Shin MJ, Choi BK and Bin
SI: Relationship between mucoid hypertrophy of the anterior
cruciate ligament (ACL) and morphologic change of the intercondylar
notch: MRI and arthroscopy correlation. Skeletal Radiol.
37:821–826. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Clayton RA and Court-Brown CM: The
epidemiology of musculoskeletal tendinous ligamentous injuries.
Injury. 39:1338–1344. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Boden BP, Torg JS, Knowles SB and Hewett
TE: Video analysis of anterior cruciate ligament injury:
abnormalities of hip and ankle kinematics. Am J Sports Med.
37:252–259. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Amin S, Guermazi A, Lavalley MP, Niu J,
Clancy M, Hunter DJ, Grigoryan M and Felson DT: Complete anterior
cruciate ligament tear and the risk for cartilage loss and
progression of symptoms in men and women with knee osteoarthritis.
Osteoarthritis Cartilage. 16:897–902. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Podraza JT and White SC: Effect of knee
flexion angle on ground reaction forces, knee moments and muscle
co-contraction during an impact-like deceleration landing:
implications for the non-contact mechanism of ACL injury. Knee.
17:291–295. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mizuno KI, Andrish JT, van den Bogert AJ
and McLean SG: Gender dimorphic ACL strain in response to combined
dynamic 3D knee joint loading: implications for ACL injury risk.
Knee. 16:432–440. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Boden BP, Sheehan FT, Torg JS and Hewett
TE: Noncontact anterior cruciate ligament injuries: mechanisms and
risk factors. J Am Acad Orthop Surg. 18:520–527. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nagano Y, Ida H, Akai M and Fukubayashi T:
Biomechanical characteristics of the knee joint in female athletes
during tasks associated with anterior cruciate ligament injury.
Knee. 16:153–158. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shimokochi Y and Shultz SJ: Mechanisms of
noncontact anterior cruciate ligament injury. J Athl Train.
43:396–408. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Simon RA, Everhart JS, Nagaraja HN and
Chaudhari AM: A case-control study of anterior cruciate ligament
volume, tibial plateau slopes and intercondylar notch dimensions in
ACL-injured knees. J Biomech. 43:1702–1707. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Stein V, Li L, Guermazi A, Zhang Y, Kwoh
Kent C, Eaton CB and Hunter DJ: OAI Investigators: The relation of
femoral notch stenosis to ACl tears in persons with knee
osteoarthritis. Osteoarthritis Cartilage. 18:192–199. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gianotti SM, Marshall SW, Hume PA and Bunt
L: Incidence of anterior cruciate ligament injury and other knee
ligament injuries: a national population-based study. J Sci Med
Sport. 12:622–627. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Alentorn-Geli E, Myer GD, Silvers HJ,
Samitier G, Romero D, Lázaro-Haro C and Cugat R: Prevention of
non-contact anterior cruciate ligament injuries in soccer players.
Part 1: Mechanisms of injury and underlying risk factors. Knee Surg
Sports Traumatol Arthrosc. 17:705–729. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ekstrand J, Hägglund M and Waldén M:
Injury incidence and injury patterns in professional football: the
UEFA injury study. Br J Sports Med. 45:553–558. 2011. View Article : Google Scholar : PubMed/NCBI
|