Introduction
Digital subtraction angiography (DSA) allows the
degree of patency or stenosis of blood vessels to be rapidly
quantified and is now a routine clinical imaging modality; DSA of
the coronary artery is one of its main applications (1). Delayed enhancement magnetic resonance
imaging (DE-MRI) enables the accurate detection and visualization
of myocardial scar tissue. When compared with single-photon
emission computed tomography (SPECT), DE-MRI has been found to be
more likely to detect small myocardial scars as it has higher
sensitivity (2). DE-MRI has been
reported to be capable of detecting lesions with a mass of ~2 g
while SPECT could only detect those with a mass of ≥10 g (3). These missed small infarcts could
potentially be more dangerous than larger infarcts (4,5).
Although DE-MRI has certain advantages in the
detection of myocardial infarction, particularly for small infarcts
and subendocardial infarcts, its clinical application remains rare.
Therefore, the present study aimed to investigate the correlation
between the transmural extent of infarction in myocardial segments
detected by DE-MRI and the degree of coronary artery stenosis
detected by DSA.
Materials and methods
Patients
This prospective study involved 40 patients with a
history of coronary artery disease (CAD) and with myocardial
infarction segments determined by DE-MRI. The study group included
32 men and 8 women, whose ages ranged from 26 to 72 years (mean,
53.3±11.6 years). Patients were recruited from the Second
Affiliated Hospital of Kunming Medical University (Kunming, China),
between June 2009 and November 2013. The study was approved by the
ethics committee of rhe Second Affiliated Hospital of Kunming
Medical University and written informed consent was obtained from
each patient or their guardians
DE-MRI and coronary DSA
MRI investigations were performed using a 1.5T
scanner (Siemens Sonata; Siemens AG, Munich, Germany). Imaging
parameters were as follows: repetition time (msec)/echo time
(msec)/inversion time (msec), 700/4.18/250-300; matrix, 256×64;
flip angle, 25°; inversion pulse, section thickness, 6 mm; field of
view, 280×75 mm; bandwidth, 130 Hz.
Images were obtained in the following orientations:
4-chamber, 2-chamber-long axis and a short axis stack covering the
entirety of the left ventricle from the base to the apex.
Gadolinium-diethylenetriamine pentaacetic acid (Guangdong Consun
Pharmaceutical Group, Guangzhou, China) was injected twice, with a
total dose of 0.2 mmol/kg administered intravenously. Following a
5–30 min delay, images were obtained under breath-holding
conditions. Coronary angiography was performed with an Axiom Artis
dTA angiography system (Siemens AG).
Image analysis
On the images obtained by DE-MRI, the left ventricle
was divided into 17 segments according to the American Heart
Association standards (6). The
transmural extent of myocardial infarction in each segment was
graded from 0 to IV: 0, normal; I, <25% transmural extent,
scored 1; II, 26–50%, scored 2; III, 51–75%, scored 3; IV, 76–100%,
scored 4. These tests were carried out by two radiologists using a
blinding method.
DSA coronary artery analysis
The Gensini scoring system that was used has been
described and validated previously (7). The severity of coronary artery stenosis
was given a total score of between 1 and 32, as follows: <25%,
scored 1; 26–50%, scored 2; 51–75%, scored 4; 76–90%, scored 8;
91–99%, scored 16; 100%, scored 32. All scores were confirmed
together by one senior interventional cardiologist and one
interventional radiologist.
Statistical analysis
Statistical analysis was performed using SPSS
software, version 13.0 (SPSS, Inc., Chicago, IL, USA). Correlation
between coronary artery Gensini scores and myocardial infarction
segmental scores was analyzed by Spearman's rank correlation
analysis. The Kendall rank correlation method was used to analyze
the correlation between the extent of coronary artery stenosis as
determined by DSA and the transmural extent of myocardial
infarction.
Results
DSA coronary angiography
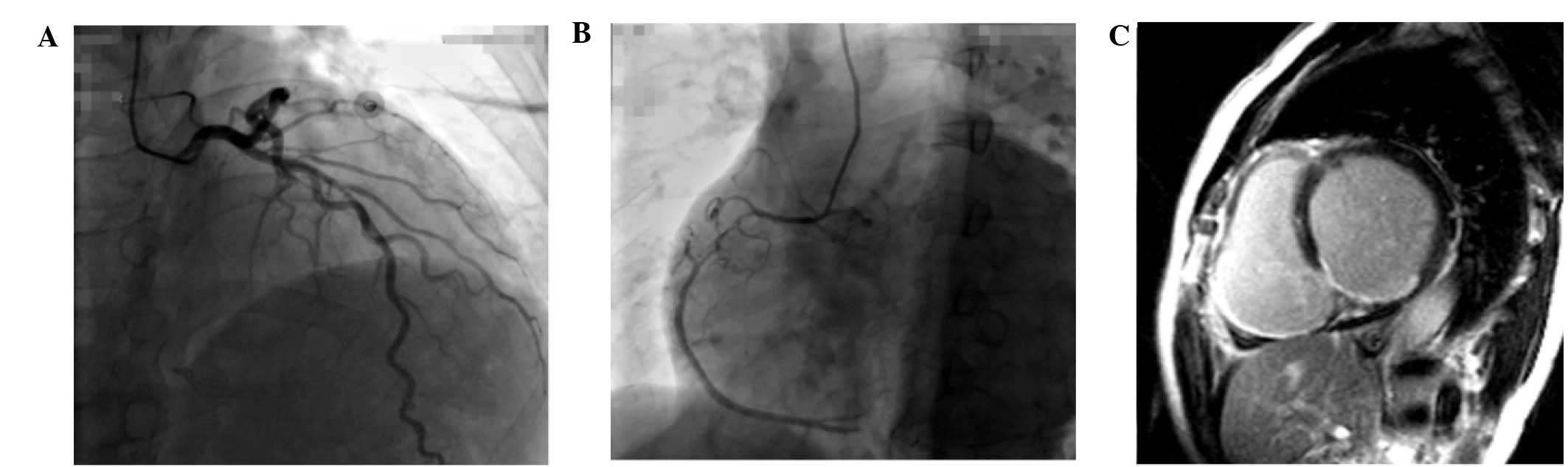
Analysis of the DSA coronary angiography images
indicated that there were 37 cases of coronary artery stenosis
among the 40 patients: There was single-vessel disease in 12 cases,
double-vessel disease in 10 cases, and triple or more-vessel
disease in 15 cases. In total, 87 vessels containing angiostenosis
were identified and 3 cases showed no signs of abnormality. DSA
images from a patient with coronary artery stenosis are shown in
Fig. 1A and B, and from a patient
with no signs of stenosis are shown in Fig. 2A and B.
DE-MRI detection
The DE-MRI results revealed 126 segments with
myocardial infarction and delayed enhancement in the 40 cases
(Figs. 1C and 2C). Among these segments, the percentages
of grade I, II, III and IV were 31.75% (n=40), 19.05% (n=24),
22.22% (n=28) and 26.98% (n=34).
Correlation analysis between coronary
Gensini score and segmental myocardial infarction detected by
DE-MRI
The total coronary Gensini score was 587, while the
total DE-MRI score was 308. For the Spearman's rank correlation,
the correlation coefficient, rs=0.786 (P<0.001),
indicating a good correlation between DE-MRI-detected myocardial
infarction and the extent of coronary artery stenosis. The Kendall
rank correlation coefficient was 0.405 (P<0.001).
Table I shows the
extent of coronary artery stenosis as determined by DSA and the
transmural extent of myocardial infarction in each segment as
detected by DE-MRI.
 | Table I.Extent of coronary artery stenosis and
segments with myocardial infarction of different transmural extents
detected by DE-MRI. |
Table I.
Extent of coronary artery stenosis and
segments with myocardial infarction of different transmural extents
detected by DE-MRI.
|
| Transmural extent of
myocardial infarction |
|---|
|
|
|
|---|
| Extent of coronary
artery stenosis (%) | I | II | III | IV | Overall |
|---|
| ≤25 | 9 | 4 | 6 | 4 | 23 |
| ≤50 | 19 | 2 | 0 | 2 | 23 |
| ≤75 | 4 | 2 | 2 | 2 | 10 |
| ≤90 | 6 | 12 | 10 | 4 | 32 |
| ≤99 | 2 | 0 | 6 | 10 | 18 |
| ≤100 | 0 | 4 | 4 | 12 | 20 |
| Overall | 40 | 24 | 28 | 34 | 126 |
Discussion
DSA is the gold standard for the imaging of coronary
arteries. However, in the clinic, knowing only the extent of
coronary stenosis is insufficient to assess the coronary arteries.
Patients with coronary artery disease and myocardial infarction can
exhibit myocardium with a variety of functional states including
stunned, hibernating and nonviable (8). The first two states are reversible
damage, and the myocardium is viable, while the last state is
irreversible. The identification of viable myocardium is important
for the guidance of treatment and the judgment of prognosis.
Clinical studies have shown an excellent correspondence between
infarction as revealed by DE-MRI and histopathology (9–12).
Therefore, the ability of DE-MRI to accurate identify the viable
myocardium suggests its potential as a diagnostic procedure to be
combined with DSA.
In the 40 patients involved in the present study,
the Spearman's rank correlation coefficient between DSA coronary
artery Gensini score and DE-MRI myocardial infarction score was
0.786 (P<0.001), indicating a positive correlation between
coronary stenosis and myocardial infarction. A higher transmural
extent of myocardial infarction was found to correlate with more
severe stenosis of the coronary artery (Table I). Furthermore, 81.74% of the
segments with myocardial infarction were located in areas of
vascular blood flow with a degree of coronary artery stenosis of
≥50%. Among the segments in which the transmural extent of
myocardial infarction was >75%, and 64.71% of the segments were
present in areas of blood supply that had >90% coronary
stenosis.
The identification of segments and sites affected by
myocardial infarction, and the transmural extent of myocardial
infarction by DE-MRI can be used to supplement examination of
coronary arteries by DSA, and may guide the treatment and prognosis
of patients. A study of chronic myocardial recovery capability
found that blood supply reconstruction is inversely proportional to
the transmural extent of myocardial infarction; in segments with
>50% transmural extent of infarction, the cardiac function was
unlikely to be completely recovered (13). Therefore, the assessment of the
transmural extent of myocardial infarction in myocardial segments
by DE-MRI is a potential option in clinical diagnosis.
Echocardiography and SPECT are two of the commonly
used tools to clinically evaluate myocardial activity. However, due
to their limited spatial resolution, these tools only provide an
‘all’ or ‘nothing’ result for myocardial activity (14). Notably, even in a single myocardial
segment, there may be both viable and unviable parts, for example,
the outer membrane of an endocardium with myocardial infarction may
be viable. Therefore, the transmural extent of myocardial
infarction should be considered segmentally, rather than the
activity of a myocardial segment being judged by the concept of
‘all’ or ‘nothing’ (15,16). Therefore, analysis of the extent of
coronary artery stenosis together with analysis of the transmural
extent of myocardial infarction by DE-MRI should benefit both the
clinical treatment and prognosis of patients.
The present study showed only a subtle correlation
(τ=0.405, P<0.001) between the extent of coronary artery
stenosis and Kendall rank of the transmural extent of myocardial
infarction. It was found that 46 of the segments with myocardial
infarction occurred in areas of vascular distribution that
exhibited <50% coronary artery stenosis. Stenosis <50% is
unlikely to result in myocardial ischemia due to a compensatory
effect in which the resistance of the coronary small vasculature is
reduced (17). Therefore, >50%
coronary artery stenosis can be considered as clinically
significant for lesions. However, acute coronary syndrome may
potentially occur due to plaque rapture in stenosis sites showing
<50% coronary artery stenosis. In the present study, 18.25%
(23/126) of segments with myocardial infarction were observed in
patients without significant coronary artery stenosis (<25%
stenosis). In addition to plaque rupture and fall off, severe
stenosis in coronary spasm may also result in irreversible
myocardial damage (18).
Myocardial scarring was found in patients whose
coronary artery showed no significant stenosis in a previous study
that analyzed the correlation between the severity of coronary
artery lesions and DE-MRI results by Bexell et al (19). In addition, the majority of the
infarcts were generally subendocardial (with <25% transmural
extent). The results of the present study were consistent with
these data. It was found that 60.87% of the segments with
myocardial infarction showed a transmural extent <25% in a
coronary artery blood-supplying area in which the extent of
coronary stenosis was <50%. Misdiagnosis may potentially occur
if SPECT or positron emission tomography (PET) is used as a
diagnosis tool. In a previous study, only 28% of the segments
affected by myocardial infarction were detected by PET compared
with 92% by DE-MRI; this may have been because small areas of
scarring could only be detected by DE-MRI (2). Another study with 31 cases of severe
heart failure found that 55% of subendocardial infarction was
missed by PET (20). The mortality
rate for individuals with undiagnosed myocardial infarction is
significantly higher than that for diagnosed myocardial infarction
(4). DE-MRI exhibits clear
advantages in subendocardial myocardial infarction and small
infarcts (21,22).
No evident stenosis was observed by coronary artery
DSA in 3 patients. Two of these cases were inferior infarction,
mainly subendocardial, with 25–50% transmural extent (as shown for
one patient in Fig. 2). At present,
the incidence of coronary artery disease is exhibiting a trend
towards younger patients. The patients with no evident stenosis
included 2 patients younger than 30 years old, and one was a
26-year-old female patient. This patient was first diagnosed with
inferior wall infarct by DE-MRI, and then right coronary artery
stenosis was identified with an extent of 90% by DSA. Therefore,
DE-MRI is helpful in determining the causes of myocardial damage,
which are of great significance to prognosis and intervention. A
previous study showed a correlation between DE-MRI-detected
myocardial infarction and short- or long- term adverse cardiac
events, which is also helpful for the evaluation of prognosis
(23).
In conclusion, DSA evaluation and DE-MRI may
complement each other advantageously, and should not only be
helpful for the identification of transmural extent in the viable
or irreversible myocardium, but also for the elimination of
misdiagnosis.
Acknowledgements
This study was supported by the National Science
Foundation of China (grant no. 81260213), the National Science
Foundation of Yunnan Province (grant no. 2012FB054) and Key
Projects of Science Research of the Department of Education in
Yunnan Province (grant no. 2015HB068).
References
|
1
|
Struyven JJ, Delcour C, Brion JP,
Vandenbosch G and Claessens J: Digital subtraction angiography
(DSA) of the heart and coronary arteries. Ann Radiol (Paris).
29:107–111. 1986.PubMed/NCBI
|
|
2
|
Ibrahim T, Bulow HP, Hackl T, Hörnke M,
Nekolla SG, Breuer M, Schömig A and Schwaiger M: Diagnostic value
of contrast-enhanced magnetic resonance imaging and single-photon
emission computed tomography for detection of myocardial necrosis
early after acute myocardial infarction. J Am Coll Cardiol.
49:208–216. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Larose E: Below radar: Contributions of
cardiac magnetic resonance to the understanding of myonecrosis
after percutaneous coronary intervention. Circulation. 114:620–622.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schelbert EB, Cao JJ, Sigurdsson S,
Aspelund T, Kellman P, Aletras AH, Dyke CK, Thorgeirsson G,
Eiriksdottir G, Launer LJ, et al: Prevalence and prognosis of
unrecognized myocardial infarction determined by cardiac magnetic
resonance in older adults. JAMA. 308:890–896. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
McManus DD, Chinali M, Saczynski JS, Gore
JM, Yarzebski J, Spencer FA, Lessard D and Goldberg RJ: 30-year
trends in heart failure in patients hospitalized with acute
myocardial infarction. Am J Cardiol. 107:353–359. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cerqueira MD, Weissman NJ, Dilsizian V,
Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T and
Verani MS: American Heart Association Writing Group on Myocardial
Segmentation and Registration for Cardiac Imaging: Standardized
myocardial segmentation and nomenclature for tomographic imaging of
the heart. A statement for healthcare professionals from the
Cardiac Imaging Committee of the Council on Clinical Cardiology of
the American Heart Association. Circulation. 105:539–542. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gensini GG, Kelly AE, Da Costa BC and
Huntington PP: Quantitative angiography: The measurement of
coronary vasomobility in the intact animal and man. Chest.
60:522–530. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Okada DR, Liu Z, Johnson G III, Beju D,
Khaw BA and Okada RD: 99mTc-glucarate kinetics differentiate
normal, stunned, hibernating and nonviable myocardium in a perfused
rat heart model. Eur J Nucl Med Mol Imaging. 37:1909–1917. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ingkanisorn WP, Rhoads KL, Aletras AH,
Kellman P and Arai AE: Gadolinium delayed enhancement
cardiovascular magnetic resonance correlates with clinical measures
of myocardial infarction. J Am Coll Cardiol. 43:2253–2259. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Choi KM, Kim RJ, Gubernikoff G, Vargas JD,
Parker M and Judd RM: Transmural extent of acute myocardial
infarction predicts long-term improvement in contractile function.
Circulation. 104:1101–1107. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu E, Judd RM, Vargas JD, Klocke FJ, Bonow
RO and Kim RJ: Visualisation of presence, location and transmural
extent of healed Q-wave and non-Q-wave myocardial infarction.
Lancet. 357:21–28. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang J, Ma H, Liu J, Wang C, Shi Y, Xie H,
Huo F, Liu F and Lin K: Delayed-enhancement magnetic resonance
imaging at 3.0T using 0.15 mmol/kg of contrast agent for the
assessment of chronic myocardial infarction. Eur J Radiol.
83:778–782. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim RJ, Wu E, Rafael A, Chen EL, Parker
MA, Simonetti O, Klocke FJ, Bonow RO and Judd RM: The use of
contrast-enhanced magnetic resonance imaging to identify reversible
myocardial dysfunction. N Engl J Med. 343:1445–1453. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Baumgartner H, Porenta G, Lau YK, Wutte M,
Klaar U, Mehrabi M, Siegel RJ, Czernin J, Laufer G, Sochor H, et
al: Assessment of myocardial viability by dobutamine
echocardiography, positron emission tomography and thallium-201
SPECT: Correlation with histopathology in explanted hearts. J Am
Coll Cardiol. 32:1701–1708. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Prati F, Pawlowski T, Gil R, Labellarte A,
Gziut A, Caradonna E, Manzoli A, Pappalardo A, Burzotta F and
Boccanelli A: Stenting of culprit lesions in unstable angina leads
to a marked reduction in plaque burden: A major role of plaque
embolization? A serial intravascular ultrasound study. Circulation.
107:2320–2325. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ricciardi MJ, Wu E, Davidson CJ, Choi KM,
Klocke FJ, Bonow RO, Judd RM and Kim RJ: Visualization of discrete
microinfarction after percutaneous coronary intervention associated
with mild creatine kinase-MB elevation. Circulation. 103:2780–2783.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kuncheng L: China Medical Imagine
(cardiovascular system volume). People's Health Publishing House;
Beijing: pp. 882007
|
|
18
|
Maseri A, L'Abbate A, Baroldi G, Chierchia
S, Marzilli M, Ballestra AM, Severi S, Parodi O, Biagini A,
Distante A and Pesola A: Coronary vasospasm as a possible cause of
myocardial infarction. A conclusion derived from the study of
“preinfarction” angina. N Engl J Med. 299:1271–1277. 1978.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bexell D, Setser RM, Schoenhagen P, Lieber
ML, Brener SJ, Ivanc TB, Balazs EM, O'Donnell TP, Stillman AE,
Arheden H, et al: Influence of coronary artery stenosis severity
and coronary collateralization on extent of chronic myocardial
scar: Insights from quantitative coronary angiography and
delayed-enhancement MRI. Open Cardiovasc Med J. 2:79–86. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Barbier CE, Bjerner T, Johansson L, Lind L
and Ahlstrom H: Myocardial scars more frequent than expected:
Magnetic resonance imaging detects potential risk group. J Am Coll
Cardiol. 48:765–771. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wagner A, Mahrholdt H, Holly TA, Elliott
MD, Regenfus M, Parker M, Klocke FJ, Bonow RO, Kim RJ and Judd RM:
Contrast-enhanced MRI and routine single photon emission computed
tomography (SPECT) perfusion imaging for detection of
subendocardial myocardial infarcts: An imaging study. Lancet.
361:374–379. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu YW, Tadamura E, Yamamuro M, Kanao S,
Marui A, Tanabara K, Komeda M and Togashi K: Comparison of
contrast-enhanced MRI with 18F-FDG PET/201Tl SPECT in
dysfunctional myocardium: Relation to early functional outcome
after surgical revascularization in chronic ischemic heart disease.
J Nucl Med. 48:1096–1103. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kwong RY, Sattar H, Wu H, Vorobiof G,
Gandla V, Steel K, Siu S and Brown KA: Incidence and prognostic
implication of unrecognized myocardial scar characterized by
cardiac magnetic resonance in diabetic patients without clinical
evidence of myocardial infarction. Circulation. 118:1011–1020.
2008. View Article : Google Scholar : PubMed/NCBI
|