Introduction
Oral lichen planus (OLP) is a chronic inflammatory
disease that affects oral mucosa of squamous cell origin (1), and is most commonly observed in middle
aged women (2). The etiopathogenesis
of OLP has yet to be elucidated. However, it is known to be
associated with multiple factors and their immunological,
endocrine, infective and psychological etiologies have been
suggested in previous studies (3,4). In
recent years, the involvement of genetic factors in OLP has
attracted increased attention.
OLP may occur in the buccal mucosa, tongue, gingiva,
lip and palate, it may present in papular, reticular, plaque-like,
atrophic, bullous and erosive forms (3–5), and
frequently appears as a mixture of the forms (6). The lesions are typically multiple,
symmetrical, bilateral and painless. However, erosive and atrophic
lesions may cause pain or a burning sensation, and are considered
to be premalignant (5).
OLP is one of the most common diseases of the oral
mucosa, with a prevalence of 1–2% (3,5,7–9).
Typically, it presents sporadically, so familial OLP is rare. The
current study reports cases of familial OLP in eight different
Chinese families and analyzes their clinical characteristics.
The present study supports the notion that genetic
predisposition may be important in OLP, and it also reminds us that
OLP patient's relatives should be advised to perform check-ups in
time in order to exclude or confirm OLP. Furthermore, the present
study also provides samples for large-scale genetic studies of OLP
in the future.
Subjects and methods
Ethics statement
The present study was approved by the Institutional
Ethics Committee of Qingdao Municipal Hospital (Qingdao, China).
Informed consent was obtained from one of the patients.
Subjects and inclusion criteria
A retrospective review was performed on eight
families of individuals affected by familial OLP who were diagnosed
between January 1, 2012 and December 31, 2013 at the Oral Medical
Center of Qingdao Municipal Hospital. A diagnosis of familial OLP
was concluded if the patient met the following criteria: i) The
diagnosis of OLP was supported by clinical and pathological
findings; and ii) at least two members of the patient's family had
OLP.
Diagnosis criteria
The criteria for the diagnosis of OLP has been
established by World Health Organization (10). Clinically, OLP frequently presents as
multiple lesions with white striations that typically occur in the
buccal mucosa, tongue and gingiva. The lesions may become erosive
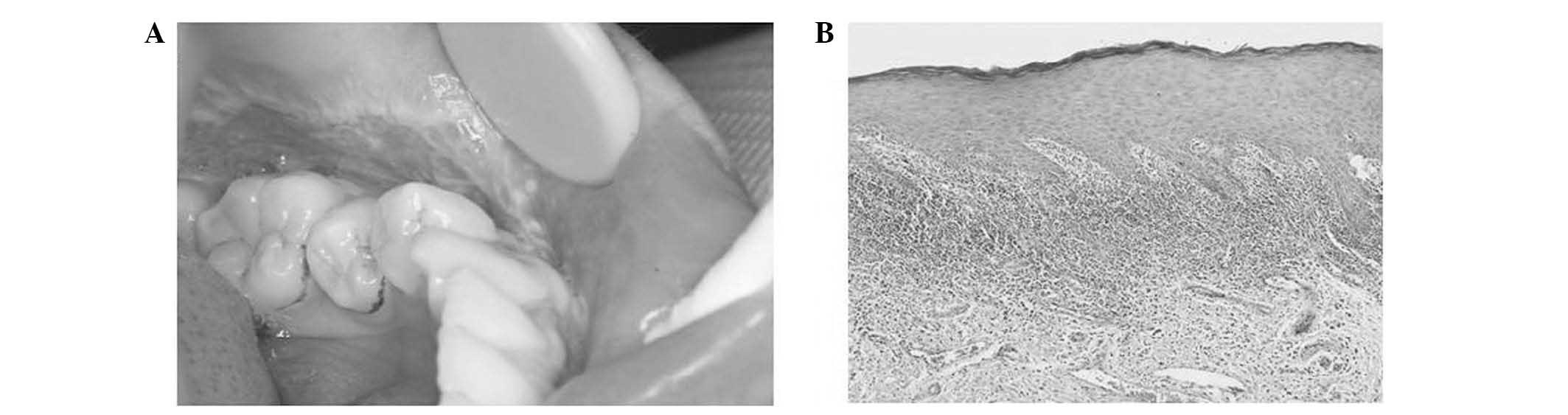
or atrophic, or may present in other clinical patterns (8). Histologically, OLP is characterized by
a dense band-like lymphocytic infiltrate in the immediate
sub-epithelial region with basal epithelial cell destruction
(6). In the present study, the
clinical and histological diagnosis was made by the same oral
medicine doctor and the same pathology doctor, respectively.
Histological examination
In total, ~0.5 mm × 0.5 mm of mucosa with OLP lesion
was incised under local anesthesia. The sample was fixed in 10%
formalin for 24 h, paraffin-embedded and sectioned into 4-µm
slices. Furthermore, it was dewaxed by gradient alcohol, rinsed
with H2O, dyed by hematoxylin and eosin, dehydrated by
gradient alcohol, hyalinized by xylene, sealed by neutral gum and
observed using a BX51 microscope (Olympus Corporation, Tokyo
Japan).
Each individual that met the diagnosis criteria of
familial OLP was surveyed and recorded. For each patient, the
gender, age at diagnosis, lesion distribution and lesion type were
recorded and analyzed, and the follow-up was a minimum of 1
year.
Results
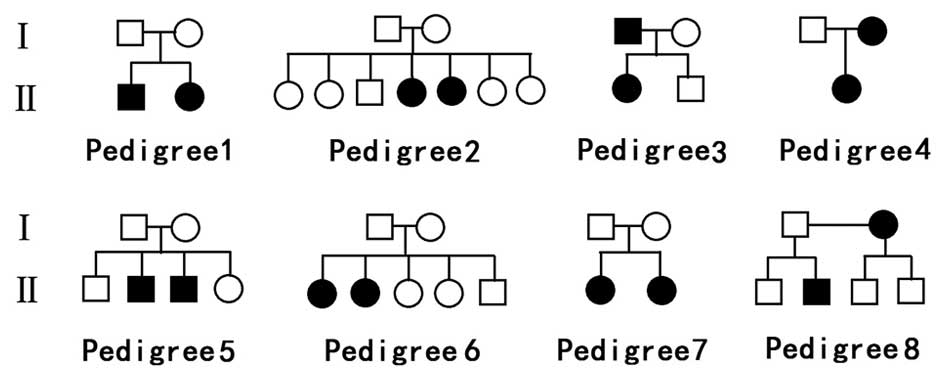
Genetic predisposition. The pedigrees of the eight
families are shown in Fig. 1. Six
families had two affected members and two families had three
affected members among the three generations. Fig 1 supports the hypothesis that OLP has a
genetic predisposition.
Among the 88 family members, 18 individuals were
affected (female, n=13; male, n=5), and the female to male ratio
was 2.6:1, which was higher compared with nonfamilial OLP (1.4:1)
(6).
Clinical characteristics. The clinical
characteristics of the individuals with OLP from the eight families
are presented in Table I. Patients
age at diagnosis ranged between 25 and 70 years old, and the
majority of the patients were aged between 40 and 49 years.
 | Table I.Clinical features of 18 individuals
from eight different families (I–VIII) with familial oral lichen
planus. |
Table I.
Clinical features of 18 individuals
from eight different families (I–VIII) with familial oral lichen
planus.
| Number |
|
| Lesion
distribution |
|
|---|
|
|
|
|
|
|---|
| Patient | Family | Gender | Age at diagnosis | B | G | T | L | P | Lesion type |
|---|
| 1 | I | M | 60 | + |
| + |
|
| R, E, PL, A |
| 2 | I | F | 58 | + |
|
|
|
| R |
| 3 | II | F | 49 | + |
| + |
|
| R, PL |
| 4 | II | F | 47 | + |
|
|
|
| PA |
| 5 | III | M | 48 | + |
|
|
|
| R, E, A |
| 6 | III | F | 25 | + |
|
|
|
| R |
| 7 | IV | F | 70 | + |
| + |
|
| R, E, A |
| 8 | IV | F | 62 | + |
|
|
|
| R, E |
| 9 | IV | F | 38 | + | + |
|
| + | R, E |
| 10 | V | M | 48 | + | + | + |
| + | R, E |
| 11 | V | M | 46 | + |
|
|
|
| R |
| 12 | VI | F | 31 | + |
|
|
|
| R |
| 13 | VI | F | 30 |
|
| + | + |
| PL, R |
| 14 | VII | F | 58 |
|
|
| + |
| R, E |
| 15 | VII | F | 53 | + |
|
|
|
| R |
| 16 | VIII | F | 62 | + | + | + |
|
| R, E, A |
| 17 | VIII | F | 44 | + |
|
|
|
| R, E |
| 18 | VIII | M | 27 | + |
|
| + |
| R |
With respect to the locations of the lesions, the
buccal mucosa was the most frequently affected site, followed by
the tongue, lip, gingiva and palate, and a number of patients had
lesions at more than one location.
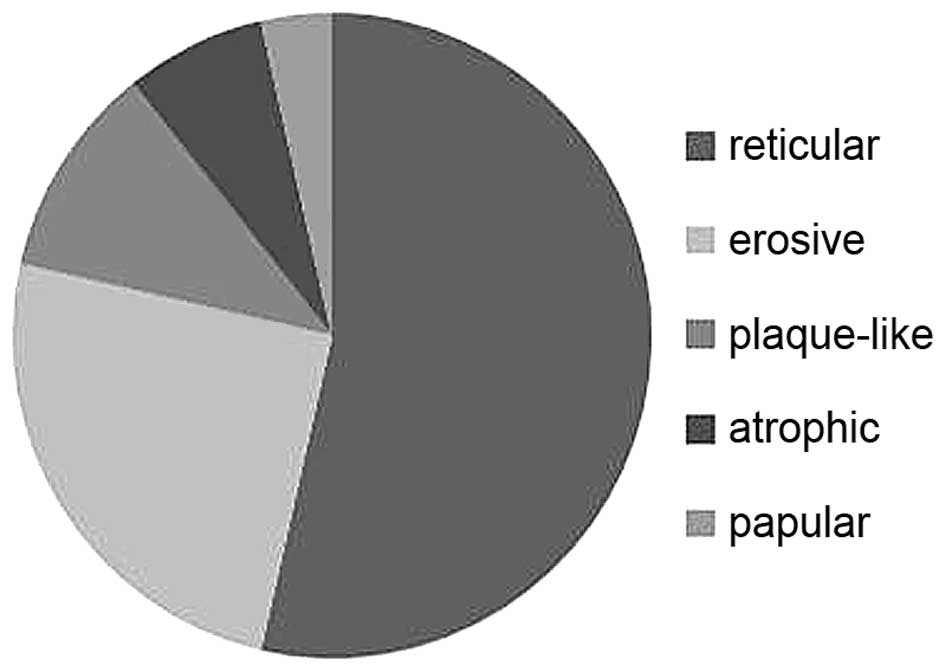
With respect to the lesion types, those with a
reticular pattern accounted for the predominant clinical form of
OLP, followed by erosive lesions, atrophic lesions, plaque-like
lesions and papular lesions (Fig.
2). The majority of patients had multiple lesions, and bullous
lesions were not detected (Table
I).
No malignant/premalignant lesions were identified,
and none of the patients had cutaneous lesions of LP. Other members
of the families were clinically examined, however none showed
mucosal or skin LP lesions, except family VI. This family included
5 children; two of the children had OLP, one had LP cutaneous
lesions on the face and one had LP cutaneous lesions on the
legs.
Discussion
Familial LP is uncommon, and its prevalence in a
large sample study has been reported to be 1.5% (9), whilst familial OLP is even less
common.
Compared with nonfamilial LP, familial LP is
reported to be characterized by its early age of onset, its ability
to become severe and chronic and to have atypical and widespread
clinical presentation (11). In the
present study concerning familial OLP, the clinical and
pathological manifestations (Fig. 3)
and parameters (gender, age at diagnosis, lesion distribution and
lesion type) showed no difference compared with nonfamilial OLP,
except in family VI, in which 4/5 children had OLP/LP lesions and
were of an early age at diagnosis. In addition, it was identified
that patients of the same generation in the same family were of a
similar age at diagnosis.
In the eight families analyzed, once one member of
the family had been initially diagnosed with OLP, other members
were surveyed and further cases were identified. As papular,
reticular and plaque-like lesions are typically asymptomatic,
family members of individuals with OLP frequently fail to notice
the existence of lesions prior to their clinical confirmation
(6). Thus, the exact time of onset
and duration is unknown to the patient. Consequentially, there is
no record and analysis of the time of onset and duration in this
study.
The etiology of OLP is associated with numerous
factors. Previous studies have suggested that OLP is a T
cell-mediated autoimmune disease (3,12).
Particular tendencies, such as smoking, alcohol consumption, drugs,
eating spicy foods and bad hygiene, may exasperate symptoms of OLP
(3,4,6). In
addition, psychological disorders, such as anxiety, depression and
stress, are associated with OLP (3,6,13). In addition, accidental abrasion of
the oral mucosa by brushing of teeth causing an ulcer, pointed
cusps, cracked teeth or worn dental restorations may worsen or
trigger new lesions (4). Previously,
OLP has been reported to be associated with systemic medical
conditions, such as diabetes, hepatitis C viral infections,
hypertension, ulcerative colitis, myasthenia gravis and lupus
erythematosus (2,3,4,11). Recently, several studies have
revealed the genetic susceptibility of OLP through case control
association testing (14–17).
The role of genetic factors in OLP have yet to be
elucidated. In certain studies, the role of genetic predisposition
was considered. Watanabe et al (18) concluded that human leukocyte antigen
(HLA) served a role in the pathogenesis of OLP. Hedberg and Hunter
(19) reported that epithelium
affected by OLP was consistently positive for HLA-antigen D
related. There are a number of clinical reports describing familial
OLP and genetic predisposition. Wang et al (5) assessed a Chinese family affected with
OLP and identified genetics as the cause for the disease. In
addition, a report of OLP in three successive generations was
highly indicative of a genetic predisposition to the disease
(9). The aforementioned data, in
addition to the current study, suggests that genetic predisposition
serves a role in OLP.
The risk of malignant potential should be considered
in OLP (1), which was classified as
a premalignant condition by the World Health Organization in 1997
(8,12). Currently, however, whether OLP is a
premalignant condition remains controversial. Using stringent
diagnostic criteria, a number of authors have found that patients
with OLP are not at increased risk of oral squamous cell carcinoma.
Accurso et al (20) evaluated
loss of heterozygosity using laser capture microdissection or
microsatellite instability and found that OLP exhibited a genetic
profile that had greater similarity to a benign or reactive process
compared with a premalignant/malignant one. Certain studies have
concluded that several of the reported cases of oral carcinomas
arising from OLP may have developed from lichenoid lesions with
dysplasia (8,18,21–24).
However, there is a consensus supporting the potential for the
malignant transformation of OLP, with a transformation rate from
prospective studies ranging between 0.4 and 6.5%. This is
particularly true in erosive-type OLP, and in OLP occurring in the
lateral and ventral side of the tongue (12,25).
Whether familial OLP is a premalignant condition
remains controversial. Wang et al (5) reported the case of a Chinese family
with OLP affected by a severe form of oral reticular and erosive
lesions, and 2 of the 5 affected individuals had developed oral
cancer at an early age. However, Bermejo-Fenoll and López-Jornet
(11) reported familial OLP in six
families in Spain, none of whom developed oral cancer. The present
report of familial OLP in eight Chinese families was in agreement
with the aforementioned study. However, further investigation with
a larger sample size for patients with familial OLP, and with
longer-term clinical follow-up, is required.
The exact etiology of familial OLP has yet to be
elucidated. The current study supports the notion that genetic
predisposition may serve a role in the disease, and we speculate
that this may be associated with the same family having similar
habits, disposition and pedigree; however, the possibility of
coincidence can not be ignored. Further studies with a larger
sample of the population is essential to investigate genetic
factors to reveal the pathogenesis of this rare condition. Whether
there is a risk of malignant transformation requires longer term
follow-up and further research. Furthermore, when a patient is
diagnosed with OLP, the possibility of canceration should be
considered, and the patients relatives should be advised to undergo
a check-up in time to exclude or confirm presence of the disease,
in order to achieve an early diagnosis and early treatment.
Acknowledgements
The present study was supported by funding from the
National Natural Science Foundation of China (grant no. 81271141)
and Qingdao Municipal Science and Technology Commission Major
Project (grant no. 11-2-3-2-(7)-nsh).
References
|
1
|
Jin X, Wang J, Zhu L, Wang L, Dan H, Zeng
X and Chen Q: Association between −308 G/A polymorphism in TNF-α
gene and lichen planus: A meta-analysis. J Dermatol Sci.
68:127–134. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Srinivas K, Aravinda K, Ratnakar P, Nigam
N and Gupta S: Oral lichen planus-Review on etiopathogenesis. Natl
J Maxillofac Surg. 2:15–16. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Barbosa NG, Silveira ÉJ, Lima EN, Oliveira
PT, Soares MS and de Medeiros AM: Factors associated with clinical
characteristics and symptoms in a case series of oral lichen
planus. Int J Dermatol. 54:e1–e6. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Di Stasio D, Guida A, Salerno C, Contaldo
M, Esposito V, Laino L, Serpico R and Lucchese A: Oral lichen
planus: A narrative review. Front Biosci (Elite Ed). 6:370–376.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang Z, Yao H, Cui B, Ning G and Tang GY:
Genetic linkage analysis of oral lichen planus in a Chinese family.
Genet Mol Res. 10:1427–1433. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sandhu SV, Sandhu JS, Bansal H and Dua V:
Oral lichen planus and stress: An appraisal. Contemp Clin Dent.
5:352–356. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ghapanchi J, Haghshenas MR, Ghaderi H,
Amanpour S, Nemati V and Kamali F: Ctla-4 gene polymorphism in +49
a/g position: A case control study on patients with oral lichen
planus. J Int Oral Health. 6:17–21. 2014.PubMed/NCBI
|
|
8
|
Zhang L, Michelsen C, Cheng X, Zeng T,
Priddy R and Rosin MP: Molecular analysis of oral lichen planus. A
premalignant lesion? Am J Pathol. 151:323–327. 1997.PubMed/NCBI
|
|
9
|
Singal A: Familial mucosal lichen planus
in three successive generations. Int J Dermatol. 44:81–82. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rad M, Hashemipoor MA, Mojtahedi A, Zarei
MR, Chamani G, Kakoei S and Izadi N: Correlation between clinical
and histopathologic diagnoses of oral lichen planus based on
modified WHO diagnostic criteria. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 107:796–800. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bermejo-Fenoll A and López-Jornet P:
Familial oral lichen planus: Presentation of six families. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod. 102:e12–e15. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Al-Nasser L and El-Metwally A: Oral lichen
planus in Arab countries: A review. J Oral Pathol Med. 43:723–727.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gavic L, Cigic L, Lukenda D Biocina,
Gruden V and Pokupec JS Gruden: The role of anxiety, depression,
and psychological stress on the clinical status of recurrent
aphthous stomatitis and oral lichen planus. J Oral Pathol Med.
43:410–417. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Supic G, Kozomara R, Zeljic K,
Stanimirovic D, Magic M, Surbatovic M, Jovic N and Magic Z: HMGB1
genetic polymorphisms in oral squamous cell carcinoma and oral
lichen planus patients. Oral Dis. 21:536–543. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jiang C, Yao H, Cui B, Zhou Y, Wang Y and
Tang G: Association of interleukin 12A gene polymorphisms with oral
lichen planus in Chinese population. J Oral Pathol Med. 44:602–606.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wu D, Chen X, Dong C, Liu Q, Yang Y, He C,
Wang J, Sun M and Wu Y: Association of single nucleotide
polymorphisms in MPO and COX genes with oral lichen planus. Int J
Immunogenet. 42:161–167. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Al-Mohaya MA, Al-Harthi F, Arfin M and
Al-Asmari A: TNF-α, TNF-β and IL-10 gene polymorphism and
association with oral lichen planus risk in Saudi patients. J Appl
Oral Sci. 23:295–301. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Watanabe T, Ohishi M, Tanaka K and Sato H:
Analysis of HLA antigens in Japanese with oral lichen planus. J
Oral Pathol. 15:529–533. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hedberg NM and Hunter N: The expression of
HLA-DR on keratinocytes in oral lichen planus. J Oral Pathol.
16:31–35. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Accurso BT, Warner BM, Knobloch TJ,
Weghorst CM, Shumway BS, Allen CM and Kalmar JR: Allelic imbalance
in oral lichen planus and assessment of its classification as a
premalignant condition. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 112:359–366. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Esquivel-Pedraza L, Fernández-Cuevas L,
Ruelas-Villavicencio AL, Guerrero-Ramos B, Hernández-Salazar A,
Milke-García MP and Méndez-Flores S: Oral squamous cell carcinoma
and lichen planus vs. lichenoid lesions. Case report. Rev Med Inst
Mex Seguro Soc. 54:673–679. 2016.(In Spanish). PubMed/NCBI
|
|
22
|
Gonzalez-Moles MA, Gil-Montoya JA,
Ruiz-Avila I and Bravo M: Is oral cancer incidence among patients
with oral lichen planus/oral lichenoid lesions underestimated? J
Oral Pathol Med. July 18–2016.(Epub ahead of print) doi:
10.1111/jop.12480. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mares S, Ben Slama L, Gruffaz F, Goudot P
and Bertolus C: Potentially malignant character of oral lichen
planus and lichenoid lesions. Rev Stomatol Chir Maxillofac Chir
Orale. 114:293–298. 2013.(In French). PubMed/NCBI
|
|
24
|
Fitzpatrick SG, Hirsch SA and Gordon SC:
The malignant transformation of oral lichen planus and oral
lichenoid lesions: A systematic review. J Am Dent Assoc. 145:45–56.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lodi G, Scully C, Carrozzo M, Griffiths M,
Sugerman PB and Thongprasom K: Current controversies in oral lichen
planus: Report of an international consensus meeting. Part 2.
Clinical management and malignant transformation. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 100:164–178. 2005. View Article : Google Scholar : PubMed/NCBI
|