Introduction
Stroke constitutes a substantial clinical and
socioeconomic burden. It is the second leading cause of death in
Korea and the third most common cause of disability-adjusted
life-years worldwide (1).
Approximately 87% of all strokes are of ischemic origin (2). Extracranial carotid artery disease
accounts for up to 15–20% of all ischemic strokes (3,4) and
represents an important target in stroke prevention.
Carotid endarterectomy (CEA) is efficacious in
stroke prevention. The North American Symptomatic Carotid
Endarterectomy Trial showed the significant benefit of CEA in
symptomatic patients compared with antiplatelet therapy over 5
years (5). The rate of ipsilateral
stroke, including perioperative events, was 15.7% with CEA, as
compared with 22% for medically managed patients. The European
Carotid Surgery Trial findings indicated that the use of CEA was
beneficial for patients with 70–99% stenosis (6). It has previously been demonstrated that
successful CEA for asymptomatic patients aged <75 years reduces
the 10-year stroke risk (7).
The use of carotid artery stenting (CAS) as a less
invasive alternative to surgical intervention has been increasingly
performed. The randomized, multicenter Carotid Revascularization
Endarterectomy versus Stent Trial compared CAS with CEA for
symptomatic and asymptomatic patients (8). There was no significant difference in
primary events including stroke, death or myocardial infarction
during the periprocedural period and ipsilateral stroke between the
two treatment arms (7.2% with CAS compared with 6.8% with CEA;
hazard ratio for stenting, 1.11; 95% confidence interval (CI),
0.81–1.51).
Since the introduction of CAS, its annual rate of
use increased 250% between 2001 and 2010 in the United States, and
there was a 41% decrease in the annual incidence of CEA (9). In the United Kingdom, 17,560 carotid
procedures were performed between 2006 and 2009 (10). CAS accounted for <5% of all
carotid revascularizations.
A limited amount of comparable information is
available in Asian countries, including Korea. Therefore, the
present study evaluated the national trends of treatment modality
for carotid artery disease in Korea between 2004 and 2013.
Materials and methods
Data collection
Health Insurance Review and Assessment Service
(HIRA) data were used to evaluate the trends in carotid
revascularization in South Korea. The country has a universal
health coverage system, in which National Health Insurance covers
~98% of the Korean population. HIRA claims data are collected when
South Korean healthcare service providers seek reimbursements for
healthcare services that the National Health Insurance Corporation
agrees to cover. Approximately 46 million Korean patients submit
health insurance claims each year. HIRA claims data are compiled
nationally from healthcare providers, and correspond to the number
of claims submitted by patients (11).
The Electronic Data Interchange (EDI) database of
HIRA contains the operation and management codes. Carotid
revascularization data were collected using EDI codes. Table I summarizes the EDI codes for
patients who received CEA and CAS. The codes for commonly performed
procedures for carotid artery disease include O0226, O0227 and
O2066, which refer to open surgery with CEA, and M6602, which is
the code for an endovascular CAS procedure.
 | Table I.EDI codes of the carotid artery
procedures. |
Table I.
EDI codes of the carotid artery
procedures.
| EDI codes | Procedure |
|---|
| O0226 | Carotid
endarterectomy, complex |
| O0227 | Carotid
endarterectomy, complex |
| O2066 | Carotid
endarterectomy with patch closure |
| M6602 | Carotid artery
stenting |
Carotid revascularization in the previous 10 years
was evaluated using EDI data between 2004 and 2013. The total
numbers of CEA and CAS procedures used for the treatment of carotid
artery disease were calculated for this period. The present study
assessed the trends in the number of carotid revascularization
procedures using the aforementioned codes. The present study was
approved by the Institutional Review Board of Kyung Hee University
Hospital (Seoul, Korea).
Statistical analysis
For statistical analysis, a linear-by-linear
association was performed to determine the trends in the amount of
carotid revascularization procedures performed between 2004 and
2013. P<0.05 (two sided) was considered to indicate a
statistically significant difference. Data were analyzed using SPSS
statistical software (version 19.0; IBM SPSS, Armonk, NY, USA).
Results
Carotid revascularization
A total of 23,142 patients received carotid
revascularization between 2004 and 2013, which comprised 4,012 CEA
procedures and 19,130 CAS procedures. The year-by-year profile is
detailed in Table II. The
proportion of CEA procedures increased from 18.3% in 2004 to 20.2%
in 2013. Concurrently, the proportion of CAS procedures decreased
from 81.7% in 2004, to 79.8% in 2013. Revascularization was
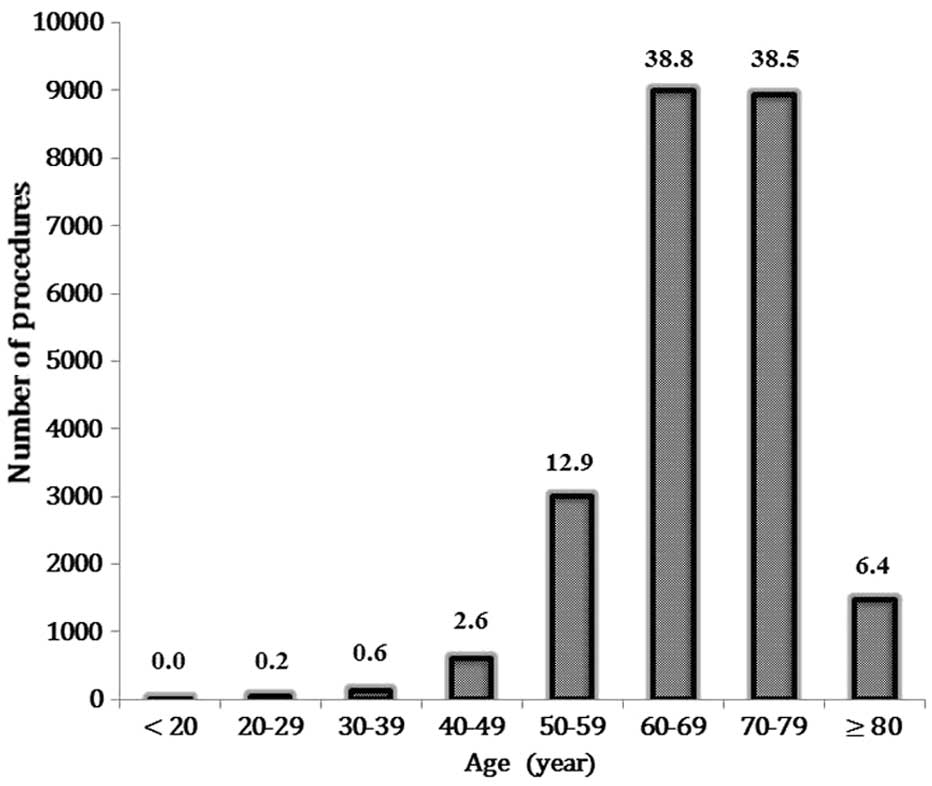
observed to increase with age, and was 12.9% in patients 50–59
years-of-age, 38.8% in those 60–69 years-of-age and 38.5% in
patients 70–79 years-of-age (Fig.
1).
 | Table II.Distribution of carotid artery
procedures by year for 10 years. |
Table II.
Distribution of carotid artery
procedures by year for 10 years.
| Year | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|
| CEA | 198 | 202 | 98 | 224 | 642 | 460 | 450 | 567 | 584 | 587 |
| (%) | 18.3 | 9.9 | 5.3 | 9.6 | 22.0 | 22.3 | 18.6 | 20.6 | 21.1 | 20.2 |
| CAS | 882 |
1,850 |
1,744 | 2,116 |
2,280 |
1,606 | 1,971 |
2,187 |
2,182 |
2,312 |
| (%) | 81.7 | 90.1 | 94.7 | 90.4 | 78.0 | 77.7 | 81.4 | 79.4 | 78.9 | 79.8 |
| Total | 1,080 | 2,053 | 1,843 | 2,340 | 2,922 | 2,066 | 2,421 | 2,754 | 2,766 | 2,899 |
Trends in carotid
revascularization
The total number of carotid revascularizations for
the treatment of carotid artery disease increased significantly
from 1,080 in 2004, to 2,899 in 2013 (risk ratio (RR), 2.55; 95%
CI: 2.38–2.73; Fig. 2A). The
frequency of CAS also increased from 882 in 2004 to 2,312 in 2013
(RR 2.49; 95% CI: 2.30–2.69). The number of CEA procedures
increased from 198 in 2004, to 587 in 2013 (RR 2.82; 95% CI:
2.39–3.31). The differences in the trends for the two procedures
were all statistically significant (P<0.0001).
Carotid revascularization per
1,000,000 Medicare beneficiaries
Population-adjusted frequencies of total, CEA and
CAS over 10 years are displayed in Fig.
2B. The rate of total carotid revascularization per 1,000,000
Medicare beneficiaries significantly increased from 22 procedures
in 2004, to 57 procedures in 2013 (RR 2.59; 95% CI: 1.58–4.24;
P=0.001). The number of CAS procedures performed increased in a
similar trend, from 18 procedures in 2004 to 45 in 2013 (RR 2.50;
95% CI: 1.45–4.32; P=0.001). The number of CEA procedures performed
per 1,000,000 Medicare beneficiaries increased from four procedures
in 2004, to 11 in 2013 (RR 2.75; 95% CI: 0.88–8.64; P=0.08).
Discussion
Several important findings are presented in the
current study. Primarily, the overall rate of carotid
revascularization was observed to have significantly increased by
255%. Secondly, the proportion of CEA procedures compared with CAS
procedures was contrary to the findings reported in Western
countries. In the United States, CEA was performed in preference to
the CAS procedure in 86.5–96.5% of cases (9). A study conducted in the United Kingdom
reported that the majority (96.2%) of carotid revascularizations
involved CEA (10). By contrast, CEA
is only performed in 5.3–22.3% of South Koreans. Thirdly, the
overall rate of CEA procedures increased by 282% between 2004 and
2013, contrary to the declining trend in Western countries.
Finally, the actual number of carotid revascularizations, including
CEA and CAS procedures, was relatively low compared with Western
countries.
Several factors may explain the increase in the
number of carotid revascularization procedures in South Korea. The
overall trend in carotid revascularization was similar to the
alteration in CAS, as CAS was performed in 77.7–94.7% of cases.
Another reason for the increment in the number of carotid
revascularization procedures may be a result of the increased
frequency of risk factors associated with carotid artery disease.
Diabetes and chronic kidney disease, which result in the necessity
for hemodialysis, are independent risk factors for the development
of carotid artery disease (12,13).
Between 1970 and 2000, the prevalence of diabetes in Korea
increased ~3-fold (14). A previous
epidemiologic study reported that the incidence of diabetes in
those between 70 and 79 years-of-age increased between 2009 and
2011 (15). The number of patients
with end-stage renal disease in South Korea has been increasing
rapidly, with an annual increase of ~12% between 2000 and 2009,
according to registry data (16).
CAS was performed 3.5–17.8 times more frequently
when compared with CEA procedures during the study period. In
Western countries, CEA is performed more frequently than CAS
(10). There are several reasons for
the discordance in the use of the two procedures between South
Korea and Western countries. The relatively late introduction of
CEA to Korea is one such reason. In addition, CAS is less invasive,
therefore a decrease in the threshold for CAS in the treatment of
carotid artery disease likely represents a major contribution to
the increase in the number of CAS procedures (17).
The actual number and population-based rates of
carotid revascularization observed during the present study
differed from those presented in the US study (9). In the US, the annual rate of all
carotid revascularization procedures was demonstrated to be 483–737
per million adults per year (9);
whereas the annual incidence of CEA was 418–710 procedures per
million adults per year. Although the CAS procedure was less
commonly performed, the annual rate was 26–65 procedures per
million adults per year. However, in the present study, the annual
rate of all carotid revascularizations was 22–59 procedures per
million adults per year. Annual incidences of CEA and CAS were 2–13
and 18–46 procedures per million adults per year, respectively. The
current study indicated that ~1/20 of revascularization procedures
were performed in Korea compared with data from US Medicare
beneficiaries.
The changes in the national trend were affected by
the publication of randomized trials, including an increase in the
utilization of the CAS procedure subsequent to the publication of
trials favorable to CAS, and a decrease following the publication
of trials indicating the superiority of the CEA procedure (18). Following the publication of
CAS-favorable trials, including the Carotid and Vertebral Artery
Transluminal Angioplasty Study (19), and Stenting and Angioplasty with
Protection in Patients at High Risk for Endarterectomy (20) in 2004, an increase in the use of the
CAS procedure was noted for 4 years. Publication of CEA-favorable
trials, such as Endarterectomy versus Stenting in Patients with
Symptomatic Severe Carotid Stenosis (21) and Stent-Supported Percutaneous
Angioplasty of the Carotid Artery versus Endarterectomy (22), influenced the decrease in the
utilization of the CAS procedure after 2 years. Since the
publication of the CAS-favorable Carotid Revascularization
Endarterectomy Versus Stenting Trial (23), the CAS procedure has been
increasingly utilized.
Several limitations of the present study should be
acknowledged. Foremost, this is a retrospective study based on data
from HIRA. In addition, this study analyzed only the annual
prevalence of the use of CEA and CAS procedures. The association
between the utilization of each of the two procedures and major
adverse events including mortality, stroke and myocardial
infarction after carotid revascularization has yet to be explored,
and requires further elucidation. Finally, it is important to
analyze patients with symptomatic and asymptomatic carotid artery
disease; however, HIRA data does not account for this issue.
In conclusion, 23,142 Korean patients underwent
carotid revascularization between 2004 and 2013. Total carotid
revascularization increased by 255% during this period. This
increase is predominantly due to the 249% increase in CAS
procedures. In addition, contrary to the decreasing trend in the
use of CEA procedures in Western countries, the number of CEA
procedures increased in Korea over this time period. The actual
number and population-based rates of carotid revascularization were
considerably low compared with those of Western countries.
Acknowledgements
The present study was supported by a grant from the
Kyung Hee University in 2010 (grant no. KHU-20101886)
References
|
1
|
Murray CJ, Vos T, Lozano R, Naghavi M,
Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S,
et al: Disability-adjusted life years (DALYs) for 291 diseases and
injuries in 21 regions, 1990-2010: A systematic analysis for the
Global Burden of Disease Study 2010. Lancet. 380:2197–2223. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ooi YC and Gonzalez NR: Management of
extracranial carotid artery disease. Cardiol Clin. 33:1–35. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sacco RL, Kargman DE, Gu Q and Zamanillo
MC: Race-ethnicity and determinants of intracranial atherosclerotic
cerebral infarction. The Northern Manhattan Stroke Study. Stroke.
26:14–20. 1995.
|
|
4
|
Wityk RJ, Lehman D, Klag M, Coresh J, Ahn
H and Litt B: Race and sex differences in the distribution of
cerebral atherosclerosis. Stroke. 27:1974–1980. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Barnett HJ, Taylor DW, Eliasziw M, Fox AJ,
Ferguson GG, Haynes RB, Rankin RN, Clagett GP, Hachinski VC,
Sackett DL, et al: Benefit of carotid endarterectomy in patients
with symptomatic moderate or severe stenosis. North American
Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J
Med. 339:1415–1425. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
European Carotid Surgery Trialists'
Collaborative Group, . Randomised trial of endarterectomy for
recently symptomatic carotid stenosis: Final results of the MRC
European Carotid Surgery Trial (ECST). Lancet. 351:1379–1387. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Halliday A, Harrison M, Hayter E, Kong X,
Mansfield A, Marro J, Pan H, Peto R, Potter J, Rahimi K, et al:
Asymptomatic Carotid Surgery Trial (ACST) Collaborative Group:
10-year stroke prevention after successful carotid endarterectomy
for asymptomatic stenosis (ACST-1): A multicentre randomised trial.
Lancet. 376:1074–1084. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brott TG, Hobson RW II, Howard G, Roubin
GS, Clark WM, Brooks W, Mackey A, Hill MD, Leimgruber PP, Sheffet
AJ, et al: Stenting versus endarterectomy for treatment of
carotid-artery stenosis. N Engl J Med. 363:11–23. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kim LK, Yang DC, Swaminathan RV, Minutello
RM, Okin PM, Lee MK, Sun X, Wong SC, McCormick DJ, Bergman G, et
al: Comparison of trends and outcomes of carotid artery stenting
and endarterectomy in the United States, 2001 to 2010. Circ
Cardiovasc Interv. 7:692–700. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee AHY, Busby J, Brooks M and
Hollingworth W: Uptake of carotid artery stenting in England and
subsequent vascular admissions: An appropriate response to emerging
evidence? Eur J Vasc Endovasc Surg. 46:282–289. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim L, Kim JA and Kim S: A guide for the
utilization of health insurance review and assessment service
national patient samples. Epidemiol Health. 36:e20140082014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tanaka M, Abe Y, Furukado S, Miwa K,
Sakaguchi M, Sakoda S and Kitagawa K: Chronic kidney disease and
carotid atherosclerosis. J Stroke Cerebrovasc Dis. 21:47–51. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kadoglou NPE, Avgerinos ED and Liapis CD:
An update on markers of carotid atherosclerosis in patients with
Type 2 diabetes. Biomarkers Med. 4:601–609. 2010. View Article : Google Scholar
|
|
14
|
Kim DJ: The epidemiology of diabetes in
Korea. Diabetes Metab J. 35:303–308. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Koo BK, Lee CH, Yang BR, Hwang SS and Choi
NK: The incidence and prevalence of diabetes mellitus and related
atherosclerotic complications in Korea: A National Health Insurance
Database Study. PLoS One. 9:e1106502014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jin DC: Current status of dialysis therapy
in Korea. Korean J Intern Med. 26:123–131. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Paraskevas KI and Loftus IM: Carotid
artery stenting: High-risk interventionist versus high-risk center.
J Cardiovasc Surg (Torino). 56:153–157. 2015.PubMed/NCBI
|
|
18
|
Dumont TM and Rughani AI: National trends
in carotid artery revascularization surgery. J Neurosurg.
116:1251–1257. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
CAVATAS Investigators, . Endovascular
versus surgical treatment in patients with carotid stenosis in the
Carotid and Vertebral Artery Transluminal Angioplasty Study
(CAVATAS): A randomised trial. Lancet. 357:1729–1737. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yadav JS, Wholey MH, Kuntz RE, Fayad P,
Katzen BT, Mishkel GJ, Bajwa TK, Whitlow P, Strickman NE, Jaff MR,
et al: Stenting and Angioplasty with Protection in Patients at High
Risk for Endarterectomy Investigators: Protected carotid-artery
stenting versus endarterectomy in high-risk patients. N Engl J Med.
351:1493–1501. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mas JL, Chatellier G, Beyssen B,
Branchereau A, Moulin T, Becquemin JP, Larrue V, Lièvre M, Leys D,
Bonneville JF, et al: EVA-3S Investigators: Endarterectomy versus
stenting in patients with symptomatic severe carotid stenosis. N
Engl J Med. 355:1660–1671. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ringleb PA, Allenberg J, Brückmann H,
Eckstein HH, Fraedrich G, Hartmann M, Hennerici M, Jansen O, Klein
G, Kunze A, et al: SPACE Collaborative Group: 30 day results from
the space trial of stent-protected angioplasty versus carotid
endarterectomy in symptomatic patients: A randomised
non-inferiority trial. Lancet. 368:1239–1247. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mantese VA, Timaran CH, Chiu D, Begg RJ
and Brott TG: CREST Investigators: The Carotid Revascularization
Endarterectomy versus Stenting Trial (CREST): Stenting versus
carotid endarterectomy for carotid disease. Stroke. 41(Suppl):
S31–S34. 2010. View Article : Google Scholar : PubMed/NCBI
|