Introduction
With its growing prevalence, obesity is emerging as
a serious health issue worldwide (1). Obesity has been documented as a risk
factor for a number of systemic disorders with an inflammatory
background (2). In addition, obesity
has been reported to be associated with an increased incidence and
prevalence of periodontal disease in adults (3). A longitudinal study in Japan identified
a positive correlation between body mass index (BMI) and 5-year
incidence of periodontal disease (4).
Obesity is typically associated with unhealthy
lifestyle behaviors, such as a high-calorie diet and low physical
activity, and the modification of these behaviors is essential to
prevent obesity (5). In addition, it
has been reported that oral health behaviors are associated with
general health-related behaviors, in particular, the frequency of
tooth brushing is an indicator of general health-related behaviors
(6). Furthermore, previous studies
have shown that a lower frequency of tooth brushing is associated
with cardiovascular disease risk factors, including metabolic
syndrome (7,8).
However, there is limited information available
regarding the association of oral health behaviors and obesity in
the South Korean population. In addition, the aforementioned
studies used BMI or waist circumference (WC) as indicators of
cardiovascular risk (including obesity). Although these are popular
measurements for evaluation of obesity, they may not accurately
correspond to the degree of adiposity. A direct measurement of
adiposity, such as percentage of body fat (PBF) may be a better
indicator of obesity in relation to cardiometabolic changes
(9). Thus, the present study aimed
to assess the relationship between oral health behaviors and
obesity, as defined by BMI, WC or PBF, in South Korean adults using
nationally representative data.
Materials and methods
Source of data analyzed
This study retrospectively analyzed on data obtained
from the Korea National Health and Nutrition Examination Surveys
[KNHANES; Korea Centers for Disease Control and Prevention (KCDC),
Cheongju, Korea; and the Korean Ministry of Health and Welfare,
Sejong, Korea] between 2008 and 2010 (10). The KNHANES is a nation-wide survey of
non-institutionalized civilians that uses a stratified and
multi-stage probability sampling design, and a rolling
survey-sampling model (11).
Sampling units are based on population and housing from the 2005
National Census Registry in Korea, which records the age, gender
and geographic of the population. Initially, 20,730 participants
≥19 years old were targeted for the survey, and finally, a total of
15,666 individuals (6,744 males and 8,922 females aged 19–92) with
complete data, including socio-demographic and lifestyle
characteristics, oral health behaviors, periodontitis and
anthropometric measurements, were included in the present analyses.
All participants in the survey signed an informed consent form
prior to participation. This survey was reviewed and approved by
the Institutional Review Board of the KCDC.
Socio-demographic and lifestyle
characteristics of participants
All participants were asked about their
socio-demographic status and lifestyle by trained interviewers.
Educational level was classified as a high school diploma or
higher, or under a high school diploma. Monthly household income
was divided into quartiles following adjustment for the number of
family members. Participants were categorized based on the quantity
of alcohol consumed (per day for a month prior to the interview)
into the following three groups: Non-drinker, light to moderate
drinker (1–30 g/day) and heavy drinker (≥30 g/day) (12). Smoking status of participants was
categorized into the following three groups in accordance with
respondents' answers on a self-report questionnaire: Non-smokers
(those who had never smoked or had smoked <100 cigarettes in
their lifetime), ex-smokers (those who had smoked ≥100 cigarettes
in the past) and current smokers (those smoking currently and who
had smoked ≥100 cigarettes). Based upon responses to a modified
form of the International Physical Activity Questionnaire for
Koreans (13), individuals were
regarded as regular physical exercisers if they performed moderate
exercise ≥5 times per week for ≥30 min per session or vigorous
exercise ≥3 times per week for ≥20 min per session (14). Daily food intake over 24 h was
assessed using the 24-h recall method and a food frequency
questionnaire (15). This was used
to calculate the caloric and fat intake of participants using a
food database developed for the KNHANES (13) and the food composition table
published by the National Rural Living Science Institute under the
Rural Development Administration (Suwon, Korea) (10).
Measuring and defining obesity.
General obesity, abdominal obesity and high PBF
A trained staff member performed anthropometric
measurements. Body weight and height were measured to the nearest
0.1 kg and 0.1 cm, respectively, with participants in light indoor
clothing without shoes. BMI was calculated as body weight (kg)
divided by height squared (m2). WC was measured at the
narrowest point between the lower border of the rib cage and the
iliac crest in a standing position. A BMI ≥25 kg/m2 was
defined as general obesity (16),
and abdominal obesity was defined as a WC ≥90 cm in men or ≥85 cm
in women (17). Total body fat mass
(g) and lean mass (g) were measured using whole-body dual-energy
X-ray absorptiometry (DEXA; QDR-4500A fan-beam densitometer;
Hologic, Inc., Bedford, MA, USA) performed by qualified technicians
according to the manufacturer's instructions. Results were analyzed
with industry standard techniques outlined by the Korean Society of
Osteoporosis using Hologic Discovery Software (version 13.1;
Hologic, Inc.). Total PBF was calculated as total body fat mass /
total body mass × 100 (%), and total body mass (g) was calculated
as the sum of fat mass, lean mass and total body mineral content
(g). Participants defined as having a high PBF were those whose PBF
was in the highest quartile of individuals in the current
study.
Oral health behaviors and
periodontitis
The number of times (frequency) and the time of day
when tooth brushing was performed, and the use of secondary oral
products were recorded based upon responses to the questionnaire
(13). Time of day was categorized
as prior to or following breakfast, after lunch and dinner, or
prior to bedtime. Secondary oral products included the following:
dental floss, mouthwash, interdental brushes and electric
toothbrushes.
The World Health Organization (WHO) community
periodontal index (CPI) was used to assess periodontitis, defined
as CPI ≥code 3 (18–21). A code 3 CPI score indicates that
there is ≥1 periodontal pocket of >3.5 mm in 11, 16, 17, 26, 27,
31, 36, 37, 46 and 47 teeth, according to the Federation Dentaire
Internationale system (22,23). Participant's mouths were divided into
sextants and a trained dentist used a CPI probe (Osung MND Co.,
Ltd., Seoul, Korea) with a 0.5 mm ball tip that met WHO guidelines
(21) was used to measure CPI scores
at a probing force of ~20 g. Training was provided to minimize
errors in the measurement of periodontal pocket depth by each
examiner during the examination. Participant's mouths were divided
into sextants, where a sextant was examined if there were ≥2 teeth
present that were not scheduled for extraction. If no index teeth
were present in the sextant qualifying for examination, all
remaining teeth were examined and the highest score was recorded as
the score for that sextant. In the 2008, 2009 and 2010 KNHANES, 24,
29 and 36 trained dentists examined the periodontal status of
participants, respectively, and this data was used for the present
secondary analysis.
Statistical analysis
Results are presented as the mean ± standard error
or as a percentage. A chi-squared test was applied to the data
acquired to examine the relationship between the time of day of
tooth brushing, frequency of tooth brushing, or usage of secondary
oral products and obesity. Independent t-test was used for
continuous variables. A multivariate logistic regression analysis
was performed to estimate the odds ratios (ORs) and 95% confidence
intervals (CIs) of obesity according to the frequency of tooth
brushing per day and what secondary oral products were used.
Variables were adjusted for multivariate logistic regression
analysis as follows: Model 1 was adjusted for age and sex; model 2
was adjusted for the same as model 1, plus alcohol drinking,
smoking status, physical activity, education level and monthly
household income level; and model 3 was adjusted for the same
variables as model 2, plus daily total energy intake, fat intake
per day and periodontitis (CPI ≥3). Statistical analysis was
performed using statistical analysis software (version 9.2; SAS
Institute, Inc., Cary, NC, USA), using survey sampling and analysis
procedures to account for the complex sampling design. P<0.05
was considered to indicate a statistically significant
difference.
Results
Relationship between socio-economic
and lifestyle characteristics of study participants and general
obesity, abdominal obesity or high PBF
Table I describes
characteristics of study participants according to their obesity
status. The mean age, BMI, WC and PBF were found to be
significantly higher in obese participants (general obesity,
abdominal obesity or high PBF) compared with non-obese participants
(all P<0.001). In addition, there was a significant difference
in the status of alcohol consumption, smoking, education level
(decrease; all P<0.001), household income (increase in the
lowest quartile; P<0.05) and daily energy intake (increase;
P<0.001) between obese (all definitions) and non-obese
participants. The percentage of periodontitis was significantly
higher in individuals with general obesity (P<0.001), abdominal
obesity (P<0.001) or high PBF (P=0.032) compared with non-obese
participants. The percentage of individuals who had had a dental
checkup within a year was decreased in generally obese (P=0.054),
abdominally obese (P<0.001) and high PBF (P=0.113) individuals.
The percentage of feeling discomfort whilst chewing or speaking was
significantly different between non-obese and obese participants
(all definitions of obesity; all P<0.05).
 | Table I.Characteristics of study participants
according to their obesity status. |
Table I.
Characteristics of study participants
according to their obesity status.
|
| General obesity
status | Abdominal obesity
status | High body fat
percentage status |
|---|
|
|
|
|
|
|---|
| Characteristic | No | Yes | P-value | No | Yes | P-value | No | Yes | P-value |
|---|
| No. of people
(unweighted) | 10,720 | 4946 | <0.001 | 10,143 | 5523 | <0.001 | 11,750 | 3916 | <0.001 |
| Age (years) | 43.1±0.3 | 46.5±0.3 | <0.001 | 41.4±0.3 | 50.2±0.3 | <0.001 | 43.4±0.3 | 46.3±0.4 | <0.001 |
| No. of males | 46.3 (0.5) | 57.7 (0.8) | <0.001 | 55.2 (0.5) | 38.5 (0.8) | <0.001 | 49.8 (0.5) | 50.3 (0.9) | 0.641 |
| No. of females | 53.7 (0.5) | 42.3 (0.8) | <0.001 | 44.8 (0.5) | 61.5 (0.8) | <0.001 | 50.2 (0.5) | 49.7 (0.9) | 0.641 |
| BMI
(kg/m2) | 21.8±0.0 | 27.5±0.0 | <0.001 | 22.1±0.0 | 26.8±0.1 | <0.001 | 22.7±0.0 | 26.4±0.1 | <0.001 |
| WC (cm) | 76.2±0.1 | 90.5±0.2 | <0.001 | 76.1±0.1 | 90.7±0.1 | <0.001 | 78.2±0.1 | 88.3±0.3 | <0.001 |
| PBF (%) | 26.0±0.1 | 30.6±0.2 | <0.001 | 25.1±0.1 | 32.6±0.1 | <0.001 | 25.2±0.1 | 34.3±0.1 | <0.001 |
| Education (beyond
high school) | 73.6 (0.8) | 66.3 (0.9) | <0.001 | 78.4 (0.7) | 56.1 (1.0) | <0.001 | 72.7 (0.8) | 67.3 (1.1) | <0.001 |
| Household income
(lowest quartile) | 15.0 (0.6) | 16.8 (0.8) | 0.017 | 13.7 (0.6) | 19.7 (0.8) | <0.001 | 14.8 (0.6) | 18.0 (0.9) | <0.001 |
| Alcohol
consumption |
|
|
<0.001a |
|
|
<0.001a |
|
|
<0.001a |
| Non
drinker | 22.5 (0.5) | 23.0 (0.7) |
| 19.8 (0.5) | 28.9 (0.8) |
| 21.7 (0.5) | 25.6 (0.9) |
|
|
Light-moderate | 60.3 (0.6) | 54.4 (0.8) |
| 60.6 (0.6) | 53.8 (0.9) |
| 59.0 (0.6) | 56.7 (1.0) |
|
|
Heavy | 17.3 (0.5) | 22.6 (0.8) |
| 19.7 (0.5) | 17.3 (0.7) |
| 19.3 (0.5) | 17.7 (0.8) |
|
| Smoking status |
|
| <0.001 |
|
| <0.001 |
|
| 0.004 |
|
Non-smoker | 58.4 (0.6) | 51.2 (0.8) |
| 53.1 (0.6) | 62.8 (0.8) |
| 55.9 (0.5) | 57.0 (0.9) |
|
|
Ex-smoker | 15.6 (0.4) | 19.5 (0.7) |
| 17.3 (0.4) | 15.8 (0.6) |
| 16.3 (0.4) | 18.2 (0.8) |
|
| Current
smoker | 26.0 (0.5) | 29.3 (0.8) |
| 29.6 (0.6) | 21.4 (0.7) |
| 27.8 (0.5) | 24.8 (0.9) |
|
| Physical active
regularly | 24.6 (0.6) | 27.8 (0.9) | <0.001 | 26.1 (0.6) | 24.6 (0.8) | 0.073 | 26.5 (0.6) | 22.7 (0.9) | <0.001 |
| Energy intake
(kcal/day) | 1989.7±12.7 | 2098.3±21.5 | <0.001 | 2072.0±13.6 | 1920.0±17.8 | <0.001 | 2054.5±13.2 | 1933.2±20.0 | <0.001 |
| Fat intake/day
(%) | 18.2±0.1 | 17.7±0.2 | 0.023 | 18.8±0.1 | 16.3±0.2 | <0.001 | 18.1±0.1 | 17.8±0.2 | 0.118 |
| Periodontitis | 26.8 (0.8) | 34.0 (1.1) | <0.001 | 25.9 (0.8) | 35.8 (1.1) | <0.001 | 28.5 (0.8) | 30.8 (1.1) | 0.032 |
| Dental checkup in
<year | 25.3 (0.7) | 23.4 (1.0) | 0.054 | 26.2 (0.7) | 21.4 (0.9) | <0.001 | 25.4 (0.8) | 23.6 (1.2) | 0.113 |
| Experience of
caries in permanent teeth | 90.9 (0.4) | 89.0 (0.6) | 0.003 | 90.0 (0.4) | 91.0 (0.5) | 0.110 | 90.7 (0.4) | 89.2 (0.7) | 0.037 |
| Chewing
discomfort |
|
| 0.006a |
|
|
<0.001a |
|
| 0.419a |
| Great
discomfort | 5.0 (0.2) | 5.9 (0.4) |
| 4.3 (0.2) | 7.4 (0.4) |
| 5.3 (0.3) | 5.3 (0.4) |
|
|
Discomfort | 20.2 (0.5) | 22.6 (0.7) |
| 19.2 (0.5) | 24.8 (0.7) |
| 21.0 (0.5) | 20.8 (0.8) |
|
| Minor
problem | 16.3 (0.5) | 15.1 (0.7) |
| 16.3 (0.5) | 15.1 (0.6) |
| 16.1 (0.5) | 15.3 (0.8) |
|
| Minimal
problem | 26.4 (0.8) | 25.6 (1.0) |
| 27.1 (0.8) | 24.3 (0.9) |
| 26.4 (0.8) | 25.4 (1.3) |
|
| No
discomfort | 32.0 (0.9) | 30.8 (1.0) |
| 33.0 (1.0) | 28.5 (1.0) |
| 31.1 (0.9) | 33.2 (1.4) |
|
| Speech
discomfort |
|
| 0.038a |
|
|
<0.001a |
|
| 0.007a |
| Great
discomfort | 1.2 (0.1) | 1.2 (0.2) |
| 1.1 (0.1) | 1.4 (0.2) |
| 1.3 (0.1) | 0.9 (0.1) |
|
|
Discomfort | 5.7 (0.3) | 7.1 (0.4) |
| 5.1 (0.3) | 8.4 (0.4) |
| 5.7 (0.3) | 7.3 (0.5) |
|
| Minor
problem | 7.7 (0.3) | 7.9 (0.5) |
| 7.5 (0.4) | 8.3 (0.5) |
| 8.0 (0.3) | 7.1 (0.5) |
|
| Minimal
problem | 26.5 (1.0) | 25.9 (1.1) |
| 26.1 (1.0) | 26.7 (1.2) |
| 26.7 (1.0) | 25.2 (1.4) |
|
| No
discomfort | 58.9 (1.1) | 58.0 (1.2) |
| 60.2 (1.1) | 55.2 (1.3) |
| 58.3 (1.0) | 59.5 (1.6) |
|
Time of day of tooth brushing and type
of secondary oral products used in relation to obesity status
Table II shows the
relationship between obesity status and the time of day tooth
brushing occurred or the secondary oral products that were used.
Participants with general obesity or high PBF brushed their teeth
significantly less after meals or snacks compared with non-obese
individuals (P<0.05). In addition, abdominally obese individuals
had a lower tooth brushing rate following lunch or snacks
(P<0.05). Participants with general obesity, abdominal obesity
or high PBF exhibited a significantly lower rate of using floss
(P<0.001) compared with non-obese individuals. A significantly
lower amount of those with general obesity (P=0.002) or a high PBF
(P=0.002) used mouthwash compared to individuals without general
obesity or high PBF.
 | Table II.Time of day of tooth brushing and
type of secondary oral products used in relation to obesity
status. |
Table II.
Time of day of tooth brushing and
type of secondary oral products used in relation to obesity
status.
|
| General
obesity | Abdominal
obesity | High body fat
percentage |
|---|
|
|
|
|
|
|---|
| Parameter | No | Yes | P-value | No | Yes | P-value | No | Yes | P-value |
|---|
| Time of tooth
brushing |
|
|
|
|
|
|
|
|
|
| Before
breakfast | 30.7 (0.5) | 33.5 (0.9) | 0.004 | 31.9 (0.6) | 30.6 (1.0) | 0.197 | 24.7 (0.8) | 25.6 (1.1) | 0.366 |
| After
breakfast | 33.9 (0.8) | 30.4 (0.5) | <0.001 | 30.4 (1.0) | 32.1 (0.6) | 0.111 | 26.7 (1.0) | 24.2 (0.8) | 0.008 |
| Before
lunch | 31.5 (0.5) | 31.9 (4.3) | 0.919 | 31.6 (0.6) | 28.4 (3.4) | 0.351 | 25.0 (0.8) | 23.1 (3.4) | 0.583 |
| After
lunch | 34.5 (0.6) | 27.2 (0.7) | <0.001 | 35.6 (0.7) | 25.9 (0.7) | <0.001 | 26.6 (0.9) | 22.7 (0.9) | <0.001 |
| Before
dinner | 31.5 (0.5) | 29.0 (2.6) | 0.347 | 31.6 (0.6) | 30.8 (2.8) | 0.788 | 25.0 (0.8) | 22.3 (2.6) | 0.290 |
| After
dinner | 33.2 (0.8) | 30.4 (0.6) | 0.003 | 32.7 (0.9) | 30.9 (0.7) | 0.069 | 27.2 (1.1) | 23.7 (0.8) | <0.001 |
| After
snacks | 31.6 (0.5) | 25.5 (2.6) | 0.027 | 31.8 (0.6) | 23.8 (2.3) | 0.001 | 25.1 (0.8) | 20.1 (2.2) | 0.039 |
| Before
bedtime | 32.1 (0.6) | 30.3 (0.7) | 0.058 | 33.6 (0.7) | 28.1 (0.8) | <0.001 | 25.4 (0.9) | 24.2 (1.0) | 0.233 |
| Secondary oral
products used |
|
|
|
|
|
|
|
|
|
|
Floss | 32.3 (0.5) | 25.3 (1.2) | <0.001 | 32.7 (0.6) | 24.0 (1.2) | <0.001 | 25.7 (0.8) | 19.5 (1.2) | <0.001 |
|
Interdental brush | 31.6 (0.5) | 29.6 (1.7) | 0.248 | 32.0 (0.6) | 27.0 (1.5) | 0.001 | 25.0 (0.8) | 24.7 (1.6) | 0.868 |
|
Mouthwash | 32.0 (0.5) | 27.3 (1.3) | 0.002 | 31.9 (0.6) | 29.4 (1.2) | 0.054 | 25.4 (0.8) | 21.3 (1.3) | 0.002 |
|
Electric toothbrush | 31.4 (0.5) | 32.3 (1.9) | 0.650 | 31.7 (0.6) | 29.1 (1.9) | 0.189 | 25.1 (0.8) | 22.7 (1.8) | 0.200 |
|
Other(s) | 31.5 (0.5) | 26.8 (3.6) | 0.224 | 31.6 (0.6) | 28.4 (3.6) | 0.397 | 25.0 (0.8) | 25.1 (3.8) | 0.979 |
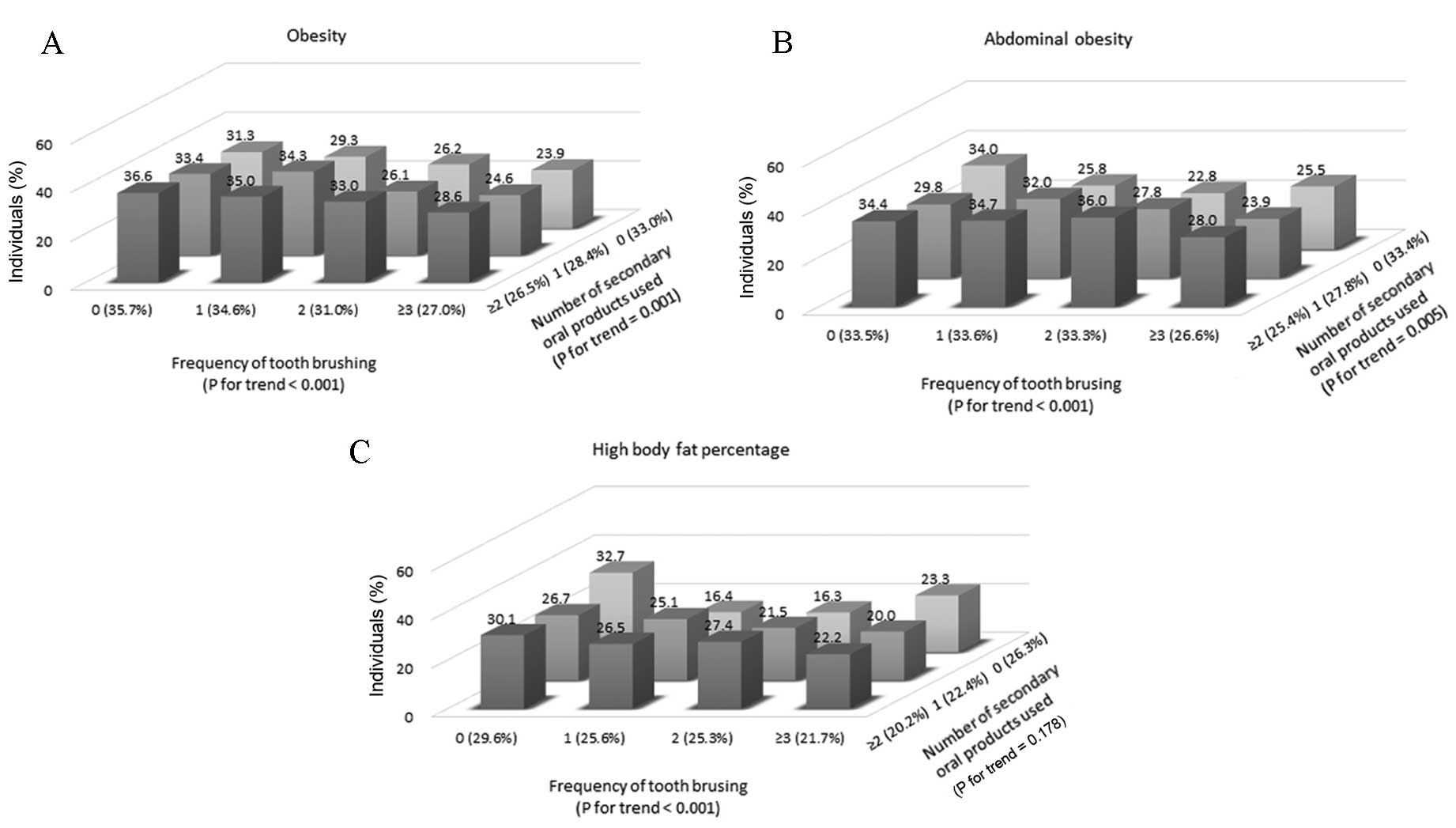
Daily frequency of tooth brushing and
secondary oral products used in relation to obesity status
Figure 1 shows the
percentage of participants with general obesity, abdominal obesity
or a high PBF related to daily frequency of tooth brushing and
secondary oral products used. The prevalence of general obesity and
abdominal obesity significantly decreased (P<0.001 for overall
trend) with increasing number of tooth brushing episodes
(P<0.001 for trend) and secondary oral products used (P<0.001
for trend). The prevalence of high PBF significantly decreased as
the frequency of tooth brushing episodes increased (P<0.001 for
trend). Table III shows the
adjusted ORs and their 95% CIs for all definitions of obesity
according to the frequency of tooth brushing and the number of
secondary oral products used. According to trend analysis using a
generalized linear model, the OR of all definitions of obesity
significantly increased as the frequency of tooth brushing
decreased (all P<0.001) and the number of secondary oral
products used (all P<0.05) decreased in all variable-adjusted
models.
 | Table III.Adjusted odds ratios for general
obesity, abdominal obesity and high body fat percentage according
to the daily frequency of tooth brushing and number of secondary
oral products used. |
Table III.
Adjusted odds ratios for general
obesity, abdominal obesity and high body fat percentage according
to the daily frequency of tooth brushing and number of secondary
oral products used.
|
| Frequency of tooth
brushing per day | Number of secondary
oral products used per day |
|---|
|
|
|
|
|---|
| Type of obesity and
model | ≥3 | 2 | 1 | 0 | P-value for
trend | ≥2 | 1 | 0 | P-value for
trend |
|---|
| General
obesity |
|
|
|
|
|
|
|
|
|
| Model
1 | 1 | 1.19
(1.06–1.33) | 1.34
(1.20–1.49) | 1.36
(1.19–1.56) | <0.001 | 1 | 1.04
(0.87–1.25) | 1.18
(0.98–1.41) | 0.008 |
| Model
2 | 1 | 1.34
(1.20–1.49) | 1.45
(1.30–1.60) | 1.50
(1.30–1.73) | <0.001 | 1 | 1.14
(0.94–1.38) | 1.33
(1.12–1.59) | 0.029 |
| Model
3 | 1 | 1.21
(1.08–1.35) | 1.22
(1.08–1.38) | 1.48
(1.28–1.72) | <0.001 | 1 | 1.12
(0.91–1.39) | 1.32
(1.07–1.61) | 0.021 |
| Abdominal
obesity |
|
|
|
|
|
|
|
|
|
| Model
1 | 1 | 1.17
(1.05–1.31) | 1.33
(1.19–1.48) | 1.38
(1.20–1.58) | <0.001 | 1 | 1.02
(0.85–1.22) | 1.14
(0.95–1.36) | <0.001 |
| Model
2 | 1 | 1.30
(1.16–1.45) | 1.39
(1.25–1.54) | 1.48
(1.27–1.71) | <0.001 | 1 | 1.10
(0.91–1.34) | 1.23
(1.03–1.48) | 0.004 |
| Model
3 | 1 | 1.21
(1.08–1.35) | 1.23
(1.09–1.39) | 1.55
(1.34–1.80) | <0.001 | 1 | 1.10
(0.88–1.36) | 1.28
(1.04–1.57) | 0.013 |
| High body fat
percentage |
|
|
|
|
|
|
|
|
|
| Model
1 | 1 | 1.13
(0.99–1.27) | 1.28
(1.13–1.45) | 1.37
(1.17–1.61) | <0.001 | 1 | 1.03
(0.85–1.25) | 1.16
(0.96–1.40) | <0.001 |
| Model
2 | 1 | 1.28
(1.14–1.43) | 1.41
(1.25–1.58) | 1.54
(1.32–1.81) | <0.001 | 1 | 1.16
(0.94–1.44) | 1.25
(1.03–1.51) | 0.002 |
| Model
3 | 1 | 1.18
(1.04–1.34) | 1.21
(1.07–1.38) | 1.60
(1.36–1.87) | <0.001 | 1 | 1.17
(0.93–1.48) | 1.38
(1.10–1.73) | <0.001 |
Discussion
The aim of the present study was to assess the
relationship between oral health behaviors and a number of measures
of obesity. A strong association was identified between poor oral
health behavior and obesity (all definitions). Typically,
individuals with obesity defined by BMI, WC or PBF brushed their
teeth less frequently and used fewer secondary oral products
compared with participants without obesity. A previous study found
that the hazard ratios after adjusting for age, smoking status and
clinical history of diabetes mellitus were 1.30 (P<0.001) and
1.44 (P=0.072) in males and 1.70 (P<0.01) and 3.24 (P<0.05)
in females for those with a BMI between 25 and 30 kg/m2
and ≥30 kg/m2, respectively, compared with those with
BMI <22 kg/m2 (4). In
addition, a systematic review and meta-analysis reported
significant associations between periodontitis and BMI category,
with an OR of 1.81 for obesity, 1.27 for overweight, and 2.13 for
obese and overweight participants combined (24).
Inflammation may be the causative factor for the
association identified between oral health behavior and obesity.
Poor oral health behavior and a low frequency of tooth brushing may
increase inflammation (25,26). Previous studies have found that poor
oral hygiene is associated with higher levels of inflammatory
markers in the blood, such as C-reactive protein and fibrinogen
(27,28). In addition, a recent systematic
review determined that an elevated level of C-reactive protein was
associated with obesity (29).
Studies on fibrinogen levels from the blood of obese patients prior
to and following weight reduction observed negative correlations
between BM and fibrinogen levels (30).
Oral health behavior is typically associated with
other health-related behaviors, which may explain the association
between oral health behavior and obesity (31). A previous study noted that oral
disease, such as dental caries, has substantial negative medical
consequences, which may not be fully appreciated due to the
separation of the fields of medicine and dentistry (32). Authors of previous studies emphasize
that health-promotion activities should include promotion of oral
health (31,33). Furthermore, the results of a previous
study examining the relationships among health-enhancing behaviors,
indicated that regular tooth brushing reinforces other healthy
lifestyle habits (34). Moreover,
the results of a study on Korean university students highlighted
the importance of oral health behavior, and suggested that obesity,
oral health and nutrition need to be addressed jointly in
health-promotion strategies (35).
In addition, due to the links between nutrition and obesity with
caries, pediatric dentists have a growing role in the battle
against childhood obesity (36).
General obesity and abdominal obesity have
classically been defined by BMI and WC, respectively. However,
adiposity has recently been determined to be closely correlated
with metabolic risk, and measurements, such as PBF and waist to hip
ratios, have been noted as valuable tools for the assessment of
obesity (37). In the present study,
BMI, WC and PBF were used to define obesity, which revealed that
poor oral health behaviors were significantly associated with
obesity, irrespective of the measurement used. However, a previous
study found that independent variables representing dental health
were more often associated with BMI and WC obesity indicators
compared with waist to hip ratio (38). Thus, the choice of obesity
measurements may affect the results of studies related to oral
health.
The present study identified that obese individuals
had higher rates of periodontitis, which was in agreement with the
findings of a recent systemic review (39). In addition, the current study
observed that the percentage of participants who had a dental
check-up within the past year was lower in those with obesity (all
measurements) compared with non-obese individuals. This is in
agreement with previous studies, which have shown that obesity is
associated with behaviors such as irregular dental visits (36,38).
Furthermore, in the present study, a higher percentage of non-obese
participants had no discomfort when chewing compared with generally
obese and abdominally obese participants, similarly to previous
studies that showed a cause-and-effect association between
masticatory function and obesity (40,41).
The present study has several limitations. Firstly,
the cross-sectional design of the KNHANES prevents the deduction of
causal relationships between poor oral health behaviors and
obesity, thus the directions of the demonstrated associations could
not be established. Secondly, DEXA scanning during the KNHANES
study may lead to hydration-induced errors, and therefore may vary
in accuracy according to each individuals' fluid balance (42). Thirdly, visceral fat and inflammatory
markers could not be investigated due to the limited data of the
KNHANES. However, the current study analyzed a nationally
representative sample of South Koreans, considered different
measurements of obesity and adjusted for a number of relevant
confounding factors.
In conclusion, the present study identified that
individuals with obesity, irrespective of the method used to define
obesity, had a lower daily frequency of tooth brushing and used
fewer secondary oral products. Conversely, poor oral health
behaviors were positively associated with general obesity,
abdominal obesity and a high PBF. This indicates that good oral
health behaviors should be emphasized in the health-promotion
strategies for obese patients.
Acknowledgements
This present study was supported by Basic Science
Research Program through the National Research Foundation of Korea
funded by the Ministry of Science, ICT & Future Planning (grant
no. NRF-2014R1A1A1003106). The authors thank the Korea Centers for
Disease Control and Prevention for providing the data used in the
present study.
References
|
1
|
Hossain P, Kawar B and El Nahas M: Obesity
and diabetes in the developing world-a growing challenge. N Engl J
Med. 356:213–215. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Khanna S and Mali AM: Evaluation of tumor
necrosis factor-α (TNF-α) levels in plasma and their correlation
with periodontal status in obese and non-obese subjects. J Indian
Soc Periodontol. 14:217–221. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pischon N, Heng N, Bernimoulin JP, Kleber
BM, Willich SN and Pischon T: Obesity, inflammation, and
periodontal disease. J Dent Res. 86:400–409. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Morita I, Okamoto Y, Yoshii S, Nakagaki H,
Mizuno K, Sheiham A and Sabbah W: Five-year incidence of
periodontal disease is related to body mass index. J Dent Res.
90:199–202. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kushner RF: Weight loss strategies for
treatment of obesity. Prog Cardiovasc Dis. 56:465–472. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tada A and Matsukubo T: Relationship
between oral health behaviors and general health behaviors in a
Japanese adult population. J Public Health Dent. 63:250–254. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kobayashi Y, Niu K, Guan L, Momma H, Guo
H, Cui Y and Nagatomi R: Oral health behavior and metabolic
syndrome and its components in adults. J Dent Res. 91:479–484.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim YH, Kim DH, Lim KS, Ko BJ, Han BD, Nam
GE, Park YG, Han KD, Kim JH and Cho KH: Oral health behaviors and
metabolic syndrome: The 2008–2010 Korean national health and
nutrition examination survey. Clin Oral Investig. 18:1517–1524.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Joseph L, Wasir JS, Misra A, Vikram NK,
Goel K, Pandey RM, Chandra M, Poddar P and Kondal D: Appropriate
values of adiposity and lean body mass indices to detect
cardiovascular risk factors in Asian Indians. Diabetes Technol
Ther. 13:899–906. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee JY, Jun N and Baik I: Associations
between dietary patterns and screen time among Korean adolescents.
Nutr Res Pract. 7:330–335. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Park YG: Comments on statistical issues in
march 2014. Korean J Fam Med. 35:107–108. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Agarwal DP: Cardioprotective effects of
light-moderate consumption of alcohol: A review of putative
mechanisms. Alcohol Alcohol. 37:409–415. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Korea Center for Disease Control and
Prevention & Ministry of Health and Welfare, . (2008–2010)
Korean national health and examination surveys: the 4th and 5th
surveys. Available at. http://knhanes.cdc.go.kr/.JournalMarch
31–2013
|
|
14
|
Oh JY, Yang YJ, Kim BS and Kang JH:
Validity and reliability of Korean version of International
Physical Activity Questionnaire (IPAQ) short form. J Korean Acad
Fam Med. 28:532–541. 2007.
|
|
15
|
Friis S, Kjaer S Kruger, Stripp C and
Overvad K: Reproducibility and relative validity of a
self-administered semiquantitative food frequency questionnaire
applied to younger women. J Clin Epidemiol. 50:303–311. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Oh SW, Shin SA, Yun YH, Yoo T and Huh BY:
Cut-off point of BMI and obesity-related comorbidities and
mortality in middle-aged Koreans. Obes Res. 12:2031–2040. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee S, Park HS, Kim SM, Kwon HS, Kim DY,
Kim DJ, Cho GJ, Han JH, Kim SR, Park CY, et al: Cut-off points of
waist circumference for defining abdominal obesity in the Korean
population. Korean J Obes. 15:1–9. 2006.(In Korean). View Article : Google Scholar
|
|
18
|
World Health Organization, . A guide to
oral epidemiological investigations. WHO; Geneva: 1979
|
|
19
|
World Health Organization, . Monitoring
and evaluation of oral health: Report of a WHO expert. WHO; Geneva:
1989
|
|
20
|
World Health Organization, . Oral health
surveys: Basic methods. 3rd. WHO; Geneva: 1987
|
|
21
|
World Health Organization, . Oral health
surveys: Basic methods. 4th. WHO; Geneva: 1997
|
|
22
|
Lee JB, Yi HY and Bae KH: The association
between periodontitis and dyslipidemia based on the Fourth Korea
National Health and Nutrition Examination Survey. J Clin
Periodontol. 40:437–442. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Park JB, Han K, Park YG and Ko Y:
Association between alcohol consumption and periodontal disease:
The 2008 to 2010 Korea national health and nutrition examination
survey. J Periodontol. 85:1521–1528. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Suvan J, D'Aiuto F, Moles DR, Petrie A and
Donos N: Association between overweight/obesity and periodontitis
in adults. A systematic review. Obes Rev. 12:e381–e404. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kim YH, Kim DH, Lim KS, Ko BJ, Han BD, Nam
GE, Park YG, Han KD, Kim JH and Cho KH: Oral health behaviors and
metabolic syndrome: The 2008–2010 Korean national health and
nutrition examination survey. Clin Oral Investig. 18:1517–1524.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Vysniauskaite S and Vehkalahti MM: Impacts
of toothbrushing frequency on periodontal findings in a group of
elderly Lithuanians. Oral Health Prev Dent. 7:129–136.
2009.PubMed/NCBI
|
|
27
|
de Oliveira C, Watt R and Hamer M:
Toothbrushing, inflammation, and risk of cardiovascular disease:
Results from scottish health survey. Bmj. 340:c24512010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bickel C, Rupprecht HJ, Blankenberg S,
Espiniola-Klein C, Schlitt A, Rippin G, Hafner G, Treude R, Othman
H, Hofmann KP, et al: Relation of markers of inflammation
(C-reactive protein, fibrinogen, von Willebrand factor, and
leukocyte count) and statin therapy to long-term mortality in
patients with angiographically proven coronary artery disease. Am J
Cardiol. 89:901–908. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Choi J, Joseph L and Pilote L: Obesity and
C-reactive protein in various populations: A systematic review and
meta-analysis. Obes Rev. 14:232–244. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ditschuneit HH, Flechtner-Mors M and Adler
G: Fibrinogen in obesity before and after weight reduction. Obes
Res. 3:43–48. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Cinar AB and Murtomaa H: Interrelation
between obesity, oral health and life-style factors among Turkish
school children. Clin Oral Investig. 15:177–184. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mouradian WE, Wehr E and Crall JJ:
Disparities in children's oral health and access to dental care.
Jama. 284:2625–2631. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ostberg AL, Nyholm M, Gullberg B, Råstam L
and Lindblad U: Tooth loss and obesity in a defined Swedish
population. Scand J Public Health. 37:427–433. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Donovan JE, Jessor R and Costa FM:
Structure of health-enhancing behavior in adolescence: A
latent-variable approach. J Health Soc Behav. 34:346–362. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Park HJ, Lee MJ, Kim SH and Jeong MA:
Effects of health practices and oral health behaviors on obesity in
university students. J Korea Cont Ass. 11:395–406. 2011.(In
Korean). View Article : Google Scholar
|
|
36
|
Vann WF Jr, Bouwens TJ, Braithwaite AS and
Lee JY: The childhood obesity epidemic: A role for pediatric
dentists? Pediatr Dent. 27:271–276. 2005.PubMed/NCBI
|
|
37
|
Saxlin T, Ylöstalo P, Suominen-Taipale L,
Männistö S and Knuuttila M: Association between periodontal
infection and obesity: Results of the health 2000 survey. J Clin
Periodontol. 38:236–242. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Östberg AL, Bengtsson C, Lissner L and
Hakeberg M: Oral health and obesity indicators. BMC Oral Health.
12:502012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Moura-Grec PG, Marsicano JA, Carvalho CA
and Sales-Peres SH: Obesity and periodontitis: Systematic review
and meta-analysis. Cien Saude Colet. 19:1763–1772. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Katagiri S, Nitta H, Nagasawa T, Izumi Y,
Kanazawa M, Matsuo A, Chiba H, Miyazaki S, Miyauchi T, Nakamura N,
et al: Reduced masticatory function in non-elderly obese Japanese
adults. Obes Res Clin Pract. 5:e267–e360. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ekbäck G, Näslund I, Montgomery SM and
Ordell S: Self-perceived oral health and obesity among 65 years old
in two Swedish counties. Swed Dent J. 34:207–215. 2010.PubMed/NCBI
|
|
42
|
Lang PO, Trivalle C, Vogel T, Proust J and
Papazian JP: Markers of metabolic and cardiovascular health in
adults: Comparative analysis of DEXA-based body composition
components and BMI categories. J Cardiol. 65:42–49. 2015.
View Article : Google Scholar : PubMed/NCBI
|