Introduction
Perioperative myocardial injury remains one of the
most serious complications of cardiac surgery (1–3), and
numerous factors have been implicated during the pathogenesis
process, including the technique of cardiac surgery, induction of
cardioplegia and period of cardiac arrest (4–6). The
primary mechanisms underlying myocardial dysfunction in this
process are ischemic-reperfusion injury and the associated
inflammatory responses (6–9). Several cardioprotective agents have
been investigated for preventing iatrogenic myocardial injury.
However, the majority of these agents affect only a single aspect
of the pathogenesis of ischemic-reperfusion injury, and results of
pilot studies are not consistent (10,11).
β-adrenergic receptor blockers (β-blockers) have been extensively
used as cornerstone medications in the management of ischemic heart
disease, most likely by reducing myocardial oxygen demands and
mitigating the ischemia-induced injury (12,13).
However, to the best of our knowledge, the direct effect of
preprocedural administration of esmolol on the markers of
myocardial injury, as well as hemodynamic characteristics, have
rarely been evaluated in Asian patients who were scheduled for
elective open-heart surgery. Therefore, the present study describes
a pilot single-center randomized controlled trial that was
performed in order to evaluate the potential myocardial protective
effects of esmolol, as well as its impact on hemodynamic
parameters, in Chinese patients who underwent elective open-heart
cardiac surgery under a cardiopulmonary bypass (CPB).
Patients and methods
Study design
The study protocol was approved by the Local Ethics
Committee of The First Affiliated Hospital of Dalian Medical
University (KY2009-38; Dalian, China), and written informed consent
was obtained from all the participating patients. The present
investigation was designed as a single-center, randomized
controlled trial on patients scheduled to undergo open-heart
cardiac surgery with CPB at the Department of Cardiovascular
Surgery in the First Affiliated Hospital of Dalian Medical
University.
Petient inclusion and exclusion
criteria
Patients were included in the current study if they
met the following criteria: i) Age between 40 and 80 years; ii)
patients undergoing elective primary cardiac surgery, including
coronary artery bypass graft (CABG) or heart valvular replacement
(HVR); iii) a cardiac function of New York Heart Association class
II or III; and iv) no evidence of myocardial ischemia or elevation
of serum levels of myocardial markers (troponin I [TnI], creatine
kinase [CK] or CK-MB fraction [CK-MB]) within the last 24 h prior
to surgery. The exclusion criteria were as follows: i) A diagnosis
of acute myocardial infarction within the last 4 weeks prior to the
scheduled surgery; ii) an activated phase of rheumatic diseases;
iii) left ventricular ejection fraction of <40%; iv)
preoperatively confirmed intra-cardiac shunt; v) a hematocrit of
<30%; and vi) severe systemic diseases, including pulmonary
diseases, hepatic, renal, musculoskeletal diseases or immune system
illnesses. Additionally, patients receiving oral hypoglycemic
agents or theophyllines were excluded since these medications are
known to influence the process of ischemia-reperfusion injury
(14).
Patient groups
Eligible patients were assigned to one of the two
study arms on the basis of a computer-generated randomization list:
One group was administered the conventional care (control group;
n=12), while the other was administered conventional care plus
intravenous esmolol infusion (esmolol group; n=12; Sanlian
Pharmacy, Harbin, China). The mean age of the patients was 60.5
years old and 14 of the enrolled patients were male.
Anesthetic protocols
All patients included were administered
intramuscular injections of scopolamine (0.6 µg/kg; Minsheng
Pharmacy, Hangzhou, China), morphine (0.1 mg/kg) and pethidine (1
mg/kg) (both purchased from Shenyang 1st Pharmacy of Northeastern
China, Shenyang, China) 30 min prior to the induction of
anesthesia. Preoperative sedation and anesthesia were achieved with
the intravenous injection of midazolam (0.1 mg/kg; Enhua Pharmacy,
Jiangsu, China), fentanyl (10 µg/kg; Renfu Pharmacy, Yichang,
China), etomidate (0.2–0.3 mg/kg; Enhua Pharmacy) and cisatracurium
besilate (0.2 mg/kg; Hengrui Pharmacy, Jiangsu, China), and these
drugs were administered during the surgery in order to maintain a
stable hemodynamic status. Following tracheal intubation, the
patients were placed on artificial ventilation such that the
end-tidal carbon dioxide pressure was maintained at 30–35 mmHg and
the airway pressure at 8–18 cm H2O. Anesthesia was
maintained using the standard method with continuous administration
of propofol at 3–6 mg/kg/h.
Patients in the esmolol group were administered
intravenous esmolol (70 µg/kg/min) during the incision until the
initiation of CPB, and the dosages of esmolol were titrated every 2
min to maintain the heart rate (HR) of each patient within 80% of
the baseline level. Patients assigned to the control group were
administered equal volumes of 0.9% saline.
CPB and surgical protocols
All patients underwent cardiac surgery under CPB
according to the standard method using a roller pump and a membrane
oxygenator with a priming solution (Jinyao Pharmacy, Tianjin,
China). During CPB, pump flow was set such that the mean arterial
pressure (MAP) was maintained between 50 and 80 mmHg. The blood
temperature was allowed to drop to <30°C and restored back to
36°C with active rewarming at the end of CPB. Myocardial protection
was ensured with the induction of cardioplegia by administration of
cold potassium solution (10–15 ml/kg) and by placement of ice chips
in the pericardial region to maintain the heart in a hypothermic
condition. Moreover, cardioplegia was achieved using the
single-clamp technique in an anterograde fashion. Following the
establishment of CPB, vasoactive medications, including dopamine,
nitroglycerin and norepinephrine, were administered to maintain the
arterial blood pressure at a relatively stable level.
The aortic cross-clamp was completely released,
followed by the placement of the epicardial atrial or ventricular
pacing wires. The aortic and venous cannulas were removed following
the administration of the appropriate test dose of protamine such
that the activated clotting time was maintained at 110–140 sec, and
the surgery was continued with the closure of the pericardium and
sternum. Following surgery, the patients were closely monitored
during their stay in the intensive care unit (ICU) at The First
Affiliated Hospital of Dalian Medican University for at least 12
h.
Study outcomes
The primary outcomes analyzed in the present study
were perioperative changes in the concentrations of the serum
markers of myocardial injury, including TnI, CK and CK-MB. Briefly,
arterial blood samples (3 ml for each time point) of the patients
were collected from the radial artery or from the arterial
catheters during CPB at the following time points: Baseline (prior
to the start of the CPB procedure), prior to aortic cannulation, 30
min prior to the placement of the aortic cross-clamp at the time of
releasing the aortic cross-clamp, and 120 min after the release of
the aortic cross-clamp. The levels of the markers of myocardial
injury were measured using the Roche Biochemical Analyzer (ADVIA
centaur-CP; Siemens AG, Munich, Germany) according to the
manufacturer's instructions. The secondary outcomes analyzed were
the changes in the levels of the hemodynamic parameters, including
HR, MAP and central venous pressure (CVP), during the surgery and
during the 12-h ICU follow-up. In addition to the abovementioned
parameters, other related clinical outcomes were also evaluated,
including the characteristics of CPB, usage of vasoactive
medications, rebeating status of the heart and the incidence of
postoperative adverse events.
Statistical analysis
The results are presented as mean values with
standard deviation. Significant intergroup differences at the
different time points were analyzed using the Student's
t–test. Moreover, one-way analysis of variance was used for
intragroup comparison of the values of the hemodynamic parameters
if the data were normally distributed; if the distribution was
abnormal, the Friedman test was used. P<0.05 was used to
indicate a statistically significant difference. All the
statistical analyses were performed using SPSS Software (version
13.0; SPSS, Inc., Chicago, IL, USA).
Results
Patient baseline characteristics
In total, 14 patients enrolled underwent CABG, while
10 patients underwent HVR. All the surgical procedures were
executed successfully, and the patients were closely monitored
during their 12-h postoperative ICU follow-up period. The baseline
characteristics of the patients included are listed in Table I. The two study groups were well
balanced in terms of the demographic characteristics, prevalence of
hypertension, diabetes, types of surgery and class of cardiac
function.
 | Table I.Baseline characteristics of patients
enrolled in the esmolol and control groups. |
Table I.
Baseline characteristics of patients
enrolled in the esmolol and control groups.
| Characteristics | Esmolol group
(n=12) | Control (n=12) |
|---|
| Male (n, %) | 8 (66.7) | 6 (50) |
| Age, years | 58.9±9.8 | 62.1±7.1 |
| Height, cm | 166.3±9.8 | 164.9±8.6 |
| BW, kg | 69.9±9.0 | 66.8±8.9 |
| LVEF, % | 52.7±6.0 | 55.8±3.2 |
| Hypertension (n,
%) | 8 (66.7) | 8 (66.7) |
| Diabetic (n, %) | 4 (33.3) | 3 (25.0) |
| Smokers (n, %) | 7 (58.3) | 6 (50) |
| Preoperative |
|
|
| β blockers (n,
%) | 1 (8.3) | 0 (0.0) |
| Surgery |
|
|
| CABG (n,
%) | 7 (58.3) | 7 (58.3) |
| HVR (n,
%) | 5 (41.7) | 5 (41.7) |
| NYHA
classification |
|
|
| Class II
(n, %) | 4 (33.3) | 4 (33.3) |
| Class III
(n, %) | 8 (66.7) | 8 (66.7) |
Effects of preprocedural esmolol
administration on outcomes related to surgical and perioperative
care of the enrolled patients
The two groups did not differ significantly in terms
of the characteristics of the surgery and CPB procedure (CPB time,
aortic cross-clamp time, surgical duration and quantity of
potassium cardioplegic solution used) (Table II). Furthermore, no significant
differences were detected between the two groups with respect to
the following parameters: Perioperative fluid infusion, urinary
volumes, usage of vasoactive medications during the surgery and
status of the heart rebeating. Similarly, no significant intergroup
differences were noted in the length of the ICU stay, decannulation
times and urinary volumes during the ICU stay (Table II).
 | Table II.Surgical and perioperative
care-related outcomes of patients in the esmolol and control
groups. |
Table II.
Surgical and perioperative
care-related outcomes of patients in the esmolol and control
groups.
| Outcomes | Esmolol group
(n=12) | Control group
(n=12) | P-value |
|---|
| Surgical
characteristics |
|
|
| CPB time,
min | 136.2±26.0 | 126.2±33.8 | 0.318 |
| Aortic
cross-clamp time, min | 96.7±23.5 | 94.8±30.1 | 0.424 |
| Surgery
duration, min | 317.9±77.5 | 302.1±66.1 | 0.298 |
| Potassium
cardioplegic solution, ml | 1729.8±147.8 | 1716.7±153.6 | 0.420 |
| Perioperative fluid
volumes |
|
|
|
| Total
fluid infusion, ml | 966.7±206.7 | 933.3±250.7 | 0.363 |
| Urinary
volume, ml | 1329.2±689.7 | 1208.3±520.4 | 0.316 |
| Medication
dosages |
|
|
|
|
Nitroglycerin, mg | 3.0±3.0 | 5.4±9.7 | 0.211 |
| Dopamine,
mg | 34.0±15.4 | 30.6±24.0 | 0.344 |
| Esmolol,
mg | 233.3±77.9 | 0 | – |
| Heart rebeating
status |
|
|
|
|
Spontaneous rebeating (n,
%) | 6 (50) | 6 (50) | 1.00 |
| Atrial
fibrillation (n, %) | 8 (66.7) | 7 (58.3) | 0.67 |
| Normal
ventricular rate (n, %) | 10 (83.3) | 11 (91.7) | 0.54 |
| Postoperative
care |
|
|
|
| Time to
decannulation, h | 22.4±17.2 | 30.7±22.6 | 0.188 |
| ICU
stay, h | 59.5±23.7 | 45.7±37.4 | 0.385 |
| Fluid
infusion within 20 h, ml | 3882.9±1104.1 | 4072.5±953.6 | 0.327 |
| Urinary
volume within 20 h, ml | 3350.1±1081.4 | 3041.3±609.5 | 0.199 |
Effects of preprocedural esmolol on
hemodynamic parameters during the perioperative period of the
patients included
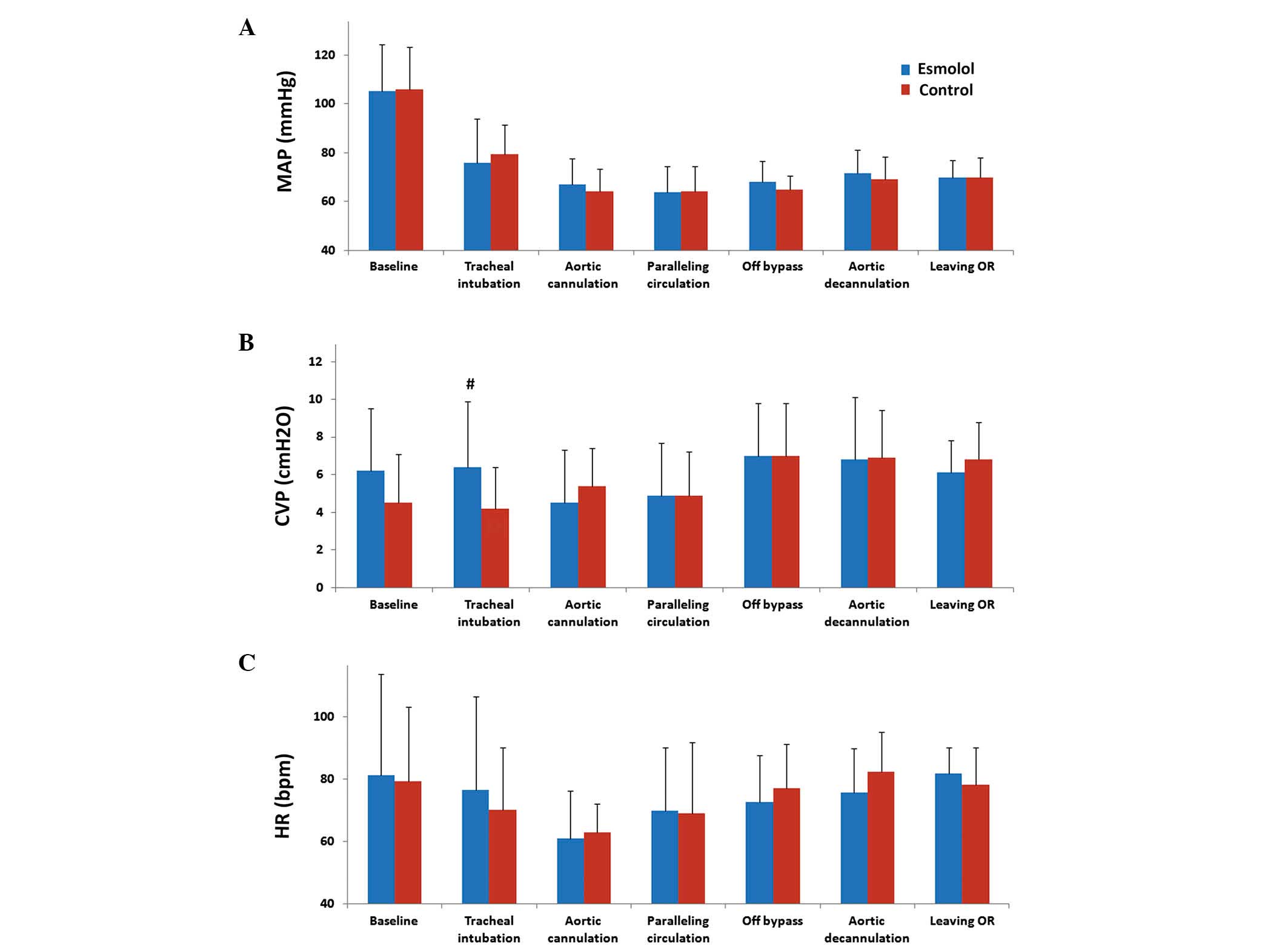
The mean MAP of the patients in both groups was
gradually reduced from the baseline levels (esmolol group,
105.4±18.9 mmHg; control group, 106.1±17.1 mmHg; P=0.464 between
groups), and remained at relatively low levels throughout the
surgical procedures (60–70 mmHg for both groups) (Fig. 1A). Furthermore, no significant
differences were noted between the two groups in the measurement of
MAP at the aforementioned 6 time points of assessment. Although CVP
(at the time of tracheal intubation) in the patients of the esmolol
group was found to be significantly greater than that in the
control group (6.4±3.5 vs. 4.2±2.2 cm H2O; P=0.039), the
values at the other time points did not show any significant
difference (Fig. 1B). Moreover, the
HR in the esmolol group appeared to be lower than that in the
control group at the majority of time-points, which may partially
reflect the potential negative chronotropic effects of esmolol;
however, these differences were not statistically significant
(Fig. 1C). These observations
suggest that preprocedural administration of esmolol did not induce
any significant changes in the levels of venous and arterial
hemodynamic parameters during the perioperative period in patients
who underwent elective cardiac surgery with CPB.
Effects of preprocedural
administration of esmolol on serum markers of myocardial injury in
patients undergoing on-pump cardiac surgeries
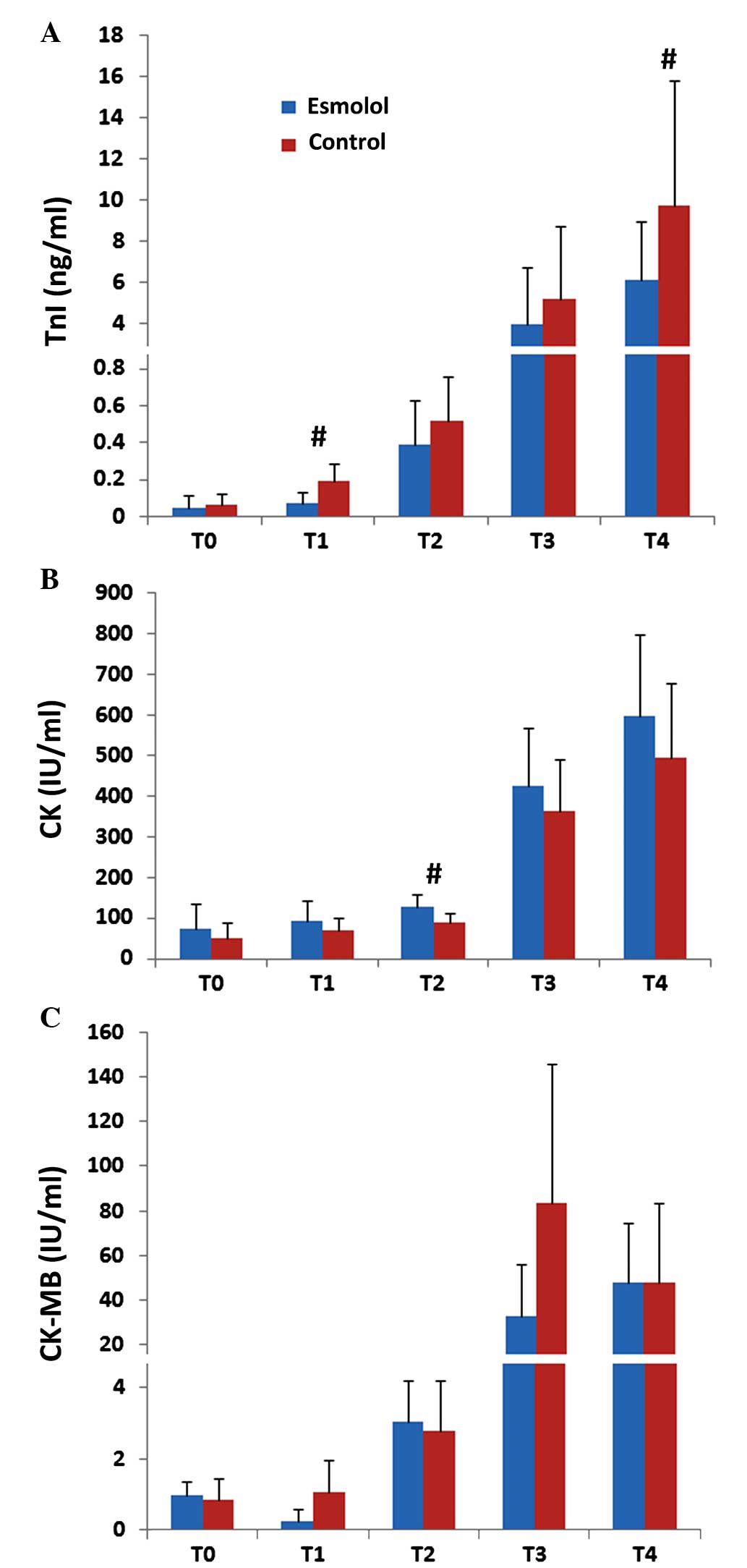
As shown in Fig. 2A,
the baseline levels of serum TnI did not differ significantly in
the two groups (esmolol group, 0.048±0.064 ng/ml; control group,
0.064±0.056 ng/ml; P=0.282). However, prior to aortic cannulation
(~30 min after esmolol administration) and at 120 min after the
release of the aortic cross-clamp, the serum TnI levels were
significantly lower in the esmolol group than in the control group
(esmolol group, 6.114±2.864 ng/ml and 0.072±0.058 ng/ml,
respectively; control group, 9.709±6.146 ng/ml and 0.188±0.094
ng/ml, respectively; P=0.039 and P<0.001, respectively).
Similarly, the TnI levels in the esmolol group were lower than
those in the control group at 30 min prior to the aortic
cross-clamp and at the time of release of the aortic cross-clamp,
although the difference was not significant (P=0.099 and P=0.163,
respectively). The serum levels of CK (Fig. 2B) did not show any significant
difference between the two groups at four of the five time points
(baseline, before aortic cannulation, before aortic cross-clamp and
120 min after the release of aortic cross-clamp); however, the
levels were significantly higher in the esmolol group compared with
the control group (esmolol group, 125.67±30.81 IU/ml; control
group, 89.67±23.31 IU/ml; P=0.002). With regard to the serum levels
of CK-MB, which is an isoenzyme considered to be more specifically
reflective of myocardial injury than CK, no significant intergroup
differences were detected (Fig.
2C).
Effects of preprocedural esmolol on
hemodynamic parameters during the first 12 postoperative hours in
ICU
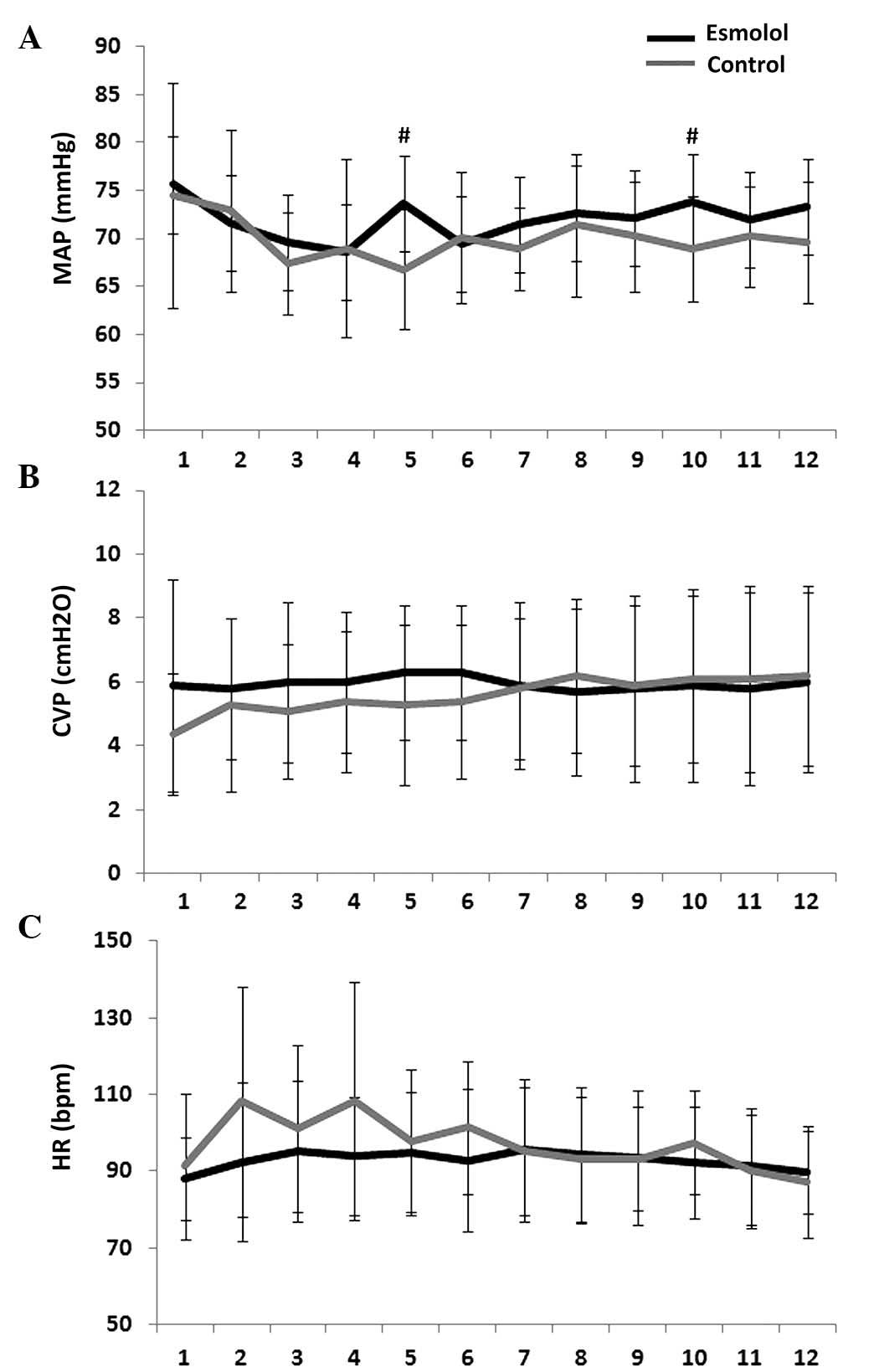
The dynamic changes in the MAP, CVP and HR in both
groups during the 12-h ICU follow-up period are presented in
Fig. 3A-C, respectively. The levels
of all three parameters were similar in the two groups, except for
significantly higher levels of MAP at the 5th and the 10th hour in
the esmolol group compared with the control group (P=0.026). This
indicates that the preprocedural administration of esmolol did not
have any significant effect on the postoperative hemodynamic
status.
Complications and adverse events
The incidences of the most common complications and
adverse events occurring in the two groups are provided in Table III. Postoperative pulmonary
infection was noted in two patients in the esmolol group and in
three patients in the control group. Furthermore, one patient in
the control group had neurological complications manifesting as
delayed postoperative recovery. No other instances of infection of
incision, pericardial tamponade, open-chest hemostasis or mortality
were recorded in the present study.
 | Table III.Incidences of complications and
adverse events of included patients in esmolol and control
group. |
Table III.
Incidences of complications and
adverse events of included patients in esmolol and control
group.
| Complications and
adverse events | Esmolol group
(n=12) | Control group
(n=12) |
|---|
| Neurological
complications (n) | 0 | 1 |
| Pulmonary infection
(n) | 2 | 3 |
| Infection of
incision (n) | 0 | 0 |
| Pericardial
tamponade (n) | 0 | 0 |
| Open-chest
hemostasis (n) | 0 | 0 |
| Death (n) | 0 | 0 |
Discussion
One of the most important observations of the
present randomized controlled trial on Chinese patients scheduled
for elective open-heart cardiac surgery under CPB was that esmolol
administration was able to maintain the HR within 80% of the
pre-bypass levels that resulted in a marked reduction in the serum
levels of a TnI-a specific marker of myocardial injury. In
addition, the results of the present study revealed that
preoperative esmolol administration did not induce any significant
changes of the hemodynamic parameters, including MAP, CVP and HR,
during the surgery and during the first 12 postoperative hours in
ICU. These results suggest that the preoperative administration of
esmolol may be an effective strategy for myocardial protection in
patients scheduled for elective cardiac surgery under CPB, without
increasing the risk of hemodynamic disorders. In addition,
administration of esmolol was not associated with increased risks
for severe complications and adverse events in these patients,
thereby indicating that this preventative strategy is safe.
Injury due to surgical maneuvers and
ischemia-reperfusion injury induced by CPB and hypothermia are
considered the most important mechanisms underlying the occurrence
of perioperative myocardial injury (7). The early phase of perioperative
myocardial ischemia is characterized by a lack of oxygen supply,
resulting in the upregulation of anaerobic metabolism in the
myocardium to cope with the anoxic environment. If the anoxic
condition is maintained for long, cellular dysfunction occurs as a
result of decreased adenosine 5′ phosphate supply and the resultant
changes in the internal environment homeostasis lead to structural
damage to cardiomyocytes. The damage to cardiomyocytes has been
attributed to several pathophysiological processes, including
oxidative stress (15),
overactivated inflammatory responses (16,17) and
calcium overload (18) in the plasma
of the cardiomyocytes. Therefore, interventional strategies
targeting these processes may help identify cardioprotective agents
that may be useful for administration during the procedures of CPB
and open-heart cardiac surgery. Although β-blockers are known to
lower the oxygen demand by eliciting an inotropic response
(19), they have been shown to have
numerous other potential cardioprotective actions (20). It has been suggested that the tonic
activation of the beta-adrenergic system associated with
proinflammatory and proapoptotic changes in the heart may be
alleviated by β-blockers (21).
Metoprolol, a regular β-blocker, has been demonstrated to cause a
reduction in oxidative stress and an increase in the antioxidant
activity in patients undergoing elective angioplasty, thereby
highlighting the antioxidative action of β-blockers (22). In addition, it has been reported that
propranolol, another commonly used β-blocker, is likely to exert
its protective effect on mitochondrial function in the ischemic
heart by attenuating the calcium overload in cardiomyocytes
(23). Therefore, the potential
protective action of perioperative β-blockers against myocardial
injury may be attributed to their widespread beneficial effects,
which may render them more effective than the other agents that
only influence limited aspects of the pathophysiological
process.
Consistent with our observations, early studies in
humans have provided evidence of the protective effect of
β-blockers against myocardial injury during CPB and open-heart
surgery. However, their use in cardiac surgery has been limited by
their potential negative inotropic effects and their unfavorable
effects on hemodynamics (24–26). To
overcome this problem, the ultra-short-acting β-blocker esmolol
appeared to be an attractive agent in the current settings, since
it is rapidly metabolized, and is expected to have little impact on
the hemodynamic parameters. The half-life of esmolol is ~2 min, the
time to peak effect is ~6–10 min after administration and the
washout time is 9 min after stopping the infusion (27). Due to these properties, this
β-blocker is the first-choice drug in critical patients in whom the
possible adverse effects of β-blockers, including cardiac failure,
hypotension and bradycardia, may necessitate immediate
discontinuation of the drug.
A number of pilot studies have explored the
potential benefits of esmolol in patients undergoing cardiac
surgeries. Deng et al (28)
reported that in a direct vision of an intracardiac beating-heart
surgery, esmolol protects the myocardium and facilitates the
operation, as demonstrated by the maintenance of the myocardial
ultrastructure. In addition, Scorsin et al (29) measured the transmyocardial gradient
of the oxygen content and revealed that esmolol provides potent
myocardial protection in hypertrophied hearts, at least partly, by
reducing the myocardial oxygen metabolism. In addition, a
meta-analysis revealed that esmolol reduces the incidence of
myocardial ischemia and arrhythmias when administered prior to
cardiac surgery, although it does cause an increase in bradycardia
(30). However, none of the above
studies have systematically analyzed the dynamic changes in the
levels of the markers of myocardial injury and hemodynamic
parameters and compared the levels of these markers prior to,
during and within the first number of hours following the
surgery.
The results of the present study indicated that the
preoperative administration of esmolol for the maintenance of the
HR within 80% of the baseline levels before CPB led to a
significant reduction in the serum TnI levels, without causing any
disturbances in the hemodynamic parameters at least for the first
12 postoperative hours. This reveals the cardioprotective effect of
the drug and suggests that the preoperative administration of
esmolol may be effective and safe for patients undergoing cardiac
surgery under CPB.
The observations of the present study should be
interpreted in the light of a number of limitations. Initially, it
is a pilot study that included only 24 patients from a single
medical center in China. The potential effects of perioperative
administration of esmolol on the clinical outcomes and adverse
events in this situation should be demonstrated in future studies.
In addition, due to the small sample size of the study population,
it is difficult to detect whether the benefits of esmolol were more
remarkable in certain subgroups of patients, such as those with
diabetes. The clinical applicability of the observations of the
present study need to be verified in a multi-center study
comprising a large number of patients. In addition, although TnI
has been established as a reliable marker of myocardial injury, the
potential benefits of esmolol on the myocardium should be verified
by other assessment criteria, including histopathological
examinations. In addition, the present study did not include any
blinding strategy, which may induce bias in the results. Finally,
the effects of esmolol on the perioperative levels of the markers
of myocardial injury and the changes in the hemodynamic parameters
for the first 12 postoperative hours were evaluated. The long-term
outcomes, such as the cardiac function and mortality data, need to
be addressed in future studies to further confirm the beneficial
effects of administering preoperative esmolol to patients.
In conclusion, the present study indicates that the
administration of esmolol prior to starting the surgical procedure
may be an effective and safe strategy for myocardial protection in
the case of patients undergoing elective cardiac surgery under CPB.
However, further studies on a larger sample population are required
in order to confirm the long-term beneficial effects of
preoperative administration of esmolol in such patients.
References
|
1
|
Biccard BM: Detection and management of
perioperative myocardial ischemia. Curr Opin Anaesthesiol.
27:336–343. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Beattie WS and Wijeysundera DN:
Perioperative cardiac biomarkers: The utility and timing. Curr Opin
Crit Care. 19:334–341. 2013.PubMed/NCBI
|
|
3
|
Bousselmi R, Lebbi MA and Ferjani M:
Myocardial ischemic conditioning: Physiological aspects and
clinical applications in cardiac surgery. J Saudi Heart Assoc.
26:93–100. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Salis S, Mazzanti VV, Merli G, Salvi L,
Tedesco CC, Veglia F and Sisillo E: Cardiopulmonary bypass duration
is an independent predictor of morbidity and mortality after
cardiac surgery. J Cardiothorac Vasc Anesth. 22:814–822. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ngaage DL, Cowen ME and Cale AR:
Cardiopulmonary bypass and left ventricular systolic dysfunction
impacts operative mortality differently in elderly and young
patients. Eur J Cardiothorac Surg. 35:235–240. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Salerno TA: Myocardial protection era:
From valve surgery to heart transplantation. Artif Organs.
36:939–942. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mentzer RM Jr: Myocardial protection in
heart surgery. J Cardiovasc Pharmacol Ther. 16:290–297. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ma J, Li XH, Yan ZX, Liu AJ, Zhang WK and
Yang LN: Effect of myocardial protection during beating heart
surgery with right sub-axiliary approach. Chin Med J (Engl).
122:150–152. 2009.PubMed/NCBI
|
|
9
|
Ji B and Liu J: Myocardial protection
during heart surgery in China. Chin Med J (Engl). 120:62–67.
2007.PubMed/NCBI
|
|
10
|
De Hert S and Moerman A: Myocardial injury
and protection related to cardiopulmonary bypass. Best Pract Res
Clin Anaesthesiol. 29:137–149. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chambers DJ and Fallouh HB: Cardioplegia
and cardiac surgery: Pharmacological arrest and cardioprotection
during global ischemia and reperfusion. Pharmacol Ther. 127:41–52.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bolsin S, Colson M and Marsiglio A:
Perioperative β blockade. BMJ. 347:f56402013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
McGory ML, Maggard MA and Ko CY: A
meta-analysis of perioperative beta blockade: What is the actual
risk reduction? Surgery. 138:171–179. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zaugg M, Lucchinetti E, Garcia C, Pasch T,
Spahn DR and Schaub MC: Anaesthetics and cardiac preconditioning.
Part II. Clinical implications. Br J Anaesth. 91:566–576. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ballester M, Llorens J,
Garcia-de-la-Asuncion J, Perez-Griera J, Tebar E, Martinez-Leon J,
Belda J and Juez M: Myocardial oxidative stress protection by
sevoflurane vs. propofol: A randomised controlled study in patients
undergoing off-pump coronary artery bypass graft surgery. Eur J
Anaesthesiol. 28:874–881. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Karuppasamy P, Chaubey S, Dew T, Musto R,
Sherwood R, Desai J, John L, Shah AM, Marber MS and Kunst G: Remote
intermittent ischemia before coronary artery bypass graft surgery:
A strategy to reduce injury and inflammation? Basic Res Cardiol.
106:511–519. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Steffens S, Montecucco F and Mach F: The
inflammatory response as a target to reduce myocardial ischaemia
and reperfusion injury. Thromb Haemost. 102:240–247.
2009.PubMed/NCBI
|
|
18
|
Gao Q, Hu J, Hu J, Yu Y, Ye H, Li Z and
Guan S: Calcium activated potassium channel and protein kinase C
participate in the cardiac protection of remote post conditioning.
Pak J Pharm Sci. 26:285–290. 2013.PubMed/NCBI
|
|
19
|
Kloner RA and Rezkalla SH: Cardiac
protection during acute myocardial infarction: Where do we stand in
2004? J Am Coll Cardiol. 44:276–286. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kloner RA and Rezkalla SH: Cardiac
protection during acute myocardial infarction: where do we stand in
2004? J Am Coll Cardiol. 44:276–286. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hu A, Jiao X, Gao E, Li Y, Sharifi-Azad S,
Grunwald Z, Ma XL and Sun JZ: Tonic beta-adrenergic drive provokes
proinflammatory and proapoptotic changes in aging mouse heart.
Rejuvenation Res. 11:215–226. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ciçek D, Tamer L, Pekdemir H, Cin VG,
Yildirim H, Kara AA and Yurtdaş M: Coronary angioplasty induced
oxidative stress and its relation with metoprolol use and plasma
homocysteine levels. Anadolu Kardiyol Derg. 6:308–313.
2006.PubMed/NCBI
|
|
23
|
Iwai T, Tanonaka K, Kasahara S, Inoue R
and Takeo S: Protective effect of propranolol on mitochondrial
function in the ischaemic heart. Br J Pharmacol. 136:472–480. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lucas SK, Magee PG, Flaherty JT, Gott VL
and Gardner TJ: Additive myocardial protection during ischemic
arrest with propranolol and potassium cardioplegia. Surg Forum.
30:257–260. 1979.PubMed/NCBI
|
|
25
|
Ruff ME, Karayannacos PE, Baba N, Kakos
GS, Vasko JS, Williams TE and Kilman JW: Protective effect of
beta-adrenergic blockade and hypothermia on myocardial
ultrastructure. J Surg Res. 29:430–440. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Miyazawa K, Fukuyama H, Komatsu E and
Yamaguchi I: Effects of propranolol on myocardial damage resulting
from coronary artery occlusion followed by reperfusion. Am Heart J.
111:519–524. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wiest D: Esmolol. A review of its
therapeutic efficacy and pharmacokinetic characteristics. Clin
Pharmacokinet. 28:190–202. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Deng YK, Wei F, Li ZL, Zhang DG and Yang
SY: Esmolol protects the myocardium and facilitates direct version
intracardiac operation with a beating heart. Circ J. 66:715–717.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Scorsin M, Mebazaa A, Al Attar N, Medini
B, Callebert J, Raffoul R, Ramadan R, Maillet JM, Ruffenach A,
Simoneau F, et al: Efficacy of esmolol as a myocardial protective
agent during continuous retrograde blood cardioplegia. J Thorac
Cardiovasc Surg. 125:1022–1029. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zangrillo A, Turi S, Crescenzi G, Oriani
A, Distaso F, Monaco F, Bignami E and Landoni G: Esmolol reduces
perioperative ischemia in cardiac surgery: A meta-analysis of
randomized controlled studies. J Cardiothorac Vasc Anesth.
23:625–632. 2009. View Article : Google Scholar : PubMed/NCBI
|