Introduction
Bacteria and their products are major etiologic
factors in pulpal and periapical pathosis (1,2). It has
also been shown that periapical inflammation does not occur in the
absence of microorganisms, regardless of the quality of the root
canal filling (3). Enterococci are
commensal microorganisms that are found in the mucosal tissues of
the oral cavity, gastrointestinal tract and genital tract in humans
(4). Enterococci are of clinical
importance since they are the third most common nosocomial
pathogens (5) and the cause of
refractory apical periodontitis (6).
They are often resistant to germicides and antiseptics as they can
persist under harsh conditions, such as high alkalinity, due to
their efficient use of proton pumps (7). To date, 12 enterococci species have
been identified, and ~90% of the Enterococcus clinical
isolates are of the Enterococcus faecalis species(8).
E. faecalis can survive various extreme
environmental conditions and for long periods of time under
nutritional deprivation. In addition, it has been shown to be
resistant to the calcium hydroxide treatment that is commonly used
in the course of endodontic therapy (9). Endodontic therapy mainly attempts to
eliminate bacteria from the root canal. The use of chemical
irrigation and mechanical instrumentation along with medication of
the root canal system between treatment sessions can significantly
reduce the population of bacteria inside the infected root canal
(10). However, eradication of all
bacteria from the root canal system is difficult (11,12).
Plasmas have been used for a number years for the
disinfection of medical equipment, implants, blood coagulation and
tooth bleaching (13–20). Chen et al reported that
He/O2 plasma more effectively killed E. faecalis
than pure He plasma (21). Recently,
our group designed a special low-temperature plasma device that
generates plasma plumes in open space (surrounding air), rather
than only in a confined discharge gap (22). This low-temperature plasma device has
been used in previous studies to efficiently kill E.
faecalis bacteria (19,20,22,23). The
aim of the present study was to assess the antimicrobial activity
of the plasma jet device with He flowing through 3% hydrogen
peroxide in root canals infected with E. faecalis.
Materials and methods
Experimental setup
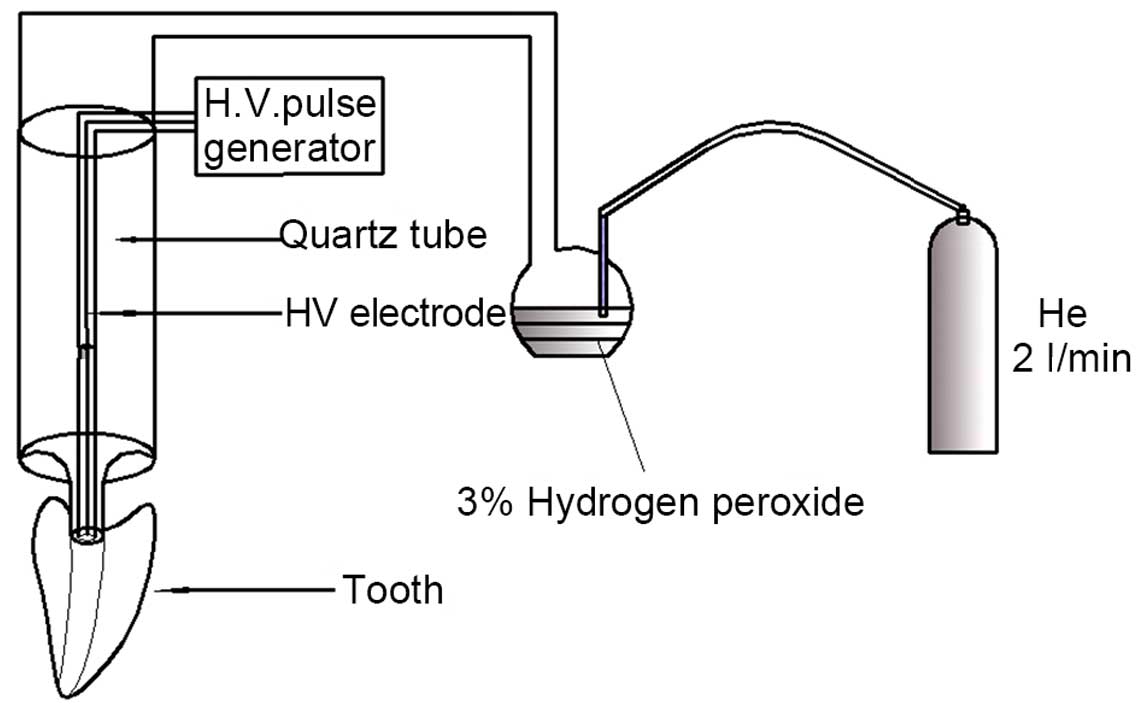
Fig. 1 shows the
plasma jet device with the working gas flowing through 3% hydrogen
peroxide, which is used in the treatment of a root canal infected
with E. faecalis. The inner diameter of the syringe nozzle
was ~1.0 mm. When the root canals were treated, the syringe nozzle
was vertically put on the root-canal orifice. The working gas used
in all the experiments was He with a flow rate of 2 l/min. All the
experiments in the present study used the same frequency of 8 kHz,
applied voltage of 8 kV and pulse width of 1,600 ns.
Microbial preparation. E.
faecalis
(ATCC 29212; American Type Culture Collection,
Manassas, VA, USA) were grown in Müller-Hinton (M-H) agar (Difco
Laboratories, Detroit, MI, USA), and incubated overnight at 37°C.
The microorganisms were then inoculated into a test tube containing
2 ml sterile physiological saline. The suspension was adjusted to a
turbidity of 6.0×108 colony forming units (CFU)/ml.
Subsequently, the same amount of brain heart infusion (BHI) broth
(Difco Laboratories) was added to the test tube. At this point, the
concentration of bacteria was 3.0×108 CFU/ml (equivalent
to 1.0 McFarland unit).
Preparation of teeth
The study protocol was reviewed and approved by the
Ethical Review Board of Investigation at the Tongji Hospital of
Huazhong University of Science and Technology (Wuhan, China).
Informed consent was obtained from the patients. A total of 42
extracted, human single-rooted anterior teeth with curvatures
between 0 and 10 degrees were obtained and stored in physiological
saline. The external root surface was cleaned with curettes to
remove periodontal soft tissues and calculus. All root canals were
prepared in a crown-down technique with K-file (Dentsply Maillefer,
Ballaigues, Switzerland) and ProTaper instruments (Dentsply
Maillefer) by an experienced endodontist and the size of ProTaper
files included sizes 10/15/SX/S1/S2/F1/F2 and F3. Next, the teeth
were placed in an ultrasonic bath in 17% ethylenediaminetetraacetic
acid for 5 min, followed by 5.25% sodium hypochlorite for a further
5 min in order to remove the smear layer. Root canals were then
rinsed with sterile water and placed in an ultrasonic cleaner for
20 min. Next, all teeth were autoclaved for 30 min at 121°C, and
parafilm was used to seal all the apical foramina of root canals. A
sterile micropipette was used to introduce 10 µl of the bacterial
suspension into each root canal, and root canal orifices were
sealed with parafilm. Subsequently, the teeth were incubated
aerobically at 37°C for 7 days. After 3.5 days of incubation, 10 µl
BHI broth was introduced into each root canal. Following the
incubation, the root canals were blotted dry with size 40 sterile
paper points.
The teeth were randomly divided into one control and
six experimental groups (6 teeth in each group), according to the
various times and methods of plasma sterilization. The groups were
as follows: Plasma jet sterilization with He flowing through 3%
hydrogen peroxide for 1 min (Group 1), 2 min (Group 2) or 4 min
(Group 3); plasma jet sterilization without He gas flowing through
3% hydrogen peroxide for 1 min (Group 4), 2 min (Group 5) or 4 min
(Group 6); and He gas flowing at 2 l/min for 4 min with the plasma
off (Group 7; control group).
After the treatment, an experienced endodontist used
a new sterile ProTaper file with size F3 to manually file the root
canal of each tooth, with each root canal filed 20 times. The
parafilm was removed from the root canal orifice, and the tooth and
debris in each file were irrigated with 1 ml sterile physiological
saline from the apical foramen to the root canal orifice.
Subsequently, the debris was collected in a test tube and agitated
with adding sterile physiological saline to 5 ml. Serial dilutions
(×10) of the samples were plated onto M-H agar and the plates were
incubated at 37°C for 48 h. The number of CFU/ml was then obtained
for each sample by an observer in a blinded manner.
Optical emission spectra
To identify the various reactive species generated,
the optical emission spectrum of plasma jet without or with He
flowing through 3% hydrogen peroxide is measured in the 200–1,100
nm wavelength range. A spectrometer (Acton SP-2500i; Princeton
Instruments, Acton, MA, USA) was used to measure the emission
spectra of the plasma jet with or without the He gas flowing
through 3% hydrogen peroxide.
Scanning electron microscopy
A total of 100 µl of the bacterial suspension were
seeded on two sterile cellulose nitrate membrane filters (Merck
Millipore, Billerica, CA, USA), which were placed in BHI broth and
incubated at 37°C for 72 h in an aerobic atmosphere. The
experimental group membrane was treated by plasma jet sterilization
with He gas flowing through 3% hydrogen peroxide at 2 l/min for 2
min. The control group membrane was treated with He gas flowing at
2 l/min for 4 min with the plasma off. Subsequently, the two
membranes were fixed with 2.5% glutaraldehyde, rinsed with
distilled water and dehydrated in a series of ethanol. The two
dried specimens were coated with gold and then observed under
scanning electron microscopy (JEOL JSM-6700F system; JEOL, Tokyo,
Japan).
Statistical analysis
Data are expressed as the mean ± standard deviation.
SPSS software, version 17.0 (SPSS, Inc., Chicago, IL, USA) was
used to analyze the data. Cell counts were logarithmically
converted prior to statistical comparison. Kruskal-Wallis test and
Mann-Whitney analysis were used to determine the differences in
bactericidal efficacy. Statistically significant differences among
the groups were considered at P-values of <0.01.
Results
Antibacterial effects of the plasma
jet with and without He flowing through 3% hydrogen peroxide
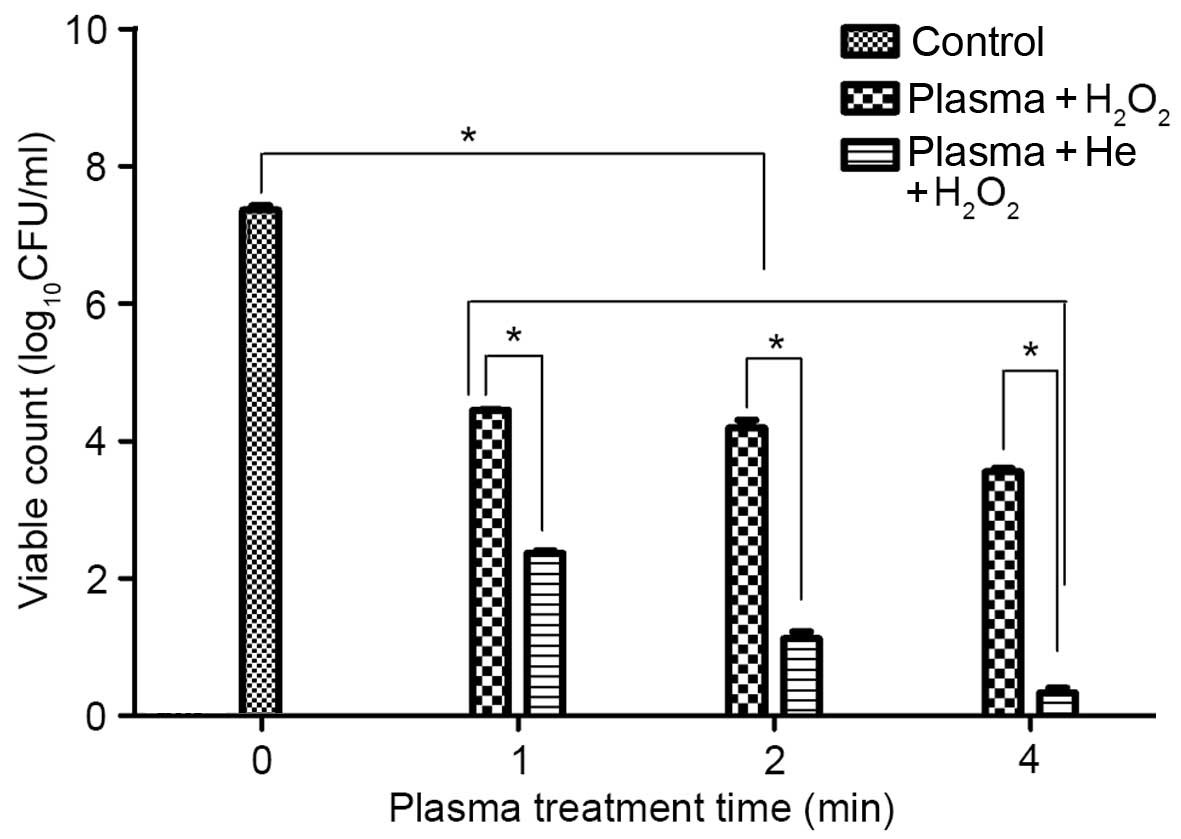
Fig. 2 demonstrates
the results of the antibacterial effects of the plasma jet with and
without He flowing through 3% hydrogen peroxide. Overall, the
viable count of E. faecalis was significantly decreased
(P=0.001) in all plasma treatment groups relative to the control
group. However, the antibacterial effects of the plasma jet with He
flowing through 3% hydrogen peroxide were better when compared with
the effect of the plasma jet without He. In addition, a longer
sterilization time resulted in improved bactericidal effects of the
treatment as observed by the decreased viable count of bacteria
after treatment for 4 min (Fig. 2).
The greatest reduction in CFU/ml was observed in Group 2 (plasma
jet with He for 2 min) and Group 3 (plasma jet with He for 4 min),
which presented a reduction by 6.237 and 7.027 log units,
respectively (Fig. 2). The reduction
in the bacterial count observed in Groups 1, 2 and 3 (treated by
plasma jet with He) was significantly greater compared with that in
Groups 4, 5 and 6, which were treated by plasma jet without He
(P<0.005). In addition, Group 3 showed a significant CFU/ml
reduction compared with Groups 1 and 2, which were treated by
plasma jet with He for a shorter time length (P=0.0015,
P=0.002).
Optical emission spectra of plasma jet
without or with He flowing through 3% hydrogen peroxide
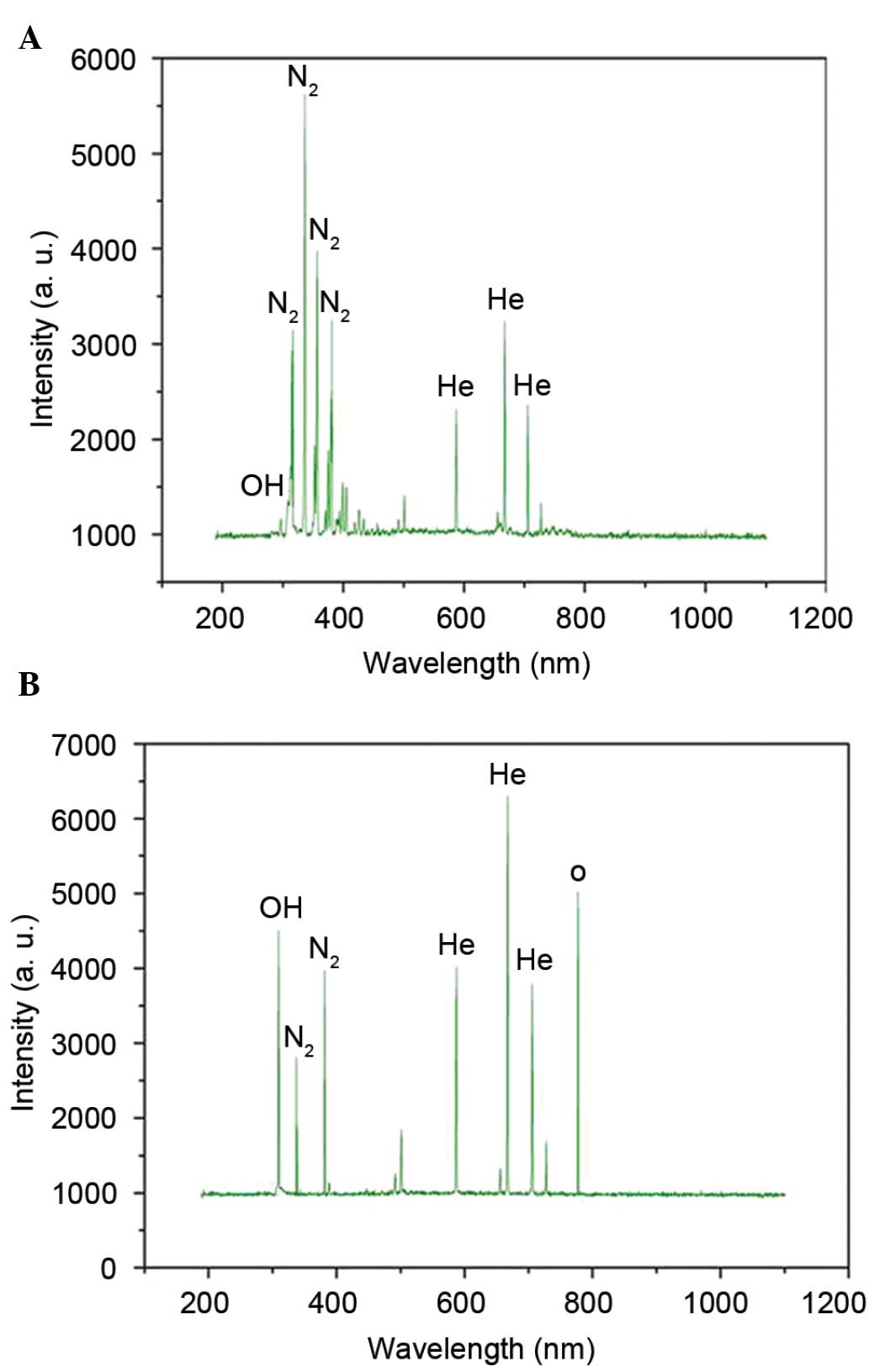
Fig. 3 demonstrates
the optical emission spectra of plasma jet without or with He
flowing through 3% hydrogen peroxide at wavelengths between 200 and
1,100 nm. The spectra indicated that plasma jet with He flowing
through 3% hydrogen peroxide presented stronger emission lines of
atomic oxygen (777.2 nm) and hydroxyl radical (309 nm) compared
with that in the plasma jet without He flowing through 3% hydrogen
peroxide (Fig. 3). The results
indicated that reactive species, including atomic oxygen and
hydroxyl radical, serve a dominant role in the plasma jet
sterilization, whereas N2 and He are not expected to
serve a significant direct role.
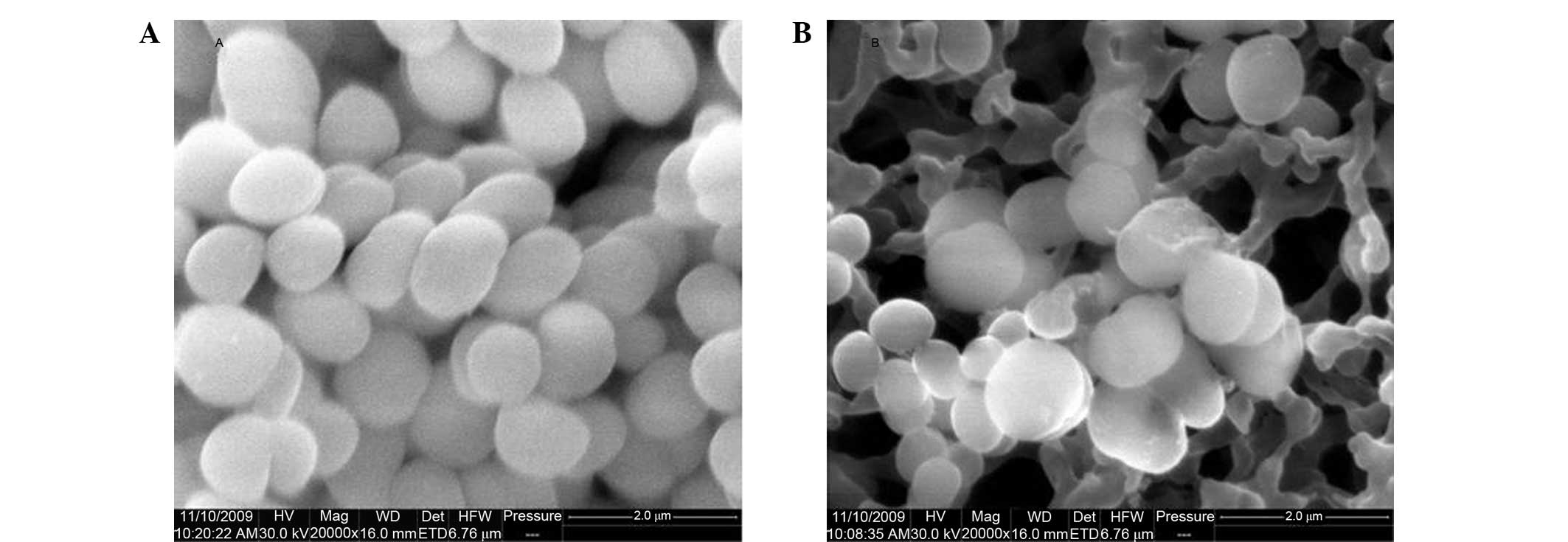
E. faecalis cells in Group 2 and the control
group were investigated by scanning electron microscopy. As shown
in Fig. 4, the images captured
following plasma jet treatment demonstrated reduced size, rupture
and death of E. faecalis cells, compared with the control
cells. The results of scanning electron microscopy clearly
explained the reduced viability of bacterial cells observed
following treatment by plasma jet with He flowing through 3%
hydrogen peroxide.
Discussion
E. faecalis was selected as the test
microorganism in the present study owing to its high frequency of
isolation from cases of failed endodontic treatment. E.
faecalis had been shown to have a high affinity for biofilm
formation, and bacteria in the biofilm form were up to 1,000-fold
more resistant to phagocytosis, antibodies and other antibiotics
compared with those in the planktonic form (24).
In the present study, Groups 3 and 2 treated by
plasma jet with He flowing through 3% hydrogen peroxide produced a
7.027 and 6.237 log reduction, respectively, in the bacterial CFU,
when compared with the control group. This result suggests that the
E. faecalis biofilms were eradicated in Groups 3 and 2. The
other experimental groups obtained reductions of at least 2.909 log
units. Therefore, the results in all groups were promising.
The bactericidal effect of the plasma jet with or
without He flowing through 3% hydrogen peroxide resulted mainly
from the atomic and molecular radicals. Reactive oxygen species
(ROS) are generally considered to serve a key role in the
bactericidal process. Short-time plasma treatment can induce DNA
fragmentation (25). The ROS are
able to penetrate the cells and, therefore, may induce high levels
of DNA damage, which then causes the induction of apoptosis
(26,27). Hydrogen peroxide is an oxidizing
agent that leads to microbial death by protein denaturation. It is
widely applied for disinfection processes in the food, water
treatment, healthcare and contact lens industries (28). Hydrogen peroxide decomposition and
the recombination of radicals can lead to the formation of
molecular oxygen, atomic oxygen and hydroxyl radical (29,30). In
the present study, stronger emission lines of atomic oxygen and
hydroxyl radical were detected in the plasma jet with He flowing
through 3% hydrogen peroxide using a spectrometer, when compared
with plasma jet without He flowing through 3% hydrogen peroxide.
The atomic oxygen and hydroxyl radical are considered to be
responsible for the improved antibacterial effects of the plasma
jet with He flowing through 3% hydrogen peroxide when compared with
the plasma jet without He. The results indicate that reactive
species, including atomic oxygen and hydroxyl radical, serve a
dominant role in the plasma jet sterilization, whereas
N2 and He are not expected to serve a significant direct
role, and these findings are consistent with the results of a
previous study (31).
In the current study, the UV intensity emitted by
the plasma jet with or without the working gas flowing through 3%
hydrogen peroxide was detected, and it was found that the UV
intensity was approximately 0.05–0.1 mW/cm2. Therefore,
the UV radiation served a minor role in the sterilization of the
bacteria (19,32). Heat was not responsible for the
bactericidal effect, since the plasma jet with or without the
working gas flowing through 3% hydrogen peroxide was at room
temperature. Scanning electron microscopy was also used in the
present study to reveal damage to E. faecalis by plasma jet
with He flowing through 3% hydrogen peroxide. The obtained images
of E. faecalis cells demonstrated reduction in size, rupture
and death, when compared with the normal cells.
Single-rooted anterior teeth with curvatures between
0 and 10 degrees used in the present study were easily standardized
to exclude interference of the dental anatomic complexity. Thus,
further studies should examine the sterilizing effect of the plasma
jet with He flowing through 3% hydrogen peroxide in complexity root
canal systems.
In conclusion, the results of the present study
suggested that the antibacterial effects of the plasma jet with He
flowing through 3% hydrogen peroxide were better compared with the
antibacterial effects of the plasma jet without He flowing through
3% hydrogen peroxide. The atomic oxygen and hydroxyl radical were
considered to be responsible for the improved antibacterial effects
of the plasma jet with He when compared with the plasma jet without
He. The results also suggested that the plasma jet device with or
without He flowing through 3% hydrogen peroxide is a valuable tool
for root canal disinfection of E. faecalis, and that plasma
treatment could be considered as an alternative method for root
canal disinfection of E. faecalis in endodontic
treatments.
Acknowledgements
The present study was supported by a grant from the
Natural Science Foundation of China (grant no. 10875048).
References
|
1
|
Kakehashi S, Stanley HR and Fitzgerald RJ:
The effects of surgical exposures of dental pulps in germ-free and
conventional laboratory rats. Oral Surg Oral Med Oral Pathol.
20:340–349. 1965. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Möller AJ, Fabricius L, Dahlén G, Ohman AE
and Heyden G: Influence on periapical tissues of indigenous oral
bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res.
89:475–484. 1981.PubMed/NCBI
|
|
3
|
Fabricius L, Dahlén G, Sundqvist G,
Happonen RP and Möller AJ: Influence of residual bacteria on
periapical tissue healing after chemomechanical treatment and root
filling of experimentally infected monkey teeth. Eur J Oral Sci.
114:278–285. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Walter J: Ecological role of lactobacilli
in the gastrointestinal tract: Implications for fundamental and
biomedical research. Appl Environ Microbiol. 74:4985–4996. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wisplinghoff H, Seifert H, Tallent SM,
Bischoff T, Wenzel RP and Edmond MB: Nosocomial bloodstream
infections in pediatric patients in United States hospitals:
Epidemiology, clinical features and susceptibilities. Pediatr
Infect Dis J. 22:686–691. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hancock HH III, Sigurdsson A, Trope M and
Moiseiwitsch J: Bacteria isolated after unsuccessful endodontic
treatment in a North American population. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 91:579–586. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Evans M, Davies JK, Sundqvist G and Figdor
D: Mechanisms involved in the resistance of Enterococcus faecalis
to calcium hydroxide. Int Endod J. 35:221–228. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gordon S, Swenson JM, Hill BC, Pigott NE,
Facklam RR, Cooksey RC, Thornsberry C, Jarvis WR and Tenover FC:
Antimicrobial susceptibility patterns of common and unusual species
of enterococci causing infections in the United States.
Enterococcal Study Group. J Clin Microbiol. 30:2373–2378.
1992.PubMed/NCBI
|
|
9
|
Haapasalo M and Orstavik D: In vitro
infection and disinfection of dentinal tubules. J Dent Res.
66:1375–1379. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Siqueira JF Jr, Rôças IN, Favieri A and
Lima KC: Chemomechanical reduction of the bacterial population in
the root canal after instrumentation and irrigation with 1%, 2.5%,
and 5.25% sodium hypochlorite. J Endod. 26:331–334. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nair PN, Henry S, Cano V and Vera J:
Microbial status of apical root canal system of human mandibular
first molars with primary apical periodontitis after ‘one-visit’
endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 99:231–252. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sjögren U, Figdor D, Persson S and
Sundqvist G: Influence of infection at the time of root filling on
the outcome of endodontic treatment of teeth with apical
periodontitis. Int Endod J. 30:297–306. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sladek REJ, Stoffels E, Walraven R,
Tielbeek PJA and Koolhoven RA: Plasma treatment of dental cavities:
A feasibility study. IEEE Trans Plasma Sci. 32:1540–1543. 2004.
View Article : Google Scholar
|
|
14
|
Sladek REJ and Stoffels E: Deactivation of
Escherichia coli by the plasma needle. J Phys D: Appl Phys.
38:1717–1721. 2005. View Article : Google Scholar
|
|
15
|
Stoffels E, Kieft IE and Sladek REJ:
Superficial treatment of mammalian cells using plasma needle. J
Phys D: Appl Phys. 36:2908–2913. 2003. View Article : Google Scholar
|
|
16
|
Fridman G, Friedman G, Gutsol A, Shekhter
AB, Vasilets VN and Fridman A: Applied plasma medicine. Plasma
Process Polym. 5:503–533. 2008. View Article : Google Scholar
|
|
17
|
Sun P, Pan J, Tian Y, Bai N, Wu H, Wang L,
Yu C, Zhang J, Zhu W, Becker K and Fang J: Tooth whitening with
hydrogen peroxide assisted by a direct-current cold
atmospheric-pressure air plasma microjet. IEEE Trans Plasma Sci.
38:1892–1896. 2010. View Article : Google Scholar
|
|
18
|
Lee HW, Nam SH, Mohamed AAH, Kim GC and
Lee JK: Atmospheric pressure plasma jet composed of three
electrodes: Application to tooth bleaching. Plasma Process Polym.
7:274–280. 2010. View Article : Google Scholar
|
|
19
|
Zhou X, Xiong Z, Cao Y, Lu X and Liu D:
The antimicrobial activity of an atmospheric-pressure
room-temperature plasma in a simulated root-canal model infected
with Enterococcus faecalis. IEEE Trans Plasma Sci. 38:3370–3374.
2010. View Article : Google Scholar
|
|
20
|
Cao Y, Yang P, Lu X, Xiong Z, Ye T, Xiong
Q and Sun Z: Efficacy of atmospheric pressure plasma as an
antibacterial agent against Enterococcus faecalis in vitro. Plasma
Sci Tech. 13:932011. View Article : Google Scholar
|
|
21
|
Chen W, Huang J, Du N, Liu XD, Wang XQ, Lv
GH, Zhang GP, Guo LH and Yang SZ: Treatment of Enterococcus
faecalis bacteria by a helium atmospheric cold plasma brush with
oxygen addition. J Appl Phys. 112:0133042012. View Article : Google Scholar
|
|
22
|
Lu X, Xiong Z, Zhao F, Xiam Y, Xiong Q,
Gong W, Zhou C, Jiang Z and Pan Y: A simple atmospheric pressure
room-temperature air plasma needle device for biomedical
applications. Appl Phys Lett. 95:1815012009. View Article : Google Scholar
|
|
23
|
Lu X, Cao Y, Yang P, Xiong Q, Xiong Z,
Xian Y and Pan Y: An RC plasma device for sterilization of root
canal of teeth. IEEE Trans Plasma Sci. 37:668–673. 2009. View Article : Google Scholar
|
|
24
|
Distel JW, Hatton JF and Gillespie MJ:
Biofilm formation in medicated root canals. J Endod. 28:689–693.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kim GJ, Kim W, Kim KT and Lee JK: DNA
damage and mitochondria dysfunction in cell apoptosis induced by
nonthermal air plasma. Appl Phys Lett. 96:0215022010. View Article : Google Scholar
|
|
26
|
Buttke TM and Sandstrom PA: Oxidative
stress as a mediator of apoptosis. Immunol Today. 15:7–10. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Simon HU, Haj-Yehia A and Levi-Schaffer F:
Role of reactive oxygen species (ROS) in apoptosis induction.
Apoptosis. 5:415–418. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Heaselgrave W, Andrew PW and Kilvington S:
Acidified nitrite enhances hydrogen peroxide disinfection of
Acanthamoeba, bacteria and fungi. J Antimicrob Chemother.
65:1207–1214. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Soloshenko IA, Tsiolko VV, Khomich VA,
Bazhenov VY, Ryabtsev A, Schedrin AI and Mikhno IL: Features of
sterilization using low-pressure DC-discharge hydrogen-peroxide
plasma. IEEE Trans Plasma Sci. 30:1440–1444. 2002. View Article : Google Scholar
|
|
30
|
Locke BR and Shih KY: Review of the
methods to form hydrogen peroxide in electrical discharge plasma
with liquid water. Plasma Sources Sci Technol. 20:34006–34020,
(34015). 2011. View Article : Google Scholar
|
|
31
|
Wang D, Zhao D, Feng K, Zhang X, Liu D and
Yang S: The cold and atmospheric-pressure air surface barrier
discharge plasma for large-area sterilization applications. Appl
Phys Lett. 98:1615012011. View Article : Google Scholar
|
|
32
|
Lu X, Ye T, Cao Y, Sun Z, Xiong Q, Tang Z,
Xiong Z, Hu J, Jiang Z and Pan Y: The roles of the various plasma
agents in the inactivation of bacteria. J Appl Phys.
104:0533092008. View Article : Google Scholar
|