Introduction
Acute hypoxic respiratory failure (AHRF) in children
is a common and critical illness that occurs in the pediatric
intensive care unit (PICU). It mostly progresses to acute
respiratory distress syndrome (ARDS) and is a common cause of death
in the PICU. In PICUs of China, the occurrence rate of AHRF is 4%,
and the mortality rate is 41.8%. The occurrence rate of ARDS is
1.44–2.7% and the mortality rate is 46.4–60.3% (1,2). In
PICUs in other countries, the occurrence rate of ARDS is 0.7–4.2%
and the mortality rate is 20–75% (3–6). Owing
to the gradual wide application of respiratory support and
intensive care technologies, a large number of fatal cases have
survived, with a mortality rate of <1.6% (7). Non-invasive ventilation via mechanical
ventilation improves gas exchange and establishes a good
environment for reducing the occurrence of low blood oxygen in
patients with acute respiratory failure (8). However, the relatively complex
multiple-organ dysfunctions caused by various unexpected, rare, and
complicated respiratory infections, and large differences among
nationwide developmental levels of respiratory support technologies
caused by unequal levels of economic and medical development, have
limited the spread of the use of respiratory support and intensive
care technologies in children with AHRF (9).
After the cooperative studies from our center on
children with ARDS and AHFR in 2004 and from 2005 to 2006, the
clinical epidemiological characteristics of ARDS and AHRF in
domestic PICUs have changed (10).
Therefore, assisted research on respiratory support for children
with AHRF was conducted in 2010, and children with AHRF among 30
hospitals across various regions of China were selected to perform
a prospective multicenter epidemiological study. The prognosis
associated with treatment with respiratory support in different
regions and different PICUs of hospitals with different mechanical
ventilation strategies were analyzed and compared in this
study.
Materials and methods
Research design
Before beginning the study, the person in charge and
PICU-related hospital staff of each cooperation unit participated
in professional training. Patient data were recorded and counted by
specially designated personnel of each cooperation unit. PICU basic
data forms were completed by those responsible and transferred
through electronic mail, telephone, physical mail, or through a
dedicated website established by the cooperation groups to the
coordination center (Department of Respiratory and Critical Care
Laboratory, Department of Pediatric Hospital, Fudan University,
Shanghai, China), and were then entered in the database of the
coordination center for analysis. Since most of the collaboration
units participated in the collaborative study on AHRF in 2006, they
were relatively familiar with the research data. Therefore, they
mainly solved problems that occurred in everyday contact and
monthly data collection process, as well as stage summary.
This was a descriptive and prospective multicenter
clinical epidemiological study. The study period was from 1 June,
2010 to 31 May, 2011, lasting 12 consecutive months. PICUs of 30
hospitals in China were enrolled including the original national
children AHRF collaboration group. Sixteen of these were
university-affiliated hospitals and the remaining 14 were
non-affiliated. Simultaneously, in accordance with the per capita
gross national product (GNP) rankings and the rankings of per
capita income of urban residents of the provinces and cities that
each unit belonged to, the first 15 hospitals were ranked as
hospitals in economically developed regions, while the remaining 15
were in less developed regions.
Case selection and data
collection
Children aged from 29 days to 6 years who were
admitted to the PICU and in accordance with AHRF diagnostic
criteria were included in the current study. To reduce the
selection bias of the data of children with critical illnesses
admitted to different hospitals and in different periods of each
hospital, and to ensure the uniformity of admission standards, the
pediatric critical illness scoring system, as well as American
guidelines for admission (11) and
discharge policies for PICUs (12)
were used for the research group as the criteria for critically ill
patients.
Diagnostic criteria
Diagnostic criteria for respiratory failure were
(13): Acute onset (≤2 weeks);
pressure of artery O2 (PaO2) ≤50 mmHg or
PaO2/fraction of inspired O2
(FiO2) ≤50 mmHg; mechanical ventilation via tracheal
intubation [FiO2 ≥30%, positive end-expiratory pressure
(PEEP) ≥2 cm H2Ο] can maintain PaO2 ≥60 mmHg,
or percutaneous pulse oxygen saturation (SpO2) ≥90% for
>12 h, and respiratory failure exists after 12 h of ventilation;
PaO2/FiO2 ≤250 mmHg; at the same time, acute
ventilatory dysfunction induced respiratory failure caused by the
central nervous system or neuromuscular diseases as well as heart
diseases should be excluded.
For the diagnosis of acute lung injury (ALI)/ARDS,
the criteria formulated by the American-European Consensus
Conference (AECC) in 1994 was used (14): i) Acute onset (≤2 weeks); ii)
PaΟ2/FiΟ2 ≤300 mmHg (ALI) or
PaΟ2/FiO2 ≤200 mmHg (ARDS); iii) exudation
shadows in both lungs are shown on chest radiograph; and iv) no
clinical evidence of left atrial hypertension (pulmonary arterial
wedge pressure ≤18 mmHg or diagnosis by portable color Doppler
ultrasound).
Statistical analysis
Patient data were entered in the computer to
establish a Microsoft Access database. SPSS 13.0 statistical
software (SPSS, Inc., Chicago, IL, USA) was used for statistical
analysis. The continuous variables with normal distribution in
measurement data were presented as mean ± SD, and mean values were
compared by one-way analysis of variance (ANOVA). Partial
distributors were expressed as medians and quartiles (P25 and P75),
and the mean values were compared using the Wilcoxon test.
Non-continuous variables or categorical data, which included
ratios, were compared with the Chi-square test.
Results
General conditions in the PICU
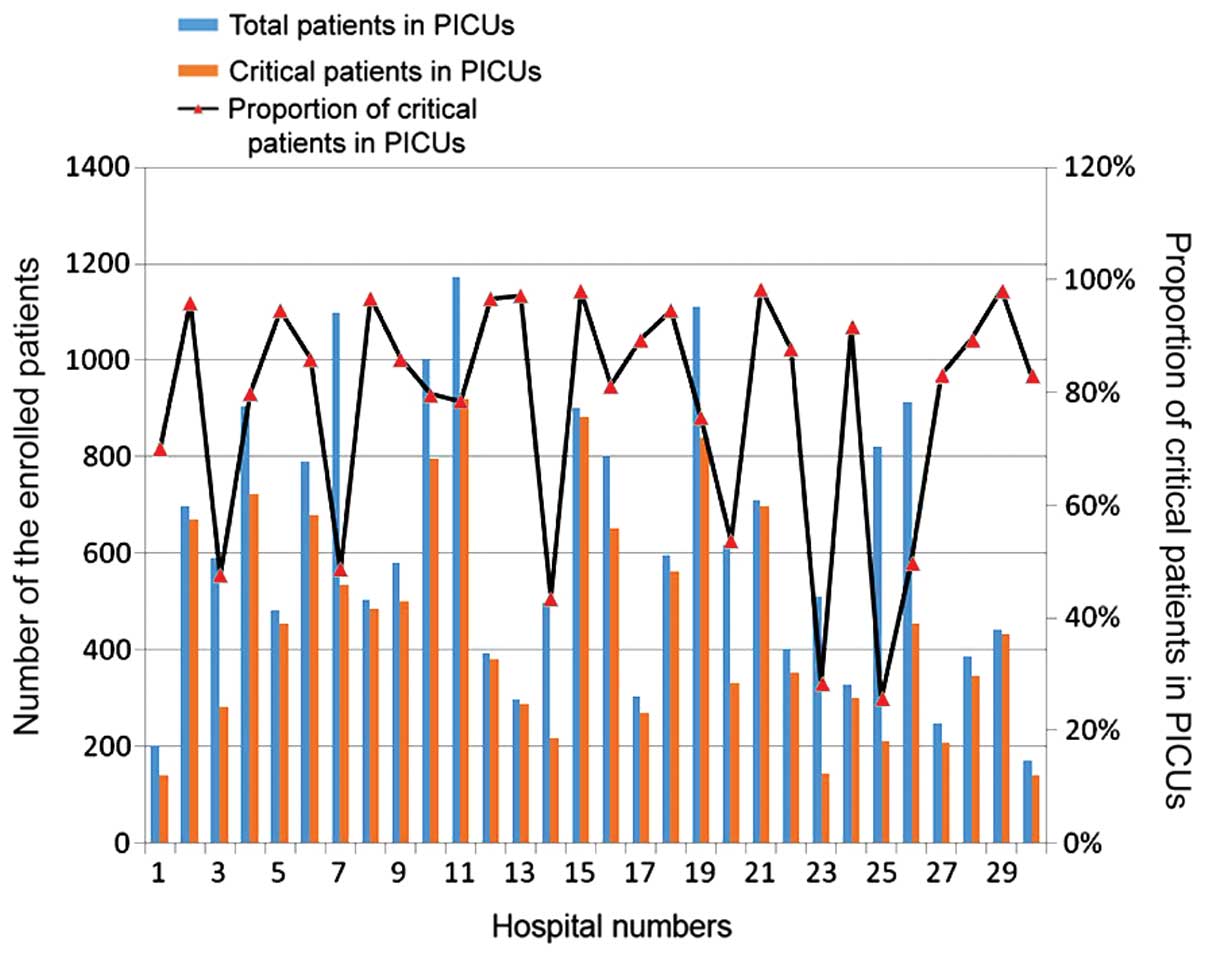
During the 12-month study period, 18,648 cases were
admitted among the 30 PICUs, and 13,906 cases were critical (75.3%,
13,906/18,468), including 8,149 cases with pediatric critical
illness scores ≤90 (58.6%, 8,179/13,906) and 5,757 cases with
scores >90 but were in accordance with the criteria of American
discharge policies for PICUs (41.4%, 5,757/13,906). The median
value of the proportion of critical patients was 77.6% (22.6–88.7%)
(Fig. 1). The number of dead
patients with critical illness was 1,436 for the whole year
(including 583 cases that died within 3 days after discharge from
the hospital), the annual average mortality rate from PICUs was
10.3% (1,436/13,906), the number of patients who gave-up treatment
and discharged from the hospital was 1,826 including those who died
within three days after discharging automatically from the
hospital, and the rate of abandonment from the study was 13.1%.
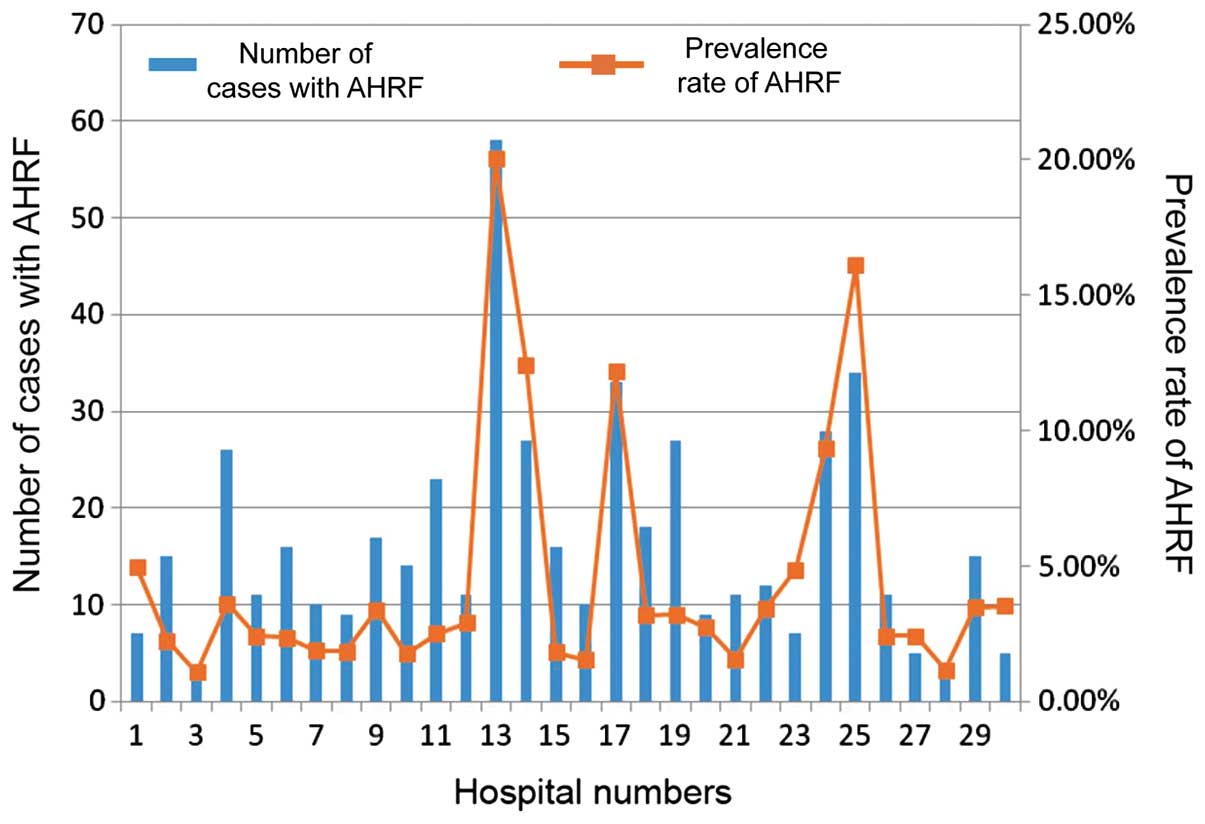
A total of 560 cases from 30 PICUs conforming to the
diagnostic criteria of AHRF were enrolled and 68 cases were
eventually removed. Therefore, a total of 492 cases with AHRF were
included. All the cases were treated with mechanical ventilation
via tracheal intubation. The total prevalence rate of AHRF was
3.54% (492/13,906), the median value of the prevalence rate in each
PICU was 4.54%, with the lowest value of 1.07% and the highest
value of 20.1% (Fig. 2). The total
mortality rate of patients with AHRF was 26.6% (131/492), the
mortality rates of each unit were unequal and differed greatly, and
the median value was 31.7%. Among 492 cases with AHRF, 286 were
female (58.1%), and the ratio of males-to-females was 1.4:1. The
average age of all children was 1.3 years, and the median age was
0.8 years (0.3–2.4). Children younger than 1 year accounted for
57.1% (42.9 cases), and others younger than 2 years accounted for
66.7% (328 cases) (Table I).
 | Table I.The basic conditions and respiratory
parameters of included patients with AHRF. |
Table I.
The basic conditions and respiratory
parameters of included patients with AHRF.
| Parameters | Data |
|---|
| Age (years) | 0.8 (0.3–2.4) |
| <1
year | 281 (57.1) |
| ≥1
year | 211 (42.9) |
| <2
years | 328 (66.7) |
| ≥2
years | 164 (33.3) |
| Female | 286 (58.1) |
| PEEP, cm
H2Ο | 5 (36) |
| PIP, cm
H2Ο | 20 (16–24) |
| MAP, cm
H2Ο |
|
| MAP, cm
H2Ο | 12 (10–14) |
|
PaΟ2/FiΟ2 | 138 (106–192) |
| OI | 8.4 (106–187) |
Comparisons of prevalence rates,
mortality rates, and disease burden of AHRF in hospitals of
different areas and different grades
The per capita gross domestic product (GDP) of
provinces and cities of the 15 hospitals in economically developed
areas was 56,152 yuan, the per capita disposable income of urban
residents was 22,346 yuan, and the per capita income of rural
residents was 8,674 yuan. The per capita GDP of residents in
economically less developed areas was 22,330 yuan, which was half
of the average value of the economically developed areas; the per
capita disposable income of urban residents was 15,689 yuan, which
was ~2/3 of the average of developed areas; and there were 6 less
university-affiliated hospitals in less developed areas than in
developed areas in this study.
Regarding economic burdens, the ratio of average
cost associated with AHRF in hospital and the annual income of
urban residents in developed areas was 1.05 (23,687/22,364), and
was 2.6 when it comes to the rural residents (23,687/8,674), while
the ratio in less developed areas was 1.50 (23,461/15,689) of urban
residents and 4.97 (23,461/4,723) of rural residents (Table II). Therefore, according to the
incomes of patients' family in different areas, although the
critical degrees of admitted patients in developed areas were
higher, the total medical costs between them differed
insignificantly (P>0.05). By contrast, the disease burdens of
patients in developed areas were lighter.
 | Table II.The per capita GDP and per capita
income of residents in hospitals of different areas and different
grades. |
Table II.
The per capita GDP and per capita
income of residents in hospitals of different areas and different
grades.
| Hospitals | Per capita GDP
(Yuan) | Per capita income of
rural residents (Yuan) | Per capita income of
urban residents (Yuan) |
|---|
| Hospitals in
developed areas | 6,152 | 8,674 | 22,364 |
| Hospitals in less
developed areas | 22,330 | 4,723 | 15,689 |
| University-affiliated
hospitals | 35,189 | 6,020 | 15,900 |
| Non-affiliated
hospitals | 20,561 | 3,678 | 15,670 |
| AHRF costs | 23,687 | 23,461 | 25,123 |
Our analysis revealed the incidence of AHRF and ARDS
in hospitals in less developed areas was higher than that in
developed areas, which was also the case for the mortality rates,
albeit the mortality rate was not statistically significant
(P>0.05). Similarly, the incidence of AHRF and ARDS in the
non-university-affiliated hospitals was lower than that in
university-affiliated hospitals, while the mortality rates were
higher than those of the latter, with no statistically significant
differences (P>0.05). The rate of giving-up in
university-affiliated hospitals was 16.9%, which was lower than
that of non-university-affiliated hospitals which was 21.4%, and
there was no statistically significant difference (P>0.05)
(Table III).
 | Table III.Comparison of AHRF and ARDS in
hospitals of different areas and different grades. |
Table III.
Comparison of AHRF and ARDS in
hospitals of different areas and different grades.
| Rates | Developed areas | Less developed
areas | University-affiliated
hospitals | Non-affiliated
hospitals |
|---|
| Occurrence rate of
AHRF, % (n) | 3.1 (188) | 3.8 (304) | 3.2 (227) | 3.9 (265) |
| Occurrence rate of
ARDS, % (n) | 1.9 (112) | 3.4 (272) | 2.4 (169) | 3.3 (225) |
| Mortality rate of
AHRF, % (n) | 28.4 (42) | 32.6 (99) | 23.8
(54)a | 29.1 (77) |
| Mortality rate of
ARDS, % (n) | 25.6 (29) | 32.0 (87) | 27.2 (46) | 30.7 (69) |
| Abandonment rate of
AHRF, % (n) | 16.9 (24) | 21.4 (65) | 19.8
(45)b | 24.9 (66) |
Comparisons of respiratory support
therapy in different hospitals and regions
The proportion of use of mechanical ventilation for
critical cases in developed areas was 26.5%, which was <30.5% in
the less developed areas, and the proportion of use of mechanical
ventilation in university-affiliated hospitals was 38.4%, which was
significantly higher than that of 18.7% in non-affiliated hospitals
(Table IV). From the comparison of
specific respiratory parameters, it was found that LIS of patients
admitted to university-affiliated hospitals and hospitals in
developed areas was higher and the ratio of
PaΟ2/FiΟ2 was relatively lower. In addition,
oxygenation index of patients in university-affiliated hospitals
was higher than that of non-affiliated hospitals, which indicated
the critical degree was higher. Comparing specific respiratory
parameters, PEEP, peak inspiratory pressure (PIP), and MAP, which
were measured in patients of university-affiliated hospitals, were
higher than those in non-affiliated hospitals, but the differences
were not statistically significant (P>0.05). Similarly,
expiratory tidal volume (Vte) and mean airway pressure (MAP) of
hospitals in the developed areas were slightly higher than those of
hospitals in less developed areas, and the differences were not
statistically significant. The trends of PEEP and PIP were in
contrast with those in university-affiliated hospitals and
non-university-affiliated hospitals (Tables V and VI).
 | Table IV.Comparisons of total PICU data in
different regions and different hospitals. |
Table IV.
Comparisons of total PICU data in
different regions and different hospitals.
| Data | Developed areas | Less developed
areas | University-affiliated
hospitals | Non-affiliated
hospitals |
|---|
| Critical cases, %
(n) | 82.3 (5,917) | 75.6 (7,989) | 88.3 (7,115) | 72.5 (6,791) |
| Mortality rate, %
(n) | 9.5 (543) | 10.1 (893) | 10.3 (734) | 9.1 (702) |
| Rate of
abandonment, % (n) | 12.2 (581) | 16.8 (1,245) | 11.5 (786) | 17.2 (1,040) |
| Mechanical
ventilation, % (n) | 26.5 (1,568) | 30.5 (2,436) | 38.4 (2,732) | 18.7 (1,272) |
 | Table V.Comparison of mechanical ventilation
parameters on the first, third and seventh day after admission of
patients to hospitals of economically developed and underdeveloped
areas. |
Table V.
Comparison of mechanical ventilation
parameters on the first, third and seventh day after admission of
patients to hospitals of economically developed and underdeveloped
areas.
|
| Day 1 | Day 3 | Day 7 |
|---|
|
|
|
|
|
|---|
| Parameters | DH | UH | DH | UH | DH | UH |
|---|
|
FiO2 | 46.2 (19) | 44.8 (14) | 39 (14) | 39.2 (14) | 39 (24) | 39.2 (9) |
| No. of cases | 214 | 161 | 143 | 99 | 67 | 49 |
| PIP (cm
H2O) | 26 (9)a | 27 (8) | 25.4 (9.3) | 26 (9) | 24.2 (4.5) | 28.6 (10) |
| No. of cases | 146 | 113 | 102 | 89 | 57 | 39 |
| MAP (cm
H2O) | 12.5 (6) | 11.9 (3.0) | 10.8 (7.3) | 10.9 (4.4) | 11 (6.6) | 10.9 (5.5) |
| No. of cases | 130 | 108 | 99 | 85 | 45 | 34 |
| Vte (ml/kg) | 7.9
(3.5)a | 9.0 (3.9) | 7.9 (3.8) | 8.5 (4.3) | 8.6 (3.2) | 9.1 (5.7) |
| No. of cases | 99 | 106 | 68 | 55 | 39 | 23 |
| PEEP (cm
H2O) | 4.5
(2)a | 4.5 (2) | 4.2 (2) | 4.5 (2) | 4.2 (2) | 4.5 (2) |
| No. of cases | 162 | 138 | 115 | 80 | 59 | 37 |
| RR | 29 (11) | 30 (13) | 29 (10) | 30 (12) | 30 (11) | 31 (14) |
| No. of cases | 152 | 112 | 119 | 71 | 29 | 40 |
| MV (l/min) | 2.5 (2.8) | 2.6 (2.9) | 2.6 (2.3) | 2.4 (2.6) | 2.1 (1.3) | 2.9 (3.3) |
| No. of cases | 108 | 97 | 82 | 63 | 45 | 30 |
 | Table VI.Comparison of mechanical ventilation
parameters on the first, third and seventh day after admission of
patients to university-affiliated hospitals and non-affiliated
hospitals. |
Table VI.
Comparison of mechanical ventilation
parameters on the first, third and seventh day after admission of
patients to university-affiliated hospitals and non-affiliated
hospitals.
|
| Day 1 | Day 3 | Day 7 |
|---|
|
|
|
|
|
|---|
| Parameters |
University-affiliated hospitals | Non-affiliated
hospitals |
University-affiliated hospitals | Non-affiliated
hospitals |
University-affiliated hospitals | Non-affiliated
hospitals |
|---|
|
FiO2 | 49 (19) | 44 (14) | 43 (10) | 39 (14) | 43 (20) | 39 (14) |
| No. of cases | 213 | 192 | 148 | 129 | 73 | 58 |
| PIP (cm
H2O) | 25.4
(7.9)a | 24.2 (8.4) | 23.5
(6.7)a | 24.3 (9.2) | 23.9 (7.2) | 25.2 (10.1) |
| No. of cases | 150 | 134 | 105 | 93 | 49 | 56 |
| MAP (cm
H2O) | 13.4 (6) | 11.0 (3.2) | 11.9 (7) | 10.1 (4.0) | 12.8 (7.5) | 10.5 (5.1) |
| No. of cases | 146 | 138 | 112 | 95 | 66 | 53 |
| Vte (ml/Kg) | 8.4
(3.9)a | 8.7 (3.3) | 8.5 (4.2) | 7.6 (3.7) | 8.9 (3.7) | 7.2 (4.2) |
| No. of cases | 109 | 88 | 79 | 53 | 33 | 20 |
| PEEP (cm
H2O) | 5 (4)a | 4 (2) | 5 (4) | 4 (2) | 5 (3) | 4 (2) |
| No. of cases | 168 | 151 | 121 | 106 | 64 | 53 |
| RR | 29 (13) | 31 (11) | 29 (12.6) | 34 (11) | 34 (10.8) | 31 (13) |
| No. of cases | 166 | 125 | 137 | 104 | 75 | 53 |
| MV (l/min) | 2.6 (3.1) | 2.3 (2.7) | 2.4 (2.2) | 2.3 (2.0) | 2.1 (1.7) | 2.8 (2.5) |
| No. of cases | 123 | 101 | 89 | 68 | 34 | 37 |
Discussion
We found that the proportions of critical
cases/total AHRF cases and the mortality of AHRF were markedly
different among various hospitals, considering hospitals with high
medical condition may have more critical cases admitted in PICU and
the gaps of medical condition in these hospitals were small
(15). In subsequent studies, to
eliminate bias caused by the differences of overall medical level
between different units, units with greater proportions of critical
cases, higher proportions of use of mechanical ventilation, and
more enrolled cases were selected as cooperative units (16). However, a comparison of the rates of
abandonment, mortality rates, and total medical costs of AHRF of
different hospitals and different areas, the results showed that
there were no statistically significant differences between them in
the developed and less developed areas. Additionally, the total
medical expenses were not significantly different. With the
development of the academic exchange, multicenter clinical studies,
and economic development, the gaps between the medical levels of
large hospitals in China are becoming increasingly smaller
(17). The results showed that in
patients between 29 days and 6 years, the occurrence rate of AHRF
in domestic PICUs was equal to the level from 2006. However, there
was a significant decrease in the mortality rates of the patients,
in AHRF, and ARDS, suggesting that respiratory support technology
has gradually improved.
Data from the study have shown that cases of AHRF
were primarily concentrated in the preschool age groups (<1
year, 57.1 vs. 42.9%; <2 years, 66.7 vs. 33.3%), which was
similar to the age spectrum previously observed (13). The disease spectrum of this age group
was simpler than that of the 6-year group, which was more suitable
for the study of small tidal volume ventilation. The comparison
between the AHRF respiratory supported treatment of our study and
that of the 2006 study showed that PEEP (5 vs. 4 cm H2Ο,
P=0.018), FiO2 (0.5 vs. 0.4, P<0.001),
PaΟ2 (70 vs. 60 mmHg, P<0.001), and PIP (20 vs. 24 cm
H2Ο, P<0.001), were all statistically different. In
the present study, the conditions of PIP and PEEP when included,
were more suitable for the requirements of low tidal volume
ventilation than those in 2006. The current study therefore
provided strong evidence for the safety and effectiveness of
respiratory support in the PICU through a lung-protective, small
tidal volume ventilation strategy, which was also confirmed in
adult patients with ARDS (18,19).
Therefore, the lung-protective, small tidal volume ventilation
strategy (20) should be gradually
used by PICU physicians.
The occurrence rates of AHRF and ARDS, and the
proportion of mechanical ventilation used in patients of
non-university-affiliated hospitals were higher than those of
university-affiliated hospitals. In addition, the mortality rates
and rates of abandonment of non-affiliated hospitals were higher
than those of university-affiliated hospitals, while the higher LIS
and OI, and relatively lower PaΟ2/FiO2 ratio
of the included critical patients indicated that the critical
degree of patients in university-affiliated hospitals was higher
than that in non-affiliated hospitals. From the comparison of
specific respiratory parameters, it was found that Vte of patients
in university-affiliated hospitals was higher than that of patients
in non-affiliated hospitals. PEEP, PIP and MAP, which were applied
in patients in university-affiliated hospitals, were higher than
those in non-affiliated hospitals, which indicated that because of
the influence of academic background, respiratory support levels
and diagnosis plans of university-affiliated hospitals were higher
than those of non-affiliated hospitals. The patient in
university-affiliated hospitals also had better compliance when
participated in multicenter clinical studies (21). Therefore, improving the quality of
respiratory therapy is useful to improve the prognosis of patients,
suggesting that in the popularization of respiratory support
(22), attention should be given to
improving technology and training of PICU medical teams.
In conclusion, the levels of economic development
and academic background of hospitals are important factors
affecting the prognosis of patients with AHRF. There are
significant differences in the prognosis of critical patients in
the PICU, and in respiratory support for AHRF in different regions
and various hospitals in China. However, with the development of
economic level and medical exchange, the gap between units in China
is shrinking. Subsequent clinical studies should focus on the
assessment of security and effectiveness of differences in tidal
volume ventilation for the treatment of AHRF (23). Except for Vte, more attention should
be given to the significance of setup parameters of PIP and PEEP
for the prognosis of AHRF.
References
|
1
|
Yu WL, Lu ZJ, Wang Y, Shi LP, Kuang FW,
Qian SY, Zeng QY, Xie MH, Zhang GY, Zhuang DY, et al: Collaborative
Study Group of Pediatric Respiratory Failure: The epidemiology of
acute respiratory distress syndrome in pediatric intensive care
units in China. Intensive Care Med. 35:136–143. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hu X, Qian S, Xu F, Huang B, Zhou D, Wang
Y, Li C, Fan X, Lu Z and Sun B: Chinese Collaborative Study Group
for Pediatric Respiratory Failure: Incidence, management and
mortality of acute hypoxemic respiratory failure and acute
respiratory distress syndrome from a prospective study of Chinese
paediatric intensive care network. Acta Paediatr. 99:715–721.
2010.PubMed/NCBI
|
|
3
|
Flori HR, Glidden DV, Rutherford GW and
Matthay MA: Pediatric acute lung injury: prospective evaluation of
risk factors associated with mortality. Am J Respir Crit Care Med.
171:995–1001. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Timmons OD, Dean JM and Vernon DD:
Mortality rates and prognostic variables in children with adult
respiratory distress syndrome. J Pediatr. 119:896–899. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Goh AY, Chan PW, Lum LC and Roziah M:
Incidence of acute respiratory distress syndrome: a comparison of
two definitions. Arch Dis Child. 79:256–259. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Khemani RG, Conti D, Alonzo TA, Bart RD
III and Newth CJ: Effect of tidal volume in children with acute
hypoxemic respiratory failure. Intensive Care Med. 35:1428–1437.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Randolph AG, Meert KL, O'Neil ME, Hanson
JH, Luckett PM, Arnold JH, Gedeit RG, Cox PN, Roberts JS,
Venkataraman ST, et al: Pediatric Acute Lung Injury and Sepsis
Investigators Network: The feasibility of conducting clinical
trials in infants and children with acute respiratory failure. Am J
Respir Crit Care Med. 167:1334–1340. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brochard L, Lefebvre JC, Cordioli RL,
Akoumianaki E and Richard JC: Noninvasive ventilation for patients
with hypoxemic acute respiratory failure. Semin Respir Crit Care
Med. 35:492–500. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
MacIntyre NR: Supporting oxygenation in
acute respiratory failure. Respir Care. 58:142–150. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li Y, Wang Q, Chen H, Gao HM, Zhou T and
Qian SY: Epidemiological features and risk factor analysis of
children with acute lung injury. World J Pediatr. 8:43–46. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pollack MM, Ruttimann UE and Getson PR:
Pediatric risk of mortality (PRISM) score. Crit Care Med.
16:1110–1116. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
No authors listed, . Guidelines for
developing admission and discharge policies for the pediatric
intensive care unit. Pediatric Section Task Force on Admission and
Discharge Criteria, Society of Critical Care Medicine in
conjunction with the American College of Critical Care Medicine and
the Committee on Hospital Care of the American Academy of
Pediatrics. Crit Care Med. 27:843–845. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bernard GR, Artigas A, Brigham KL, Carlet
J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A and Spragg R: The
Consensus Committee: Report of the American-European consensus
conference on ARDS: definitions, mechanisms, relevant outcomes and
clinical trial coordination. Intensive Care Med. 20:225–232. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Doyle RL, Szaflarski N, Modin GW,
Wiener-Kronish JP and Matthay MA: Identification of patients with
acute lung injury. Predictors of mortality. Am J Respir Crit Care
Med. 152:1818–1824. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kahn JM, Goss CH, Heagerty PJ, Kramer AA,
O'Brien CR and Rubenfeld GD: Hospital volume and the outcomes of
mechanical ventilation. N Engl J Med. 355:41–50. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
García I Jordan, Arriourtúa AB, Torre JA,
Antón JG, Vicente JC and González CT: A national multicentre study
on nosocomial infections in PICU. An Pediatr (Barc). 80:28–33.
2014.(In Spanish). PubMed/NCBI
|
|
17
|
Cifra CL, Bembea MM, Fackler JC and Miller
MR: The morbidity and mortality conference in PICUs in the United
States: a national survey. Crit Care Med. 42:2252–2257. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Oba Y and Salzman GA: Ventilation with
lower tidal volumes as compared with traditional tidal volumes for
acute lung injury. N Engl J Med. 343:813–824. 2000.PubMed/NCBI
|
|
19
|
Spieth PM, Güldner A, Huhle R, Beda A,
Bluth T, Schreiter D, Ragaller M, Gottschlich B, Kiss T, Jaber S,
et al: Short-term effects of noisy pressure support ventilation in
patients with acute hypoxemic respiratory failure. Crit Care.
17:R2612013. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Briel M, Meade M, Mercat A, Brower RG,
Talmor D, Walter SD, Slutsky AS, Pullenayegum E, Zhou Q, Cook D, et
al: Higher vs. lower positive end-expiratory pressure in patients
with acute lung injury and acute respiratory distress syndrome:
systematic review and meta-analysis. JAMA. 303:865–873. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
De Luca D, Piastra M, Chidini G, Tissieres
P, Calderini E, Essouri S, Villanueva A Medina, Allende A Vivanco,
Pons-Odena M, Perez-Baena L, et al: Respiratory Section of the
European Society for Pediatric Neonatal Intensive Care (ESPNIC):
The use of the Berlin definition for acute respiratory distress
syndrome during infancy and early childhood: multicenter evaluation
and expert consensus. Intensive Care Med. 39:2083–2091. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Marohn K and Panisello JM: Noninvasive
ventilation in pediatric intensive care. Curr Opin Pediatr.
25:290–296. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Desai AR and Deep A: Ventilatory
strategies and adjunctive therapy in ARDS. Indian J Pediatr.
73:661–668. 2006. View Article : Google Scholar : PubMed/NCBI
|