Introduction
Renal function is immature in premature infants, and
this can easily result in the development of acute kidney injury
(AKI) due to changes in blood pressure and respiratory conditions,
as well as administration of some drugs. It has been found that
8–24% of premature infants admitted to a neonatal intensive care
unit (NICU) develop AKI (1,2). Additionally, AKI may contribute to the
mortality of very low-birth weight (VLBW) infants with a birth
weight of <1,500 g (3). Serum
creatinine (sCre) is often used as a biomarker for renal function,
albeit it is affected by parameters including muscle mass, gender,
ethnicity, and medication (4).
Additionally, several days are usually required before an increase
in sCre level can be detected in infants with AKI (5).
Neutrophil gelatinase-associated lipocalin (NGAL) is
a 25-kDa protein from the lipocalin family that is primarily
secreted by activated neutrophils (6). NGAL is produced in the granules of
activated neutrophils and also by the nephron in response to any
damage to tubular epithelium; therefore, NGAL can serve as a
biomarker for tubulointerstitial injury (7). When the kidney is damaged, NGAL is
mainly produced in the ascending thick limb of the loop of Henle
and renal collecting tubule, and is immediately secreted into urine
(8). Urinary NGAL (uNGAL) is
increased with renal ischemia and associated acute tubular necrosis
(9), and thus uNGAL is useful for
the prediction of renal failure (10). uNGAL may also be an early marker of
renal failure in adults and children after cardiac surgery or renal
transplantation (11,12), and may be useful in the detection of
chronic kidney failure in children (13), as well as the prediction of
bronchopulmonary dysplasia in premature infants (14). The standard range of uNGAL in
newborns, particularly VLBW infants, has been suggested to range
between 2 and 150 ng/ml (15),
albeit this has not been clearly established (16).
In the present study, we investigated whether an
increase of uNGAL was useful for the early prediction of renal
failure in VLBW infants.
Materials and methods
Subjects
The study subjects were infants who were born with a
gestational age of 23 to <32 weeks and a birth weight of
500–1,500 g, and were admitted to the NICU of Dokkyo Medical
University Hospital from January, 2009 to December, 2010. Infants
with chromosomal abnormalities, external deformities and those with
life-threatening diseases were excluded. Subsequently, a
prospective single-center study was performed.
This study was performed after obtaining approval
from the ethics committee of Dokkyo Medical University (approval
no. 25042) and informed consent from the infants' parents.
Methods
uNGAL and sCre levels were measured daily from
postnatal days 0 to 8. For the measurement of uNGAL, urine was
collected using cotton balls or a urine sampling bag and the
samples were stored at −80°C. When urine was collected with a
cotton ball, the ball was applied to the vulva in the diaper and
was collected after it was immersed in urine. uNGAL and urinary Cre
(uCre) levels were unaffected by the measurement method (17,18).
Furthermore, measurements of uNGAL levels in 23 subjects using
urine sampling bags and cotton balls produced values of 134.5±128
and 132.1±125 ng/ml, respectively, with no significant difference
(P=0.95). Based on these data, we collected urine using one of
these methods.
uNGAL was measured using an NGAL ELISA kit 036
(BioPorto Diagnostics, Gentofte, Denmark) that specifically detects
human NGAL. The urine sample was diluted 500 times using dilution
solution provided in the NGAL kit. NGAL standards or diluted
samples (100 µl) were applied to precoated microwells in duplicate,
incubated for 1 h at 23±2°C, and washed with washing buffer.
Subsequently, biotinylated NGAL antibody and HRP-streptavidin were
added to wells and incubated for 1 h via centrifugation using a
shaking platform (200 rpm; Taiyo Micromixer, Taiyo Science
Industrial Co. Ltd., Tokyo, Japan). TMB substrate was added for 10
min in the dark prior to adding stop solution. The NGAL
concentration was then measured at 450 nm wavelength in each well
with a reference reading at 620 nm in blank wells. The average was
considered to be the uNGAL value. uCre was measured in the same
samples.
sCre is generally used as an index of renal
dysfunction in the first postnatal month (16) and is obtained using blood samples
obtained in daily medical routine tests. AKI is diagnosed based on
sCre ≥1.2 mg/dl (17). Subjects with
sCre levels of ≥1.2 and <1.2 mg/dl were compared using U tests
for gestational age, birth weight, and Apgar score, and Chi-square
tests for gender. Indomethacin was employed for the treatment of
patent ductus arteriosus in immature infants, and aminoglycoside
antibiotics were used, as well as mechanical ventilation, antenatal
steroid therapy, delivery method, and onset of chorioamnionitis for
the diagnosis of AKI (17).
Statistical analysis
SPSS 11.0J for Windows (SPSS, Inc., Chicago, IL,
USA) software was used for statistical analysis. Logistic
regression analyses were performed for uNGAL and uNGAL/uCre with
next-day sCre. Subjects were divided into low and high uNGAL groups
based on the median uNGAL level on each day. Logistic regression
analysis was then performed to calculate the odds ratio for
next-day sCre as a predictor of high uNGAL, with the value for the
low uNGAL group set to 1. Similar analyses were conducted for
uNGAL/uCre. P<0.05 was considered to indicate a statistically
significant difference.
Results
Subjects were stratified based on their weight into
four groups: i) 500–750 g group (n=9); ii) 751–1,000 g group
(n=15); iii) 1,001–1,250 g group (n=8); and iv) 1,251–1,500 g group
(n=8). The gestational ages ranged from 23 weeks and 0 days to
<26 weeks (n=13), 26 weeks and 0 days to <29 weeks (n=18),
and 29 weeks and 0 days to <32 weeks (n=9). During the study
period, 16 subjects had sCre ≥1.2 mg/dl. Groups with sCre ≥1.2 and
<1.2 mg/dl had significant differences in gestational age,
birthweight, and 1- and 5-min Apgar scores, but no significant
differences in gender, delivery method, use of antenatal steroids,
chorioamnionitis, use of indomethacin, use of aminoglycoside
antibiotics, or mechanical ventilation were detected (Table I).
 | Table I.Infant and maternal
characteristics. |
Table I.
Infant and maternal
characteristics.
| Characteristics | sCre ≥1.2 mg/dl
(n=16) | sCre <1.2 mg/dl
(n=24) | P-value |
|---|
| Gestational age
(weeks)a | 26.3±1.9 |
27.6±2.0 | 0.030 |
| Birthweight
(g)a |
845±251 | 1,055±252 | 0.013 |
| Normal spontaneous
delivery (%) | 7
(44) | 14 (58) | 0.520 |
| 1-min
Apgara |
4.0±2.1 |
5.6±2.1 | 0.030 |
| 5-min
Apgara |
6.9±1.1 |
7.8±1.7 | 0.029 |
| Female (%) | 9
(56) | 10 (42) | 0.520 |
| Antenatal steroids
(%) | 9
(56) | 18 (75) | 0.305 |
| Chorioamnionitis
(%) | 11 (69) | 16 (67) | 1.000 |
| Indomethacin
(%) | 12 (75) | 12 (50) | 0.188 |
| Aminoglycoside
(%) | 14 (88) | 16 (67) | 0.263 |
| Mechanical
ventilation (%) | 11 (69) | 8
(33) | 0.051 |
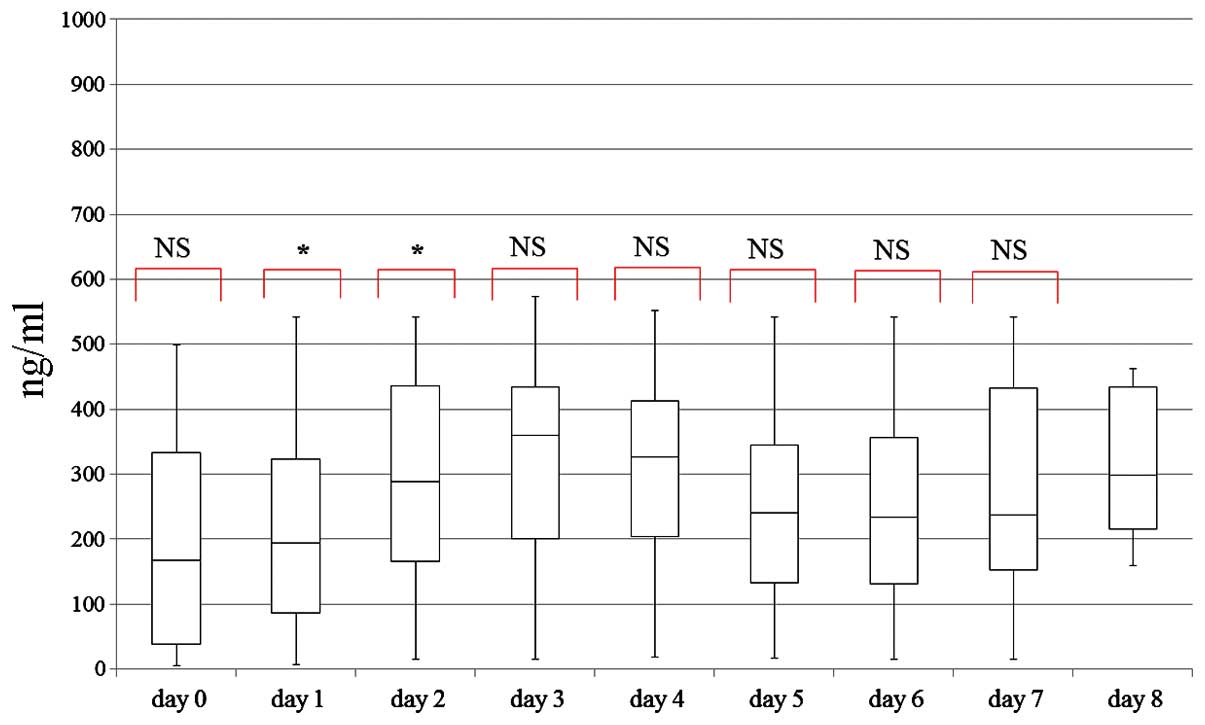
uNGAL levels measured in all subjects on postnatal
days 0 to 8 are shown in Fig. 1. The
median uNGAL was higher than the reported standard value in VLBW
infants. There were significant differences in uNGAL between
postnatal days 1 and 2, and between postnatal days 2 and 3
(Fig. 1). Based on logistic
regression analysis, an increase in next-day sCre was significantly
correlated with uNGAL on postnatal days 2, 3, 4, 5 and 6
(P<0.05), but with uNGAL/uCre only on postnatal days 5 and 6
(P<0.05).
Subjects were also divided into low and high uNGAL
groups based on the median uNGAL measured each day. Calculation of
the odds ratio showed that next-day sCre was a predictor of high
uNGAL on postnatal days 2, 3 and 6 (Table II). No relationship with next-day
sCre was detected for uNGAL/uCre on any day (Table III).
 | Table II.Logistic analysis of uNGAL and
next-day serum creatinine. |
Table II.
Logistic analysis of uNGAL and
next-day serum creatinine.
|
|
| uNGAL (ng/ml) |
|
|
|---|
|
|
|
|
|
|
|---|
| Postnatal | No. | Low | High | Odds ratio |
P-valuea |
|---|
| Day 0 | 23 |
5.9–167.7 | 167.8–499.0 | – | 0.744 |
| Day 1 | 40 |
6.6–193.2 | 193.3–542.1 | 3.00
(0.51–17.74) | 0.063 |
| Day 2 | 40 |
15.8–288.5 | 288.6–541.4 | 7.36
(1.34–40.55) | 0.009 |
| Day 3 | 40 |
14.3–359.6 | 359.7–572.6 | 15.52
(1.73–139.26) | 0.010 |
| Day 4 | 40 |
18.6–326.2 | 326.3–551.8 | – | 0.013 |
| Day 5 | 40 |
17.0–239.9 | 240.0–542.2 | – | 0.011 |
| Day 6 | 40 |
15.6–233.7 | 233.8–541.0 | 10.23
(1.12–93.34) | 0.004 |
| Day 7 | 40 |
15.0–237.6 | 237.7–542.0 | 6.33
(0.67–60.16) | 0.122 |
| Day 8 | 17 | 158.6–298.9 | 299.0–462.3 | – | 0.463 |
 | Table III.Logistic analysis of uNGAL/uCre and
next-day sCre. |
Table III.
Logistic analysis of uNGAL/uCre and
next-day sCre.
|
|
| uNGAL/uCre |
|
|
|---|
|
|
|
|
|
|
|---|
| Postnatal | No. | Low | High | Odds ratio |
P-valuea |
|---|
| Day 0 | 23 | 1.0–19.4 | 19.5–95.7 | – | 0.486 |
| Day 1 | 40 | 0.8–18.9 | 19.0–82.4 | 1.42
(0.27–7.34) | 0.228 |
| Day 2 | 40 | 1.6–26.0 | 26.1–61.8 | 2.15
(0.52–9.00) | 0.144 |
| Day 3 | 40 | 0.9–21.2 | 21.3–73.1 | 3.05
(0.66–14.13) | 0.159 |
| Day 4 | 40 | 1.6–24.6 | 24.7–53.6 | – | 0.110 |
| Day 5 | 40 | 1.7–18.1 | 18.2–52.6 | 8.14
(0.88–75.48) | 0.031 |
| Day 6 | 40 | 1.7–20.4 | 20.5–64.9 | 3.86
(0.67–22.11) | 0.014 |
| Day 7 | 40 | 1.3–21.5 | 21.6–78.0 | 2.53
(0.41–15.75) | 0.065 |
| Day 8 | 17 | 9.5–22.7 | 22.8–65.1 | – | 0.524 |
Discussion
The results of the present study have shown that,
subjects with lower gestational age, lower birth weight, and lower
1- and 5-min Apgar scores had increased levels of sCre. Similar
results were reported in previous studies (19,20).
These results were consistent with findings showing that AKI occurs
in 47–61% of cases of neonatal asphyxia with a 5-min Apgar score of
<7 (20–22). It has been suggested that, compared
to sCre, acute renal dysfunction in pediatric patients may be
diagnosed more quickly based on NGAL in urine or blood after
cardiac surgery (11). It was also
reported that renal failure may be predicted more precisely with
uNGAL because compared to blood NGAL levels, there was a marked
increase in uNGAL levels (11).
Thus, uNGAL is a more effective marker for renal dysfunction in
children (11).
Higher levels of uNGAL have been detected in VLBW
infants with a lower birth weight and lower gestational age
(17), as well as in those with
onset of AKI (23,24). The results showed that, uNGAL levels
in the current study were higher than the recently reported
standard value in VLBW infants (15,25).
This difference may be explained by the fact that there were many
premature infants with a gestational age <27 weeks among our
subjects.
Next-day sCre, rather than sCre on the day of uNGAL
measurement, was found to be a predictor for uNGAL. A difference in
correlations of uNGAL with uNGAL/uCre and sCre were found (26), but our results support those of
previous studies showing that correction of uNGAL with uCre was not
necessary (15,17,27). An
increase in uNGAL (a marker of proximal tubular epithelium
disorder) may occur before an increase in sCre (a marker of
glomerular disorder), because nephrogenic renal dysfunction may
develop when prerenal failure is protracted (28). Additionally, Cre excreted due to
tubular disorder may be reabsorbed due to insufficient tubular
function, which can cause an increase in sCre in infants with LBW
(29,30). uNGAL is excreted from renal proximal
tubular cells as a response to AKI (31) and nephrogenic injury (32), and is increased in patients with
late-onset sepsis (33).
uNGAL is not correlated with sCre in VLBW infants
(16), however, our results
suggested that uNGAL was a useful biomarker for the early diagnosis
of renal failure in premature infants by predicting an increase in
next-day sCre. The increase in sCre levels was significant in the
high uNGAL group, and thus this group was likely to be at risk for
AKI.
Further studies using bigger samples are needed to
establish standard daily uNGAL levels for early postnatal days.
Measurement of uNGAL has the advantage of being non-invasive for
VLBW infants, and use of uNGAL in clinical practice may allow the
prediction of renal failure, control of water intake, control of
dosage of antibiotics that may induce renal failure, such as
aminoglycosides and vancomycin for MRSA, and the need for use of
indomethacin.
The most significant shortcoming of the present
study was that we were not able to completely collect the maternal
sCre data samples. This was because the sCre level of neonates 0 to
3 days after birth were influenced by the maternal sCre through the
placenta, and data were not reflected adequately (34–36). In
retrospect, this aspect should have been taken into consideration.
Furthermore, because we only evaluated the relationship between
uNGAL and sCre, the correlation with AKI was poor. We cannot
disregard the possibility that AKI was overvalued. However, our
results indicate that there was a correlation between uNGAL and
sCre in VLBW infants, because it had the potential to function as
the basic data for additional studies in the future. More clinical
and basic studies on NGAL have been reported recently (37–43). In
summary, more research on the biological mechanism of the NGAL is
necessary.
Acknowledgements
The present study was supported by Grants-in-Aid for
The Morinaga Foundation for Health and Nutrition. We would like to
express our gratitude and appreciation to the entire Department of
Pediatrics and NICU medical staff, Dokkyo Medical University
Hospital, Tochigi, Japan.
References
|
1
|
Hentschel R, Lödige B and Bulla M: Renal
insufficiency in the neonatal period. Clin Nephrol. 46:54–58.
1996.PubMed/NCBI
|
|
2
|
Stapleton FB, Jones DP and Green RS: Acute
renal failure in neonates: Incidence, etiology and outcome. Pediatr
Nephrol. 1:314–320. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Askenazi DJ, Griffin R, McGwin G, Carlo W
and Ambalavanan N: Acute kidney injury is independently associated
with mortality in very low birthweight infants: A matched
case-control analysis. Pediatr Nephrol. 24:991–997. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Askenazi DJ, Ambalavanan N and Goldstein
SL: Acute kidney injury in critically ill newborns: What do we
know? What do we need to learn? Pediatr Nephrol. 24:265–274.
2009.PubMed/NCBI
|
|
5
|
Jo SK, Rosner MH and Okusa MD:
Pharmacologic treatment of acute kidney injury: Why drugs haven't
worked and what is on the horizon. Clin J Am Soc Nephrol.
2:356–365. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Soni SS, Pophale R and Ronco C: New
biomarkers for acute renal injury. Clin Chem Lab Med. 49:1257–1263.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kuwabara T, Mori K, Mukoyama M, Kasahara
M, Yokoi H, Saito Y, Yoshioka T, Ogawa Y, Imamaki H, Kusakabe T, et
al: Urinary neutrophil gelatinase-associated lipocalin levels
reflect damage to glomeruli, proximal tubules, and distal nephrons.
Kidney Int. 75:285–294. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gonzalez F and Vincent F: Biomarkers for
acute kidney injury in critically ill patients. Minerva Anestesiol.
78:1394–1403. 2012.PubMed/NCBI
|
|
9
|
Mishra J, Mori K, Ma Q, Kelly C, Yang J,
Mitsnefes M, Barasch J and Devarajan P: Amelioration of ischemic
acute renal injury by neutrophil gelatinase-associated lipocalin. J
Am Soc Nephrol. 15:3073–3082. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mori K, Lee HT, Rapoport D, Drexler IR,
Foster K, Yang J, Schmidt-Ott KM, Chen X, Li JY, Weiss S, et al:
Endocytic delivery of lipocalin-siderophore-iron complex rescues
the kidney from ischemia-reperfusion injury. J Clin Invest.
115:610–621. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mishra J, Dent C, Tarabishi R, Mitsnefes
MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, et al:
Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker
for acute renal injury after cardiac surgery. Lancet.
365:1231–1238. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Parikh CR, Jani A, Mishra J, Ma Q, Kelly
C, Barasch J, Edelstein CL and Devarajan P: Urine NGAL and IL-18
are predictive biomarkers for delayed graft function following
kidney transplantation. Am J Transplant. 6:1639–1645. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nishida M, Kawakatsu H, Okumura Y and
Hamaoka K: Serum and urinary neutrophil gelatinase-associated
lipocalin levels in children with chronic renal diseases. Pediatr
Int. 52:563–568. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Inoue H, Ohga S, Kusuda T, Kitajima J,
Kinjo T, Ochiai M, Takahata Y, Honjo S and Hara T: Serum neutrophil
gelatinase-associated lipocalin as a predictor of the development
of bronchopulmonary dysplasia in preterm infants. Early Hum Dev.
89:425–429. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huynh TK, Bateman DA, Parravicini E,
Lorenz JM, Nemerofsky SL, Sise ME, Bowman TM, Polesana E and
Barasch JM: Reference values of urinary neutrophil
gelatinase-associated lipocalin in very low birth weight infants.
Pediatr Res. 66:528–532. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gubhaju L, Sutherland MR, Horne RS,
Medhurst A, Kent AL, Ramsden A, Moore L, Singh G, Hoy WE and Black
MJ: Assessment of renal functional maturation and injury in preterm
neonates during the first month of life. Am J Physiol Renal
Physiol. 307:F149–F158. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lavery AP, Meinzen-Derr JK, Anderson E, Ma
Q, Bennett MR, Devarajan P and Schibler KR: Urinary NGAL in
premature infants. Pediatr Res. 64:423–428. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Roberts SB and Lucas A: Measurement of
urinary constituents and output using disposable napkins. Arch Dis
Child. 60:1021–1024. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Miall LS, Henderson MJ, Turner AJ,
Brownlee KG, Brocklebank JT, Newell SJ and Allgar VL: Plasma
creatinine rises dramatically in the first 48 hours of life in
preterm infants. Pediatrics. 104:e761999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Karlowicz MG and Adelman RD: Nonoliguric
and oliguric acute renal failure in asphyxiated term neonates.
Pediatr Nephrol. 9:718–722. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Aggarwal A, Kumar P, Chowdhary G, Majumdar
S and Narang A: Evaluation of renal functions in asphyxiated
newborns. J Trop Pediatr. 51:295–299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gupta BD, Sharma P, Bagla J, Parakh M and
Soni JP: Renal failure in asphyxiated neonates. Indian Pediatr.
42:928–934. 2005.PubMed/NCBI
|
|
23
|
Askenazi DJ, Montesanti A, Hunley H,
Koralkar R, Pawar P, Shuaib F, Liwo A, Devarajan P and Ambalavanan
N: Urine biomarkers predict acute kidney injury and mortality in
very low birth weight infants. J Pediatr. 159:907–12.e1. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Askenazi DJ, Koralkar R, Levitan EB,
Goldstein SL, Devarajan P, Khandrika S, Mehta RL and Ambalavanan N:
Baseline values of candidate urine acute kidney injury biomarkers
vary by gestational age in premature infants. Pediatr Res.
70:302–306. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Parravicini E, Lorenz JM, Nemerofsky SL,
O'Rourke M, Barasch J and Bateman D: Reference range of urinary
neutrophil gelatinase-associated lipocalin in very low-birth-weight
infants: Preliminary data. Am J Perinatol. 26:437–440. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
La Manna G, Galletti S, Capelli I, Vandini
S, Nisi K, Aquilano G, Mancini R, Carretta E, Montini G, Faldella
G, et al: Urinary neutrophil gelatinase-associated lipocalin at
birth predicts early renal function in very low birth weight
infants. Pediatr Res. 70:379–383. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Parravicini E: The clinical utility of
urinary neutrophil gelatinase-associated lipocalin in the neonatal
ICU. Curr Opin Pediatr. 22:146–150. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mori K and Nakao K: Neutrophil
gelatinase-associated lipocalin as the real-time indicator of
active kidney damage. Kidney Int. 71:967–970. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Levey AS, Perrone RD and Madias NE: Serum
creatinine and renal function. Annu Rev Med. 39:465–490. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Perrone RD, Madias NE and Levey AS: Serum
creatinine as an index of renal function: New insights into old
concepts. Clin Chem. 38:1933–1953. 1992.PubMed/NCBI
|
|
31
|
Schmidt-Ott KM, Mori K, Li JY, Kalandadze
A, Cohen DJ, Devarajan P and Barasch J: Dual action of neutrophil
gelatinase-associated lipocalin. J Am Soc Nephrol. 18:407–413.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gwira JA, Wei F, Ishibe S, Ueland JM,
Barasch J and Cantley LG: Expression of neutrophil
gelatinase-associated lipocalin regulates epithelial morphogenesis
in vitro. J Biol Chem. 280:7875–7882. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Parravicini E, Nemerofsky SL, Michelson
KA, Huynh TK, Sise ME, Bateman DA, Lorenz JM and Barasch JM:
Urinary neutrophil gelatinase-associated lipocalin is a promising
biomarker for late onset culture-positive sepsis in very low birth
weight infants. Pediatr Res. 67:636–640. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lao TT, Loong EP, Chin RK and Lam YM:
Renal function in the newborn. Newborn creatinine related to birth
weight, maturity and maternal creatinine. Gynecol Obstet Invest.
28:70–72. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Filler G, Guerrero-Kanan R and
Alvarez-Elías AC: Assessment of glomerular filtration rate in the
neonate: Is creatinine the best tool? Curr Opin Pediatr.
28:173–179. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Filler G, Lopes L and Awuku M: The
Importance of Accurately Assessing Renal Function in the Neonate
and Infant. Adv Clin Chem. 71:141–156. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wu J, Ding Y, Zhu C, Shao X, Xie X, Lu K
and Wang R: Urinary TNF-α and NGAL are correlated with the
progression of nephropathy in patients with type 2 diabetes. Exp
Ther Med. 6:1482–1488. 2013.PubMed/NCBI
|
|
38
|
Du Y, Hou L, Guo J, Sun T, Wang X and Wu
Y: Renal neutrophil gelatinase-associated lipocalin and kidney
injury molecule-1 expression in children with acute kidney injury
and Henoch-Schönlein purpura nephritis. Exp Ther Med. 7:1130–1134.
2014.PubMed/NCBI
|
|
39
|
Wu BL, Li CQ, Du ZP, Zhou F, Xie JJ, Luo
LW, Wu JY, Zhang PX, Xu LY and Li EM: Functional analysis of the
mRNA profile of neutrophil gelatinase associated lipocalin
overexpression in esophageal squamous cell carcinoma using multiple
bioinformatic tools. Mol Med Rep. 10:1800–1812. 2014.PubMed/NCBI
|
|
40
|
Zhang P, Li Y, Zhang LD, Wang LH, Wang X,
He C and Lin ZF: Proteome changes in mesenteric lymph induced by
sepsis. Mol Med Rep. 10:2793–2804. 2014.PubMed/NCBI
|
|
41
|
Olguner CG, Koca U, Altekin E, Ergür BU,
Duru S, Girgin P, Taşdöğen A, Gündüz K, Güzeldağ S, Akkuş M, et al:
Ischemic preconditioning attenuates lipid peroxidation and
apoptosis in the cecal ligation and puncture model of sepsis. Exp
Ther Med. 5:1581–1588. 2013.PubMed/NCBI
|
|
42
|
Zhang PX, Zhang FR, Xie JJ, Tao LH, Lü Z,
Xu XE, Shen J, Xu LY and Li EM: Expression of NGAL and NGALR in
human embryonic, fetal and normal adult tissues. Mol Med Rep.
6:716–722. 2012.PubMed/NCBI
|
|
43
|
Kesik V, Demirkaya E and Buyukpamukçu M:
Urinary neutrophil gelatinase associated lipocalin as a biomarker
in ifosfamide induced chronic renal failure. Eur Rev Med Pharmacol
Sci. 19:4851–4857. 2015.PubMed/NCBI
|