Introduction
Scabies is an important health concern in hospitals
and care facilities. There is no standardized report about Scabies,
and occurrence rates vary in the recent literature from 0.271 to
46% (1). Although there is less
information about mortality, deaths frequently occur due to
secondary sepsis (2). There are
numerous medical staff who have not experienced scabies, and there
are previous reports that have misdiagnosed it as eczema and senile
dermal pruritus, leading to an outbreak because of its highly
contagious nature (3–6). Scabies is relatively common in tropical
areas and in developing countries because of poor hygiene
practices, and war and poverty can be causes of large epidemics
(7). However, sometimes epidemics
occur in medical institutions in elderly and immune-suppressed
patients, even in developed countries. In a previous report,
bedridden, living in a nursing home, a higher clinical severity
status before admission and a catheter inserted are identified as
being significant risk factors for acquiring scabies infection
(8). Delayed diagnosis of Norwegian
scabies, which is highly infectious, has occurred (9). Ivermectin is used worldwide in oral or
injection form . Topical application of 5% permethrin cream is also
popular and the combination of an effective topical treatment and
oral ivermectin seems to be most successful (10). The present study describes an
outbreak of Norwegian scabies at Toho University School of
Medicine, Omori Hospital (Tokyo, Japan). This study demonstrates
the need for medical staff education so that the infection can be
detected early, and the need of an early referral procedure to a
medical specialist.
Materials and methods
The present epidemiologic study was performed
between June 2014 and October 2014 in a diabetic and collagen
disease ward at the Toho University School of Medicine, Omori
Hospital. Written informed consent was obtained from all patients.
The clinical features of scabies patients and a report on a
follow-up survey that was conducted by the infection control
committee were respectively reviewed. The follow-up survey included
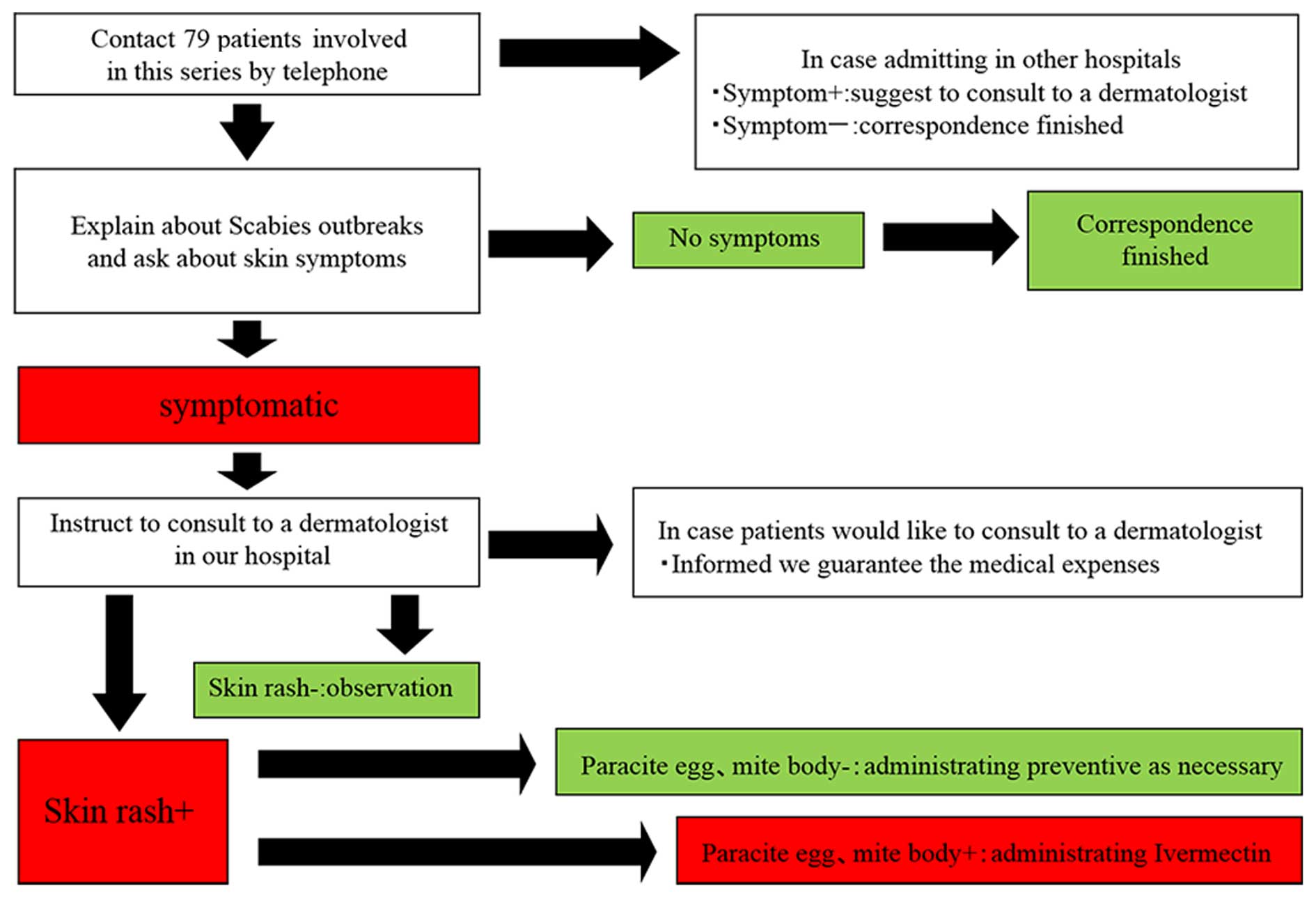
the following four steps: i) Contact patients admitted onto the
same ward as that of a confirmed case; ii) telephone interviews
with all family members of the confirmed cases; iii) instructions
to consult a dermatologist from the hospital in person or by
telephone for those who have symptoms; and iv) consult a
dermatologist from our hospital for all medical staff who worked on
the same ward (Fig. 1). The case
definition did not include suspected cases and a definitive
diagnosis of scabies was confirmed by a dermatologist based on the
presence of burrows, eggs and mites that were observed using
dermatoscopy or microscopy. A suspected case was defined as a
person who presents signs and symptoms consistent with scabies, who
had direct contact with a confirmed case within the two months
preceding the onset of symptoms and who was present in the same
room as the first infected patient (patient A). Direct contact with
patients with scabies was defined as prolonged hand contact,
touching and cleaning of the patient's bed and linen and those who
were admitted to the same room as the first infected patient
(patient A). All patients who were admitted on the same ward when
the scabies patients were hospitalized were located, and medical
staff who worked on the same ward during the period the scabies
patients were present were considered to be indirect contacts.
Patient A was an 84-year-old male with a history of
diabetes. Patient B was a 77-year-old male with a history of
diabetes. Patient C was 79-year-old female receiving
corticosteroids for rheumatoid arthritis. Patient D was a
82-year-old male receiving corticosteroids for rheumatoid
arthritis.
Results
This outbreak involved a total of 181 cases among
medical staff and patients, and 6 patients developed scabies. It
was considered that the absence of burrows, eggs and mites did not
eliminate the risk of scabies infestation. Ivermectin (Maruho Co.,
Ltd., Osaka, Japan) was administered orally as therapeutic
administration (200µg/kg twice at two-week intervals) in 6 patients
and as a preventive (one dose of 200µg/kg) in 35 individuals.
Phenothrin ointment was applied administered to 6 patients. Patient
A, who had been admitted for diabetes, was diagnosed with Norwegian
scabies on July 28, 2014 (Fig. 1).
An infection control committee was immediately set up when the
first cases were diagnosed. The aim was early prophylaxis,
surveillance and the completion of treatment. Committee members
attended weekly meetings and exchanged information about the
progress of patients and the outbreak. The investigation was
continued as outlined in the personal and telephone interview
flowchart (Fig. 2). During this
investigation, two staff (Fig. 3)
and 3 patients were newly identified as potentially having
Norwegian scabies infection. One of the patients was diagnosed as
having Norwegian scabies, and they were admitted for scleroderma
(Figs. 4–6). Thus, the outbreak was resolved in three
months. During this period, seven relatives of the medical staff
developed scabies (Table I). The
early resolution is considered to be a result of rapid response to
infection.
 | Table I.Scabies clinical course. |
Table I.
Scabies clinical course.
| Date | Patient
situation | Infection control
committee correspondence |
|---|
| 06/19 | Patient A admitted to
health facility |
|
| 06/23 | Rash appeared on
Patient A |
|
| 07/28 | Patient A
diagnosed | Infection control
committee set up with Norwegian scabies |
| 07/29 |
| Screened all medical
staff and patients admitted in the same room with Patient A →
negative |
| 09/23 | Staff A diagnosed
with scabies | Ward closure |
| 09/24 | Staff B diagnosed
with scabies | • Re-screened all
medical staff and patients admitted in the same ward |
|
|
| • Preventive
ivermectin administration performed in 2 patients and 33 medical
staff |
|
|
| • Informed every
medical office and ward |
|
|
| • Informed local
public health care center |
|
|
| • Informed every
patient who was discharged |
| 09/29 | Patient B, who was
admitted during 06/18-07/03, diagnosed with scabies | Notified by public
health care center to confirm the skin condition of patients
admitted from the onset to the present time |
| 10/01 |
| Informed the Ministry
of Welfare |
| 10/03 | Patient C, who was
admitted during | At this time: |
|
| 06/06-07/15,
diagnosed with scabies Patient | • 4 patients
developed scabies |
|
| D diagnosed with
Norwegian scabies | • 2 medical staff
developed scabies |
|
|
| • 1 medical staff
family member developed scabies → total of 7 patients |
| 10/16 |
| Investigation
according to personal and telephone interview flowchart
completed |
| 10/13 | Treatment ended for
all medical staff |
|
| 10/27 | Treatment ended for
all patients | Confirmation of
outbreak resolution |
Discussion
The present study describes a series of scabies
outbreaks in a hospital in Tokyo, Japan. Although worldwide
prevalence has been estimated to be ~300 million cases per year
(11), scabies is relatively common
in tropical areas and developing countries because of poor hygiene,
war and poverty, which has led to large epidemics. Scabies
outbreaks can be a serious health problem even in industrialized
countries, particularly in schools, prisons, hospitals and in other
health care facilities (7). Although
a definitive diagnosis is made by dermatoscopy or microscopy, early
diagnosis is sometimes made using clinical signs and symptoms
(12).
Most of the outbreaks were caused by late diagnosis
that resulted from a lack of knowledge and practice, and the
opportunity for early diagnosis was missed. Making an early
diagnosis can be more difficult in immunosuppressed and elderly
patients because they present with atypical symptoms (3), such as hyperkeratotic lesions on the
fingertips and nails (13),
microvesicular rash and generalized pruritus and hyperkeratosis
(14), and hyperpigmented crusted
plaques with hemorrhagic fissures (15). Late diagnosis, misdiagnosis or a
misleading diagnosis are thought to occur frequently even if
dermatologist recommendations are followed, which can lead to
outbreaks in medical institutions (16). It is difficult to control this
disease once an epidemic occurs, particularly in dementia patients
and in facilities where medical staff have insufficient knowledge
about scabies. Because the primary symptom of scabies is itching,
communication difficulties can sometimes lead to late diagnosis. In
addition, less experience and lack of knowledge can contribute to
late diagnosis and thereby cause Norwegian scabies epidemics
(17).
In the present study, the outbreak occurred in a
diabetic and collagen disease ward. This type of immune-related
disease could be a risk factor for the spread of scabies. It has
been reported that there is a higher risk of mortality in patients
with complications such as human immunodeficiency virus (HIV)/human
T-cell leukemia virus type 1 infection (18). Particular attention should be paid to
patients with scabies if they are undergoing immunosuppressive
therapy or if they have conditions such as diabetes or HIV
(19). In the present study, it was
thought that the spread of infection could be minimized by quick
action. There are a number of reports of limited damage and
practices that can be followed to control scabies outbreaks in
health facilities, and the studies suggest that countermeasures
should start immediately in such cases (12,16). In
the current study, the authors asked to be involved with the
infection control committee in order to gain increased knowledge
about the outbreak. Immediate organization of the infection control
committee led to quick action and resulted in an early resolution
of the outbreak. From this, it can be suggested that each facility
needs to establish the management process, and recognize that
external support may be required.
In conclusion, once the scabies outbreak occurred, a
lot of time and labor was required to contain the outbreak. The
education of medical staff to aid early detection, and the
establishment of a working system that allows wide-spread early
referrals to a medical specialist in suspected cases, can identify
and control scabies infection. Education and prompt action can
prevent a scabies outbreak.
References
|
1
|
Fuller LC: Epidemiology of scabies. Curr
Opin Infect Dis. 26:123–126. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
McCarthy JS, Kemp DJ, Walton SF and Currie
BJ: Scabies: More than just an irritation. Postgrad Med J.
80:382–387. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bouvresse S and Chosidow O: Scabies in
healthcare settings. Curr Opin Infect Dis. 23:111–118. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jeanneret L Achtari, Erard P, Gueissaz F
and Malinverni AR: An outbreak of scabies: A forgotten parasitic
disease still present in Switzerland. Swiss Med Wkly. 137:695–699.
2007.PubMed/NCBI
|
|
5
|
Scheinfeld N: Controlling scabies in
institutional settings: A review of medications, treatment models
and implementation. Am J Clin Dermatol. 5:31–37. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Obasanjo OO, Wu P, Conlon M, Karanfil LV,
Pryor P, Moler G, Anhalt G, Chaisson RE and Perl TM: An outbreak of
scabies in a teaching hospital: Lesson learned. Infect Control Hosp
Epidemiol. 22:13–18. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hay RJ, Steer AC, Chosidow O and Currie
BJ: Scabies: A suitable case for a global control initiative. Curr
Opin Infect Dis. 26:107–109. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang CH, Lee SC, Huang SS, Kao YC, See LC
and Yang SH: Risk factors for scabies in Taiwan. J Microbiol
Immunol Infect. 45:276–280. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Utsumi M, Makimoto K, Quroshi N and Ashida
N: Types of infectious outbreaks and their impact in elderly care
facilities: A review of the literature. Age Ageing. 39:299–305.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Meinking TL, Taplin D, Hermida JL, Pardo R
and Kerdel FA: The treatment of scabies with ivermectin. N Engl J
Med. 333:26–30. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chosidow O: Clinical practices: Scabies. N
Engl J Med. 354:1718–1727. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Buehlmann M, Beltramineli H, Strub C,
Bircher A, Jordan X, Battegay M, Itin P and Widmer AF: Scabies
outbreak in an intensive care unit with exposed individuals-key
factors for controlling the outbreak. Infect Control Hosp
Epidemiol. 30:354–360. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Del Borgo C, Belvisi V, Tieghi T and
Mastroianni CM: Atypical presentation of crusted (Norwegian)
scabies. Infection. 43:623–624. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Boureau AS, Cozic C, Poiraud C, Varin S,
Chaillous B and Cormier G: Does immunodepression induced by TNF
antagonists promote atypical scabies? Joint Bone Spine. 81:186–187.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fernández-Sánchez M, Saeb-Lima M,
Alvarado-de la Barrera C and Reyes-Terán G: Crusted
scabies-associated immune reconstitution inflammatory syndrome. BMC
Infect Dis. 12:3232012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tjioe M and Vissers WH: Scabies outbreaks
in nursing homes for the elderly: Recognition, treatment options
and control of reinfestation. Drugs Aging. 25:299–306. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tsutsumi M, Nishiura H and Kobayashi T:
Dementia specific risks of scabies: Retrospective epidemiologic
analysis of an unveiled nosocomial outbreak in Japan from 1989–90.
BMC Infect Diss. 5:852005. View Article : Google Scholar
|
|
18
|
Brites C, Weyll M, Pedoroso C and Badaró
R: Severe and Norwegian scabies are strongly associated with
retroviral (HIV-1/HTLV-1) infection in Bahia, Brazil. AIDS.
16:1292–1293. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Capobussi M, Sabatino G, Donadini A,
Tersalvi CA and Castaldi S: Control of scabies outbreaks in an
Italian hospital: An information-centered management strategy. Am J
Infect Control. 42:316–320. 2014. View Article : Google Scholar : PubMed/NCBI
|