Introduction
Hepatitis C virus (HCV) chronically infects ~180
million people worldwide, and is a frequent cause of liver
diseases, including liver failure and hepatocellular carcinoma
(1,2). The seroprevalence of hepatitis C
infection in the general population of China is estimated to be
0.8–2.1% (3). The rate is much
higher in certain subgroups such as injecting drug users or
subjects with hemophilia (3).
The discovery of direct-acting antiviral agents
(DAAs) in 2002 led to the development of small molecules to block
the replication of HCV, including novel antiviral targets (4,5). Based
on the impressive improvements in sustained virologic response
(SVR) rates in phase III trials (6),
the first two protease inhibitors telaprevir and boceprevir were
recently approved by the US Food and Drug Administration, and are
currently recommended first line agents for genotype 1 infections.
However, while they are generally well-tolerated, adverse events
are common, and the agents are very expensive. Furthermore, triple
therapy is not approved for use in non-genotype 1 HCV infections,
and there are numerous drug-drug interactions that preclude their
use. Prior to the development of triple therapy, peginterferon α-2b
or peginterferon α-2a alone, or in combination with weight-based
ribavirin had been the standard treatment chronic hepatitis C
resulting in SVRs of 30 and 50% (7,8)
respectively, for genotype 1 cases, and 80% for genotypes 2 and 3
(9–12).
Two polyethylene glycol (PEG)-modified interferons,
interferon (IFN)-α-2a containing a branched 40-kD PEG molecule
(PEGASYS®; F. Hoffmann-La Roche, Inc., Basel,
Switzerland) and IFN-α-2b containing a linear 12-kD PEG molecule
(PEG-INTRON®; Merck & Co., Inc., Kenilworth, NJ,
USA) are currently on the market. However, side effects are quite
problematic, and the efficacy of PEG-IFN monotherapy is limited.
Consensus interferon (CIFN) was designed in order to maximize
efficacy, and minimize side effects. It is composed of the most
frequently observed amino acids in each corresponding position in
the natural α IFNs. CIFN shares an 89, 30, and 60% homology with
IFN-α, IFN-β and IFN-ω, respectively (13). CIFN has been shown to be efficacious
in HCV genotype 1 patients who have failed therapy with PEG-IFN
(14). In order to increase the
duration of action, recombinant human CIFN was PEG-modified
(pegylated) by Chongqing Fujin Biomedical Co., Ltd. (Chongqing,
China). Compared with naturally occurring IFN-α, PEG-CIFN has
demonstrated enhanced in vivo antiviral activity in
cynomolgus monkeys; serum sample analyses from PEG-CIFN-treated
monkeys showed a dose-dependent antiviral activity (15). The PEG-CIFN investigated in the
current study was produced by the covalent attachment of a single
20-kDa methoxypolyethylene glycol-propionaldehyde molecule to the
N-terminus of IFN, forming a molecule with an average molecular
weight of ~40 kDa. This modification results in a longer half-life
and sustained antiviral action (15). PEG-CIFN has exhibited improved
pharmacokinetic properties compared with CIFN in monkeys and rats,
with 12- and 15-fold increases in elimination half-life, and 100-
and 10-fold reductions in serum clearance, as well as a 2.5- and
10-fold increases in the time to reach peak serum concentrations,
respectively (15).
In vitro studies have shown that the
antiviral mechanism of action of PEG-CIFN is identical to that of
CIFN: Competitive inhibition of virus binding with receptors on
target cells. Therefore, damage to target cells can be minimized.
Studies in animals have suggested that PEG-CIFN has significant
antiviral activity (16). The aim of
the current study was to determine the tolerability and antiviral
activity of PEG-CIFN in adults with HCV infection.
Materials and methods
Subjects
Forty-eight subjects from Jilin province, China were
enrolled in the study, and the characteristics of the subjects are
shown in Table I.
 | Table I.Characteristics of the study
subjects. |
Table I.
Characteristics of the study
subjects.
| Characteristic | Peginterferon α-2a
(Pegasys) | PEG-CIFN 1.0
µg/kg | PEG-CIFN 1.5
µg/kg | PEG-CIFN 2.0
µg/kg | PEG-CIFN 3.0
µg/kg |
|---|
| Male/female
ratio | 7/2 | 5/5 | 7/3 | 6/3 | 8/2 |
| Age (years, mean ±
SD) | 46.56±8.82 | 46.60±12.55 | 51.90±9.15 | 48.44±7.28 | 44.60±3.57 |
| Body mass index
(kg/m2, mean ± SD) | 23.38±2.62 | 23.83±2.16 | 23.92±1.87 | 22.64±2.28 | 22.83±2.82 |
| AST (IU/l, mean ±
SD) | 47.11±24.60 | 35.85±16.46 | 42.90±22.53 | 45.22±34.56 | 30.60±11.28 |
| ALT (IU/l, mean ±
SD) | 80.11±58.67 | 52.90±29.18 | 58.50±38.43 | 53.44±40.93 | 49.00±27.07 |
| Hemoglobin (g/dl,
mean ± SD) | 159.88±12.18 | 141.40±14.10 | 157.80±12.55 | 149.00±11.98 | 159.30±17.73 |
| White blood cells
(/mm3, mean ± SD) | 5.81±0.91 | 4.54±2.25 | 6.44±1.81 | 6.82±1.77 | 5.59±0.98 |
| Platelet count
(/mm3, mean ± SD) | 171.50±31.92 | 161.25±58.70 | 181.80±43.57 | 175.22±51.00 | 185.6±38.28 |
| Genotype (n) |
|
|
|
|
|
| 1b | 2 | 10 | 6a | 2 | 10 |
| 2a | 7 | 0 | 5 | 7b | 0 |
| Viral count
(log10IU/l, mean ± SD) | 5.90±1.12 | 6.58±0.59 | 6.27±0.95 | 6.65±0.63 | 6.50±0.74 |
| Fibroscan | 7.83±4.12 | 6.36±2.45 | 7.20±5.75 | 6.46±2.09 | 6.36±2.45 |
Inclusion criteria: Eligible subjects were 18–65
years old, with compensated liver disease due to chronic HCV
infection, plasma HCV RNA levels >2,000 IU/ml, and no history of
previous anti-HCV treatment, an absolute neutrophil count
>1,500/ml3, a platelet (PLT) count of
>90,000/mm3 and hemoglobin levels of >12 g/dl (for
women) or >13 g/dl (for men), body mass index (BMI) between 18
and 26 kg/m2 and alanine aminotransferase (ALT) level
<240 IU/l.
Exclusion criteria: Co-infection with human
immunodeficiency virus or hepatitis B, any other cause of liver
disease, severe depression or a severe psychiatric disorder, active
drug or alcohol abuse, liver cirrhosis, or hepatocellular
carcinoma, abnormal serum creatinine level, serum total bilirubin
level >34.2 µmol/l or serum albumin <35 g/l.
This clinical trial was approved by the Ethics
Committee of the First Hospital of Jilin University (Jilin, China).
All subjects provided signed informed consent prior to
enrollment.
Study design
The 48 adult subjects infected with HCV were divided
into five groups. The first group received weekly PEG-CIFN by
subcutaneous injections at a dose of 1.0 µg/kg, and were observed
for 4 weeks. If the subjects tolerated the dose, the next groups
received 1.5 and 2.0 µg/kg PEG-CIFN weekly for 14 weeks, but were
not given drug at weeks 2 and 14 due to pharmacokinetic
experiments. Therefore, in total the patients received 12 doses of
PEG-CIFN monotherapy. One group received the maximum dose of
PEG-CIFN (3.0 µg/kg) only to evaluate tolerance according to the
protocol. Pegylated IFNα-2a (peginterferon α-2a; Pegasys) was
administered at a dose of 180 µg using the same treatment protocol
as the PEG-CIFN groups and served as a positive control.
Safety was assessed by physicians of the First
Hospital of Jilin University, at weeks 2, 4 and 8 or other
(emergency) visits. If >50% of subjects had any of the following
adverse events, the dose escalation was terminated: Absolute
neutrophil count (ANC) <0.5×109/l, PLT count
<30×109/l, ALT >400 IU/l, persistent ALT rise or
accompanied by bilirubin elevation after dose titration, serum
total bilirubin >51.3 µmol/l, development of ascites, hepatic
encephalopathy, or psychiatric disorders, allergic reactions,
uncontrolled thyroid disease, diabetes mellitus, serious damage to
the heart, kidney, brain, lung, etc.
If a serious adverse event occurred during the
course of treatment, we discontinued or modified the dosage of
PEG-CIFN until the adverse event abated or decreased in severity.
The process for dose reduction consisted of two-steps. If the ANC
or PLT count was 0.5×109-0.75×109/l or
30×109-50×109/l, respectively, the treatment
dose of PEG-CIFN was reduced. If the ANC or PLT count fell below
0.5×109/l or 30×109/l, respectively, the drug
was discontinued. Drug doses could be increased once the cytopenia
resolved (when the ANC was ≥0.75×109/l or the PLT count
was ≥50×109/l).
Study drugs
PEG-CIFN was developed by Chongqing Fujin Biomedical
Co., Ltd., and produced by Beijing Kain Science and Technology Co.,
Ltd. (Beijing, China). Peginterferon α-2a was produced by F.
Hoffmann-La Roche, Inc. Agents were stored until use under
conditions recommended by the manufacturers.
Follow-up
The subjects were monitored every week by physical
examination, vital signs, inquiries of adverse reactions and weight
measurements. At weeks 4, 8 and 14, HCV RNA levels were measured by
quantitative polymerase chain reaction using the COBAS TaqMan HCV
test (Roche Molecular Systems, Pleasanton, CA, USA), which has a
low limit of quantitation (15 IU/ml). Complete blood cell counts
were measured weekly and drug dosages adjusted accordingly for
abnormalities in hemoglobin levels, ANC and PLT count. Subjects
were randomly assigned to groups. If subjects missed more than one
follow-up visit, those persons were considered non-compliant and
were removed from the study. Evaluation of tolerability index test
results for PEG-CIFN and peginterferon α-2a groups were compared
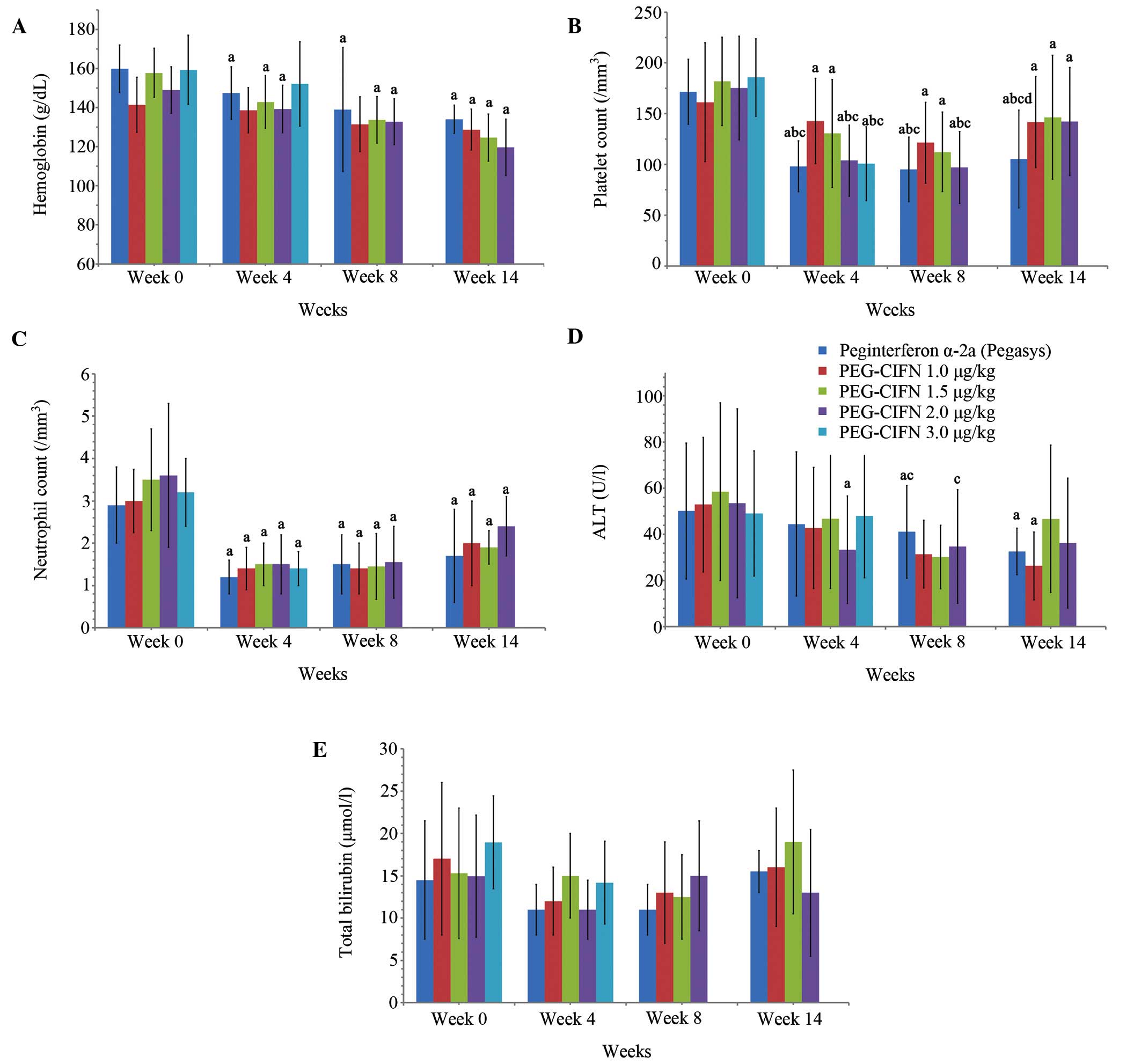
with the same dose group at week 0 (Fig.
1).
Efficacy
The primary efficacy criterion was the percentage of
subjects whose HCV RNA levels were undetectable at week 14 [early
virologic response (EVR) after 12 doses of PEG-CIFN]. The secondary
efficacy criterion was the percentage of subjects whose HCV RNA
levels were undetectable at week 4 and after a further 3 doses of
PEG-CIFN at week 8. Reductions in HCV RNA levels at weeks 4, 8 and
14 were expressed as log10.
Statistical analysis
The results were analyzed with analysis of variance
tests or Kruskal-Wallis tests using SAS software, version 9.0 (SAS
Institute, Cary, NC, USA). The results were presented as means ±
standard deviations. Multivariable logistic regression analyses
involving age, gender, baseline HCV RNA levels, baseline ALT
levels, baseline aspartate aminotransferase levels, BMI and
treatment regimens were performed to determine virologic responses
at weeks 4, 8 and 14. Virologic response was defined as an
undetectable HCV RNA level (<15 IU/ml). P<0.05 in two-sided
tests were considered to indicate a statistically significant
difference.
Results
Baseline characteristics
The study enrolled 48 HCV-infected subjects of whom
15 subjects were female (31.2%). The average age of the patients
was 47.4 years, ranging from 20 to 65 years. There were no
significant differences between the dose groups at baseline for any
of these characteristics (Table
I).
Tolerance
PLT counts
The PLT counts of each group decreased from the
baseline to week 8, and then began to rebound at week 9. The PLT
counts of all PEG-CIFN dose groups were significantly higher than
that of the peginterferon α-2a group at weeks 4, 8 and 14. Actual
numbers and percentage changes are listed in Table II.
 | Table II.Evaluation of tolerability results
for the PEG-CIFN and Peg interferonα-2a groups. |
Table II.
Evaluation of tolerability results
for the PEG-CIFN and Peg interferonα-2a groups.
| Evaluation
index | Time (week) | Peginterferon α-2a
(n=9) | PEG-CIFN 1.0 µg/kg
(n=10) | PEG-CIFN 1.5 µg/kg
(n=10) | PEG-CIFN 2.0 µg/kg
(n=9) | PEG-CIFN 3.0 µg/kg
(n=10) |
|---|
| Hemoglobin <100
g/dl, | 0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| n (%) | 4 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| 8 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
|
| 14 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| ANC <0.75 and
>0.5/mm3, | 0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| n (%) | 4 | 0 (0) | 1 (10) | 0 (0) | 1 (11.11) | 0 (0) |
|
| 8 | 1 (11.11) | 0 (0) | 1 (10) | 0 (0) |
|
|
| 14 | 0 (0) | 1 (10) | 0 (0) | 0 (0) |
|
| Platelet
count, | 0 | 171.50±31.92 | 161.25±58.70 | 181.80±43.57 | 175.22±51.00 | 185.6±38.28 |
| /mm3,
mean ± SD | 4 | 98.11±25.10 |
142.70±42.05a |
130.40±53.18a |
103.78±35.13a |
100.80±36.41a |
|
| 8 |
95.11±31.80a |
121.40±39.79a |
112.30±39.27a |
97.00±35.40a |
|
|
| 14 |
105.33±48.07a,b |
141.80±44.98a,c,d |
146.50±60.92a,c,e |
142.30±53.21a,c,f |
|
| ALT | 0 |
110.11±37.34a | 52.90±29.18 | 58.50±38.43 |
53.44±40.93 | 49.00±27.07 |
| IU/l, mean ±
SD | 4 | 80.11±58.67 |
42.80±26.28a |
46.80±30.29a |
33.33±23.36a |
|
|
| 8 |
44.44±30.82a |
31.40±14.70a | 66.60±30.57 |
34.78±24.60a |
|
|
| 14 |
41.11±16.80a |
26.33±14.65a |
46.70±31.97a |
36.20±28.14a |
|
| Total
bilirubin>34.2 µmol/l, | 0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| n (%) | 4 | 0 (0) | 0 (0) | 1 (10) | 0 (0) |
|
|
| 8 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
|
| 14 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
It was observed that the thrombocytopenic effect of
PEG-CIFN was more moderate compared with that of peginterferon α-2a
(180 µg) group. Therefore, subjects with cirrhosis and
pre-treatment thrombocytopenia may be more suitably treated with
PEG-CIFN rather than with the currently approved pegylated IFNs.
However, even in the PEG-CIFN groups, PLT counts decreased until
week 8, and then became relatively stable. This suggests that the
clinical observation time should be extended from to 4 to 8 weeks
(16).
Hemoglobin levels
The hemoglobin levels in each group remained >100
g/dl. None of the groups required adjustments in dosage due to
anemia.
Neutrophil counts
ANCs at weeks 4, 8 and 14 were significantly lower
than that at baseline (P<0.05). There were no statistically
significant differences in ANCs between any dose group at baseline,
and weeks 4, 8 and 14.
At weeks 4, 8 and 14, there were 5 subjects whose
ANCs were <0.75/mm3 but >0.5/mm3 in the
PEG-CIFN 1.0, 1.5 and 2.0 µg/kg groups and the peginterferon α-2a
group combined. According to the protocol, their doses were reduced
by 25%. After 1 week, the neutrophil counts rose to
>0.75×109/l. Original doses were then
re-instated.
PLT counts and ANCs decreased following the
initiation of treatment, and then slowly rose with increasing
treatment time or dose adjustment. The rebound in counts was
significant in all PEG-CIFN groups compared with the peginterferon
α-2a group.
Total bilirubin levels
Total bilirubin levels did not change significantly
between any group at any time point.
Fibroscan values
Fibroscan values were tested at screening and week
14 of the study. FibroScan use the vibration control of the
instantaneous elastic imaging to assess the hardness of the liver.
The larger the value of elasticity, the greater the value of liver
tissue hardness. For viral hepatitis, fibrosis was staged on a
scale as follows: F2 (stiffness 0–7.3 kPa); F2-F3 (stiffness
7.3–12.4 kPa); F3-F4 (stiffness 12.4–17.5 kPa) and ≥F4 (stiffness
≥17.5 kPa). In the PEG-CIFN 2.0 µg/kg group, the Fibroscan values
increased significantly compared with that at baseline (P<0.05).
There were no statistically significant differences between the
baseline value and the value at week 14 in any of the other dose
groups.
Ophthalmologic complications
It has been reported that IFN-associated retinopathy
occurs in 15–64% of IFN-treated patients (17). In the current study, it was found
that 35.4% of subjects had ocular adverse reactions. These were
mostly mild or moderate and gradually diminished. These events
consisted of papilledema (5 subjects), retinopathy (5 subjects),
arteriosclerosis (5 subjects), intraocular pressure and fundus
cup-disc ratio, C/D≥0.5 (2 subjects).
Other adverse events
Adverse reactions were monitored and recorded
weekly. Common adverse reactions were fatigue, poor appetite,
feverishness, musculoskeletal pain, hair loss and depression. The
incidence of the majority of the psychiatric and physical adverse
events increased with increasing doses of PEG-CIFN, and they were
higher than those of the pegylated IFN-2a group. All the events
were mild or moderate and did not result in discontinuation of
treatment.
The incidence of adverse reactions increased with
increasing dose (Table III). The
incidence of adverse reactions was highest in the 3.0 µg/kg group,
and some adverse reactions occurred in all participants in this
group (100%).
 | Table III.Common adverse reactions [n (%)]. |
Table III.
Common adverse reactions [n (%)].
| Event | PEG-CIFN 1.0 µg/kg
(%) | PEG-CIFN 1.5 µg/kg
(%) | PEG-CIFN 2.0 µg/kg
(%) | PEG-CIFN 3.0 µg/kg
(%) | Peginterferon α-2a
(%) |
|---|
| Fatigue | 5 (50) | 3 (30) | 9 (100) | 10 (100) | 4 (40) |
| Headache | 5 (50) | 3 (30) | 8 (88.9) | 8 (80) | 5 (50) |
| Insomnia | 1 (10) | 1 (10) | 2 (22.2) | 4 (40) | 1 (10) |
| Feverishness | 2 (20) | 2 (20) | 3 (33.3) | 8 (80) | 0 |
| Musculoskeletal
pain | 7 (70) | 5 (50) | 6 (66.7) | 10 (10) | 5 (50) |
| Xerostomia | 6 (60) | 4 (40) | 9 (100) | 10 (100) | 5 (50) |
| Injection site
reaction | 0 | 4 (40) | 9 (100) | 9 (90) | 0 |
| Indigestion | 0 | 0 | 2 (22.2) | 0 | 1 (10) |
| Flu-like
symptoms | 0 | 1 (10) | 0 | 4 (40) | 0 |
| Poor appetite | 0 | 7 (70) | 6 (66.7) | 3 (30) | 1 (10) |
| Hair loss | 1 (10) | 0 (0) | 0 (0) | 4 (40) | 1 (10) |
| Depression | 3 (30) | 0 (0) | 2 (22.2) | 1 (10) | 0 (0) |
Efficacy
Virologic response
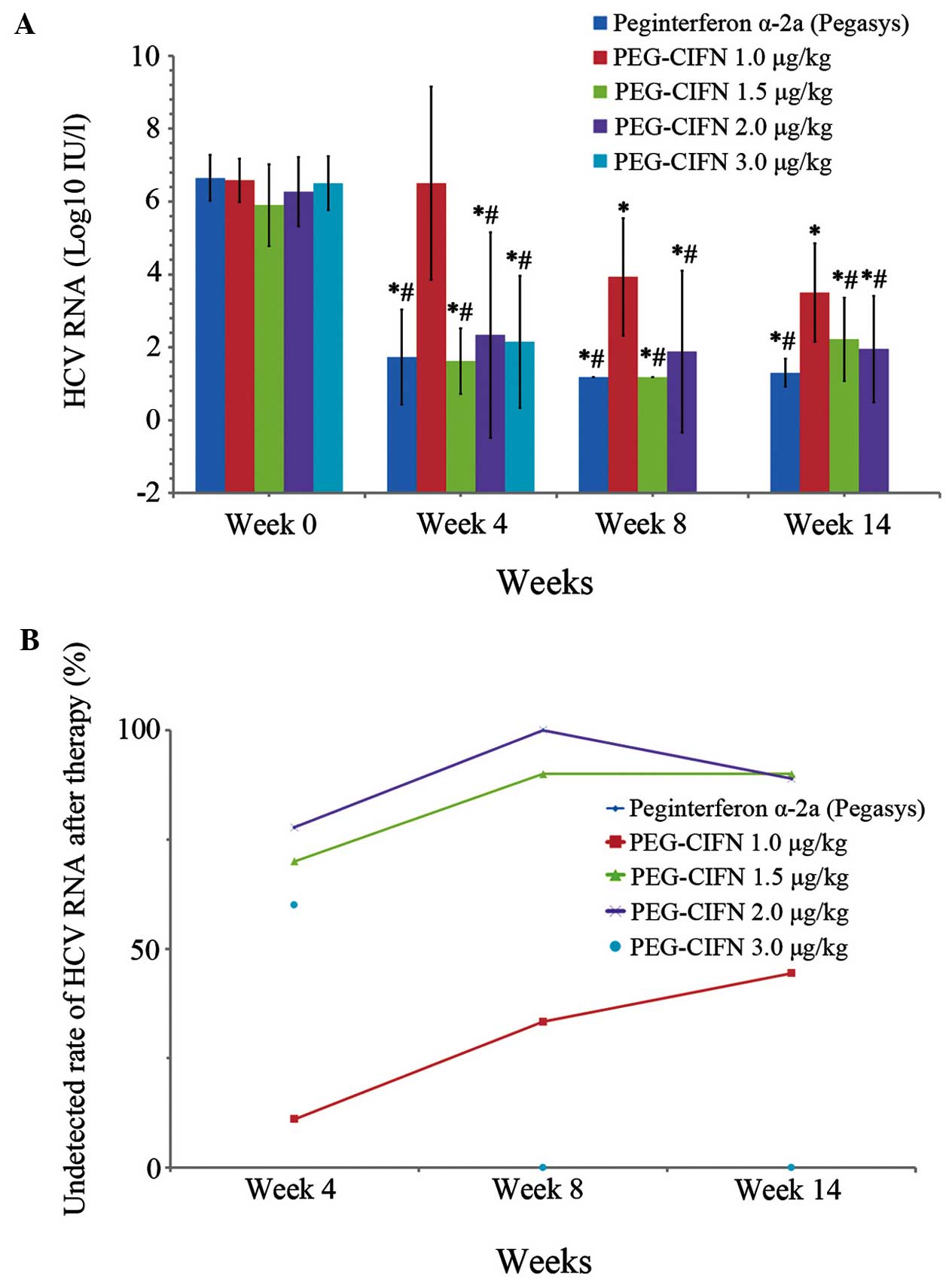
There were no significant differences in baseline
HCV RNA levels between any of the groups (Table IV). Serum HCV RNA levels decreased
significantly at weeks 4, 8 and 14 for all groups compared with
baseline (P<0.05; Fig. 2).
 | Table IV.Baseline HCV RNA levels in the
treatment groups. |
Table IV.
Baseline HCV RNA levels in the
treatment groups.
| Group | n | HCV RNA level
(log10IU/l, mean ± SD) |
|---|
| Peginterferon
α-2a | 9 | 5.90±1.12 |
| PEG-CIFN 1.0
µg/kg | 10 | 6.58±0.59 |
| PEG-CIFN 1.5
µg/kg | 10 | 6.27±0.95 |
| PEG-CIFN 2.0
µg/kg | 9 | 6.65±0.63 |
| PEG-CIFN 3.0
µg/kg | 10 | 6.50±0.74 |
The RVR rates for the PEG-CIFN 1.5, 2.0 and 3.0
µg/kg groups and for the peginterferon α-2a group were 70% (7/10),
77.8% (7/9), 60% (6/10) and 77.8% (7/9), respectively. These rates
were all significantly higher than that in the PEG-CIFN 1.0 µg/kg
group (10%, 1/10) (P<0.05).
At week 8, the extended RVR rates of the PEG-CIFN
1.0, 1.5 and 2.0 µg/kg groups and for the peginterferon α-2a group
were 10% (1/10), 70% (7/10), 77.8% (7/9) and 66.7% (6/9),
respectively.
At week 8, the HCV RNA levels decreased rate for the
PEG-CIFN 1.0, 1.5 and 2.0 µg/kg groups and for the peginterferon
α-2a group were 30% (3/10), 90% (9/10), 88.8% (8/9) and 88.8%
(8/9), respectively.
Multivariable logistic regression analyses were
performed to study the virologic responses. The virologic responses
at weeks 4, 8 and 14 were higher for the PEG-CIFN 1.5 and 2.0 µg/kg
groups and for the peginterferon α-2a group than that for the
PEG-CIFN 1.0 µg/kg group. There was no difference in virologic
response between the peginterferon α-2a and PEG-CIFN 2.0 µg/kg
groups at weeks 4 and 8. Virologic response rates increased with
increasing duration of drug administration.
Biochemical response
There were no statistically significant differences
in ALT levels between any dose groups at baseline, or at weeks 4, 8
or 14. The ALT levels were observed to decrease as the duration of
treatment increased, with no significant differences among all
values in the same dose group (P>0.05).
Discussion
In the past, treatment with pegylated IFN α-2a or
pegylated IFN α-2b, plus ribavirin, for 48 weeks was recommended
for patients infected with HCV genotype 1, the most common genotype
in the United States and Europe (18). By contrast, patients infected with
HCV genotypes 2 or 3 may be treated with ribavirin (800 mg/day) and
for just 24 weeks without compromising efficacy. These findings are
reflected in treatment guidelines for chronic hepatitis C (19,20). The
discovery of protease inhibitors as DAAs in 2002 led to the
development of numerous small molecules that block the replication
of HCV at novel antiviral targets (4,5). In
patients with HCV genotype 2 or 3 infection for whom treatment with
peginterferon and ribavirin was not an option, 12 or 16 weeks of
treatment with sofosbuvir and ribavirin was found to be effective
in early studies (21). Triple
therapy including direct-acting antiviral agents, other than
protease inhibitors, combined with pegylated IFN α-2a or pegylated
IFN α-2b, plus ribavirin) are showing promising results in clinical
trials. The possibility of decreased side effects and tolerability
with the same efficacy for PEG-CIFN indicate that it may play a
role in combination with new direct acting agents in the
future.
The virologic response rate for genotype 1 HCV
treated with dual therapy (pegylated IFN combined with ribavirin)
has been reported to be between 30 and 50% (7,8). In the
current study, the RVR rate at week 4 was 10% in the PEG-CIFN 1.0
µg/kg group, but 60% in the PEG-CIFN 3.0 µg/kg group. These results
suggest that the higher dose of PEG-CIFN may be the optimal dose
for genotype 1, and that PEG-CIFN monotherapy compares favorably
with dual therapy.
Host, virologic, and treatment factors such as viral
load, age, gender, race, state of fibrosis, BMI and HCV genotyping
have been reported to be associated with differences in response
rates to HCV treatment (22–24). In particular, the virologic response
to antiviral treatment in women has been reported to be higher with
standard-dose or high-dose peginterferon compared with low-dose
peginterferon α-2a (22,23). However, in the current study, no
significant effect of these factors on virological response was
found.
In conclusion, the rates of favorable virologic
response were similar, while the adverse event profile,
particularly the decreased degree of thrombocytopenia, was better
in patients who received PEG-CIFN compared with pegylated IFNα-2a.
This locally produced PEG-CIFN may make the treatment available to
many more patients. Limitations of this study include a small
sample size and a short observation period. Larger studies
particularly comparing PEG-CIFN in dual and triple therapy regimens
may be helpful in determining the role of PEG-CIFN in future
treatment of HCV infections.
Acknowledgements
The authors thank Medjaden Bioscience Ltd. (Hong
Kong, China) for assisting in the preparation of this manuscript.
This clinical trial was supported by National S&T Surface
Project of China (grant.oo. 81172726), Chongqing Fujin Biomedical
Co., Ltd., China and Beijing Kain Technology Co., Ltd.
References
|
1
|
Suppiah V, Moldovan M, Ahlenstiel G, Berg
T, Weltman M, Abate ML, Bassendine M, Spengler U, Dore GJ, Powell
E, et al: IL28B is associated with response to chronic hepatitis C
interferon-alpha and ribavirin therapy. Nat Genet. 41:1100–1104.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tanaka Y, Nishida N, Sugiyama M, Kurosaki
M, Matsuura K, Sakamoto N, Nakagawa M, Korenaga M, Hino K, Hige S,
et al: Genome-wide association of IL28B with response to pegylated
interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat
Genet. 41:1105–1109. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang H, Jiang YF, He SM, Sun J, Gu Q,
Feng XW, Du B, Wang W, Shi XD, Wang CY, et al: Etiology and
prevalence of abnormal serum alanine aminotransferase levels in a
general population in Northeast China. Chin Med J (Engl).
124:2661–2668. 2011.PubMed/NCBI
|
|
4
|
Hinrichsen H, Benhamou Y, Wedemeyer H,
Reiser M, Sentjens RE, Calleja JL, Forns X, Erhardt A, Crönlein J,
Chaves RL, et al: Short-term antiviral efficacy of BILN 2061, a
hepatitis C virus serine protease inhibitor, in hepatitis C
genotype 1 patients. Gastroenterology. 127:1347–1355. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pawlotsky JM, Chevaliez S and McHutchison
JG: The hepatitis C virus life cycle as a target for new antiviral
therapies. Gastroenterology. 132:1979–1998. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jacobson IM, McHutchison JG, Dusheiko G,
Di Bisceglie AM, Reddy KR, Bzowej NH, Marcellin P, Muir AJ, Ferenci
P, Flisiak R, et al: Telaprevir for previously untreated chronic
hepatitis C virus infection. N Engl J Med. 364:2405–2416. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu CH, Liu CJ, Lin CL, Liang CC, Hsu SJ,
Yang SS, Hsu CS, Tseng TC, Wang CC, Lai MY, et al: Pegylated
interferon-alpha-2a plus ribavirin for treatment-naive Asian
patients with hepatitis C virus genotype 1 infection: A
multicenter, randomized controlled trial. Clin Infect Dis.
47:1260–1269. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
de Segadas-Soares JA, Villela-Nogueira CA,
Perez RM, Nabuco LC, Brandão-Mello CE and Coelho HS: Is the rapid
virologic response a positive predictive factor of sustained
virologic response in all pretreatment status genotype 1 hepatitis
C patients treated with peginterferon-alpha2b and ribavirin? J Clin
Gastroenterol. 43:362–366. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Thomas DL, Thio CL, Martin MP, Qi Y, Ge D,
O'Huigin C, Kidd J, Kidd K, Khakoo SI, Alexander G, et al: Genetic
variation in IL28B and spontaneous clearance of hepatitis C virus.
Nature. 461:798–801. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ahlenstiel G, Booth DR and George J: IL28B
in hepatitis C virus infection: Translating pharmacogenomics into
clinical practice. J Gastroenterol. 45:903–910. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Thompson AJ, Muir AJ, Sulkowski MS, Ge D,
Fellay J, Shianna KV, Urban T, Afdhal NH, Jacobson IM, Esteban R,
et al: Interleukin-28B polymorphism improves viral kinetics and is
the strongest pretreatment predictor of sustained virologic
response in genotype 1 hepatitis C virus. Gastroenterology.
139:120–129, e18. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Clark PJ, Thompson AJ and McHutchison JG:
IL28B genomic-based treatment paradigms for patients with chronic
hepatitis C infection: The future of personalized HCV therapies. Am
J Gastroenterol. 106:38–45. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Melian EB and Plosker GL: Interferon
alfacon-1: A review of its pharmacology and therapeutic efficacy in
the treatment of chronic hepatitis C. Drugs. 61:1661–1691. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Moore CM, George M and Van Thiel DH:
Consensus interferon used to treat prior partial-responders to
pegylated interferon plus ribavirin. Dig Dis Sci. 56:3032–3037.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cai Y, Zhang Z, Fan K, Zhang J, Shen W, Li
M, Si D, Luo H, Zeng Y, Fu P and Liu C: Pharmacokinetics, tissue
distribution, excretion, and antiviral activity of pegylated
recombinant human consensus interferon-α variant in monkeys, rats
and guinea pigs. Regul Pept. 173:74–81. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cheng J: New progress in therapy of
patients with chronic hepatitis C. Zhonghua Lin Chuang Gan Ran Bing
Za Zhi. 4:1–5. 2010.(In Chinese).
|
|
17
|
Bajaire BJ, Paipilla DF, Arrieta CE and
Oudovitchenko E: Mixed vascular occlusion in a patient with
interferon-associated retinopathy. Case Rep Ophthalmol. 2:23–29.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
McHutchison JG, Lawitz EJ, Shiffman ML,
Muir AJ, Galler GW, McCone J, Nyberg LM, Lee WM, Ghalib RH, Schiff
ER, et al: Peginterferon alfa-2b or alfa-2a with ribavirin for
treatment of hepatitis C infection. N Engl J Med. 361:580–593.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dienstag JL and McHutchison JG: American
Gastroenterological Association medical position statement on the
management of hepatitis C. Gastroenterology. 130:225–230. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hadziyannis SJ, Sette H Jr, Morgan TR,
Balan V, Diago M, Marcellin P, Ramadori G, Bodenheimer H Jr,
Bernstein D, Rizzetto M, et al: Peginterferon-alpha2a and ribavirin
combination therapy in chronic hepatitis C: A randomized study of
treatment duration and ribavirin dose. Ann Intern Med. 140:346–355.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jacobson IM, Gordon SC, Kowdley KV,
Yoshida EM, Rodriguez-Torres M, Sulkowski MS, Shiffman ML, Lawitz
E, Everson G, Bennett M, et al: Sofosbuvir for hepatitis C genotype
2 or 3 in patients without treatment options. N Engl J Med.
368:1867–1877. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rodriguez-Torres M, Jeffers LJ, Sheikh MY,
Rossaro L, Ankoma-Sey V, Hamzeh FM and Martin P: Latino Study
Group: Peginterferon alfa-2a and ribavirin in Latino and non-Latino
whites with hepatitis C. N Engl J Med. 360:257–267. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shiffman ML, Salvatore J, Hubbard S, Price
A, Sterling RK, Stravitz RT, Luketic VA and Sanyal AJ: Treatment of
chronic hepatitis C virus genotype 1 with peginterferon, ribavirin,
and epoetin alpha. Hepatology. 46:371–379. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Daw MA, Elasifer HA, Dau AA and Agnan M:
The role of hepatitis C virus genotyping in evaluating the efficacy
of INF-based therapy used in treating hepatitis C infected patients
in Libya. Virol Discov. 1:32013. View Article : Google Scholar
|