Introduction
Fetal abdominal cysts are rare and few cases have
been described in the literature. With recent advances in
ultrasound techniques and increasing clinical experience, routine
ultrasound screening has facilitated the early detection of fetal
structural abnormalities (1–4). The abnormal cystic structures mainly
originate from either gastrointestinal tract or genitourinary tract
(5–9). However, since abdominal cysts may be
derived from different reproductive, urinary and digestive systems
(6–9), it becomes more difficult to accurately
determine the nature of cysts antenatally via ultrasound and
predict the postnatal outcome.
In the present study, 41 cases of fetal abdominal
cysts diagnosed by ultrasound were investigated to reveal the
differences in ultrasound image features between the various
different types of cyst and discuss how to differentiate from other
diseases with similar characteristics. Further experience to
differentiate between different types of cysts may assist in the
clinical assessment of disease outcome and determine the choice of
treatment
Materials and methods
Study subjects
A retrospective analysis of 41 cases with fetal
abdominal cyst diagnosed by routine prenatal ultrasound examination
between February 2005 and February 2015 at Women and Children's
Hospital of Linyi (Linyi, China) was performed. In the present
study, pregnant women were aged 21–39 years (mean, 24 years) with a
range of 19–39 weeks of pregnancy. Among 41 pregnant women, 36 were
primiparous whereas five were non-primiparous. When assessed during
pregnancy, abdominal circumference and cervical length were
coincident with gestational age, and no discomfort was observed in
the pregnant women. The fetal abdominal cystic cases examined in
the present study included ovarian cysts, choledochal cysts,
intestinal duplication and mesenteric cysts. Other cysts, such as
intraparenchymal cyst, cystic changes found in the urinary system
and gastrointestinal obstruction were excluded.
Instruments and methods
Volusoiv E8,730 expert, Logiq E9 (both GE Healthcare
Life Sciences, Logan, UT, USA) and Phillips iU22 color Doppler
(Phillips Healthcare, DA Best, The Netherlands) ultrasonic
diagnostic apparatus with a probe frequency of 3.0–5.0 HMz were
used. Pregnant women were positioned in the supine position for a
routine comprehensive fetal ultrasound. Ultrasound measurements
included fetal biparietal diameter, head circumference, abdominal
circumference, femur length, maximum anteroposterior diameter of
amniotic fluid or amniotic fluid index, umbilical artery
systolic/diastolic ratio, resistive index and pulsatility index.
Subsequent multi-slice scanning of the fetal abdomen was performed,
which included the fetal abdomen from the diaphragm to the pelvis
level at each cross-section, sagittal section and oblique surface.
In addition to scanning these sections, a continuous scan from one
side of the fetal abdomen slowly sliding to the other side was
performed, followed by another continuous scanning after the probe
was rotated 90°.
Results
Patient characteristics
Of 41 cases with fetal abdominal cysts identified by
regular ultrasound examination, ovarian cysts, choledochal cysts,
duplication of small intestine and mesenteric cysts were observed
in 21, 11, 6 and 3 cases respectively. All cases were confirmed by
prenatal and postnatal ultrasound, surgery or abortion.
Details of ultrasound
manifestation
Ovarian cysts
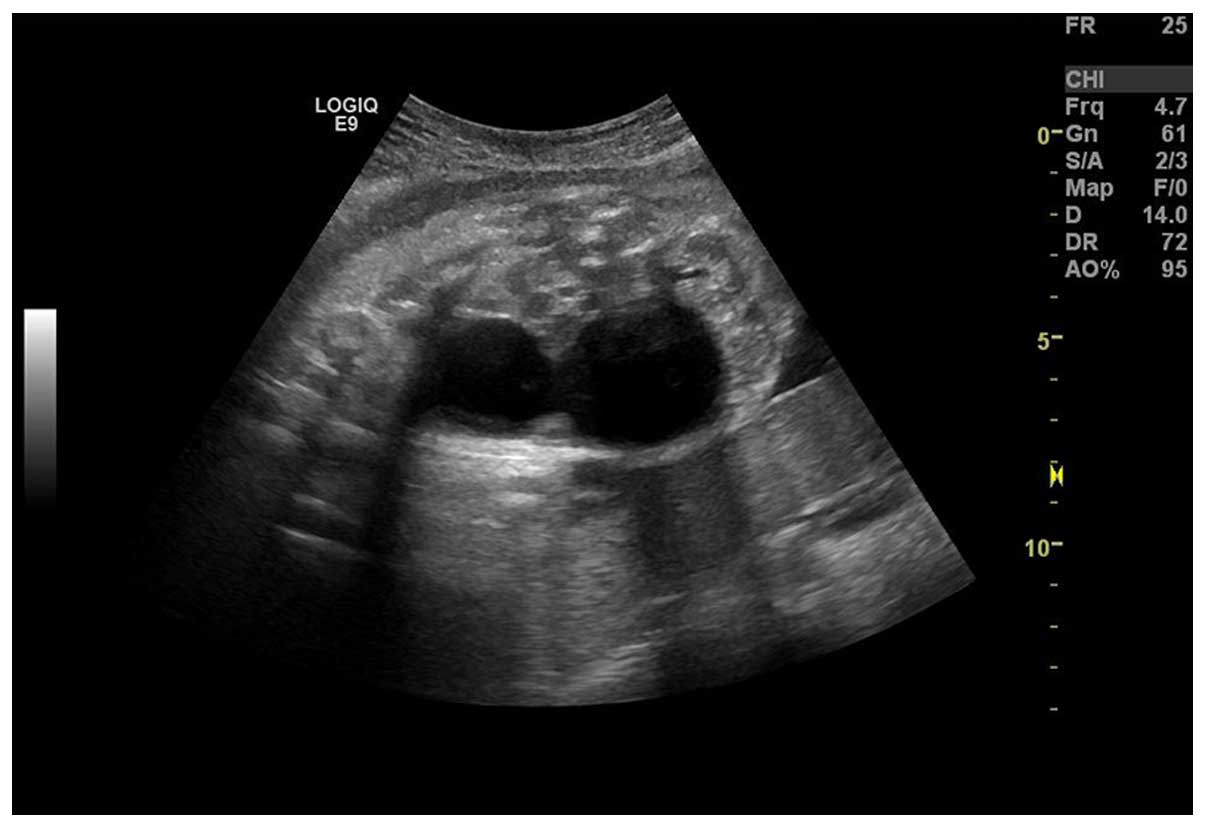
A representative ovarian cyst is presented in
Fig. 1. Among 21 cases of fetal
ovarian cysts which all appeared in female fetuses, 18 and 3 cases
exhibited cysts detected in the lower and upper abdomen,
respectively. In 20 cases of ovarian cysts found along the midline
of the abdomen, 17 were detected at one side of the bladder and one
at the midline. The majority of cases exhibited single cysts
(n=19), whereas two cases exhibited multiple cysts. There was no
significant movement of cyst location in 15 cases whereas slight
movement, predominantly up-and-down movement, was observed in six
cases. The shortest and longest diameters of the ovarian cysts were
2.1 and 5.5 cm respectively. A total of 19 cases exhibited cysts
that appeared as round-shaped, whereas two were oval-shaped, and
all of them were regular in appearance. A total of 19 cases of
cysts had a smooth contour, and only two did not. Cyst wall
thickness <0.3 cm was observed in 18 cases, whereas a thickness
of ≥0.3 cm was detected in three cases. Good sound transmission was
detected in nine cases, whereas two cases exhibited poor sound
transmission, and all cases showed posterior echo enhancement. Upon
repeated ultrasound examination, cysts were demonstrated to have
reduced in size in 12 cases, had subsequently disappeared in four
cases, exhibited no change in three cases, and had enlarged in two
cases.
Choledochal cysts
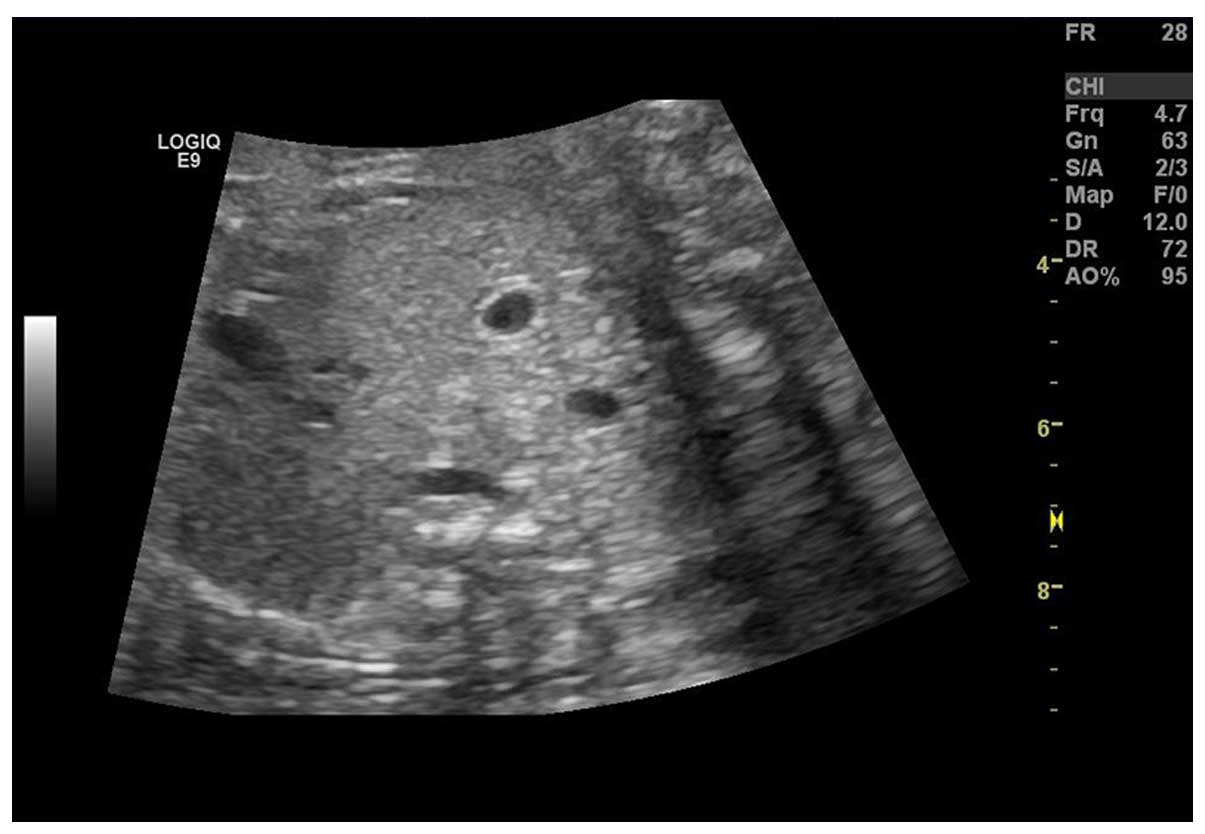
A representative choledochal cyst is presented in
Fig. 2. A total of 11 cases with
choledochal cysts were identified. This type of cyst was seen at
the hepatic hilar, behind the portal vein, in the right upper
quadrant of the abdomen. All cases presented with single cysts. The
smallest cyst size was 2.7×2.1 cm, whereas the largest one was
4.5×3.2 cm. Nine cysts were oval-shaped and two were round-shaped.
All cysts were found connected to bile ducts, whereas only eight
cases were clearly discernible and two cases were unclear.
Furthermore, two cases presented with liver echo enhancement and
three cases were complicated with intrahepatic bile duct cystic
dilatation.
Duplication of small intestine
Of six cases that presented with duplication of the
small intestine, five were observed at the lower abdomen and one on
the right abdomen. Four cases were single cysts and two cases
presented with multiple cysts. The majority of the cysts had a
certain degree of motility. The smallest cyst size was 2.6×1.8 cm
and the largest one was 6.3×2.0 cm. Three cases were round-shaped
and three cases were oblong- and oval-shaped. The wall of the cysts
was relatively thicker compared with other types of cysts, which
was closely associated with the digestive tract (Fig. 3). Three cases presented with
intestinal wall-like structure and two cases exhibited cyst wall
motility. The cyst showed a clear boundary in two cases, whereas
the boundary was unclear in four cases. One case presented with a
cyst near the intestinal dilatation.
Mesenteric cysts
Of three cases of mesenteric cysts, all were single
cysts observed at the middle of the abdomen. Two cases were
oval-shaped and one exhibited a irregular shape, which was possibly
due to the effects of pressure. The cyst wall was relatively thin
and was separated. Two cases demonstrated good sound transmission
whereas the remaining cyst showed poor sound transmission. All
cysts were movable and their shapes were altered when pressure was
applied via the ultrasound probe.
Discussion
Etiology of fetal abdominal cysts
Ovarian cysts are the most common type of abdominal
cysts in fetuses (10,11); however, the etiology remains unclear.
However, it has been postulated that the occurrence is associated
with maternal and fetal gonadotropin levels. In particular,
pregnant women who have preeclampsia, diabetes, maternal
hypertension, maternal-fetal rhesus blood group incompatibility may
have increased gonadotrophin levels, which may result in the
formation of fetal follicular cysts
Intracapsular bleeding may occur in fetal ovarian
cysts and hemorrhage may accompany a ruptured capsule. Torsion and
necrosis of the cysts and ovary may occur and the larger cysts may
compress or even cause obstruction of the gastrointestinal or
urinary tract. While the majority of cases are benign and some
cysts may disappear prior to or four months after birth, other
cysts may continue to grow and present with torsion following birth
(12). In the present study, there
were two cases that exhibited cysts that increased in size after
birth, among which one with torsion and necrosis required surgical
resection.
A choledochal cyst is also known as congenital bile
duct dilatation, primary bile duct dilatation or bile duct cystic
dilatation. Fetal choledochal cysts are rare in the Chinese
population, and neonatal incidence has been demonstrated to be
1/100,000–1/150,000 (13). Although
the etiology of the disease remains unclear, it has been suggested
that pancreaticobiliary maljunction may cause pancreatic enzyme
reflux into the biliary ducts and result in bile duct dilatation
(14). Bile duct dysplasia was also
suggested to be associated with developmental defects in periductal
connective tissues, a thin bile duct wall, or proximal bile duct
dilatation, which results from increased bile duct pressure induced
by distal common bile duct obstruction. The lack of ganglion cells
in the distal common bile duct wall may reduce the rhythmic
movement of the bile duct, and the structural and functional
abnormalities of its distal muscle may cause bile duct obstruction
and subsequently bile duct dilation.
Intestinal duplication refers to the tubular hollow
structure that appears in the small intestine mesentery. It can
occur in any part of the intestine, although it is predominantly
observed in the ileum. Different theories have been proposed for
the cause of the disease. One suggested that, during vacuole fusion
in the lumenal space, duplication may form if the lumenal space is
not fully integrated with the intestine (15). Another suggested that, during the
early development of the embryonic digestive tract, the sac- and
pouch-like diverticulum will gradually degenerate and disappear
under normal circumstances, otherwise it will form cystic
duplication (15). Other theories
have suggested that intestinal duplication may be associated with
developmental disorders of spinal cord and blood vessels (16).
Mesenteric cysts are generated from mesenteric
lymphatic swelling and cystic changes. The cyst wall is composed of
epithelial cells and connective tissues. Within the cyst, there is
chylous fluid or a small amount of blood and cellulose, and it is
sometimes referred to as a celiac mesenteric cyst. Formation of a
mesenteric cyst may be due to congenital dysplasia of the lymphatic
tissue, characterized by unusual tumor-like expansion of the
lymphatic vessels. It has also been proposed that cyst formation is
the result of lymph flow obstruction due to occlusion between the
lymphatic and venous collaterals (17). Mesenteric cysts predominantly occur
in the small bowel mesentery, which is near the mesenteric edge of
the small intestine and a number have been known to occur beyond
the mesocolon or retroperitoneal colon (18).
Ultrasound imaging features of fetal
abdominal cysts
With a certain regularity of ultrasound images,
fetal abdominal cysts were observed in female fetuses, and they
were predominantly found in the lower abdomen or pelvis, with a few
in the upper abdomen close to one side of the bladder. The majority
of the cases presented with a singular cysts, and only a few
individual cases exhibited multiple cysts. The majority of the
cysts were able to move slightly up and down and their diameters
were measured at ~4.0 cm, with only a few >6.0 cm. The shape of
the cysts was regular, and they were predominantly round- or
oval-shaped. The cysts wall was generally thin with a smooth
contour. Regular ultrasound scanning revealed that the cysts
decreased in size or disappeared over time; however, some cases did
not exhibit any significant change in size, whereas others
increased in size.
Choledochal cysts were found in the right upper
quadrant behind the portal vein and were predominantly oval-shaped.
This type of cysts was characterized by its connection with the
bile ducts and gallbladder, which was observed in 11 cases in the
present study. Intestinal duplication cysts presented as a round-
or oval-shaped mass, and a few of them were oblong- or
tubular-shaped. The cyst wall was thicker and exhibited an
intestinal wall-like structure that was closely associated with the
digestive tract. This type of cyst was movable to a certain degree
when manipulated by the ultrasound probe. In addition, it shared
the same blood vessels with the accompanying intestine, and in some
individual cases, the cyst compressed the adjacent intestine
resulting in intestinal obstruction (19,20). In
the present study, mesenteric cysts were solitary, and observed to
be unilocular or multilocular on ultrasound. These cysts tended to
be round- or oval-shaped with thin walls that lacked tension. Those
close to the intestine may form dumbbell cysts (21), and were movable or deformable when
manipulated by the ultrasound probe.
Comprehensive analysis of the fetal
abdominal cyst
Fetal abdominal cyst may be derived from different
organ systems. Since most of the characteristics are consistent
between the different types of cysts on ultrasound examination,
accurate ultrasound diagnosis remains difficult. Therefore, it is
important to identify the cystic characteristics on ultrasound
examination and integrate these with clinical observations in order
to achieve a correct diagnosis. To accurately identify the type of
fetal abdominal cyst, the following aspects should be considered
(22):
Cyst location and adjacent
structures
Ovarian cysts are commonly found at one side of the
bladder in the lower abdomen and can be found at the middle of
abdomen; however, they are rarely observed in the upper abdomen.
Choledochal cysts are typically found at the right upper quadrant
of the abdomen, close to the liver, with its rear part near the
portal vein. Since this type of cyst is fixed in position, it can
be easily differentiated from others types of cyst. Although the
locations of intestinal duplication and mesenteric cyst remain
relatively variable, they are commonly found at the middle of the
abdomen. Intestinal duplication cysts can be found along the small
intestine and are closely associated with the adjacent bowel.
Cyst morphology and tension
Ovarian cysts are predominantly round- and
oval-shaped with high tension; choledochal cyst are non-circular
and are typically oval- and oblong-shaped with low tension;
intestinal duplication cysts may be round, oval, oblong, or tubular
in shape with a certain tension; and mesenteric cysts are round-,
oval-, or dumbbell-shaped with low or no tension, thus they are
easily deformed under pressure.
Cyst wall thickness
The ovarian cyst wall is typically thinner than that
of other types of cyst, with smooth contours; the choledochal cyst
wall is slightly thicker with discontinuous wall contours that can
be seen in connection with the bile duct or gallbladder; the wall
of an intestinal duplication cyst is thicker with smooth contours
and appears as an intestinal wall-like structure, running in
parallel with the major intestinal wall, with careful observation;
and the mesenteric cyst wall is thin, with separate capsules
observed seen within the cyst.
Cyst motility
Ovarian cyst exhibit a certain degree of motility;
choledochal cysts are relatively fixed in position; mesenteric and
intestinal duplication cysts both have a greater degree of motility
when manipulated by the ultrasound probe; peristalsis is
occasionally observed in intestinal duplication cysts (23).
Follow-up observation
Larger alterations in size are observed in ovarian
cysts and the majority reduce in size or disappear. However,
choledochal cysts become larger in size on follow-up observation,
and intestinal duplication and mesenteric cysts typically do not
change in size at all during follow-up.
Ultrasound diagnosis of fetal
abdominal cyst
Ovarian cysts
Ovarian cyst can be differentiated from ureteral
dilatation, which is seen as a tubular structure visualized behind
the bladder on ultrasound that is typically accompanied by an
ipsilateral hydronephrosis. Ovarian cysts can be easily mistaken as
the bladder when there is no urine in the bladder. However, ovarian
cysts are often located at one side of the abdomen midline, whereas
the bladder is located along the lower abdomen midline near to the
anterior abdominal wall (24). On
Color Doppler ultrasonography, umbilical artery blood flow is
observed at both sides of the bladder with alterations in size from
dynamic observation. When compared with ovarian cysts, urachal
cysts are found in the superficial area close to the anterior
abdominal wall in the middle of the abdomen. Anal atresia, during
which bowel dilatation in the lower pelvis shows the ‘double leaf
sign’ image, which is different from the circular structure of
ovarian cyst (25).
Choledochal cysts
Distinct from the larger size of choledochal cysts,
which become bigger in size with increasing gestational age and are
accompanied by normal gallbladder, cystic biliary atresia tends to
be smaller with no significant alterations in cystic size.
Furthermore, the gallbladder is typically not visualized or is
small. When compared with choledochal cysts, the image exhibits a
double-bubble sign that is observed during duodenal obstruction,
accompanied by the enlarged stomach bubble. Notably, the enlarged
duodenum is not connected with the bile duct.
Intestinal duplication
Intestinal duplication can be differentiated from
small bowel obstruction where the resulting enlarged intestine is
displayed as echo-free and multiple stacked or a honeycomb-shaped
tube (26,27).
Mesenteric cysts
Distinct from omental cysts, mesenteric cysts are
small and distributed in the intestine. On occasions, the small
intestine can be observed between the cyst and the anterior
abdominal wall and it may compress the other intestine. Omental
cysts are typically found in the upper abdomen, closer to the
anterior abdominal wall, and are larger in size compared to
mesenteric cysts. Mesenteric cysts are also distinguishable from
cystic teratoma, which have a thicker cyst wall and calcification
on image analysis. In addition, cystic teratoma are typically
associated with poor sound transmission and an uneven echo.
Sometimes, hyperechoic floating fat balls or globules can be
observed inside the teratoma (28).
In conclusion, there are various different types of
fetal abdominal cyst that are distinguished by the site of
occurrence and have a differential impact on fetal development.
Prenatal ultrasound is important to identify the cause and nature
of the cyst, assist in the assessment of disease outcome and
determine the choice of treatment. An appropriate ultrasound
examination with comprehensive analysis and careful judgement would
therefore directly affect the accuracy of diagnosis and proper
treatment of the fetal abdominal cyst.
References
|
1
|
Snijders RM, Noble P, Sebire N, Souka A
and Nicolaides KH: UK multicentre project on assessment of risk of
trisomy 21 by maternal age and fetal nuchal-translucency thickness
at 10–14 weeks of gestation. Fetal medicine foundation first
trimester screening group. Lancet. 352:343–346. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nicolaides KH: Nuchal translucency and
other first-trimester sonographic markers of chromosomal
abnormalities. Am J Obstet Gynecol. 191:45–67. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Souka AP, Pilalis A, Kavalakis Y, Kosmas
Y, Antsaklis P and Antsaklis A: Assessment of fetal anatomy at the
11-14-week ultrasound examination. Ultrasound Obstet Gynecol.
24:730–734. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Malone FD, Canick JA, Ball RH, Nyberg DA,
Comstock CH, Bukowski R, Berkowitz RL, Gross SJ, Dugoff L, Craigo
SD, et al: First-trimester or second-trimester screening, or both,
for Down's syndrome. N Engl J Med. 353:2001–2011. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gabrielli S, Rizzo N and Reece EA:
Gastrointestinal and genitourinary anomaliesClinical Obstetrics.
The Fetus & Mother (3rdedn). Reece EA and Hobbins JC: Blackwell
Publishing; Malden, MA: pp. 377–400. 2007, View Article : Google Scholar
|
|
6
|
Hyett J: Intra-abdominal masses: Prenatal
differential diagnosis and management. Prenat Diagn. 28:645–655.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
McEwing R, Hayward C and Furness M: Foetal
cystic abdominal masses. Australas Radiol. 47:101–110. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nyberg DA and Neilson IR: Abdomen and
gastrointestinal tractDiagnostic Imaging of Fetal Anomalies. Nyberg
DA, McGahan JP, Pretorius DH and Pilu G: Lippincott Williams &
Wilkins; Philadelphia, PA: pp. 547–602. 2003
|
|
9
|
Hill LM: Ultrasound of fetal
gastrointestinal tractUltrasonography in Obstetrics and Gynecology.
4th. Callen PW: W. B. Saunders; Philadelphia, PA: pp. 457–487.
2000
|
|
10
|
Chang H, Li Y, Liu Y, Cao H, Zhang F and
Pan Q: Ultrasound diagnosis of fetal ovarian cysts. Zhong Hua Chao
Sheng Ying Xiang Xue Za Zhi. 11:253–254. 2002.(In Chinese).
|
|
11
|
Feng W, Cui G and Fu T: Advances in
diagnosis and treatment of fetal ovarian cysts. Contemp Med.
18:274–275. 2012.
|
|
12
|
deSa DJ: Follicular ovarian cysts in
stillbirths and neonates. Arch Dis Child. 50:45–50. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hu J, Liu Q, Wu Y, Zhou Y, Wang J and Pan
W: Clinical analysis of prenatal diagnosis of choledochal cyst in
37 infants. J Clin Pediatr. 3:858–861. 2013.
|
|
14
|
Jensen KK and Sohaey R: Antenatal
sonographic diagnosis of choledochal cyst: Case report and imaging
review. J Clin Ultrasound. 43:581–583. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Stern LE and Warner BW: Gastrointestinal
duplications. Semin Pediatr Surg. 9:135–140. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zahir I, Yusuf S, Zada F, Asif M, Akhtar N
and Abbasi MZ: Duplication Cyst in a New Born. Int J Path. 8:84–86.
2010.
|
|
17
|
Pilu G and Nicolaides KH: Gastrointestinal
tractDiagnosis of fetal abnormalities: The 18-23-week scan.
Nicolaides KH: Parthenon Publishing Group; London: pp. 741999
|
|
18
|
Kurtz RJ, Heimann TM, Holt J and Beck AR:
Mesenteric and retroperitoneal cysts. Ann Surg. 203:109–112. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lan Y, Xue X, Wang S and Liu N: Ultrasound
diagnosis of fetal intestinal duplication: a case report. Zhong Hua
Chao Sheng Ying Xiang Xue Za Zhi. 15:1192006.(In Chinese).
|
|
20
|
Pu H: Ultrasound diagnosis of fetal cecal
duplication: A case report. Zhong Guo You Sheng Yu Yi Chuan Za Zhi
She. 19:1122011.(In Chinese).
|
|
21
|
Ge Q, Li M, Li Y, Lin L and Huan F: Fetal
abdominal cystic mass of prenatal ultrasound diagnosis and
differential diagnosis. Modern Instruments & Medical Treatment.
21:10–12. 2015.(In Chinese).
|
|
22
|
Tu C: Obstetric ultrasound measurements
and diagnostics. 1st. 1. Shandong Science and Technology Press;
Jinan: 2014
|
|
23
|
Wang L, Ma X, Pan Y, Zhang H, Zhang J and
An S: The antenatal sonographic diagnosis and differential
diagnosis of fetal abdominal cysts. Chin J Clinicians (Electronic
Edition). 7:87–90. 2013.(In Chinese).
|
|
24
|
Carlson DH and Griscom NT: Ovarian cysts
in the newborn. Am J Roentgenol Radium Ther Nucl Med. 116:664–672.
1972. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cao H and Deng X: Study on the correlation
between fetal bowel dilatation and pregnancy outcomes. Chin J Med
Ultrasound. 7:577–581. 2014.(Electronic Edition).
|
|
26
|
Yang J and Ma D: Clinical and imaging
diagnosis of intestinal duplication in children. J Appl Clin
Pediatr. 23:545–547. 2008.(In Chinese).
|
|
27
|
Chen X, Huang F and Pan Y: Ultrasound
diagnosis of intestinal duplication. Chin J Ultrasound Diagn.
7:108–110. 2006.(In Chinese).
|
|
28
|
Mahomedy S, Bayat MR and Seedat M: Meat
balls: A pathognomonic ultrasound and computed tomography finding
in mature cystic teratoma. Australas Radiol. 51:(Suppl). B281–B283.
2007. View Article : Google Scholar : PubMed/NCBI
|