Introduction
Although complicated intracranial aneurysms have not
been defined thus far, they generally refer to giant, wide-necked,
tiny, irregular-shaped, dissecting, fusiform and false aneurysms
(1). Irregular aneurysm is a
complicated aneurysm that is refractory to treatment with
interventional embolization (2).
Balloon remodeling or stenting does not adequately embolize
aneurysms.
Nonetheless, the Department of Neurosurgery at Anhui
Provincial Hospital treated 37 cases of complicated intracranial
aneurysms with coils using double microcatheter technique between
July 2013 and May 2015 with satisfactory results. Thus, this method
is effective as it poses few complications.
Patients and methods
General data
Between July 2013 and May 2015, based on a
definitive diagnosis using digital subtraction angiography (DSA),
the Department of Neurosurgery at Anhui Provincial Hospital
performed interventional therapy with coils using the double
microcatheter technique on 37 cases of irregular intracranial
aneurysms, in 13 males and 24 females, aged 42–78 years (average,
57.2 years). Three of these cases were unruptured and the remaining
34 were ruptured. At admission, there were 8 cases of Hunt-Hess
grade I, 19 grade II, 9 grade III, and 1 grade IV. The aneurysms
were distributed as follows: 9 cases of anterior communicating
artery aneurysms, 13 posterior communicating artery aneurysm, 3
carotid-ophthalmic aneurysms, 2 anterior choroidal artery segmental
aneurysms, 3 aneurysms at the origin of PICA, 5 middle cerebral
artery bifurcation aneurysms, and 2 basilar artery apex
aneurysms.
Treatment protocol
The patient was placed in supine position, under
general anesthesia, followed by catheterization of the right
femoral artery using 6 F or 8 F catheter sheath. Systemic
heparinization was used. According to the position of aneurysm, a 6
F or 8 F introducer was connected to a Y-valve together with one or
two double-head Y-valves, in the petrous internal carotid artery or
vertebral artery at C2 spine level. The best operating angle was
selected according to the images reconstructed in a 3D workstation.
Under the guidance of a 0.014 micro-guide wire, the two
microcatheters were inserted in different tumor locations, heading
in different directions. The two microcatheters contain heads in
different shapes and angles that vary with irregular aneurysms. The
appropriate coils were selected to embolize the aneurysm according
to its size and shape. If imaging showed a wide-necked aneurysm
that required stent-assisted angioplasty, an 8 F introducer was
selected and three microcatheters were used simultaneously. The
first coil was woven into a basket based on preset microcatheter
varying with the size and shape of the aneurysm. The second coil
required the double microcatheter technique for alternate
embolization based on the coil shape inside the aneurysm, until it
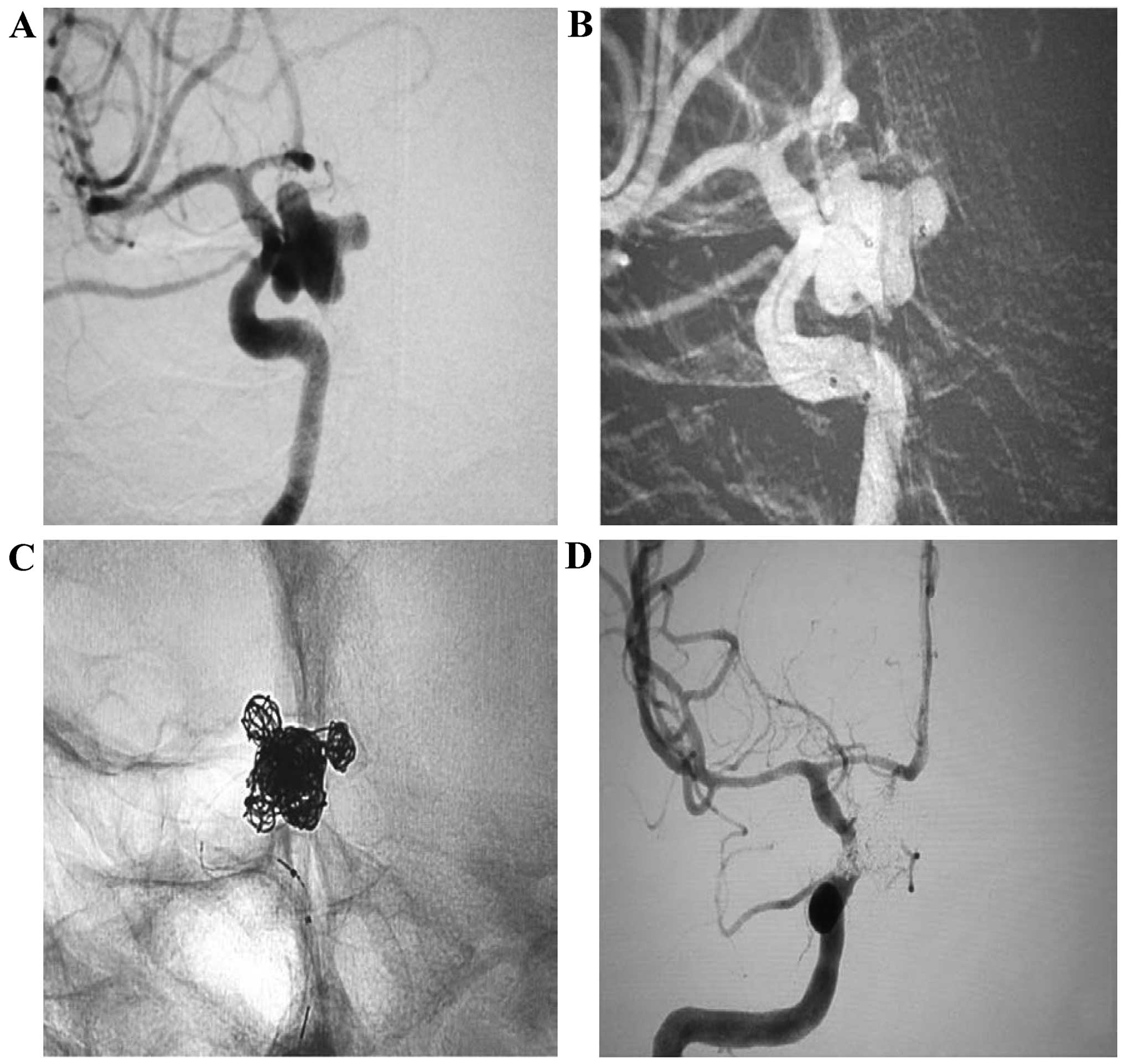
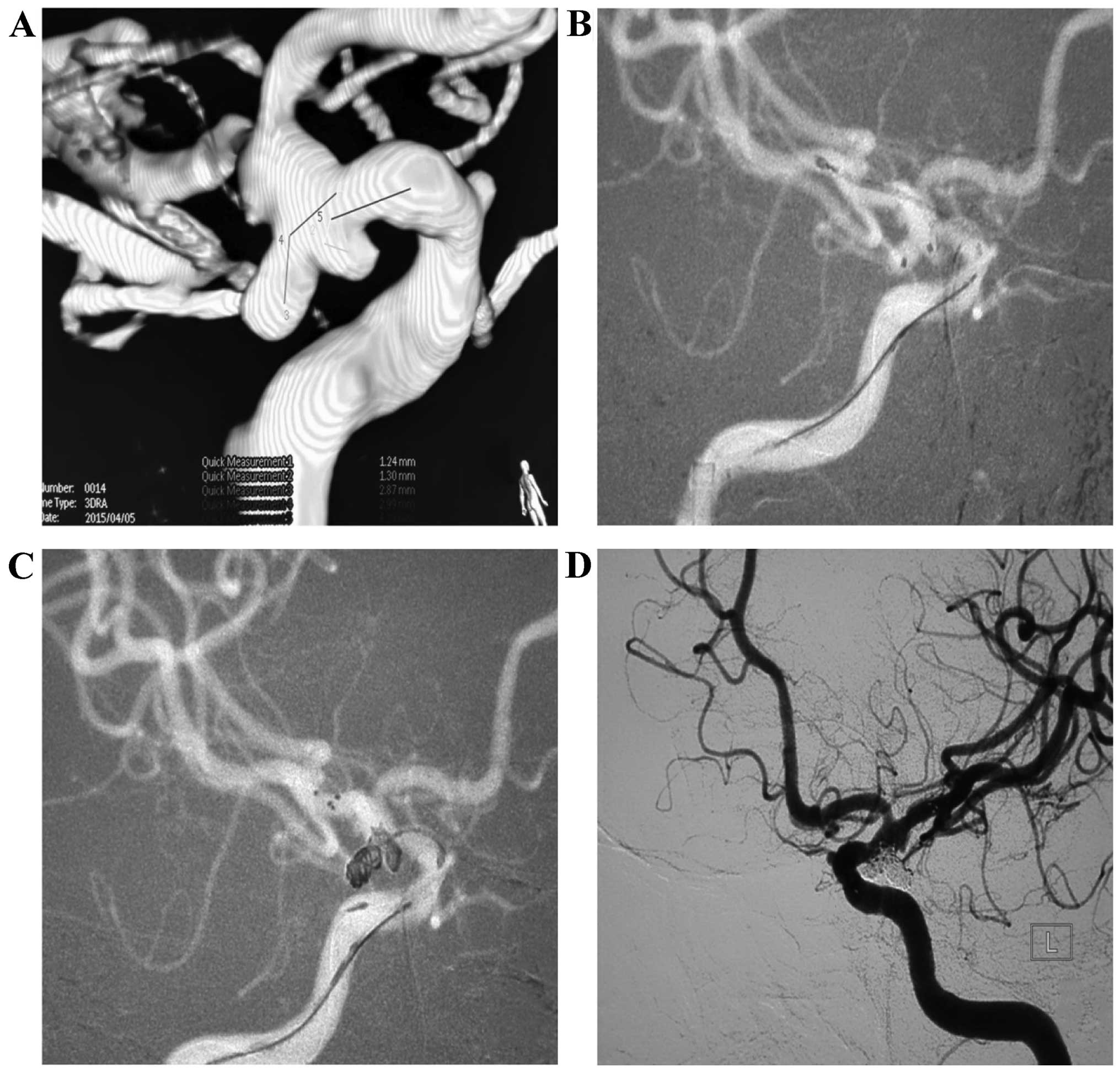
was compactly embolized (Figs. 1 and
2).
Evaluation parameters
Concerning fate of embolization, a failure to detect
the tumor and aneurysmal neck completely indicated totally compact
embolism. Detection of aneurysmal neck but not tumor indicates
near-total embolism while detection of the tumor and aneurysmal
neck suggested adequate embolism. At the time of hospital
discharge, the modified Rankin Scale score was used to evaluate the
prognosis.
Results
The 37 cases were successfully treated of
complicated irregular aneurysm. Embolization was achieved via
double microcatheter or stent-assisted double microcatheter
techniques. Immediately after the procedure, 35 of the 37 aneurysms
were compactly embolized as seen on the arteriogram and two cases
were almost completely embolized. After the procedure, the patient
did not present any neurological deficits and the general clinical
status was good. Clinical evaluation using the Modified Glasgow
Outcome Scale revealed good prognosis and all patients recovered
without any complication or death. After six months, DSA follow-up
showed no recurrence but patent vascular branches in 24 cases.
Discussion
Advances in interventional cardiology and material
science led to intravascular therapy as the primary option for
treatment of intracranial aneurysms (3). However, for irregular-shaped and
complicated intracranial aneurysms, especially lobulated or
angulated aneurysms, residual cavities are often found during
embolization (4). Despite
intervention with double microcatheter for irregular and
complicated aneurysms, few published studies are available.
Initially, the double microcatheter technique was used to treat
wide-necked complicated aneurysms. In 1998, Baxter et al
first reported the use of double microcatheter to embolize
intracranial wide-necked aneurysms with satisfactory results
(5). Over the years, new
interventional techniques have been developed, including various
intracranial stents. Currently, fewer cases of wide-necked
intracerebral aneurysm are treated using double microcatheters.
Since 2013, we used the technique to embolize irregular-shaped
aneurysms. During the procedure, the distal tips of the
microcatheter are cast into different shapes according to the shape
of the aneurysm, and the tips of the two microcatheters are
implanted in different positions inside the tumor cavities.
Embolization is then carried out using the two microcatheters
simultaneously or alternatively, resulting in embolism of
intracerebral irregular aneurysms. In case of wide-necked irregular
aneurysm, a femoral artery puncture using an 8 F sheath and 8 F
introducer is feasible along with stenting, concurrently. Our group
has successfully performed this technique using double
microcatheter or stent-assisted double microcatheter in 37 cases of
embolization involving complicated irregular aneurysms. Immediately
after the procedure, 35 cases of aneurysm were compactly embolized
on the arteriogram and two cases were almost completely embolized.
Evaluation using the Modified Glasgow Outcome Scale revealed good
prognosis without any complication or death. Follow-up after six
months with DSA revealed no recurrence but vascular branches in 24
cases.
In conclusion, the use of double microcatheters has
the following advantages (6–11): i) A single 6 F-8 F introducer can be
used to control two or three microcatheters simultaneously, which
is different from controlling a single microcatheter with
difficulty; ii) it obviates the need for reshaping the
microcatheter during late-stage embolization of aneurysms due to
changes in microcatheter position and the need for securing the
position even when the microcatheter is reshaped; iii) stent
release at the late stage of the procedure increases the difficulty
to reach the ideal position of microcatheter; iv) the rate of
compact embolism of aneurysm is greatly increased by the
simultaneous resting of the two microcatheters in different
positions inside the tumor cavity; and v) by avoiding late-stage
reshaping of microcatheter and adjustment of positions, the
duration of operation and procedural complications are dramatically
reduced.
Acknowledgements
This study was funded by the Science and Technology
Project of Anhui Province in 2015 (grant no. 1506c085017).
References
|
1
|
Lee JY, Seo JH, Cho YD, Kang HS and Han
MH: Endovascular treatment of wide-neck intracranial aneurysms
using a microcatheter protective technique: results and outcomes in
75 aneurysms. AJNR Am J Neuroradiol. 32:917–922. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ding D, Starke RM and Liu KC:
Microsurgical strategies following failed endovascular treatment
with the pipeline embolization device: case of a giant posterior
cerebral artery aneurysm. J Cerebrovasc Endovasc Neurosurg.
16:26–31. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Connolly ES Jr, Rabinstein AA, Carhuapoma
JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech
AM, Ogilvy CS, et al: American Heart Association Stroke Council;
Council on Cardiovascular Radiology and Intervention; Council on
Cardiovascular Nursing; Council on Cardiovascular Surgery and
Anesthesia; Council on Clinical Cardiology: Guidelines for the
management of aneurysmal subarachnoid hemorrhage: a guideline for
healthcare professionals from the American Heart
Association/american Stroke Association. Stroke. 43:1711–1737.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yu B, Zhang JB, Wang Z, Cai M, Yu XB and
Liu YH: Treatment of wide neck aneurysm with coils assisted by
hyper compliant balloon. Chinese J Neurol. 23:533–535. 2007.(In
Chinese).
|
|
5
|
Baxter BW, Rosso D and Lownie SP: Double
microcatheter technique for detachable coil treatment of large,
wide-necked intracranial aneurysms. AJNR Am J Neuroradiol.
19:1176–1178. 1998.PubMed/NCBI
|
|
6
|
Yu B, Hong Y, Chen LY, Xi Z, Wang MJ,
Zheng J, Kan ZY and Liu YH: Treatment of intracranial aneurysms
with coils by double micro-catheter technique. Chinese J Neurol.
29:693–69. 2013.(In Chinese).
|
|
7
|
Pu Y, Yang ZX, Yu YT, Shao Y, Miao WF and
Yu XR: The application of double microcatheter technique for the
treatment of complicated intracranial aneurysms. Chinese J Neurol.
31:31–33. 2015.(In Chinese).
|
|
8
|
Yin L, Huang Y, Wei M, Liang WL, Sun HS
and Wang SY: Double microcatheter technique for coiling
intracranial aneurysms with unfavorable configurations. Chinese J
Contemporary Neurol Neurosurg. 13:216–221. 2013.(In Chinese).
|
|
9
|
Meng L, Zuo LM, Xu SC, Zhao GY and Pang Z:
The application of double microcatheter technique for the treatment
of ruptured wide neck aneurysm at acute SAH state. Chinese J
Critical Care Med. 6:566–568. 2011.(In Chinese).
|
|
10
|
Wen HF, Zhao CX, Li JL, Wang PF and Du JC:
Double microcatheter technique for detachable coil treatment of
wide-necked and irregular intracranial aneurysms. J Intervent
Radiol. 21:890–892. 2012.
|
|
11
|
Peng Y, Xuan JG, Yang YL, Wang SN, Xia XW
and Chen RH: Application of double microcatheter technique in
endovascular b treatment of intracranial wide-necked aneurysms.
Chinese J Cerebrovascular Diseases. 7:371–373. 2009.(In
Chinese).
|