Introduction
Renal injury in asphyxiated preterm infants has a
high incidence rate (30–55%) and the mortality rate is 60–66%
(1). According to the definition of
acute kidney injury (AKI) and classification of RIFLE (2) which was presented by AKI network (AKIN)
in 2007, the likelihood of diagnosing renal injury in asphyxiated
preterm infants was poor (3).
Results obtained from at least one study showed that neutrophil
gelatinase-associated lipocalin (NGAL), kidney injury molecule-1
(KIM-1) and level of cystatin C (Cys-C) could be used as sensitive
biochemical markers for diagnosing renal injury in the early stages
(4).
The same study showed that NGAL, KIM-1 and Cys-C
in vivo levels were higher and more stable compared to serum
creatinine (Scr) and urea nitrogen levels in the early stages of
the disease (4).
Through comparative analysis, it was shown that
these three indexes (NGAL, KIM-1 and Cys-C) had peak changes at
different time-points and were closely related to the degree of
renal injury (5,6). The present study explored the
significance of using NGAL for diagnosing renal injury in
asphyxiated preterm infants and whether NGAL had a better
diagnostic value.
Materials and methods
Patients
From October 2014 to October 2015, we enrolled 48
cases of asphyxiated preterm infants which were admitted to our
hospital. We excluded cases with: i) Congenital monstrosity; ii)
inherited metabolic diseases; iii) hypoxic ischemia encephalopathy;
iv) severe asphyxia with no chance of recovery; and v) serious
conditions with expected survival time of less than one month.
There were 27 males and 21 females with an average age of 15.6±7.2
h (range, 1–24 h). Average birth weight was 2.1±0.6 kg (range,
1.7–2.3 kg).
Average gestational period was 35.6±2.4 weeks
(range, 34–37 weeks). We also enrolled 45 cases of premature
infants without renal injury after asphyxia at the same time. Of
these cases, there were 25 males and 20 females with an average age
of 15.9±7.5 h (range, 1.5–28 h). The average birth weight was
2.3±0.9 kg (range, 1.6–2.5 kg), and the average gestational period
was 35.9±2.6 weeks (range, 35–37 weeks).
Forty-five cases of normal newborn infants were also
enrolled and of those there were 26 males and 19 females with an
average age of 17.5±6.6 h (range, 2–30 h). The average birth weight
for this group was 2.6±0.8 kg (range, 2.3–3.1 kg) Differences in
gender, birth time, birth weight and gestational period for
premature infants with renal injury and that of premature infants
without renal injury had no statistical significance (P>0.05).
Differences in gender and birth time in normal newborn infants
group and that of the remaining two groups had no statistical
significance, while birth weight was significantly higher.
The present study was approved by the Ethics
Committee of Shandong Provincial Hospital. Written informed consent
of the patients guardians was obtained.
Detection index and methods
ELISA was used to detect NGAL, KIM-1, Cys-C and Scr
levels in urine. The estimated glomerular filtration rate (eGFR)
was calculated. Urine (10 ml) and blood (3 ml) specimens were
collected in 24 and 48 h. Specimens were preserved in low
temperature after centrifugation (2,500 × g for 5 min), and then
sent to the laboratory. NGAL, KIM-1 and Cys-C kits were all from
R&D Systems, Inc. (Minneapolis, MN, USA). Enzyme-labeled
instrument was purchased Bio-Tek ELx800 (Bio-Tek Instruments, Inc.,
Winooski, VT, USA). The centrifuge used was purchased from Beckman
Coulter (Brea, CA, USA). Fully automatic chemistry analyzer was
used to detect Scr, Hitachi 7170A (Hitachi, Tokyo, Japan).
Operations were strictly carried out as per the
manufacturer's instructions. Instructions included compounding
standard samples, adding specimen, incubating, allocating
transfusion, washing, adding enzyme, incubating, washing,
developing color, terminating, determining, drawing standard curve
with curve expert 1.3 using concentration of standard samples as
ordinates and corresponding optical density (OD) values as
abscissa, calculating curve equation, and then obtaining actual
concentration of samples to be detected through substituting OD
values to equation to obtain concentration of each sample which was
used to multiply dilution ratio. eGFR was calculated using
simplified MDRD software (Germantown,MD, USA) (https://www.niddkrepository.org/studies/mdrd/).
Statistical analysis
We analyzed data using SPSS 19.0 statistical
software (SPSS, Inc., Chicago, IL, USA). Measurement data were
indicated as mean ± standard deviation. We compared among groups
using one-way ANOVA and countable data were presented as samples or
percentage. The χ2 test was used to compare among
groups. Analysis of diagnostic susceptibility and specificity of
NGAL, KIM-1 and Cys-C were realized using receiver operating
characteristic curve (ROC). P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparisons of observation index of
each group
NGAL, KIM-1 and Cys-C levels in the group of
asphyxiant renal injury at 24 and 48 h were markedly higher than
the other two groups (P<0.05). Changes in Scr and eGFR within 24
h were not significant (P>0.05). Scr level in the renal injury
group in 48 h was significantly elevated while eGFR level decreased
considerably (P<0.05) (Table
I).
 | Table I.Comparison of observation index of
each group. |
Table I.
Comparison of observation index of
each group.
| Groups | 24 h | 48 h |
|---|
| Groups |
|
|
|---|
|
| NGAL (ng/ml) | KIM-1 (ng/l) | Cys-C (ng/mg) | Scr (µmol/l) | eGFR (ml/min) | NGAL | KIM-1 | Cys-C | Scr | eGFR |
|---|
| Renal injury | 55.8±15.4 | 33.4±13.6 | 23.6±10.8 | 65.8±20.3 | 105.8±23.5 | 196.3±36.7 | 76.7±25.3 | 65.5±23.4 | 194.6±42.5 | 82.5±21.4 |
| Premature infant | 12.9±4.2 | 7.5±1.4 | 9.2±1.7 | 62.3±24.5 | 109.3±24.6 | 15.7±5.3 | 8.2±1.9 | 9.7±1.5 | 65.7±25.9 | 103.2±29.7 |
| Normal | 10.6±4.9 | 6.3±1.7 | 8.7±1.3 | 56.7±23.6 | 114.5±23.8 | 11.2±5.4 | 6.9±1.6 | 8.6±1.4 | 53.4±22.3 | 115.7±26.6 |
| F-value | 16.825 | 12.364 | 10.523 | 0.657 | 0.754 | 34.527 | 25.802 | 16.957 | 9.635 | 6.754 |
| P-value | <0.001 | <0.001 | <0.001 | 0.438 | 0.632 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
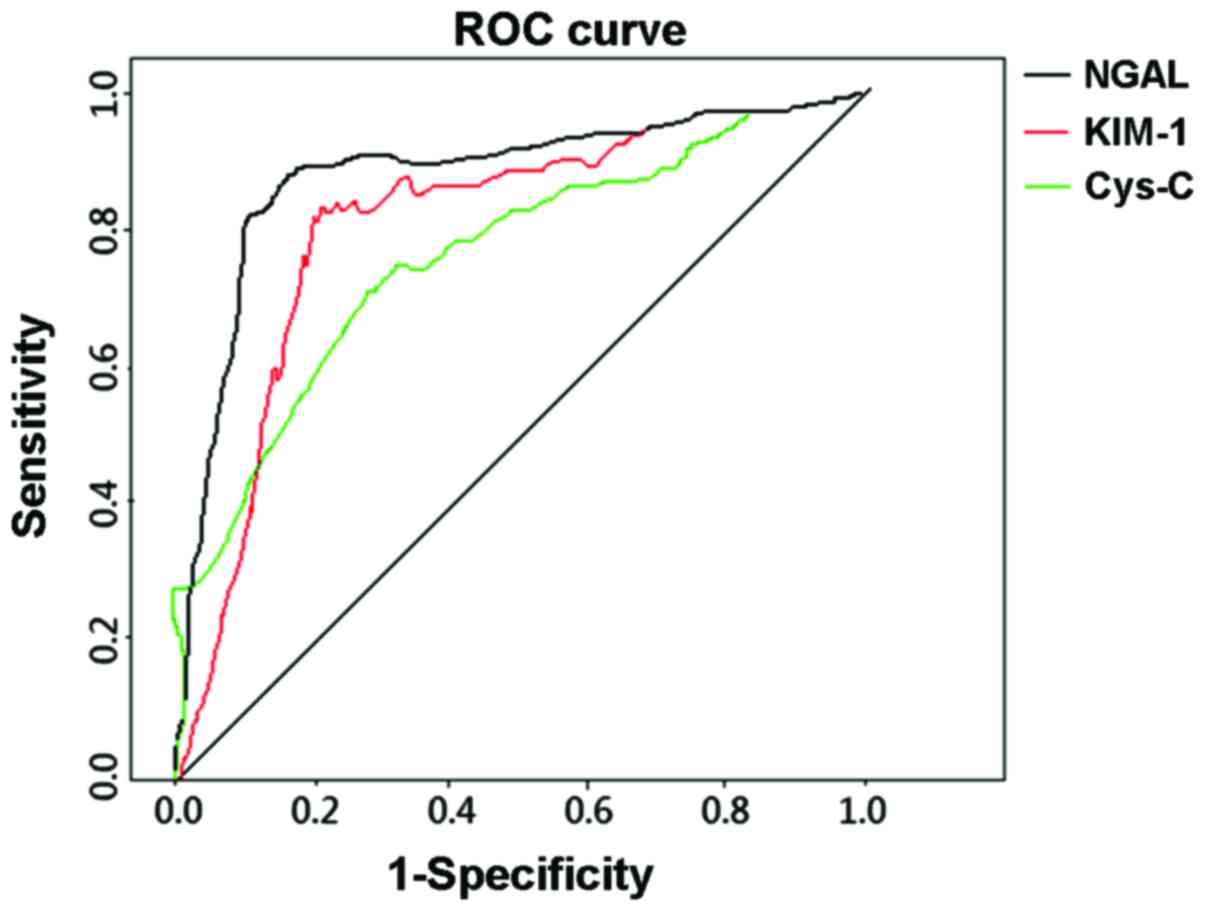
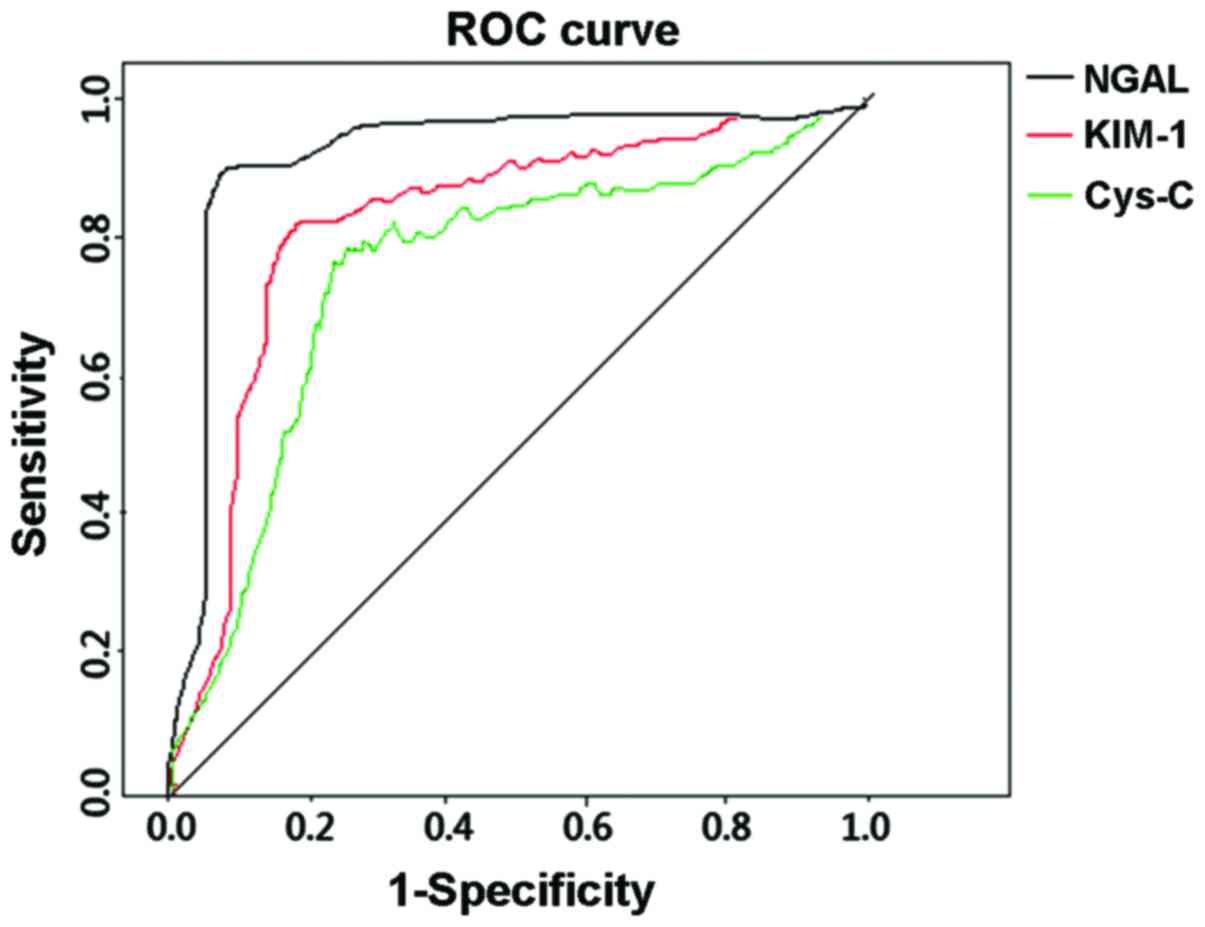
Analysis of NGAL, KIM-1 and Cys-C
Area under the curve (AUC) for NGAL in the group of
asphyxiant renal injury at 24 and 48 h was significantly higher
than KIM-1 and Cys-C. Susceptibility and specificity was improved
(Table II, and Figs. 1 and 2).
 | Table II.Analysis of NGAL, KIM-1 and Cys-C. |
Table II.
Analysis of NGAL, KIM-1 and Cys-C.
|
| 24 h AUC | 95% CI | Susceptibility
(%) | Specificity (%) | Cut-off | 48 h AUC | 95% CI | Susceptibility
(%) | Specificity (%) | Cut-off |
|---|
| NGAL | 0.836 | 0.634–0.947 | 86.4 | 83.7 | 48.5 ng/ml | 0.892 | 0.714–0.968 | 87.5 | 84.3 | 123.7 ng/ml |
| KIM-1 | 0.812 | 0.526–0.936 | 82.3 | 76.7 | 27.4 ng/l | 0.856 | 0.587–0.942 | 84.5 | 79.8 | 66.5 ng/l |
| Cys-C | 0.803 | 0.475–0.921 | 81.4 | 75.3 | 18.6 ng/mg | 0.844 | 0.496–0.939 | 82.2 | 77.9 | 58.9 ng/mg |
Discussion
Compared with glomerulus, proximal tubular in
premature infants has poorer development, reabsorption and its
ability to treat water-electrolyte as well as acid-base balance is
seriously undermined. Compared to mature infants, premature infants
with lower gestational age and lower birth weight suffer from lower
rate of nephron and lower glomerular filtration. In premature
infants, GFR that influence renal vasoconstriction and relaxation
is usually low. Thus AKI is more likely to happen in premature
infant (7–9).
NGAL is involved in the formation and reparation of
renal tubular epithelial cells. It has been established that NGAL
level is high in proximal tubular epithelial cells and in the case
of AKI, renal tubular epithelial cells are damaged and NGAL levels
in blood and urine is very high (10).
Devarajan showed that in renal ischemia reperfusion
injury model in rat, NGAL could be detected when AKI occurs for 2
h. However, at the same time, Scr level remained at its normal
level. It was concluded that compared with Scr, NGAL was more
sensitive and a better marker for early detection of AKI (11).
Results obtained by Yavuz et al on 22 cases
of burned children who were admitted to hospital within 12 h
revealed that there were no significant differences between the Scr
level in the 1–5 days AKI group and that in the non-AKI group. By
contrast, blood and urine NGAL levels increased considerably in the
AKI group which indicated the sensitivity of NGAL for early
detection of AKI (12).
Results obtained from another related study on 60
cases of neonates in critical condition showed that NGAL level had
little to do with sepsis (13). In
that study, according to diagnostic code of AKIT, the cases were
divided into the AKI group and the non-AKI group. The results of
that study revealed that, the blood NGAL level markedly increased
in the early stages of AKI. It was shown that when the NGAL level
in blood surpassed the 117.5 ng/ml mark it was an indication of
AKI. Susceptibility was 82.0% and specificity was 88.5% (13).
The results presented by Askenazi et al
demonstrated that the baseline assessment of urine NGAL in
premature infant and gestational age were negatively correlated,
while an elevated level of urine NGAL and the degree of renal
injury were positively correlated (14).
KIM-1 is a member of the immunoglobulin superfamily.
KIM-1 is a transmembrane glycoprotein which comprised mucoprotein
and immunoglobulin. It usually engages in recovering process of
renal tubule epithelial cells, renal interstitial fibrosis and
immunological reactions. It has the functions of adhering and
cleaning up the apoptotic cells (15). Under normal physiological conditions,
KIM-1 expression level in normal kidney tissue fluctuates between
zero to very low. In a case of AKI caused by ischemia or toxic
kidney injury, KIM-1 expression level in kidney tissue was markedly
increased (16). When proximal
tubular injury occurs, extracellular KIM-1 enters into urine in the
form of soluble fragment which is relatively stable and easy to
detect (17).
Cys-C is a tyep of cystatin, which is produced by
all the karyocytes in the body. It is a non-glycosylated alkaline
protein with a low molecular weight that can only be cleaned up by
passing through glomerular filtration. It is reabsorbed in proximal
convoluted tubule, then decomposed totally and metabolized. It is
an endogenous marker that reflects GFR (18).
We showed that NGAL, KIM-1 and Cys-C levels in the
group of asphyxiant renal injury within 24 and 48 h were markedly
higher than the two other groups. Changes in Scr and eGFR within 24
h were not significant. Scr of renal injury within 48 h was
markedly elevated while eGFR reduced obviously. Our results
indicated that urine NGAL, KIM-1 and Cys-C could respond to AKI in
the early stage. Compared with KIM-1 and Cys-C, AUC of NGAL in the
group of asphyxiant renal injury within 24 and 48 h was obviously
higher and both susceptibility and specificity was improved.
Results also suggested that urine NGAL may have higher diagnostic
accuracy compared with KIM-1 and Cys-C.
In conclusion, the critical value of detecting urine
NGAL in renal injury in asphyxia preterm infants at 24 h was 48.5
ng/ml, susceptibility was 86.4% and specificity was 83.7%. The
critical value of detecting urine NGAL in renal injury in asphyxia
preterm infants within 48 h was 123.7 ng/ml, susceptibility was
87.5% and specificity was 84.3%.
References
|
1
|
Beck S, Wojdyla D, Say L, Betran AP,
Merialdi M, Requejo JH, Rubens C, Menon R and Van Look PF: The
worldwide incidence of preterm birth: a systematic review of
maternal mortality and morbidity. Bull World Health Organ.
88:31–38. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ronco C, Levin A, Warnock DG, Mehta R,
Kellum JA, Shah S and Molitoris BA: AKIN Working Group: Improving
outcomes from acute kidney injury (AKI): report on an initiative.
Int J Artif Organs. 30:373–376. 2007.PubMed/NCBI
|
|
3
|
Sweetman DU and Molloy EJ: Biomarkers of
acute kidney injury in neonatal encephalopathy. Eur J Pediatr.
172:305–316. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Urbschat A, Obermüller N and Haferkamp A:
Biomarkers of kidney injury. Biomarkers. 16:(Suppl 1). S22–S30.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Peralta CA, Katz R, Bonventre JV,
Sabbisetti V, Siscovick D, Sarnak M and Shlipak MG: Associations of
urinary levels of kidney injury molecule 1 (KIM-1) and neutrophil
gelatinase-associated lipocalin (NGAL) with kidney function decline
in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Kidney
Dis. 60:904–911. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Duan SB, Liu GL, Yu ZQ and Pan P: Urinary
KIM-1, IL-18 and Cys-c as early predictive biomarkers in
gadolinium-based contrast-induced nephropathy in the elderly
patients. Clin Nephrol. 80:349–354. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dagher PC, Herget-Rosenthal S, Ruehm SG,
Jo SK, Star RA, Agarwal R and Molitoris BA: Newly developed
techniques to study and diagnose acute renal failure. J Am Soc
Nephrol. 14:2188–2198. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sutherland MR, Gubhaju L, Moore L, Kent
AL, Dahlstrom JE, Horne RS, Hoy WE, Bertram JF and Black MJ:
Accelerated maturation and abnormal morphology in the preterm
neonatal kidney. J Am Soc Nephrol. 22:1365–1374. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Walker MW, Clark RH and Spitzer AR:
Elevation in plasma creatinine and renal failure in premature
neonates without major anomalies: terminology, occurrence and
factors associated with increased risk. J Perinatol. 31:199–205.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Peco-Antić A, Ivanišević I, Vulićević I,
Kotur-Stevuljević J, Ilić S, Ivanišević J, Miljković M and Kocev N:
Biomarkers of acute kidney injury in pediatric cardiac surgery.
Clin Biochem. 46:1244–1251. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Devarajan P: Neutrophil
gelatinase-associated lipocalin (NGAL): a new marker of kidney
disease. Scand J Clin Lab Invest Suppl. 241:89–94. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yavuz S, Anarat A, Acartürk S, Dalay AC,
Kesiktaş E, Yavuz M and Acartürk TO: Neutrophil gelatinase
associated lipocalin as an indicator of acute kidney injury and
inflammation in burned children. Burns. 40:648–654. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
El-Farghali OG, El-Raggal NM, Mahmoud NH
and Zaina GA: Serum neutrophil gelatinase-associated lipocalin as a
predictor of acute kidney injury in critically-ill neonates. Pak J
Biol Sci. 15:231–237. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Askenazi DJ, Koralkar R, Levitan EB,
Goldstein SL, Devarajan P, Khandrika S, Mehta RL and Ambalavanan N:
Baseline values of candidate urine acute kidney injury biomarkers
vary by gestational age in premature infants. Pediatr Res.
70:302–306. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kirk R: Renal fibrosis: KIM-1 expression
links kidney injury with CKD in mice. Nat Rev Nephrol. 9:6272013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cruz DN, Goh CY, Haase-Fielitz A, Ronco C
and Haase M: Early biomarkers of renal injury. Congest Heart Fail.
16:(Suppl 1). S25–S31. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sabbisetti VS, Ito K, Wang C, Yang L,
Mefferd SC and Bonventre JV: Novel assays for detection of urinary
KIM-1 in mouse models of kidney injury. Toxicol Sci. 131:13–25.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dorum S, Silfeler I, Dorum BA, Silfeler
DB, Canbak Y and Say A: Reference values of serum cystatin-C for
full-term and preterm neonates in Istanbul. Indian J Pediatr.
79:1037–1042. 2012. View Article : Google Scholar : PubMed/NCBI
|