Introduction
Pregnancy-induced hypertension (PIH) is a syndrome
that occurs during pregnancy. PIH is the primary cause of maternal,
neonatal and fetal mortality and morbidity (1). PIH is defined by a diastolic blood
pressure (DBP) >90 mmHg and systolic blood pressure (SBP)
>140 mmHg, and causes complications in 6–10% of pregnancies.
Therefore, PIH is classified as either mild (SBP, 140–149 mmHg; and
DBP, 90–99 mmHg), moderate (SBP, 150–159 mmHg; and DBP, 100–109
mmHg) or severe (SBP, ≥160mmHg; and DBP, ≥110 mmHg) (2,3).
According to the Canadian Hypertension Society (4), an important condition associated with
PIH is gestational hypertension and preeclampsia (PE), a common
health problem with adverse effects for fetus and mother (5). It has been indicated that patients with
PIH may be at a higher long-term risk of other medical conditions
in later life, including diabetes mellitus, hypertension, kidney
disease and cardiovascular disease (6). Indeed, a positive association between
PIH and hypertensive diseases was observed in a study of 3,593
women with PE during their first singleton pregnancy (7).
It has been suggested that PIH is impacted by
endothelial cell injury occurring during maternal and blood vessel
formation disorder in the placenta, which may result from different
cell factors generated in placental hypoxia (8). However, the pathogenic molecular
mechanism of PIH is not yet fully understood and therefore there is
difficulty in monitoring disease progress. PIH is a genetic disease
that develops through a multi-step process (9,10).
Significant progress in the development of novel therapeutic agents
may improve the understanding of the molecular basis of
gene-disease interactions. Although a number of challenges remain
regarding the prediction, prevention and management of PIH,
previous studies have suggested that serum-based microRNAs (miRNAs)
may be potential biomarkers or effective therapy for early
detection, diagnosis and follow-up of severe PE (11,12).
This may provide novel suggestions for the management of PIH.
The discovery of miRNAs was a landmark milestone in
molecular biology and pharmacology. miRNAs are a series of small
(18–24 nucleotides) endogenous noncoding single-stranded RNAs,
which can post-transcriptionally regulate target mRNAs by a
non-perfect pairing of 6–8 nucleotides (13). Target mRNAs are subsequently degraded
by the formation of RNA-induced silencing complex, which suggests
that miRNAs may control a range of different biological functions
including cellular differentiation, proliferation and apoptosis
(14). A higher expression of miRNA
has been identified in the placenta of patients with PIH,
suggesting that they may have a function in the placenta of
patients with severe PE. These miRNAs include miR-92b, miR-342-3p,
miR-197, miR-25, miR-296-5p, miR-26a, miR-202, miR-198, miR-95 and
miR-204-5p (15–17), and alterations in miRNA expression
may serve a critical role in disease progression due to the
negative transcriptional or post-transcriptional regulation of
important target genes (18). The
present study aimed to examine whether the aforementioned miRNAs
that underwent significant alterations in expression during the
course of PIH are regulated by miRNAs.
In the present study, differentially expressed
miRNAs were investigated in the serum of patients with PIH using
reverse transcription-quantitative polymerase chain reaction
(RT-qPCR). The results indicate that miR-204-5p may affect cell
proliferation, cell apoptosis and cell cycle progression in the
hypoxic model in vitro. The results of the present study may
be therefore be the basis for further studies to examine the
pathophysiological mechanism and identify PIH biomarkers in order
to improve the diagnosis, prevention and treatment of PIH.
Materials and methods
Patient characteristics, clinical
features and serum harvest
For the identification of PIH-specific serum miRNAs,
a total of 40 patients were selected: 20 healthy female volunteers
as controls and 20 female patients with PIH, were recruited from
the Third Affiliated Hospital, Sun Yat-sen University (Guangzhou,
China; Table I) between December
2014 and March 2015, having given informed consent to be included
in the present study. Differentially expressed miRNAs were directly
validated using RT-qPCR according to previous research (19). As presented in Table I, the exclusion criteria for both
groups included: Patients with kidney disease or essential
hypertension, a history of alcohol or drug abuse, and illegal drug
addiction within the 6 months prior to signing the informed
consent. Furthermore, the PIH patients were all pathologically
diagnosed by doctors and all blood samples were collected prior to
any surgery, chemotherapy and/or radiation treatment.
 | Table I.Characteristics of study subjects in
the control and PIH groups. |
Table I.
Characteristics of study subjects in
the control and PIH groups.
|
|
|
|
| Onset |
|---|
|
|
|
|
|
|
|---|
| Group | Age, years | Height, cm | Weight, kg | GA, weeks | BP, mmHg |
|---|
| Control | 25.84±3.56 (range,
23–34) | 161.54±13.28 | 67.35±7.68 | 35.32±2.79 | 140.23±18.32 |
| PIH | 27.23±6.42 (range,
21–34) | 165.32±17.45 | 67.29±6.83 | 34.92±1.98 | 200.35±12.91 |
From each patient, 5 ml venous blood was collected
on first admission to the hospital. Blood was drawn into a sterile
tube without anticoagulant to harvest cell-free serum. The tube was
left in a standing position for 20 min prior to centrifugation at
20°C and 1,500 × g for 10 min. The supernatant serum was
quickly removed by pipette and stored immediately at −80°C until
analysis. The present study was approved by the Ethics Committee
from the Third Affiliated Hospital, Sun Yat-sen University and a
signed informed consent form was obtained from each participant
prior to the study.
Cell culture and treatment
The human choriocarcinoma (JAR) cell line was
obtained from the American Type Culture Collection (ATCC; Manassas,
VA, USA). JAR cells were cultured for 24 h in growth media
containing high glucose-Dulbecco's modified Eagle's medium and
supplemented with 10% fetal bovine serum (Hyclone; GE Healthcare
Life Sciences, Logan, UT, USA) and 1% penicillin/streptomycin
(Mediatech, Inc., Manassas, VA, USA) in a humidified atmosphere of
5% CO2 and a temperature of 37°C.
Following dilution into single cell suspensions and
seeding into 96-well plates (1×104 cells/well), a JAR
cell hypoxic model was induced using an AnaeroPack®
system (Mitsubushi Gas Chemical America, Inc., New York, NY, USA)
for 48 and 72 h, respectively, prior to harvesting for total RNA
isolation (20).
Total RNA isolation and reverse
transcription
TRIzol® reagent (Invitrogen; Thermo
Fisher Scientific, Inc., Waltham, MA, USA) was used to prepare
total RNA and subsequently, 75% ethanol replaced isopropanol for
RNA precipitation, according to the manufacturer's protocol. RNA
quality was determined using a NanoDrop 1000 spectrophotometer
(Thermo Fisher Scientific, Inc., Wilmington, DE, USA). A total of 1
µg RNA was reverse-transcribed into cDNA using a DBI
Bestar® qPCR RT kit (DBI Bioscience, Ludwigshafen,
Germany) according to the manufacturer's protocol.
Quantitative polymerase chain reaction
(qPCR) of mature miRNAs
RT-qPCR was performed using a 7500 Fast Real-Time
PCR System Light Cycler (Applied Biosystems; Thermo Fisher
Scientific, Inc.). The 20 µl PCR reaction included 1 µl reverse
transcription product (1:5), 0.5 µl sense primer, 0.5 µl universal
reverse primer and 10 µl DBI-2043 Bestar® Real time PCR
Master Mix (DBI Bioscience). The reactions were incubated at 94°C
for 2 min in a 96-well optical plate, followed by 40 cycles of 94°C
for 20 sec, 8°C for 20 sec and 72°C for 20 sec. All reactions were
completed in triplicate and primer sequences are listed in Table II. mRNAs were quantified using the
2−ΔΔCq formula (21).
 | Table II.Sequences of primers used to validate
selected miRNAs. |
Table II.
Sequences of primers used to validate
selected miRNAs.
| Gene | Sequence
(5′-3′) |
|---|
| miR-197-3p | F:
ACACTCCAGCTGGGTTCACCACCTTCT |
| miR-26a-5p | F:
ACACTCCAGCTGGGTTCAAGTAATCCA |
| miR198 | F:
ACACTCCAGCTGGGGGTCCAGAGG |
| miR-204-5p | F:
ACACTCCAGCTGGGTTCCCTTTGTCA |
| miR-92 | F:
TATTGCACTCGTCCCGGCCTCC |
| miR-95-5p | F:
ACACTCCAGCTGGGTCAATAAATGTC |
| miR-202-3p | F:
ACACTCCAGCTGGGAGAGGTATAGG |
| miR-296-5p | F:
ACACTCCAGCTGGGAGGGCCCCCC |
| For all | R:
TGGTGTCGTGGAGTCG |
| U6 | F:
CTCGCTTCGGCAGCACA |
|
| R:
AACGCTTCACGAATTTGCGT |
Cell proliferation detection
miR-204-5p inhibitor (Shanghai GenePharma, Ltd.,
Shanghai, China) was transfected into the hypoxic JAR cells using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.) prior to incubation in DMEM without FBS at 37°C
for 48 h. JAR cells were then transfected with 100 nM miR-204-5p
inhibitor and subjected to the hypoxia precondition for 48, 72 and
96 h respectively. Then, 100 µl Cell Counting Kit-8 solution
(Dojindo Molecular Technologies, Inc., Kumamoto, Japan) was added
to each well and incubation was completed for 1 h at 37°C.
Absorbance was measured at 450 nm using a microplate reader.
Apoptosis assay
Following transfection of the miRNA inhibitor in the
hypoxic environment for 48 h, quantification of the apoptotic cells
was completed using the Annexin V-FITC/PI apoptosis detection kit
(Merck Millipore, Darmstadt, Germany). JAR cells were collected by
trypsin digestion method (22),
washed with phosphate buffered saline (PBS) and re-suspended in 200
µl binding buffer containing 5 µl Annexin V (10 µg/ml) in DMEM with
FBS at 37°C for 10 min in the dark. The cells then underwent
incubation with 10 µl PI (20 µg/ml) for 15 min and samples were
analyzed using an EPICS® XL™ flow cytometer (Beckman
Coulter, Inc., Brea, CA, USA). Data acquisition and analysis were
performed using CellQuest™ software version 5.1 (BD Biosciences,
Franklin Lakes, NJ, USA) (23,24).
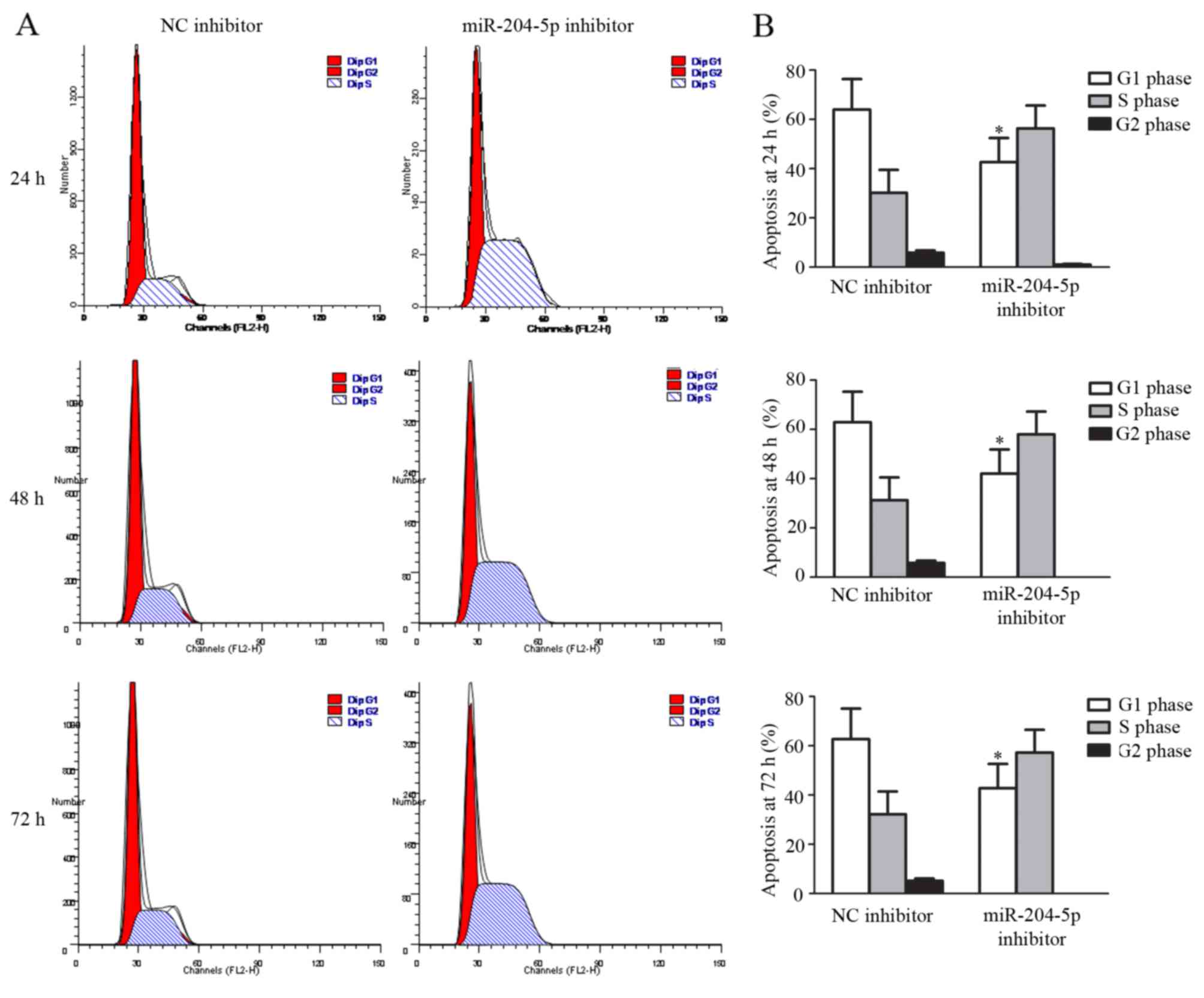
Cell cycle assay
Following transfection of the miRNA inhibitor into
the hypoxic environment and incubation at 37°C for 48 h, JAR cells
were collected by trypsin digestion method and washed with PBS
prior to re-suspension in 250 µl DMEM. Cold (4°C) dehydrated
ethanol (99%) was added to this buffer and incubated overnight at
4°C. Following treatment, cells were collected and incubated with
200 µl PI (20 µg/ml) using a cell cycle assay kit (Vazyme Biotech,
Co., Ltd., Nanjing, China) at 37°C for 15 min. Samples were
immediately analyzed using flow cytometry (EPICS® XL™;
Beckman Coulter, Inc.). Data acquisition and analysis were
performed using CellQuest software version 5.1 (BD Biosciences)
(23,24).
Data analysis
For RT-qPCR data analysis, the relative
quantification method was used to determine the changes in the
expression of the target miRNAs. U6 RNA was used to normalize the
expression and change in amplification. The fold change in
expression was calculated for each sample using 2−ΔΔCq,
where ΔΔCq=(Cq target gene-CqU6) PIH-(Cq target gene-CqU6) control
(25). A value of 2−ΔΔCq
>1.5 or <0.67 was considered to represent differentially
expressed miRNA. The Welch t-test was used to assess the
differential expression of miRNA measured by RT-qPCR.
For other data analysis, Statistical analysis was
performed using SPSS, version 17.0 (SPSS, Inc., Chicago, IL, USA).
One-way analysis of variance was used to compare
log10-transformed relative quantities of target miRNAs
between all groups. Bartlett's test was used to assess the
differences in variance between genes. P<0.05 was considered to
represent a statistically significant difference for all
experiments.
Results
Validation of eight serum miRNAs in
patients with PIH
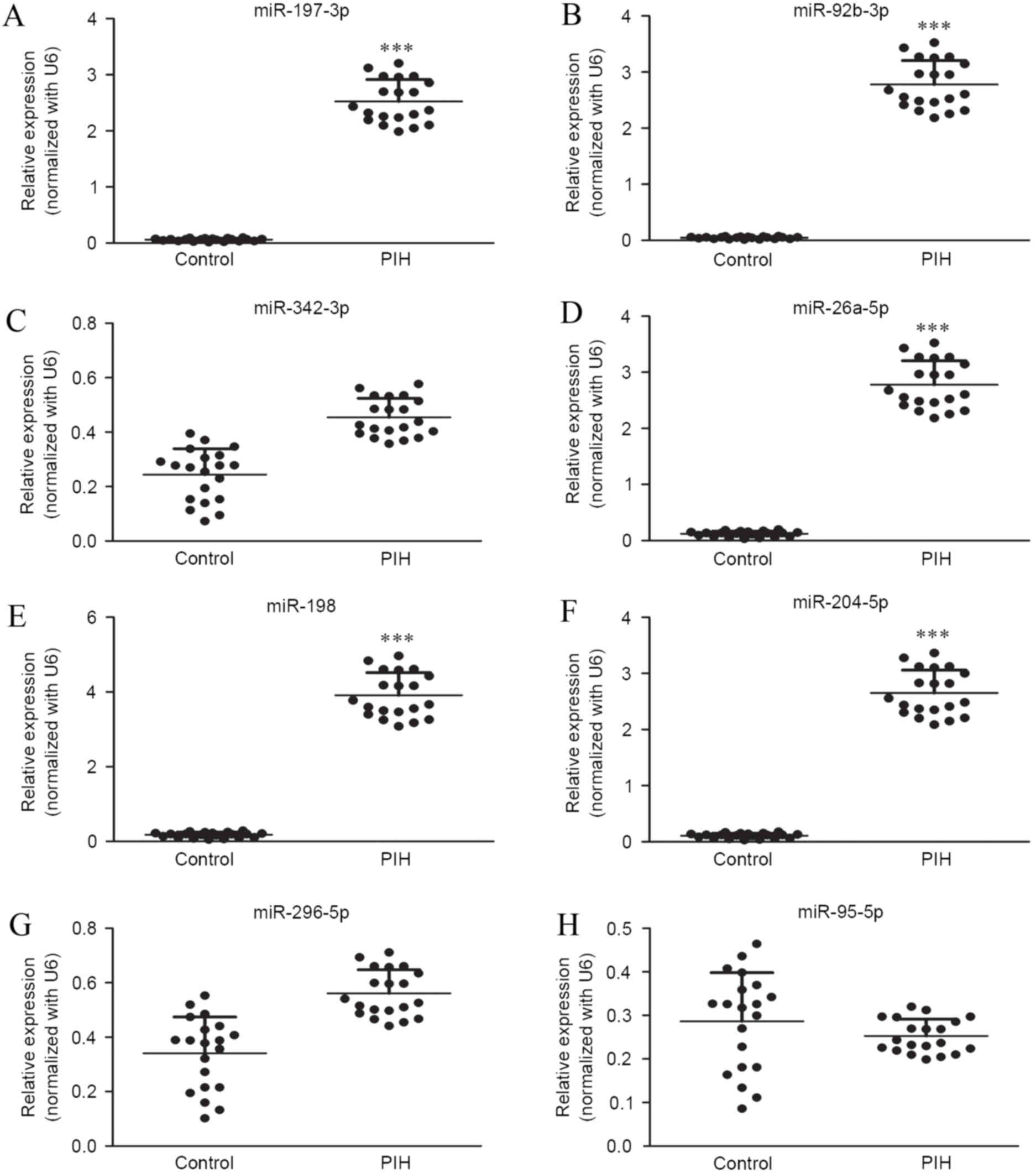
The expression profile of eight serum microRNAs were
selected, based on a previous study, (under review, data not
shown), for further examination in 18 PIH patients that represented
a significant 2-fold change using RT-qPCR. Expression levels of
miR-197-3p, miR-92b-3p, miR-342-3p, miR-26a-5p, miR-198,
miR-204-5p, miR-296-5p and miR-95-5p were measured in the serum
samples of 12 patients with PIH and 6 normal controls (Fig. 1). The results showed significantly
elevated expression of miR-197-3p, miR-92b-3p, miR-26a-5p, miR-198
and miR-204-5p in patients with PIH compared with controls
(P<0.001; Fig. 1A, B and D-F).
However, levels of miR-342-3p, miR-296-5p and miR-95-5p not differ
significantly between PIH patients and controls (Fig. 1C and G-H).
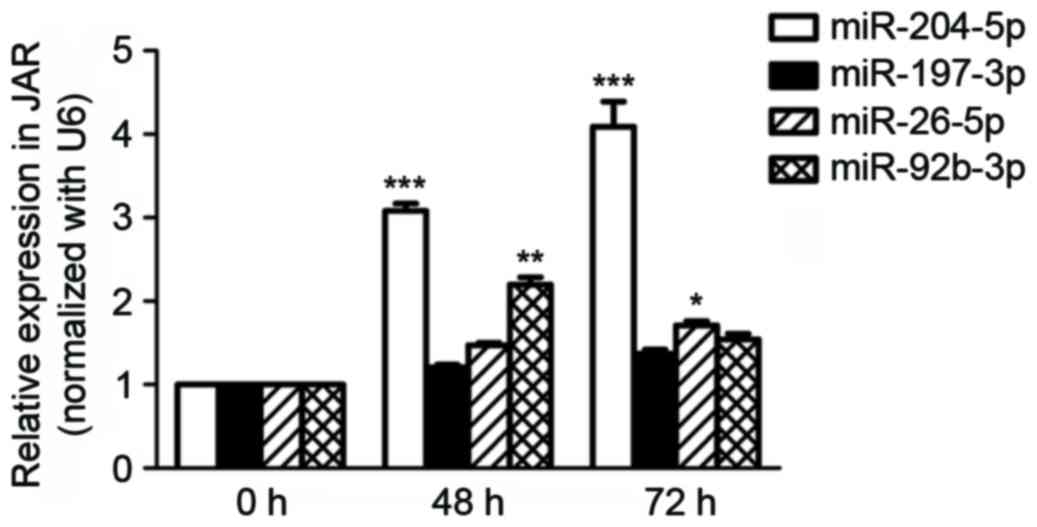
Expression of miRNAs in the hypoxic
environment in vitro
The expression of miR-197-3p, miR-92b-3p,
miR-26a-5p, miR-198 and miR-204-5p were selected to be assessed
in vitro, on the basis of the results of the aforementioned
clinical sample examination. Only miR-204-5p expression increased
significantly in a time-dependent manner in hypoxic JAR cells (0,
48 and 72 h; Fig. 2).
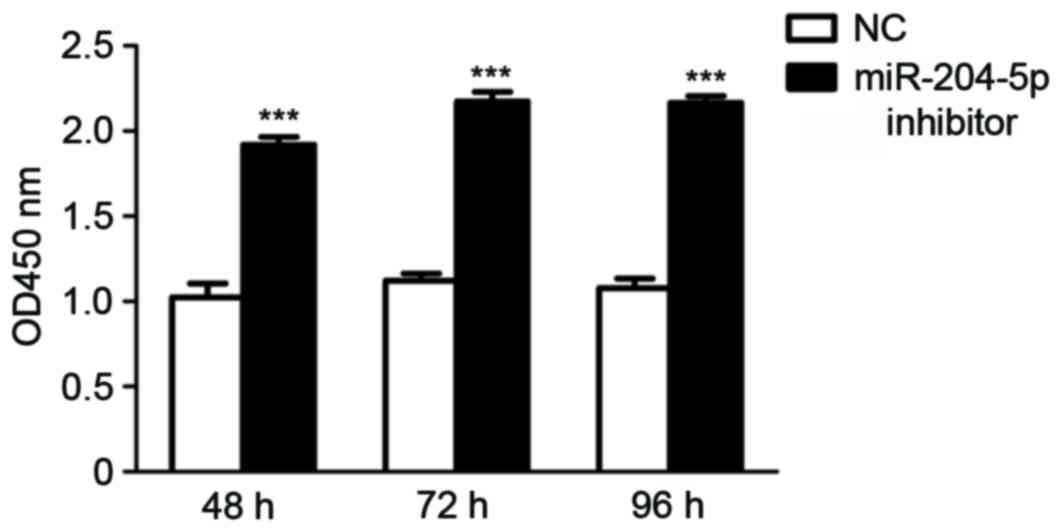
Effect of miR-204-5p inhibitor on cell
proliferation
The effect of miR-204-5p inhibitor on JAR cell
proliferation was subsequently assessed. In hypoxia pre-treatment
JAR cells, cellular proliferation was enhanced significantly in a
time-independent manner in the miR-204-5p inhibitor group, as
indicated by the number of cells detected at each time point
(P<0.001; Fig. 3).
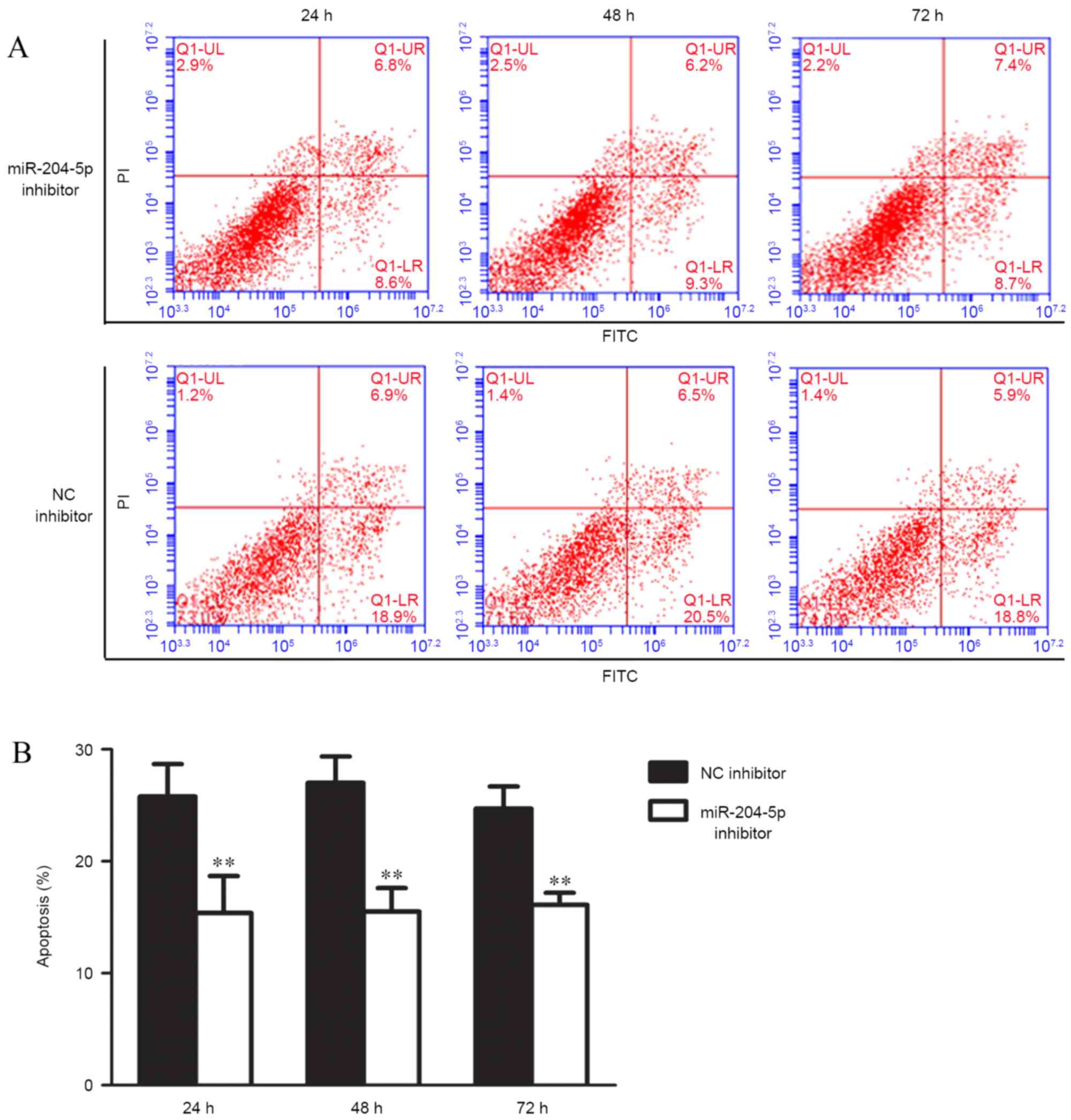
Effects of miR-204-5p inhibitor on
cell apoptosis and cell cycle progression
Apoptosis and cell cycle distribution were analyzed
using flow cytometry following the transfection of miR-204-5p
inhibitor and hypoxia pre-treatment for 48 h. Compared with the
control group, JAR cell exposure to miR-204-5p inhibitor exhibited
typical protection from apoptotic morphology with nuclear
fragmentation, cell shrinkage and cellular rupture into debris.
Apoptosis occurred at a significantly higher rate in cells treated
with the negative control compared with the group treated with
miR-204-5p inhibitor (P<0.01; Fig.
4). Assessment of the cell cycle indicated that the ratio of
cells in the G2/G1 phase increased, although this increase was not
significant. However, G1 cell cycle arrest was significantly
reduced following transfection with the miR-204-5p inhibitor
(P<0.05; Fig. 5).
Discussion
To the best of our knowledge, the molecular
mechanism during PIH pathogenesis, which is responsible for the
occurrence and progression of the syndrome, remains unknown. miRNAs
may target a large number of genes and participate in numerous
cellular events that may be important in maintaining homoeostasis
in a number of organs, including the placenta (26). In the present study, due to the
developing understanding of miRNA expression in PIH, the expression
of eight miRNAs was identified in the serum samples of healthy
controls and patients with PIH using RT-qPCR. The results of the
present study identified that five of the eight miRNAs (miR-197-3p,
miR-92b-3p, miR-26a-5p, miR-198 and miR-204-5p) are more highly
expressed in patients with PIH (Fig.
1). This indicates that a number of miRNAs may impact the
course of PIH. Further detection of these miRNAs using a hypoxia
pre-treatment cell model demonstrated that only miR-204-5p
expression increased in a time-dependent manner in hypoxic JAR
cells (Fig. 2), which suggests that
miR-204-5p reduced JAR cell proliferation as a suppressor in the
hypoxic environment. Effects of the miR-204-5p inhibitor on cell
function were also examined, the results of which suggested that
the miR-204-5p inhibitor may enhance the cellular population of JAR
cells in the hypoxic environment (Fig.
3) and protect JAR cells from apoptosis (Fig. 4) by reducing G1 cell cycle arrest
(Fig. 5). The data collected in the
present study indicates that miR-204-5p may be an important
therapeutic target for the improved prediction, prevention and
treatment of PIH.
The present study produced evidence that expression
of miR-204-5p, which acts as a potent cell survival suppressor
in vitro, is somatically increased in patients with PIH.
This is consistent with the results from a previous study, which
indicated that miR-204 is also upregulated in the serum of
endometrial carcinoma patients (27). Other previous studies have
demonstrated that miR-204-5p expression is decreased in several
types of solid tumors (28–32). It has been previously determined,
using a human miRNA microarray, that miR-204-5p is markedly
downregulated in endometrioid adenocarcinoma tissues (32), inhibiting tumor growth in renal clear
cell carcinoma (33,34), and that it suppresses invasion I
endometrial cancer (35), gastric
cancer (36), and head and neck
tumor (37). This implies that a
change of miR-204-5p may be common in tumorigenesis and reinforces
the complexity of miR-204 regulation. There have been limited
studies focusing on the association between PIH and miR-204-5p, as
a potential marker of this syndrome. The results of the present
study support the possibility that miR-204-5p may be a potential
biomarker for good prognosis of PIH. Thus, therapeutic approaches
targeting elevated levels of miR-204-5p should be investigated as a
novel approach to improve clinical outcomes for patients with
PIH.
miRNA typically targets the 3′ untranslated region
of genes and leads to a significant reduction of full-length
proteins (38). It has previously
been suggested that the ratio of fms-like tyrosine kinase-1
(sFlt-1) and placental growth factor (PIGF) may be an additional
diagnostic or predictive tool for PE (39,40). A
meta-analysis showed increased concentrations of placental sFlt1
and decreased concentrations of PIGF in pregnancies in which the
mother developed PE (41).
Furthermore, the level of vascular endothelial growth factor was
lower in women who developed PE, compared with those that did not
(42). One previous study produced a
series of gene profiles in human peripheral blood mononuclear cells
and investigated their association with PE (43). However, the molecular mechanism of
miR-204-5p of targeting these important genes during PIH or PE
requires further study.
In conclusion, the present study demonstrated that
the expression of miR-204-5p is significantly upregulated in the
clinical serum samples of patients with PIH. Suppression of
miR-204-5p by its specific inhibitor induces JAR cell growth,
decreases cell apoptosis and changes the cell cycle in
vitro. Therefore, miR-204-5p may be considered as a potential
unfavorable progression indicator for patients with PIH and may
serve as a therapeutic target in the future.
Acknowledgements
The present study was supported by funds from the
Social development project of science and Technology Department of
Guangdong (no. 2011B031800).
References
|
1
|
Li S, Xiong X, Harville E, Zhang T, Sun D,
Fernandez C, Krousel-Wood M, Chen W and Whelton PK: Childhood risk
factors and pregnancy-induced hypertension: The bogalusa heart
study. Am J Hypertens. 29:1206–1211. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kintiraki E, Papakatsika S, Kotronis G,
Goulis DG and Kotsis V: Pregnancy-induced hypertension. Hormones
(Athens). 14:211–223. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Magee LA, Pels A, Helewa M, Rey E and von
Dadelszen P: Canadian Hypertensive Disorders of Pregnancy Working
Group: Diagnosis, evaluation, and management of the hypertensive
disorders of pregnancy: Executive summary. J Obstet Gynaecol Can.
36:416–441. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Caetano M, Ornstein MP, von Dadelszen P,
Hannah ME, Logan AG, Gruslin A, Willan A and Magee LA: A survey of
Canadian practitioners regarding diagnosis and evaluation of the
hypertensive disorders of pregnancy. Hypertens Pregnancy.
23:197–209. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Magee LA, Helewa M, Moutquin JM and von
Dadelszen P: Hypertension Guideline Committee; Strategic Training
Initiative in Research in the Reproductive Health Sciences
(STIRRHS) Scholars: Diagnosis, evaluation, and management of the
hypertensive disorders of pregnancy. J Obstet Gynaecol Can.
30:(Suppl 3). S1–S48. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tranquilli AL: Hypertension during
pregnancy is associated with increased risk of later cardiovascular
disease, kidney disease and diabetes. Evid Based Nurs. 17:36–37.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kitson R, Williams V and Howell C:
Caesarean section in a parturient with type III spinal muscular
atrophy and pre-eclampsia. Anaesthesia. 59:94–95. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Heimrath J, Czekanski A, Krawczenko A and
Dus D: The role of endothelium in the pathogenesis of
pregnancy-induced hypertension. Postepy Hig Med Dosw (Online).
61:48–57. 2007.PubMed/NCBI
|
|
9
|
Padmanabhan S, Caulfield M and Dominiczak
AF: Genetic and molecular aspects of hypertension. Circ Res.
116:937–959. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen Z, Xu F, Wei Y, Liu F and Qi H:
Angiotensin converting enzyme insertion/deletion polymorphism and
risk of pregnancy hypertensive disorders: A meta-analysis. J Renin
Angiotensin Aldosterone Syst. 13:184–195. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lycoudi A, Mavreli D, Mavrou A,
Papantoniou N and Kolialexi A: miRNAs in pregnancy-related
complications. Expert Rev Mol Diagn. 15:999–1010. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ura B, Feriotto G, Monasta L, Bilel S,
Zweyer M and Celeghini C: Potential role of circulating microRNAs
as early markers of preeclampsia. Taiwan J Obstet Gynecol.
53:232–234. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zou Q, Li J, Hong Q, Lin Z, Wu Y, Shi H
and Ju Y: Prediction of MicroRNA-disease associations based on
social network analysis methods. Biomed Res Int. 2015:8105142015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Van Wynsberghe PM, Chan SP, Slack FJ and
Pasquinelli AE: Analysis of microRNA expression and function.
Methods Cell Biol. 106:219–252. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Choi SY, Yun J, Lee OJ, Han HS, Yeo MK,
Lee MA and Suh KS: MicroRNA expression profiles in placenta with
severe preeclampsia using a PNA-based microarray. Placenta.
34:799–804. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wu L, Zhou H, Lin H, Qi J, Zhu C, Gao Z
and Wang H: Circulating microRNAs are elevated in plasma from
severe preeclamptic pregnancies. Reproduction. 143:389–397. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yu Y, Wang L, Liu T and Guan H:
MicroRNA-204 suppresses trophoblast-like cell invasion by targeting
matrix metalloproteinase-9. Biochem Biophys Res Commun.
463:285–291. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lauschke VM, Mkrtchian S and
Ingelman-Sundberg M: The role of microRNAs in liver injury at the
crossroad between hepatic cell death and regeneration. Biochem
Biophys Res Commun. Oct 24–2016.(Epub ahead of print). doi:
10.1016/j.bbrc.2016.10.084. PubMed/NCBI
|
|
19
|
Abe E, Matsubara K, Ochi H, Ito M, Oka K
and Kameda K: Elevated levels of adhesion molecules derived from
leukocytes and endothelial cells in patients with pregnancy-induced
hypertension. Hypertens Pregnancy. 22:31–43. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kamiya T, Kwon AH, Kanemaki T, Matsui Y,
Uetsuji S, Okumura T and Kamiyama Y: A simplified model of hypoxic
injury in primary cultured rat hepatocytes. In Vitro Cell Dev Biol
Anim. 34:131–137. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cikos S, Bukovská A and Koppel J: Relative
quantification of mRNA: Comparison of methods currently used for
real-time PCR data analysis. BMC Mol Biol. 8:1132007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kobata A and Takeuchi M: Structure,
pathology and function of the N-linked sugar chains of human
chorionic gonadotropin. Biochim Biophys Acta. 1455:315–326. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Abu-Absi NR, Zamamiri A, Kacmar J, Balogh
SJ and Srienc F: Automated flow cytometry for acquisition of
time-dependent population data. Cytometry A. 51:87–96. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Holmes KL, Otten G and Yokoyama WM: Flow
cytometry analysis using the Becton Dickinson FACS Calibur. Curr
Protoc Immunol Chapter. 5:Unit 5.4. 2002. View Article : Google Scholar
|
|
25
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mouillet JF, Mishima T, Paffaro AM, Parks
TW, Ziegler JA, Chu T and Sadovsky Y: The expression and
post-transcriptional regulation of FSTL1 transcripts in placental
trophoblasts. Placenta. 36:1231–1238. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jia W, Wu Y, Zhang Q, Gao G, Zhang C and
Xiang Y: Identification of four serum microRNAs from a genome-wide
serum microRNA expression profile as potential non-invasive
biomarkers for endometrioid endometrial cancer. Oncol Lett.
6:261–267. 2013.PubMed/NCBI
|
|
28
|
Tarasov VA, Matishov DG, Shin EF, Boiko
NV, Timoshkina NN, Makhotkin MA, Lomonosov AM, Kirpii AA, Kit OI
and Maksimov AY: Coordinated aberranit expression of miRNAs in
colon cancer. Genetika. 50:1232–1244. 2014.(In Russian). PubMed/NCBI
|
|
29
|
Liu L, Wang J, Li X, Ma J, Shi C, Zhu H,
Xi Q, Zhang J, Zhao X and Gu M: MiR-204-5p suppresses cell
proliferation by inhibiting IGFBP5 in papillary thyroid carcinoma.
Biochem Biophys Res Commun. 457:621–626. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhang B, Yin Y, Hu Y, Zhang J, Bian Z,
Song M, Hua D and Huang Z: MicroRNA-204-5p inhibits gastric cancer
cell proliferation by downregulating USP47 and RAB22A. Med Oncol.
32:3312015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sümbül AT, Göğebakan B, Ergün S, Yengil E,
Batmacı CY, Tonyalı Ö and Yaldız M: miR-204-5p expression in
colorectal cancer: An autophagy-associated gene. Tumour Biol.
35:12713–12719. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bao W, Wang HH, Tian FJ, He XY, Qiu MT,
Wang JY, Zhang HJ, Wang LH and Wan XP: A TrkB-STAT3-miR-204-5p
regulatory circuitry controls proliferation and invasion of
endometrial carcinoma cells. Mol Cancer. 12:1552013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mikhaylova O, Stratton Y, Hall D, Kellner
E, Ehmer B, Drew AF, Gallo CA, Plas DR, Biesiada J, Meller J and
Czyzyk-Krzeska MF: VHL-regulated MiR-204 suppresses tumor growth
through inhibition of LC3B-mediated autophagy in renal clear cell
carcinoma. Cancer Cell. 21:532–546. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Atala A: Re: VHL-Regulated miR-204
suppresses tumor growth through inhibition of LC3B-mediated
autophagy in renal clear cell carcinoma. J Urol. 188:24342012.
View Article : Google Scholar
|
|
35
|
Chung TK, Lau TS, Cheung TH, Yim SF, Lo
KW, Siu NS, Chan LK, Yu MY, Kwong J, Doran G, et al: Dysregulation
of microRNA-204 mediates migration and invasion of endometrial
cancer by regulating FOXC1. Int J Cancer. 130:1036–1045. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Qiu YH, Wei YP, Shen NJ, Wang ZC, Kan T,
Yu WL, Yi B and Zhang YJ: miR-204 inhibits epithelial to
mesenchymal transition by targeting slug in intrahepatic
cholangiocarcinoma cells. Cell Physiol Biochem. 32:1331–1341. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lee Y, Yang X, Huang Y, Fan H, Zhang Q, Wu
Y, Li J, Hasina R, Cheng C, Lingen MW, et al: Network modeling
identifies molecular functions targeted by miR-204 to suppress head
and neck tumor metastasis. PLoS Comput Biol. 6:e10007302010.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Pule GD, Mowla S, Novitzky N and Wonkam A:
Hydroxyurea down-regulates BCL11A, KLF-1 and MYB through
miRNA-mediated actions to induce γ-globin expression: Implications
for new therapeutic approaches of sickle cell disease. Clin Transl
Med. 5:152016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Nevo O, Lee DK and Caniggia I: Attenuation
of VEGFR-2 expression by sFlt-1 and low oxygen in human placenta.
PLoS One. 8:e811762013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kleinrouweler CE, Wiegerinck MM,
Ris-Stalpers C, Bossuyt PM, van der Post JA, von Dadelszen P, Mol
BW and Pajkrt E: EBM CONNECT Collaboration: Accuracy of circulating
placental growth factor, vascular endothelial growth factor,
soluble fms-like tyrosine kinase 1 and soluble endoglin in the
prediction of pre-eclampsia: A systematic review and meta-analysis.
BJOG. 119:778–787. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Liu Y, Zhao Y, Yu A, Zhao B, Gao Y and Niu
H: Diagnostic accuracy of the soluble Fms-like tyrosine
kinase-1/placental growth factor ratio for preeclampsia: A
meta-analysis based on 20 studies. Arch Gynecol Obstet.
292:507–518. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Dubova EA, Pavlov KA, Lyapin VM,
Shchyogolev AI and Sukhikh GT: Vascular endothelial growth factor
and its receptors in the placental villi of pregnant patients with
pre-eclampsia. Bull Exp Biol Med. 154:792–795. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Martinez-Fierro ML, Garza-Veloz I,
Carrillo-Sanchez K, Martinez-Gaytan V, Cortes-Flores R,
Ochoa-Torres MA, Guerrero GG, Rodriguez-Sanchez IP,
Cancela-Murrieta CO, Zamudio-Osuna M, et al: Expression levels of
seven candidate genes in human peripheral blood mononuclear cells
and their association with preeclampsia. Hypertens Pregnancy.
33:191–203. 2014. View Article : Google Scholar : PubMed/NCBI
|