Introduction
Endobronchial ultrasound (EBUS) has been used in
clinical practice since the 1990s (1). EBUS may be used in combination with
needle aspiration to obtain biopsy samples of lesions outside the
airway, an application that may be termed ‘EBUS-guided
transbronchial needle aspiration (EBUS-TBNA)’ (2). This widely used technique is
recommended as an important tool for staging mediastinal lymph
nodes containing malignant cells (3,4) and is
predominantly used for scanning and needle aspiration biopsies of
mediastinal lymph nodes outside the trachea and main bronchi
(5–7). Occasionally, this approach has been
used for exploratory studies of the lesions outside the lobar
bronchi and segmental bronchi (8),
mediastinum (9,10), thoracic great vessels (11–13),
pericardium (14), heart (15), esophagus (16), thyroid (17), and other tissues and organs (18). As the thyroid gland is located near
and anterolateral to the upper trachea, the EBUS-TBNA technique may
be useful in scanning thyroid lesions and obtaining needle
aspiration samples for biopsy. Various case reports (17,19) and
a small-sample retrospective study (20) have been published on the application
of the EBUS-TBNA technique; however, few reports are available
concerning the use of this technique to diagnose thyroid cysts
(21). To date, no report has been
published on the application of the EBUS-TBNA technique to treat
thyroid cysts. Thus, the present case report investigated a case of
a thyroid cyst that was diagnosed and treated via the EBUS-TBNA
technique.
Case report
The present study was approved by the Institutional
Review Board of Shengjing Hospital of China Medical University (no.
2015PS61J; Shenyang, China) A 67-year-old male was admitted to our
hospital due to spontaneous back pain with no existing medical
conditions and presented without respiratory symptoms, such as
cough or shortness of breath. Physical examination revealed no
positive findings. Serum carcinoembryonic antigen level was <5
µg/l (reference range: 0–5 µg/l) using a Cobas E602 immunoassay
module (Roche Diagnostics, Basel, Switzerland). A positron emission
tomography-computed tomography (PET/CT) scan (Siemens AG, Munich,
Germany) was performed to exclude neoplastic diseases and revealed
a soft tissue mass in the hilum of the left lung, a soft tissue
nodule in the lower lobe of the left lung, enlarged lymph nodes
superior to the left clavicle and inferior to the carina within the
mediastinum, left-sided pleural effusion, bilateral pleural
thickening and low-density signals in the right lobe of the thyroid
(Fig. 1). To obtain a definite
diagnosis, an ultrasound bronchoscope (HI-VISION Avius; Hitachi,
Ltd., Tokyo, Japan) and an EB-1970UK video bronchoscope (Pentax,
Tokyo, Japan) was used, following an EBUS-TBNA examination on March
18th 2015 after receiving informed consent from the
patient. Ultrasound examination of the right lobe of the thyroid
indicated an 11.3×14.0-mm oval lesion with clear boundaries, and a
medium-to-low signal of an incomplete membrane containing a
medium-to-low signal center without blood flow (Fig. 2). Three needle aspiration biopsies,
using endobronchial ultrasound needles (ECHO-HD-22-EBUS-P; EchoTip
Ultra; Cook Medical, Inc., Bloomington, IN, USA), were performed at
this site (Fig. 3), and 1.5 ml of a
cloudy, yellow viscous fluid was obtained. The aspiration needles
were changed and needle aspiration biopsies for lesions in the
subcarinal area and the hilum of the left lung were performed. A
small amount of bleeding occurred at the aspiration site; however,
no major complications were reported following aspiration.
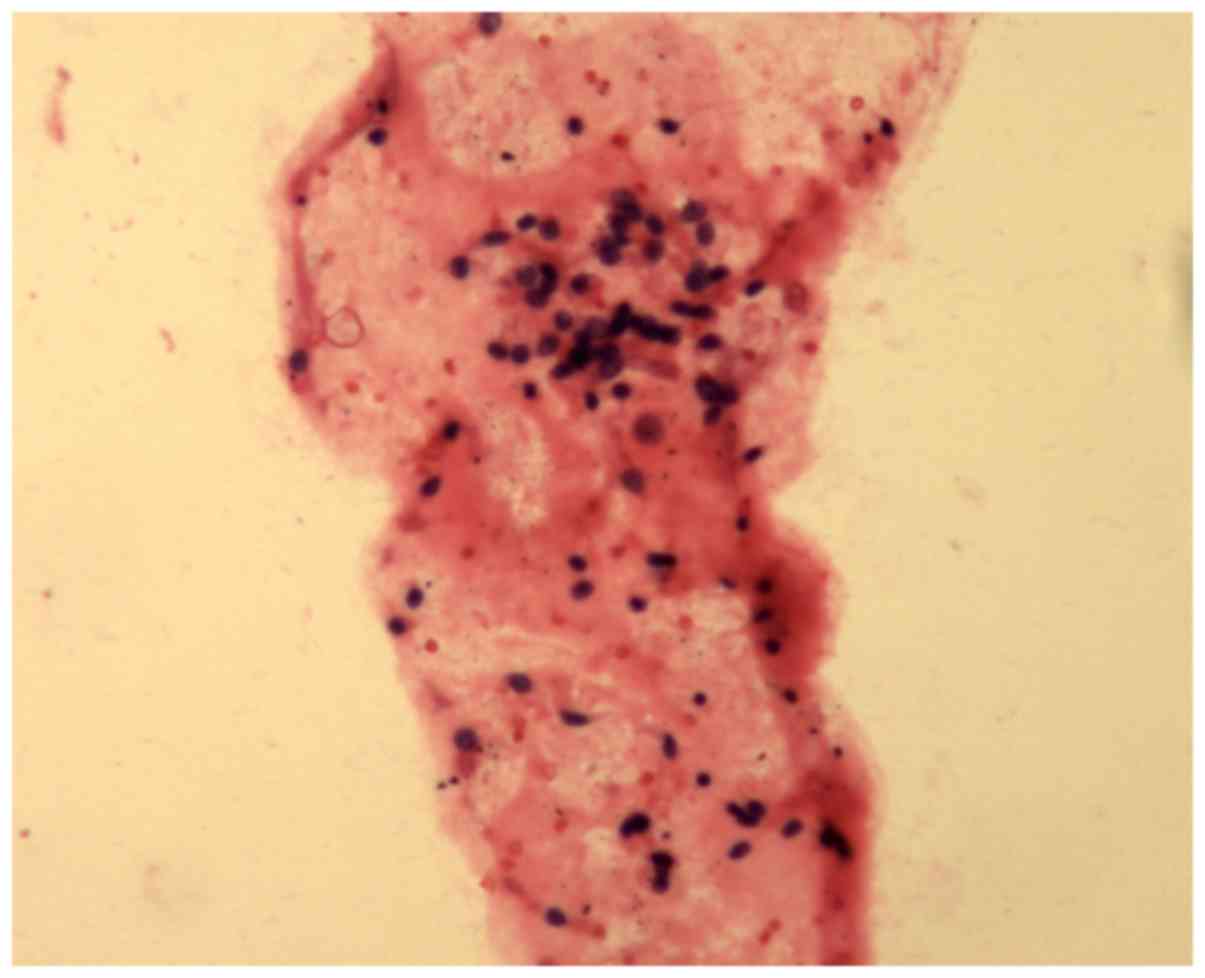
Aspirates were collected and fixed in formalin at 20°C for 18 h and
subsequently embedded in paraffin. Sections were cut (thickness, 5
µm) and stained with hematoxylin and eosin. Cytopathological
examinations were performed under a light microscope, and the
results indicated a low number of inflammatory cells and thyroid
epithelial cells; however, tumor cells associated with thyroid or
other organs were absent (Fig. 4).
The findings from the pathology examination of the subcarinal lymph
nodes and from the lesion itself were negative for malignancy.
Subsequently a percutaneous needle aspiration biopsy of the nodule
in the lower lobe of the left lung was performed. Pathological
examination of the percutaneous needle aspirates indicated lung
adenocarcinoma (bronchial mucosa) based on the following
immunohistochemistry results: Tumor proteins p63(+) and p40(−),
NapsonA(+), thyroid transcription factor-1(+), synechocystis(−),
cytokeratin(+). Reverse transcription-quantitative polymerase chain
reaction was performed as previously described (22) and the results of epidermal growth
factor receptor mutation testing were negative. Combined with the
result of the PET/CT, the final diagnoses were lung adenocarcinoma
with bone metastasis (stage IV) and thyroid cyst (21). The patient received systemic
chemotherapy on 4 occasions between March and August 2015.
Intravenous chemotherapy drugs included cisplatin (cycles 1 and 2;
140 mg per cycle; Qilu Pharmaceutical Co., Ltd., Shandong, China),
carboplatin (cycle 2; 500 mg; Qilu Pharmaceutical Co., Ltd.), and
zoledronic acid (cycle 3; Zometa; 8 mg; Novartis, Basel,
Switzerland). Local radiotherapy for bone metastasis was used in
conjunction with oral erlotinib tablets (Tarceva; 150 mg/day; Roche
Diagnostics) for cycle 4 of the chemotherapy. A follow-up chest CT
scan at 7 weeks post-aspiration showed that the low-density signal
in the right lobe of the thyroid had disappeared (Fig. 5).
Discussion
Thyroid cysts are relatively common benign lesions,
which are predominantly solitary elastic lesions that exhibit a
smooth surface and clear boundaries (21,23).
Typically, no tenderness is experienced and no adhesion between the
cyst and peripheral tissues is apparent (24,25).
Radioisotope scanning indicates the cyst as a ‘cold’ nodule,
whereas an ultrasound examination reveals its cystic nature
(26). Echo signals are mixed, with
the anechoic area containing low- or medium-strength echo signals
of deposits on the lower portion of the cyst, or attached to the
cyst wall. Occasionally septa may be present inside the cyst
(23,25). Thyroid cysts may be diagnosed
according to the characteristics mentioned above, as demonstrated
in the present case. In particular, the present study revealed that
EBUS indicated medium-strength echo signals of deposits on the
lower portion of the cyst and the cyst fluid obtained by needle
aspiration, which is the most direct diagnostic tool, indicated the
presence of a thyroid cyst. Consequently, the EBUS examination in
the present study provided the information required to diagnose a
thyroid cyst in the patient.
While most patients with thyroid cysts experience no
clinical symptoms, the cyst grows continuously, creating a risk of
intracystic bleeding. Therefore, thyroid cysts should be treated
soon after a definitive diagnosis has been made. Local aspiration
and anhydrous ethanol irrigation are appropriate techniques used
for treating superficial small cysts (<30 mm in diameter)
(27). The procedures are minimally
invasive and result in less pain for the patient and provide a
satisfactory outcome; however, secondary bleeding is a recognized
risk with this method. In order to treat deep thyroid cysts (>30
mm in diameter), surgical removal is a safe and reliable preferred
option (27). In the present case
study, the maximum diameter of the cyst was 14 mm and the cyst was
located deep but close to the trachea. The EBUS technique was used
to demonstrate its use as an alternative method for diagnosis and
treatment, which avoids possible trauma inflicted by surgery and
therefore offers an alternative for patients who cannot undergo
surgery.
In the present case, the EBUS technique was used to
diagnose the patient and treat the thyroid cyst, simultaneously.
The patient tolerated the whole process well. Combined with the
findings of case reports (19,20) and
a small-sample retrospective study (17), we believe that needle aspiration
biopsy and treatment using the EBUS technique are feasible
procedures for deep lesions near the trachea. Additionally, EBUS
guided needle aspiration to thyroid is useful to further determine
that the condition of the patient is not the result of primary
thyroid tumors or lung cancer metastasis to the thyroid (28).
In previous case reports, two patients presented
with serious complications after EBUS-TBNA of the thyroid (29,30). One
patient had a skin rash on the suprasternal notch 48 h after the
biopsy procedure. Even after flucloxacillin administration,
spontaneous drainage of pus occurred at the site of the rash;
however, the rash disappeared after 6 days of treatment (29). Culture of the pus identified the
pathogen as penicillin-sensitive Streptococcus pneumonia.
Another patient presented with a fever, swelling of the neck, and
pain arising 8 days after biopsy. The ultrasound examination
indicated an abscess in the thyroid. Ultrasound-guided percutaneous
aspiration was performed twice to remove the pus, and an antibiotic
was administered intravenously. Pus culture revealed
penicillin-sensitive Streptococcus mitis and mixed
gram-positive and gram-negative bacteria. However, the patient did
make a full recovery (30). These
cases suggest that the EBUS-TBNA technique is not aseptic and
resulted in infection, which may occur easily during aspiration and
manipulation of the thyroid lesions (31).
Casal et al (17) investigated the causes of infection
following EBUS-TBNA and identified that 11 of 12 patients examined
after the laryngeal mask airway who received EBUS-TBNA under
general anesthesia had no complications, suggesting that
manipulation under general anesthesia may reduce the risk of
infection, rather than in a less-sedated state. Moreover, previous
studies have demonstrated that the two patients described above
were infected with penicillin-sensitive Streptococcus after
EBUS-TBNA procedures of the thyroid (29,30).
Hence, perioperative antibiotic administration is necessary for
reducing the incidence of infection. In order to reduce the
incidence of infection three key steps should be considered: Using
general anesthesia, administering antibiotics perioperative and
decreasing the frequency of aspiration.
The present case study reported for the first time a
case of thyroid cyst treated with the EBUS-TBNA technique. We
believe that aspiration of the thyroid cyst using the EBUS-TBNA
technique is feasible. However, strict criteria for this procedure
are required to reduce the risk of possible complications. The
effectiveness and safety of the EBUS-TBNA technique in the
manipulation of thyroid cysts should be verified by future
large-sample clinical studies. Until randomized, controlled studies
yield positive results, the range of application of the EBUS-TBNA
technique will not be expanded (30). To conclude, EBUS-TBNA provides an
alternative for the diagnosis and treatment of deep thyroid cysts
located close to the airway. In all other cases, percutaneous
needle aspiration or surgery should be the first choice.
References
|
1
|
Hürter T and Hanrath P: Endobronchial
sonography: Feasibility and preliminary results. Thorax.
47:565–567. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wahidi MM, Herth F, Yasufuku K, Shepherd
RW, Yarmus L, Chawla M, Lamb C, Casey KR, Patel S, Silvestri GA and
Feller-Kopman DJ: Technical aspects of endobronchial
ultrasound-guided transbronchial needle aspiration: CHEST guideline
and expert panel report. Chest. 149:816–835. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
De Leyn P, Dooms C, Kuzdzal J, Lardinois
D, Passlick B, Rami-Porta R, Turna A, Van Schil P, Venuta F, Waller
D, et al: Preoperative mediastinal lymph node staging for non-small
cell lung cancer: 2014 update of the 2007 ESTS guidelines. Transl
Lung Cancer Res. 3:225–233. 2014.PubMed/NCBI
|
|
4
|
Colella S, Vilmann P, Konge L and
Clementsen PF: Endoscopic ultrasound in the diagnosis and staging
of lung cancer. Endosc Ultrasound. 3:205–212. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Geake J, Hammerschlag G, Nguyen P,
Wallbridge P, Jenkin GA, Korman TM, Jennings B, Johnson DF, Irving
LB, Farmer M and Steinfort DP: Utility of EBUS-TBNA for diagnosis
of mediastinal tuberculous lymphadenitis: A multicentre Australian
experience. J Thorac Dis. 7:439–448. 2015.PubMed/NCBI
|
|
6
|
Harris K, Maroun R, Attwood K and Chalhoub
M: Comparison of cytologic accuracy of endobronchial ultrasound
transbronchial needle aspiration using needle suction versus no
suction. Endosc Ultrasound. 4:115–119. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ozgul MA, Cetinkaya E, Kirkil G, Ozgul G,
Abul Y, Acat M, Onaran H, Urer HN, Tutar N and Dincer HE: Lymph
node characteristics of sarcoidosis with endobronchial ultrasound.
Endosc Ultrasound. 3:232–237. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kurimoto N, Inoue T, Miyazawa T, Morita K,
Matsuoka S and Nakamura H: The usefulness of endobronchial
ultrasonography-guided transbronchial needle aspiration at the
lobar, segmental, or subsegmental bronchus smaller than a
convex-type bronchoscope. J Bronchology Interv Pulmonol. 21:6–13.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eckardt J: Endobronchial ultrasound-guided
transbronchial needle aspiration of lesions in mediastinum. J
Thorac Dis. 2:125–128. 2010.PubMed/NCBI
|
|
10
|
Badaoui A, Dahlqvist C, Rahier J, Weynand
B, Ocak S, Deprez P, Eucher P and Duplaquet F: Combined endoscopic
ultrasonography and endobronchial ultrasound-fine-needle aspiration
for evaluation of mediastinal lymph nodes. Endosc Ultrasound.
3:(Suppl 1). S92014.PubMed/NCBI
|
|
11
|
Aumiller J, Herth FJ, Krasnik M and
Eberhardt R: Endobronchial ultrasound for detecting central
pulmonary emboli: A pilot study. Respiration. 77:298–302. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Harris K, Modi K, Kumar A and Dhillon SS:
Endobronchial ultrasound-guided transbronchial needle aspiration of
pulmonary artery tumors: A systematic review (with video). Endosc
Ultrasound. 4:191–197. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Modi K, Dhillon S, Kumar A, Ylagan L and
Harris K: Leiomyosarcoma of the pulmonary artery diagnosed by
endobronchial ultrasound-guided transbronchial needle aspiration.
Endosc Ultrasound. 3:249–251. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zarogoulidis P and He MC: Dr. Paul
Zarogoulidis: The exploration on pneumothorax and new use of EBUS.
J Thorac Dis. 7:E1062015.PubMed/NCBI
|
|
15
|
Cetinkaya E, Yılmaz A, Özgül A, Gençoğlu A
and Günlüoğlu G: Left atrial mass demonstrated during endobronchial
ultrasound session. Respiration. 81:57–58. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wakamatsu T, Tsushima K, Yasuo M, Yamazaki
Y, Yoshikawa S, Koide N, Fujimori M and Koizumi T: Usefulness of
preoperative endobronchial ultrasound for airway invasion around
the trachea: Esophageal cancer and thyroid cancer. Respiration.
73:651–657. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Casal RF, Phan MN, Keshava K, Garcia JM,
Grosu H, Lazarus DR, Iribarren J and Rosen DG: The use of
endobronchial ultrasound-guided transbronchial needle aspiration in
the diagnosis of thyroid lesions. BMC Endocr Disord. 14:882014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dincer HE, Gliksberg EP and Andrade RS:
Endoscopic ultrasound and/or endobronchial ultrasound-guided needle
biopsy of central intraparenchymal lung lesions not adjacent to
airways or esophagus. Endosc Ultrasound. 4:40–43. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kumar A, Mohan A, Dhillon SS and Harris K:
Substernal thyroid biopsy using Endobronchial Ultrasound-guided
Transbronchial Needle Aspiration. J Vis Exp. e518672014.PubMed/NCBI
|
|
20
|
Madan K, Mittal S, Hadda V, Jain D, Mohan
A and Guleria R: Endobronchial ultrasound-guided transbronchial
needle aspiration of thyroid: Report of two cases and systematic
review of literature. Lung India. 33:682–687. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sánchez-Font A, Peralta S and Curull V:
Thyroid cyst diagnosed by endobronchial ultrasound-guided
transbronchial needle aspiration in a patient with lung cancer.
Arch Bronconeumol. 49:38–39. 2013.(In English, Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Han CB, Ma JT, Li F, Zhao JZ, Jing W, Zhou
Y and Zou HW: EGFR and KRAS mutations and altered c-Met gene copy
numbers in primary non-small cell lung cancer and associated stage
N2 lymph node-metastasis. Cancer Lett. 314:63–72. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hegedüs L: Clinical practice. The thyroid
nodule. N Engl J Med. 351:1764–1771. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
American Thyroid Association (ATA)
Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid
Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel
SJ, Mazzaferri EL, McIver B, Pacini F, et al: Revised American
Thyroid Association management guidelines for patients with thyroid
nodules and differentiated thyroid cancer. Thyroid. 19:1167–1214.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Burch HB: Evaluation and management of the
solid thyroid nodule. Endocrinol Metab Clin North Am. 24:663–710.
1995.PubMed/NCBI
|
|
26
|
Weber AL, Randolph G and Aksoy FG: The
thyroid and parathyroid glands. CT and MR imaging and correlation
with pathology and clinical findings. Radiol Clin North Am.
38:1105–1129. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gharib H, Papini E, Garber JR, Duick DS,
Harrell RM, Hegedüs L, Paschke R and Valcavi R: Vitti P;
AACE/ACE/AME Task Force on Thyroid Nodules: American association of
clinical endocrinologists, American college of endocrinology, and
associazione medici endocrinologi medical guidelines for clinical
practice for the diagnosis and management of thyroid nodules-2016
update. Endocr Pract. 22:622–639. 2016.PubMed/NCBI
|
|
28
|
Katsenos S, Archondakis S, Vaias M and
Skoulikaris N: Thyroid gland metastasis from small cell lung
cancer: An unusual site of metastatic spread. J Thorac Dis.
5:E21–E24. 2013.PubMed/NCBI
|
|
29
|
Steinfort DP, Johnson DF and Irving LB:
Infective complications from endobronchial
ultrasound-transbronchial needle aspiration. Eur Respir J.
34:524–525. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kennedy MP, Breen M, O'Regan K, McCarthy
J, Horgan M and Henry MT: Endobronchial ultrasound-guided
transbronchial needle aspiration of thyroid nodules: Pushing the
boundary too far? Chest. 142:1690–1691. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Haas AR: Infectious complications from
full extension endobronchial ultrasound transbronchial needle
aspiration. Eur Respir J. 33:935–938. 2009. View Article : Google Scholar : PubMed/NCBI
|