Introduction
Systemic lupus erythematosus (SLE) is a chronic
complex multisystem autoimmune disease that is characterized by the
production of diverse autoantibodies (1,2). The
loss of immune tolerance to self-antigens results in the activation
of the immune system to produce autoantibodies, which leads to
clinical manifestations including lupus nephritis (LN),
nondestructive arthritis, cutaneous rash, vasculitis, central
nervous system and cardiopulmonary symptoms (3). The selection of an intensive treatment
strategy for clinical remission of SLE is based on the assessment
of the disease activity; therefore, measurement of disease activity
has become an essential step in monitoring disease progression and
assessing therapeutic effects (4).
Calreticulin (CRT) is a 46 kDa Ca2+
binding chaperone that has multiple functions both inside and
outside of the endoplasmic reticulum, including Ca2+
homeostasis and glycoprotein folding (5). Previous studies have revealed that CRT
is implicated in a number of autoimmune processes, such as
molecular mimicry, epitope spreading, complement inactivation, and
stimulation of inflammatory mediators (6–9). These
findings suggest that CRT not only acts as an autoantigen, but also
serves an active role in the pathological processes of various
autoimmune diseases (5,10). Previous findings, showed an elevation
of CRT concentration in the serum of patients with SLE and its
relation to this autoimmune disorder (11–13).
However, to the best of our knowledge, the association of CRT with
disease activity and organ damage has not been reported.
The present study evaluates the levels of serum CRT
in patients with SLE and its correlation to SLE disease activity
and organ damage. Currently, the systemic lupus erythematosus
disease activity index 2000 (SLEDAI-2K) score is widely utilised to
assess disease activity in SLE patients (14,15). The
current study investigated the association of serum CRT with
SLEDAI-2K scores, and other conventional markers of SLE disease
activity, including complement 3 (C3), complement 4 (C4) and
anti-double-stranded DNA (anti-dsDNA). Besides those markers, the
correlation between serum CRT levels and anti-Ro52 was also
analyzed in the patients with SLE, based on a previous study by
Kvarnstrom et al (16)
reporting that anti-Ro52 is significantly associated with disease
activity in patients with SLE. In addition, correlation between the
level of CRT and organ damage (defined as chronic, nonreversible
change, not associated with active inflammation, occurring since
the onset of lupus and present for at least 6 months) were also
investigated in the present study. Organ damage was evaluated in
this investigation using Systemic Lupus International Collaborating
Clinics/American College of Rheumatology Damage Index (SDI), which
is a widely accepted tool to measure organ damage and regarded as
the gold standard for this kind of assessment (17).
Materials and methods
Patients and samples
Serum samples of patients were obtained from 80
patients with SLE, 55 patients with other autoimmune disease (16
Sjögren's syndrome, 19 ankylosing spondylitis, 20 systemic
scleroderma) and 60 age and gender-matched healthy control subjects
(HC) (Table I). All patients with
SLE fulfilled the American College of Rheumatology 1997 criteria
for SLE (18). Patients with other
diseases fulfilled their corresponding diagnostic criteria
(19–21). The control group comprised healthy
volunteers with no history of autoimmune disease or
immunosuppressive therapy. Tianjin Medical University (Tianjin,
China) provided ethical approval for all experiments. Informed
consent was obtained from all patients and the control
subjects.
 | Table I.Baseline characteristics of the study
populations. |
Table I.
Baseline characteristics of the study
populations.
| Characteristic | SLE (n=80) | Other autoimmune
diseases (n=55) | Healthy control
(n=60) |
|---|
| Age, years | 35±12 | 40±14 | 38±14 |
| Gender, n |
|
|
|
|
Female | 71 | 42 | 41 |
|
Male | 9 | 13 | 19 |
| Disease duration,
years | 4.52±3.81 | 4.83±3.68 | – |
| Anti-dsDNA,
IU/ml | 309.69±238.47 | – | – |
| C3, mg/dl | 82.7±37.8 | – | – |
| C4, mg/dl | 16.3±6.80 | – | – |
| SLEDAI-2K | 10.81±5.02 | – | – |
| SDI | 0.82±1.12 | – | – |
Sample preparation
All serum samples were centrifuged at 1,800 × g for
10 min, immediately aliquoted and stored at −80°C. All samples were
only allowed to thaw once.
Determination of CRT levels in serum
samples by ELISA
The concentration of CRT in serum was measured by
sandwich ELISA (catalogue no. xl-Em1860; Xinle Biology Co., Ltd.,
Shanghai, China) according to the manufacturer's instructions.
Optical density values of each well were assessed using an ELISA
plate reader (Multiskan MK3; Thermo Scientific Inc., Waltham, MA,
USA) at 450 nm.
CRT expression in serum by western
blot analysis
All serum samples were diluted and denatured for 5
min at 95°C following addition of loading buffer. The serum
proteins (20 µg in total) were separated by 10% sodium dodecyl
sulfate-polyacrylamide gel electrophoresis and subsequently were
transferred to the polyvinylidene difluoride membrane for 1 h at a
constant current of 250 mA. The membrane was blocked for 1 h at
room temperature in 5% skim milk/TBST (20 mM Tris-HCl, pH 7.6, 137
mM NaCl and 0.05% Tween 20) and incubated with rabbit anti-human
CRT polyclonal antibody (PA3-900; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) and rabbit anti-human serum albumin antibody
(ab83465; Abcam, Cambridge, UK), which served as a control, for 1 h
at room temperature (dilution, 1:2,500 in 5% skim milk/TBST). After
washing for 30 min with TBST three times, the membranes were
incubated with horseradish peroxidase-conjugated goat anti-rabbit
immunoglobulin G (Bioworld, Irving, TX, USA) for 1 h at room
temperature (dilution, 1:1,000 in 5% skim milk/TBST). Following
washing, proteins were detected with an enhanced chemiluminescence
system (Solarbio Bioscience and Technology Co., Ltd., Shanghai,
China). These data were then analyzed using ImageJ 1.43 software.
CRT expression was normalized against albumin expression.
Clinical and laboratory
measurements
Serum samples were collected from each patient with
SLE, routine hematological tests were performed and serum was
separated and used for biochemical tests and immune assays. The
following clinical and laboratory data were collected: Age, gender
and levels of anti-dsDNA, C3, C4 and anti-Ro52. Anti-dsDNA
antibodies were tested by ELISA (catalogue no. ORG 204G; Orgentec
Diagnostika GmbH, Mainz, Germany), serum concentrations of
complement factors C3 and C4 were determined by immunization rate
scattering turbidimetry (Beckman Coulter, Inc., Brea, CA, USA)
(22) and anti-Ro52 was detected by
ANA Profile 3 EUROLINE (catalogue no. DL 1590-1601-3G, Oumeng Co.,
Beijing, China), according to the manufacturer's instructions.
Statistical analysis
Data are presented as mean ± standard deviation.
Statistical analyses were performed with SPSS software 16.0 (SPSS
Inc., Chicago, IL, USA). Differences among groups were analyzed
with one-way analysis of variance (ANOVA). Student-Newman-Keuls
test was used for a comparison between groups. Correlation was
determined by Pearson's correlation coefficient. P-value of
<0.05 were considered to represent a statistically significant
difference.
Results
Clinical characteristics of the
participants
The detailed clinical characteristics of the
participants are shown in Table I.
There was no significant difference in gender and age amongst the
groups (P>0.05).
Increased levels of CRT in serum from
patients with SLE
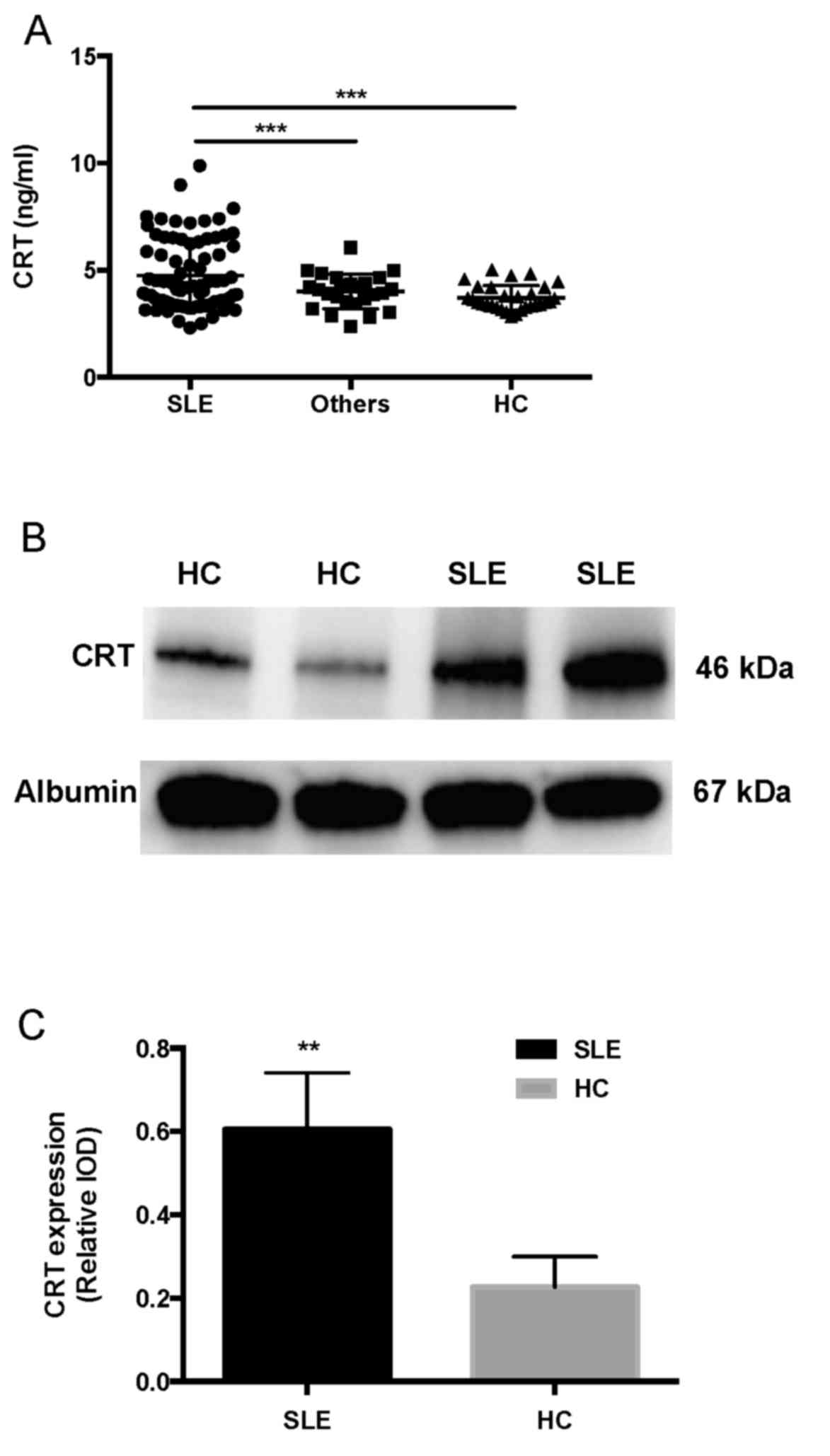
Serum CRT levels were measured by ELISA. Data of CRT
levels from three groups was analyzed by one-way ANOVA. The
difference among these groups was statistically significant
(F=7.589; P<0.001). Pairwise comparisons were performed using
the Student-Newman-Keuls test, revealing that CRT levels in
patients with SLE (4.740±0.646 ng/ml) were significantly higher
than those of other autoimmune diseases (4.008±0.815 ng/ml) and HC
(3.703±0.582 ng/ml) (P<0.001; Fig.
1A).
Western blotting analysis was used to detect the
serum CRT from the serum samples of SLE and HC. CRT levels were
increased in SLE patients compared with HC (Fig. 1B). The integrated optical density of
SLE (23,764±4.685) was significantly higher than HC (11,532±4,936;
P<0.05). The integrated optical density of serum albumin was
also analyzed (36,540±18,653). CRT expression relative to albumin
in patients with SLE (0.60±0.14) was significantly higher compared
with HC (0.23±0.07, P<0.01; Fig.
1C).
Correlation of serum CRT levels with
disease activity in SLE patients
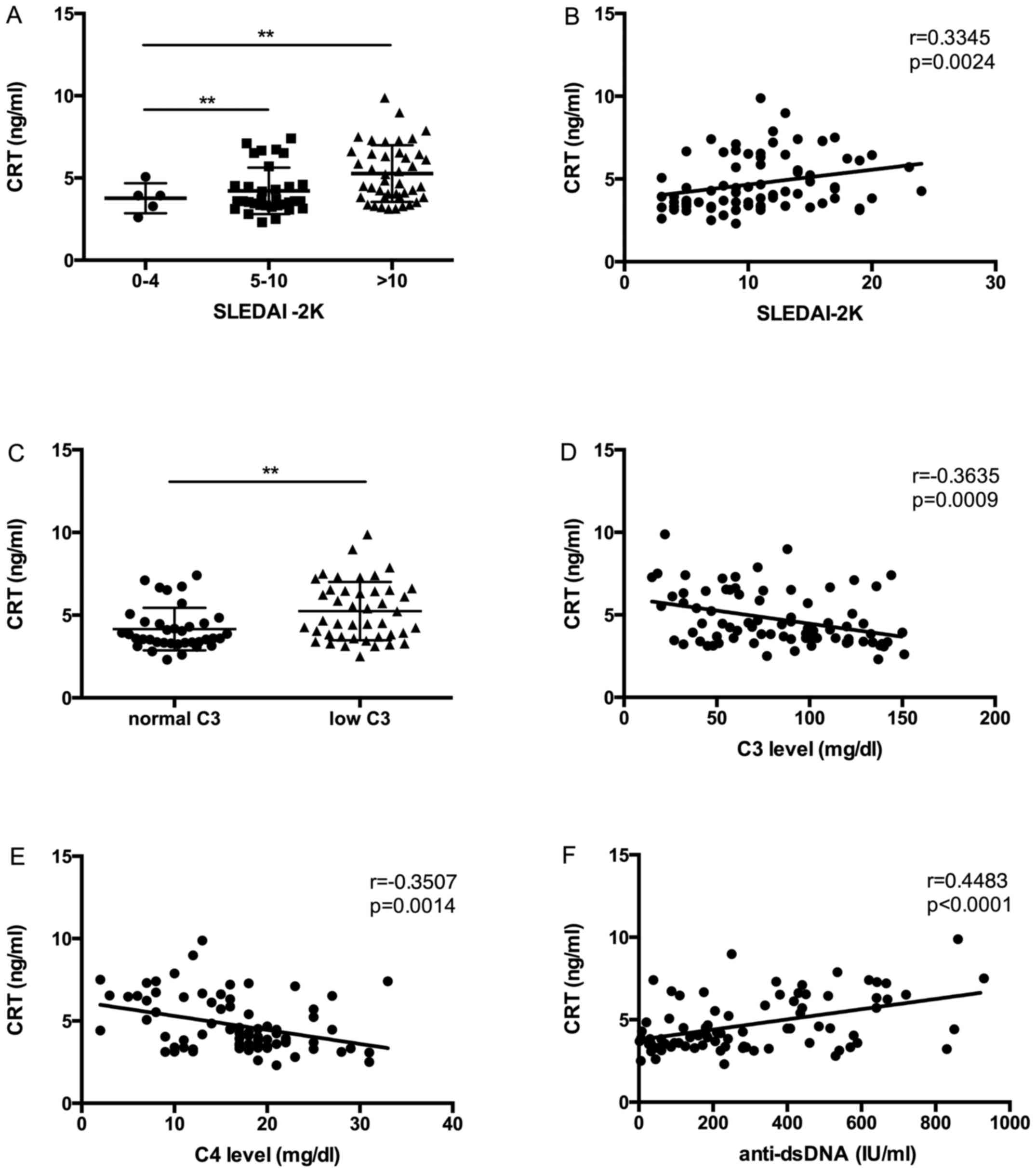
To investigate whether the expression of CRT levels
in SLE serum were correlated with disease activity, CRT levels and
disease activity indices (SLEDAI-2K, C3, C4, anti-dsDNA) were
compared and analyzed by Pearson's correlation coefficient. In
accordance with the SLEDAI-2K flare scoring system (23), SLE patients were divided into three
groups: i) Patients with stable disease (SLEDAI-2K scores from 0 to
4); ii) patients with a mild flare (SLEDAI-2K scores from 5 to 10);
and iii) SLE patients with a moderate to severe disease flare
(SLEDAI-2K scores >10). CRT levels were significantly increased
in patients with SLE who had a mild flare and a moderate to severe
flare of disease than in patients without flare (Fig. 2A). In addition, a significant
correlation was observed between CRT levels and SLEDAI-2K scores in
SLE patients (r=0.3345, P=0.0024) (Fig.
2B).
Complement deficiency is often observed in SLE with
active disease, and C3 is therefore another index of disease
activity (24,25). In the present study, CRT expression
was significantly increased in patients with SLE who had a low
level of C3 (<90 mg/dl) compared with those with normal levels
of C3 (P<0.05; Fig. 2C). It was
additionally revealed that C3 levels were negatively correlated
with CRT levels (r=−0.3635, P=0.0009) (Fig. 2D).
Correlation of serum CRT level with other disease
activity markers like C4 and anti-dsDNA were also analyzed. A
significant negative correlation between CRT level and C4 level was
observed (r=−0.3507, P=0.0014) (Fig.
2E), and a significant positive correlation between CRT level
and anti-dsDNA level was also demonstrated (r=0.4483, P<0.0001)
(Fig. 2F).
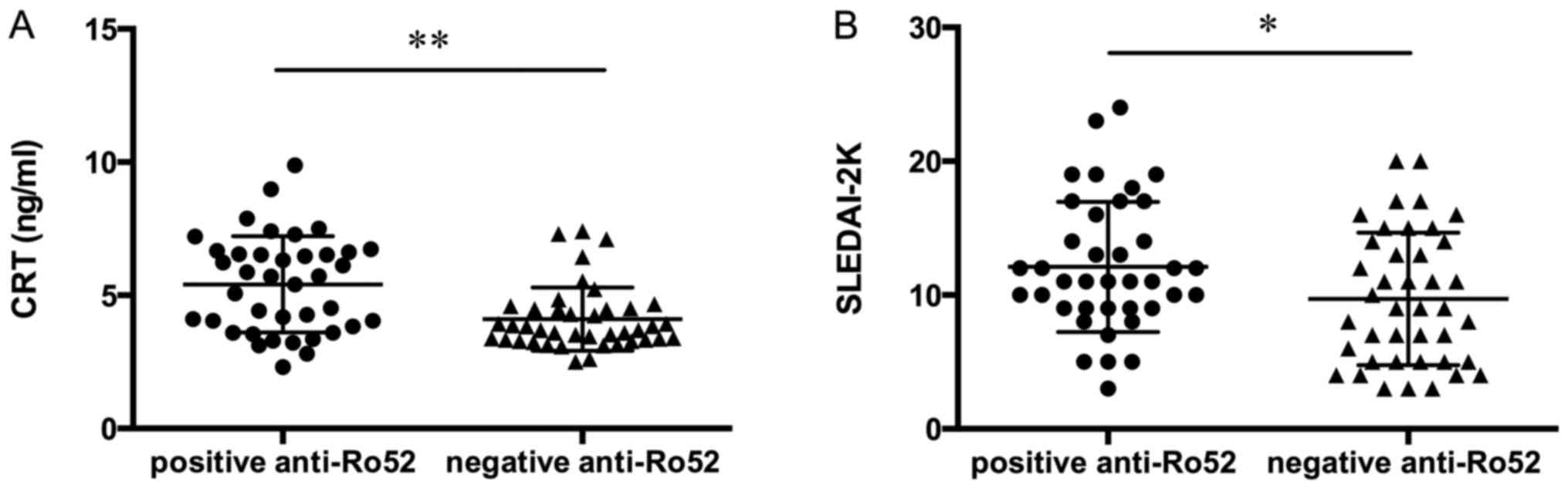
As reported in Fig.
3A, patients with SLE who were positive for anti-Ro52
demonstrated significantly increased levels of CRT compared to
patients negative for anti-Ro52. Furthermore, SLE patients with a
positive anti-Ro52 result reported significantly higher SLEDAI-2K
compared to those patients with a negative anti-Ro52 result
(Fig. 3B).
Association between CRT levels in SLE
patients and organ damage
SLE is a chronic multisystem autoimmune disease that
may lead to morbidity. It has been noted that disease activity,
particularly when individual organs are considered, may result in
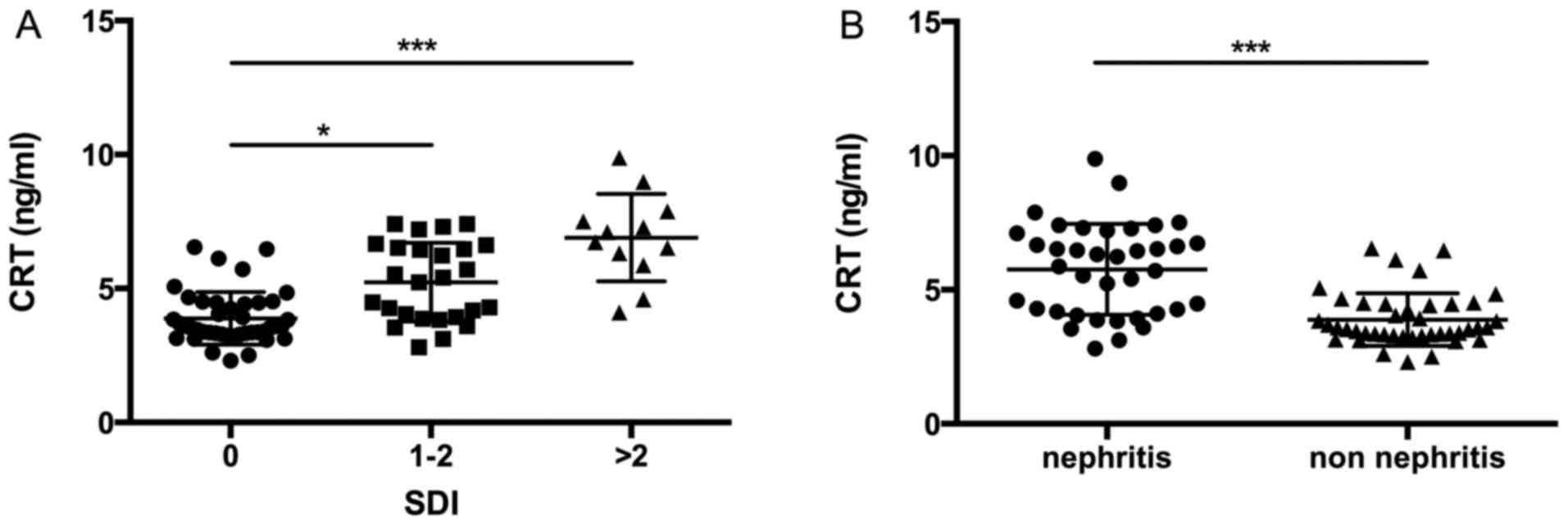
specific organ damage (26,27). The current results revealed that
increased CRT level was associated with different levels of organ
damage in patients with SLE. It was demonstrated that higher levels
of CRT were present in patients with SLE with SDI scores of 1–2 and
in those with SDI scores >2 vs. those without organ damage
(P<0.05 and P<0.001, respectively; Fig. 4A).
LN is one of the most common clinical manifestations
of organ damage in SLE. In the present cohort, 47.5% of patients
(38 of 80 patients with SLE) had either previous or current LN
(Table II). Patients with LN had
higher CRT expression level than those without renal manifestations
(P<0.001; Fig. 4B).
 | Table II.Presence and absence of clinical
features of SLE. |
Table II.
Presence and absence of clinical
features of SLE.
|
| SLE clinical
features present | SLE clinical
features absent |
|
|---|
|
|
|
|
|
|---|
| Clinical
features | N | Mean ± SD | N | Mean ± SD | P-value |
|---|
| Renal | 38 | 5.62±1.845 | 42 | 4.28 ±1.539 | 0.0009 |
| Rash | 22 | 4.79±1.790 | 58 | 4.82±1.701 | NS |
| Arthritis | 24 | 5.01±1.857 | 56 | 4.92±1.540 | NS |
| Serositis | 10 | 4.83±1.691 | 70 | 4.77±1.752 | NS |
| Mucosal ulcer | 11 | 4.85±1.876 | 69 | 4.79±1.505 | NS |
| Hematological | 19 | 4.89±1.892 | 61 | 4.98±1.597 | NS |
| Neurological | 5 | 4.93±1.654 | 75 | 4.98±1.816 | NS |
Discussion
The diagnosis of SLE requires a combination of
clinical manifestations and biomarkers. The traditional laboratory
indices fail to identify the pathogenic processes, organ damage and
therapeutic effects. It is therefore necessary to identify more
biomarkers to monitor disease progression and assess the effects of
treatment of SLE (27). In the
present study, the CRT expression level was investigated as a
correlative analysis with the degree of SLE activity and organ
damage.
Significant epidemiological evidence indicates that
elevated serum CRT is associated with various medical conditions,
particularly autoimmune diseases (28,29). A
previous report noted that serum CRT was associated with the
28-joint count Disease Activity Score and Health Assessment
Questionnaire score in patients with rheumatoid arthritis (30). The current results reported that CRT
levels were increased in patients with SLE compared with patients
with other diseases and HC. These results are consistent with a
previous study that described increased serum levels of CRT in SLE
patients (13). In the present
study, western blotting analysis and ELISA were used to observe the
expression of serum CRT; it was illustrated that the formation of
CRT that may occur in serum in dimers or oligomers, and other CRT
forms were not detected.
In the current study, the elevated serum CRT levels
in SLE patients were correlated with SLEDAI-2K scores, which is the
most common index assessing the level of disease activity in SLE
patients and C3 levels (31). In
addition, serum CRT level was correlated with other disease
activity markers such as C4 and anti-dsDNA levels. The present
investigation also revealed a significant association between CRT
and anti-Ro52 levels in the patients with SLE; the patients who
were positive for anti-Ro52 had higher levels of CRT. The
correlation between serum CRT and notable parameters associated
with SLE disease activity indicates that CRT may represent an
important potential biomarker of disease monitoring and prognosis.
Borba et al (32) previously
reported that increased disease activity in patients with SLE was
associated with the production of serum cytokines such as tumor
necrosis factor α (TNF-α) and interleukin (IL)-6, with higher serum
levels of TNF-α and IL-6 correlating with SLEDAI scores (33,34). In
previous study, Duo et al (35) reported that soluble CRT induces TNF-α
and IL-6 production through mitogen-activated protein kinase and
NF-κB signaling pathways. The present results also suggested a
possible role of CRT in disease activity and pathogenesis of
SLE.
The reason for elevated CRT levels in SLE patients
is poorly understood. Previous studies reported that antibodies of
CRT could be detected in serum of patients with SLE (11,12,36).
However, to the best of our knowledge, the present study is the
first report of a notable correlation between CRT and anti-Ro52. A
previous study suggested that CRT is a protein member of the
Ro/La-RNP complex and is specifically recognized by anti-Ro
autoantibody (12). CRT is
implicated in the phenomenon of ‘epitope spreading’, in which
initiation of immunity to Ro52 induces the production of anti-CRT
autoantibodies in a number of strains of mice (37). Anti-Ro52 reactivity is not
disease-specific but may be of importance in patients with SLE.,
and the role of anti-Ro52 in SLE patients may reflect disease
activity (16). Anti-Ro52 and CRT
are suggested to participate in pathogenesis of SLE (12,38); the
significance of CRT and anti-Ro52 in SLE therefore represent the
subject of subsequent work.
CRT expression was reported in the present study to
be increased in SLE with ongoing or cumulative organ damage, as
determined by SDI score and the presence of LN. However, CRT
expression did not participate in clinical manifestations other
than LN. Although the CRT level in SLE patients with the presence
of arthritis is higher than those with the absence of arthritis,
there was no significant correlation between these. Observations of
the current study indicate CRT as a promising biomarker for
monitoring SLE disease progression and a major manifestation in SLE
patients.
CRT serves a crucial role in regulating
intracellular Ca2+ homeostasis (39). Previous studies by Sela-Brown et
al (40) and Wheeler et
al (41) reported that
1,25-dihydroxyvitaminD3 can be inhibited by CRT in vitro and
in vivo. Subsequent study elaborated on the link between
serum concentrations of 1,25-dihydroxyvitaminD3 and the development
and progression of SLE, finding that 1,25-dihydroxyvitaminD3 serum
concentrations were inversely correlated with disease activity and
organ damage (42). Low serum
1,25-dihydroxyvitaminD3 is associated with photosensitization,
arthritis and kidney damage (43,44). The
current study focused on the relationship between serum CRT level
and organ damage in SLE patients, suggesting that elevated CRT
expression is associated with cumulative organ damage in SLE.
However, this was not a functional study of CRT, meaning that the
underlying mechanism requires additional investigation.
In conclusion, the present report demonstrates that
the elevated serum CRT levels in SLE patients parallel the degree
of disease activity and organ damage. These observations provide
additional evidence for a possible role of CRT in predicting
long-term outcome and prognosis in patients with SLE.
Acknowledgements
The current study was supported by the National
Science Foundation of China (grant no. 81601820), Tianjin Natural
Science Foundation (grant no. 15JCQNJC11600 and 15JCYBJC27400) and
Tianjin City High School Science & Technology Fund Planning
Project (grant no. 20140124).
References
|
1
|
Liang P, Tang Y, Fu S, Lv J, Liu B, Feng
M, Li J, Lai D, Wan X and Xu A: Basophil count, a marker for
disease activity in systemic lupus erythematosus. Clin Rheumatol.
34:891–896. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dipti TR, Azam MS, Sattar MH and Rahman
SA: Detection of anti-nuclear antibody by immunofluorescence assay
and enzyme immunoassay in childhood systemic lupus erythematosus:
Experience from Bangladesh. Int J Rheum Dis. 15:121–125. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Das UN: Current and emerging strategies
for the treatment and management of systemic lupus erythematosus
based on molecular signatures of acute and chronic inflammation. J
Inflamm Res. 3:143–170. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Devaraju P, Witte T, Schmidt RE, Gulati R
and Negi VS: Immunoglobulin-like transcripts 6 (ILT6) polymorphism
influences the anti-Ro60/52 autoantibody status in South Indian SLE
patients. Lupus. 23:1149–1155. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Eggleton P and Llewellyn DH:
Pathophysiological roles of calreticulin in autoimmune disease.
Scand J Immunol. 49:466–473. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Eggleton P, Ward FJ, Johnson S, Khamashta
MA, Hughes GR, Hajela VA, Michalak M, Corbett EF, Staines NA and
Reid KB: Fine specificity of autoantibodies to calreticulin:
Epitope mapping and characterization. Clin Exp Immunol.
120:384–391. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yan Q, Murphy-Ullrich JE and Song Y:
Structural insight into the role of thrombospondin-1 binding to
calreticulin in calreticulin-induced focal adhesion disassembly.
Biochemistry. 49:3685–3694. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Goëb V, Thomas-L'Otellier M, Daveau R,
Charlionet R, Fardellone P, Le Loët X, Tron F, Gilbert D and
Vittecoq O: Candidate autoantigens identified by mass spectrometry
in early rheumatoid arthritis are chaperones and citrullinated
glycolytic enzymes. Arthritis Res Ther. 11:R382009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
de Almeida DE, Ling S and Holoshitz J: New
insights into the functional role of the rheumatoid arthritis
shared epitope. FEBS Lett. 585:3619–3626. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Michalak M, Groenendyk J, Szabo E, Gold LI
and Opas M: Calreticulin, a multi-process calcium-buffering
chaperone of the endoplasmic reticulum. Biochem J. 417:651–666.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
van den Berg RH, Siegert CE, Faber-Krol
MC, Huizinga TW, van Es LA and Daha MR: Anti-C1q
receptor/calreticulin autoantibodies in patients with systemic
lupus erythematosus (SLE). Clin Exp Immunol. 111:359–364. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Boehm J, Orth T, Van Nguyen P and Söling
HD: Systemic lupus erythematosus is associated with increased
auto-antibody titers against calreticulin and grp94, but
calreticulin is not the Ro/SS-A antigen. Eur J Clin Invest.
24:248–257. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hong C, Qiu X, Li Y, Huang Q, Zhong Z,
Zhang Y, Liu X, Sun L, Lv P and Gao XM: Functional analysis of
recombinant calreticulin fragment 39–272: Implications for
immunobiological activities of calreticulin in health and disease.
J Immunol. 185:4561–4569. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yuan J, Li LI, Wang Z, Song W and Zhang Z:
Dyslipidemia in patients with systemic lupus erythematosus:
Association with disease activity and B-type natriuretic peptide
levels. Biomed Rep. 4:68–72. 2016.PubMed/NCBI
|
|
15
|
Urowitz MB, Isenberg DA and Wallace DJ:
Safety and efficacy of hCDR1 (Edratide) in patients with active
systemic lupus erythematosus: Results of phase II study. Lupus Sci
Med. 2:e0001042015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kvarnstrom M, Dzikaite-Ottosson V,
Ottosson L, Gustafsson JT, Gunnarsson I, Svenungsson E and
Wahren-Herlenius M: Autoantibodies to the functionally active
RING-domain of Ro52/SSA are associated with disease activity in
patients with lupus. Lupus. 22:477–485. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Romero-Diaz J, Isenberg D and
Ramsey-Goldman R: Measures of adult systemic lupus erythematosus:
Updated version of British Isles Lupus Assessment Group (BILAG
2004), European Consensus Lupus Activity Measurements (ECLAM),
Systemic Lupus Activity Measure, Revised (SLAM-R), Systemic Lupus
Activity Questionnaire for Population Studies (SLAQ), Systemic
Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K), and
Systemic Lupus International Collaborating Clinics/American College
of Rheumatology Damage Index (SDI). Arthritis Care Res (Hoboken).
63 Suppl 1:S37–S46. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ziegelasch M, van Delft MA, Wallin P,
Skogh T, Magro-Checa C, Steup-Beekman GM, Trouw LA, Kastbom A and
Sjöwall C: Antibodies against carbamylated proteins and cyclic
citrullinated peptides in systemic lupus erythematosus: Results
from two well-defined European cohorts. Arthritis Res Ther.
18:2892016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Imrich R, Alevizos I, Bebris L, Goldstein
DS, Holmes CS, Illei GG and Nikolov NP: Predominant glandular
cholinergic dysautonomia in patients with primary Sjögren's
syndrome. Arthritis Rheumatol. 67:1345–1352. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang C, Liao Q, Hu Y and Zhong D: T
lymphocyte subset imbalances in patients contribute to ankylosing
spondylitis. Exp Ther Med. 9:250–256. 2015.PubMed/NCBI
|
|
21
|
Johnson SR, Fransen J, Khanna D, Baron M,
van den Hoogen F, Medsger TA Jr..Peschken CA, Carreira PE,
Riemekasten G, Tyndall A, et al: Validation of potential
classification criteria for systemic sclerosis. Arthritis Care Res
(Hoboken). 64:358–367. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhu XH, Chen Q, Ke JW, Liu JM, Li L, Li J,
He MJ and Hu CL: Clinical analysis of immune function changes in
children with bronchial pneumonia. Zhongguo Dang Dai Er Ke Za Zhi.
15:175–178. 2013.(In Chinese). PubMed/NCBI
|
|
23
|
Munroe ME, Vista ES, Guthridge JM,
Thompson LF, Merrill JT and James JA: Pro-inflammatory adaptive
cytokines and shed tumor necrosis factor receptors are elevated
preceding systemic lupus erythematosus disease flare. Arthritis
Rheumatol. 66:1888–1899. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Papp K, Végh P, Hóbor R, Szittner Z, Vokó
Z, Podani J, Czirják L and Prechl J: Immune complex signatures of
patients with active and inactive SLE revealed by multiplex protein
binding analysis on antigen microarrays. PLoS One. 7:e448242012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Brendan M and Boackle SA: Linking
complement and anti-dsDNA antibodies in the pathogenesis of
systemic lupus erythematosus. Immunol Res. 55:10–21. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Magro-Checa C, Zirkzee EJ, Huizinga TW and
Steup-Beekman GM: Management of neuropsychiatric systemic lupus
erythematosus: Current approaches and future perspectives. Drugs.
76:459–483. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wu Y, Zhang F, Ma J, Zhang X, Wu L, Qu B,
Xia S, Chen S, Tang Y and Shen N: Association of large intergenic
noncoding RNA expression with disease activity and organ damage in
systemic lupus erythematosus. Arthritis Res Ther. 17:1312015.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gelebart P, Opas M and Michalak M:
Calreticulin, a Ca2+-binding chaperone of the endoplasmic
reticulum. Int J Biochem Cell Biol. 37:260–266. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
He MC, Wang J, Wu J, Gong FY, Hong C, Xia
Y, Zhang LJ, Bao WR and Gao XM: Immunological activity difference
between native calreticulin monomers and oligomers. PLoS One.
9:e1055022014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ni M, Wei W, Wang Y, Zhang N, Ding H, Shen
C and Zheng F: Serum levels of calreticulin in correlation with
disease activity in patients with rheumatoid arthritis. J Clin
Immunol. 33:947–953. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Compagno M, Gullstrand B, Jacobsen S,
Eilertsen GØ, Nilsson JÅ, Lood C, Jönsen A, Truedsson L, Sturfelt G
and Bengtsson AA: The assessment of serum-mediated phagocytosis of
necrotic material by polymorphonuclear leukocytes to diagnose and
predict the clinical features of systemic lupus erythematosus: An
observational longitudinal study. Arthritis Res Ther. 18:442016.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Borba VZ, Vieira JG, Kasamatsu T,
Radominski SC, Sato EI and Lazaretti-Castro M: Vitamin D deficiency
in patients with active systemic lupus erythematosus. Osteoporos
Int. 20:427–433. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
McCarthy EM, Smith S, Lee RZ, Cunnane G,
Doran MF, Donnelly S, Howard D, O'Connell P, Kearns G, Ní Gabhann J
and Jefferies CA: The association of cytokines with disease
activity and damage scores in systemic lupus erythematosus
patients. Rheumatology (Oxford). 53:1586–1594. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Umare V, Pradhan V, Nadkar M, Rajadhyaksha
A, Patwardhan M, Ghosh KK and Nadkarni AH: Effect of
proinflammatory cytokines (IL-6, TNF-α, and IL-1β) on clinical
manifestations in Indian SLE patients. Mediators Inflamm.
2014:3852972014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Duo CC, Gong FY, He XY, Li YM, Wang J,
Zhang JP and Gao XM: Soluble calreticulin induces tumor necrosis
factor-a (TNF-α) and interleukin (IL)-6 production by macrophages
through mitogen-activated protein kinase (MAPK) and NFκB signaling
pathways. Int J Mol Sci. 15:2916–2928. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Routsias JG, Tzioufas AG,
Sakarellos-Daitsiotis M, Sakarellos C and Moutsopoulos HM:
Calreticulin synthetic peptide analogues: Anti-peptide antibodies
in autoimmune rheumatic diseases. Clin Exp Immunol. 91:437–441.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kinoshita G, Keech CL, Sontheimer RD,
Purcell A, McCluskey J and Gordon TP: Spreading of the immune
response from 52 kDaRo and 60 kDaRo to calreticulin in experimental
autoimmunity. Lupus. 7:7–11. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Menéndez A, Gómez J, Caminal-Montero L,
Díaz-López JB, Cabezas-Rodríguez I and Mozo L: Common and specific
associations of anti-SSA/Ro60 and anti-Ro52/TRIM21 antibodies in
systemic lupus erythematosus. ScientificWorldJournal.
2013:8327892013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wang WA, Groenendyk J and Michalak M:
Calreticulin signaling in health and disease. Int J Biochem Cell
Biol. 44:842–846. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Sela-Brown A, Russell J, Koszewski NJ,
Michalak M, Naveh-Many T and Silver J: Calreticulin inhibits
vitamin D's action on the PTH gene in vitro and may prevent vitamin
D's effect in vivo in hypocalcemic rats. Mol Endocrinol.
12:1193–1200. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wheeler DG, Horsford J, Michalak M, White
JH and Hendy GN: Calreticulin inhibits vitamin D3 signal
transduction. Nucleic Acids Res. 23:3268–3274. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Amital H, Szekanecz Z, Szücs G, Dankó K,
Nagy E, Csépány T, Kiss E, Rovensky J, Tuchynova A, Kozakova D, et
al: Serum concentrations of 25-OH vitamin D in patients with
systemic lupus erythematosus (SLE) are inversely related to disease
activity: Is it time to routinely supplement patients with SLE with
vitamin D? Ann Rheum Dis. 69:1155–1157. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Mandal M, Tripathy R, Panda AK, Pattanaik
SS, Dakua S, Pradhan AK, Chakraborty S, Ravindran B and Das BK:
Vitamin D levels in Indian systemic lupus erythematosus patients:
Association with disease activity index and interferon alpha.
Arthritis Res Ther. 16:R492014. View
Article : Google Scholar : PubMed/NCBI
|
|
44
|
Schoindre Y, Jallouli M, Tanguy ML,
Ghillani P, Galicier L, Aumaître O, Francès C, Le Guern V, Lioté F,
Smail A, et al: Lower vitamin D levels are associated with higher
systemic lupus erythematosus activity, but not predictive of
disease flare-up. Lupus Sci Med. 1:e0000272014. View Article : Google Scholar : PubMed/NCBI
|