Introduction
Adult community-acquired pneumonia (ACAP) is the
most prevalent pulmonary infectious disease and is usually acquired
via inhalation or aspiration of a pathogenic organism (1). Patients with ACAP may classically
present with fever, a productive cough with purulent sputum,
dyspnea and pleuritic chest pain. If a misdiagnosis is made,
patients may become severely ill and may require a longer duration
of therapy. ACAP is typically caused by Streptococcus pneumoniae,
β-hemolytic Streptococci, Klebsiella pneumoniae or Moraxella
catarrhalis (2). General computed
tomography (CT) features of patients with pneumonia of different
etiologies include patchy opacity attenuation and ground-glass
opacity shadowing of the lobe and segment (3). In addition, ACAP patients often present
with enlarged mediastinal lymph nodes, visible in their chest CT
images. However, giant irregular swollen lymph nodes associated
with ACAP are rarely reported, and may be confused with enlarged
lymph node masses. Such masses are frequently seen in patients with
lung cancers, tuberculosis or lymphoma, and this may therefore lead
to the misdiagnosis of ACAP as one of these conditions.
Case report
Written informed consent was provided by the patient
regarding the publication of the case details in the present study.
A 24-year old male was admitted to the emergency room of Yangpu
Hospital (Shanghai, China) presenting with a moderate fever
(38.1–38.6°C), fatigue, mild cough with slight purulent yellow
sputum, and intermittent shortness of breath. He had been suffering
these symptoms for ~3 days. Prior to admission, he visited his
local hospital because of similar symptoms, and a chest X-ray as
performed. The X-ray images showed nothing remarkable. The patient
then rested at home for 3 days, and took traditional Chinese
medicine as prescribed (clearing heat and detoxification oral
liquid; 10 ml three times a day). However, there was no improvement
to his cough and fever, and so he was referred to Yangpu Hospital.
His past medical history indicated that he was healthy and had no
major or serious illness except that he caught colds frequently.
Clinical observations performed in the Emergency Department found
that he exhibited a temperature of 38.6°C, pulse rate of 92 bpm,
respiratory rate of 28 breaths/min, and blood pressure of 98/64
mmHg. The physical examination was unremarkable.
Blood was taken when the patient arrived in the
emergency room. Laboratory blood tests indicated elevated
C-reactive protein levels (22 mg/dl), normal hemoglobin with high
leukocytosis (total leukocytes, 11,200 mm3; differential
count, neutrophils 75.1%, lymphocytes 20%), a normal erythrocyte
sedimentation rate of 16 (0–20 mm/h), tuberculosis acid-fast
staining, and L-Y culture negative. No sputum culture of bacterial
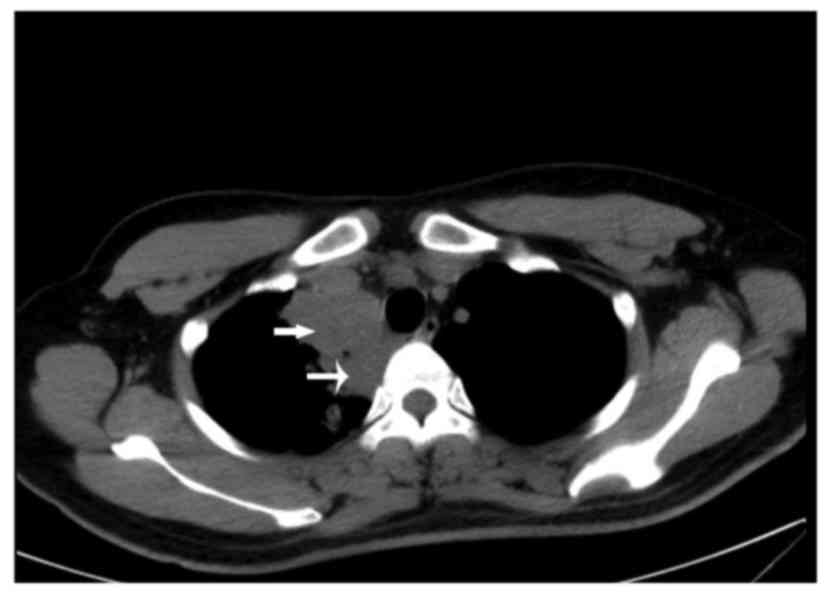
pathogens was ordered. The chest CT scan revealed patchy areas of
ground-glass attenuation and a small consolidation on the first
segment of the right upper lung zone that was accompanied by a
right upper mediastinal giant irregular lymphadenopathy mass
(Figs. 1 and 2). Mild enhancement of the giant
mediastinal lymphadenopathy mass was also noted on the
contrast-enhanced CT scan (Fig.
3).
Radiological findings of pneumonia are characterized
by the type and pattern of opacities, such as patchy areas of
ground-glass attenuation and consolidation of zonal distribution
(3). According to this, the patient
was given a clinical diagnosis of bacterial pneumonia with
lymphadenopathy and prescribed antibiotic treatment. The patient
was administered with intravenous (IV) azithromycin (0.25 g drip,
once daily for 3 days), and subsequently was IV cefuroxime was
administered (3 g drip, once daily for 10 days) as an outpatient.
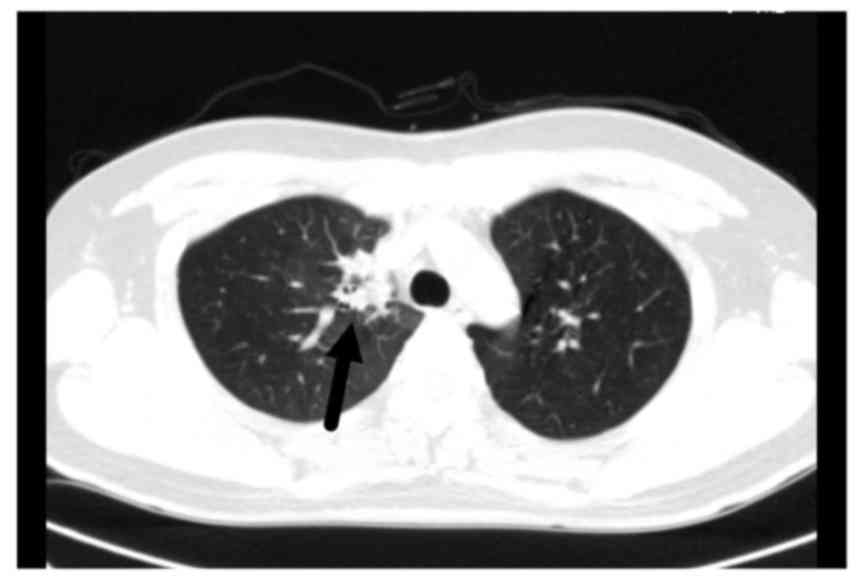
The patient was fully recovered following antibiotic therapy. All
blood results were within the normal range, and a follow-up chest
CT scan following 7 days of treatment revealed only a small nodular
lesion (Fig. 4). Another CT scan was
performed following 2 weeks of treatment and was found to be
completely normal (Fig. 5).
The patient was eventually diagnosed with ACAP,
non-severe type, based on his clinical manifestations, radiological
findings, and the local epidemiological forecast.
Discussion
Community-acquired pneumonia (CAP) is acquired
through normal social contact in the community as opposed to during
hospitalization (hospital-acquired pneumonia) (1). CAP affects people of all ages and is a
major cause of morbidity and health care expenditure (4,5). It
typically presents with problems such as difficulty breathing,
fever, chest pains, and cough (1,5). CAP may
be divided into severe and non-severe types based on the pneumonia
score (1).
The etiologies of CAP include bacteria, viruses,
fungi, and parasites (2,6). Historically, Streptococcus pneumoniae
was the pathogen most commonly responsible for CAP (1). Prior to the advent of antibiotics and
vaccination, it was a leading cause of mortality (1,5). At
present, the most common bacterial causes of pneumonia are the
so-called atypical bacteria, Mycoplasma pneumoniae and
Chlamydophila pneumonia (7).
Legionella pneumophila is also considered atypical; however, it is
less common (1,2,6). A
survey was conducted in the Chinese metropolitan areas, including
Shanghai and Beijing, where pneumonia is widespread, which found
that Mycoplasma was the most common pathogen associated with
pneumonia, followed by Streptococcus pneumonia (8). CAP may be diagnosed based on clinical
manifestations alone, or using X-rays, sputum examinations, and
other tests. In Yangpu Hospital, no routine bacterial culture is
required for the diagnosis of mild CAP. The patient presented here
fulfilled the non-severe CAP diagnosis criteria with the supporting
evidence of clinical manifestations and chest X-ray imaging. He was
safely treated as an outpatient.
Cases of pneumonia that are caused by different
pathogens nonetheless typically have common presentations and
features in chest X-rays and CT images (3,9). CT
images may reveal airspace involvement, which appears as lobular or
segmental patchy areas of consolidation, nodular lesions,
ground-glass opacity, and mild lymph node enlargement in isolated
regions (3). Chest radiography is
less accurate than CT in the detection of segmental and patchy
areas of consolidation (3,9).
In the present case study, the predominant
radiographic abnormalities observed included the patchy areas of
parenchymal opacification and ground-glass attenuation present in
the right upper lung zones, and a large irregular mild enhanced
mass mimicking lymphoma adjacent to the paratrachea in the right
upper mediastinum on CT images. To the best of our knowledge, the
enlarged lymph nodes may have resulted from infectious diseases, as
the lymph nodes had a well-defined border and were apparently
contrast-enhanced in the CT images, and the lymph nodes were
scattered in mediastinal areas. Contrastingly, the lymph nodes in
lymphoma may appear altogether in a large mass with irregular
contour, and the CT images may demonstrate that the lymph nodes are
mild-moderate contrast-enhanced with a border that is not well
defined (3,9). The follow-up CT scan performed
following 2 weeks of treatment revealed that the initial
abnormalities were resolved completely. To the best of our
knowledge, it is extremely rare to observe pneumonia lesions that
are accompanied by such a large mediastinal lymph node mass.
The pathogenic process of all types of pneumonia is
able to cause acute or chronic inflammation in the mediastinal
lymph nodes, lymph node hyperemia edema, hyperplasia of lymphocytes
and macrophages, and infiltration of neutrophils, monocytes, and
plasma cells (7,10). In addition, the lymph nodes may
experience necrosis and granuloma formation (7,11).
Clinically, lymph node enlargement induced by acute
inflammation is typically secondary to the corresponding drainage
area of infection (10,11). This case was atypical as abnormal
lymph node enlargement with irregular fragments reaching >40 mm
were observed, most probably as a result of lung inflammation
spreading to the adjacent mediastinal lymph nodes and causing
excessive inflammatory reactions causing them to merge into a
larger one. This patient was young, and his immune system was
otherwise robust, which may be why he experienced such a strong and
excessive response in the lymph nodes.
Unusually enlarged lymph nodes resulting from
pneumonia may cause confusion in diagnosis. Typically, the
inflammatory lymph nodes in pneumonia are characterized by
mediastinal scattered lymph nodes forming a circular shadow, and
the sizes are generally ≤15 mm (12). In the present case, there was a
margin with a clear boundary, with no enhancement on the enhanced
CT scan. The enlarged lymph nodes returned to their normal size
with decreasing inflammation following effective antibiotic
therapy.
In mediastinal lymph node tuberculosis, the lymph
nodes are swollen and accompanied by central necrosis that
frequently results in calcification in the healed sites (3,10,13). In
addition, ring-enhancement on the enhanced CT scan is observed
(13).
In mediastinal lymphoma, the mediastinal lymphoma is
typically located in the front mediastinum and is symmetrically and
bilaterally widened with a wavy edge (seen more in Hodgkin's
Disease) or one side is broadened (seen more in non-Hodgkin's
lymphoma) (14). The lymph nodes are
often fused into clumps, which results in mild-to-moderate
enhancement on enhanced CT scans (Fig.
6) (15). The primary clinical
symptoms include fever and superficial lymph node enlargement
(14). The lymphoma may become
smaller or disappear completely soon after radiation therapy
(14–16).
In cases of lymph node metastasis, there is often a
history of primary tumors, such as lung cancer (17). Additionally, enhanced CT scans of
metastatic lymph nodes often have a notably enhanced ring or patch
shapes (16,18). As a result, it is difficult to make a
differential diagnosis in the early metastatic stage only based on
imaging.
In conclusion, mediastinal lymph node enlargement
may be induced by many illnesses including metastasis,
tuberculosis, chronic lymphocytic leukemia, Hodgkin's disease and
more. Local lymph node enlargement typically indicates a local
infection. Atypical pneumonia may cause confusion when making a
diagnosis based on imaging analysis. The present case study
demonstrates that unusually enlarged mediastinal lymph nodes may be
present in patients with pneumonia and are most likely associated
with a strong immune response to pneumonia.
Glossary
Abbreviations
Abbreviations:
|
ACAP
|
adult community-acquired pneumonia
|
|
CT
|
computed tomography
|
|
CAP
|
community-acquired pneumonia
|
References
|
1
|
Carbonara S, Monno L, Longo B and Angarano
G: Community-acquired pneumonia. Curr Opin Pulm Med. 15:261–273.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Leesik H, Ani U, Juhani A and Altraja A:
Microbial pathogens of adult community-acquired pneumonia in
Southern Estonia. Medicina (Kaunas). 42:384–394. 2006.PubMed/NCBI
|
|
3
|
Nambu A, Ozawa K, Kobayashi N and Tago M:
Imaging of community-acquired pneumonia: Roles of imaging
examinations, imaging diagnosis of specific pathogens and
discrimination from noninfectious diseases. World J Radiol.
6:779–793. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Broulette J, Yu H, Pyenson B, Iwasaki K
and Sato R: The incidence rate and economic burden of
community-acquired pneumonia in a working-age population. Am Health
Drug Benefits. 6:494–503. 2013.PubMed/NCBI
|
|
5
|
Herzig SJ, Howell MD, Ngo LH and
Marcantonio ER: Acid-suppressive medication use and the risk for
hospital-acquired pneumonia. JAMA. 301:2120–2128. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kurutepe S, Ecemiş T, Ozgen A, Biçmen C,
Celik P, Aktoğu Özkan S and Sürücüoğlu S: Investigation of
bacterial etiology with conventional and multiplex PCR methods in
adult patients with community-acquired pneumonia. Mikrobiyol Bul
Bul methods in adult patients with community-acquired pneumonia.
Mikrobiyol Bul. 46:523–531. 2012.(In Turkish). PubMed/NCBI
|
|
7
|
Drasbek M, Nielsen PK, Persson K,
Birkelund S and Christiansen G: Immune response to Mycoplasma
pneumoniae P1 and P116 in patients with atypical pneumonia analyzed
by ELISA. BMC Microbiol. 4:72004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu YN, Chen MJ, Zhao TM, Wang H, Wang R,
Liu QF, Cai BQ, Cao B, Sun TY, Hu YJ, et al: A multicentre study on
the pathogenic agents in 665 adult patients with community acquired
pneumonia in cities of China. Zhonghua Jie He He Hu Xi Za Zhi.
29:3–8. 2006.(In Chinese). PubMed/NCBI
|
|
9
|
Okada F, Ando Y, Tanoue S, Ishii R,
Matsushita S, Ono A, Maeda T and Mori H: Radiological findings in
acute Haemophilus influenzae pulmonary infection. Br J Radiol.
85:121–126. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Attili AK, Kazerooni EA, Gross BH,
Flaherty KR and Martinez FJ: Thoracic lymph node enlargement in
usual interstitial pneumonitis and nonspecific-interstitial
pneumonitis: Prevalence, correlation with disease activity and
temporal evolution. J Thorac Imaging. 21:288–292. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Weaver JL, Chapdelaine JM, Descotes J,
Germolec D, Holsapple M, House R, Lebrec H, Meade J, Pieters R,
Hastings KL and Dean JH: Evaluation of a lymph node proliferation
assay for its ability to detect pharmaceuticals with potential to
cause immune-mediated drug reactions. J Immunotoxicol. 2:11–20.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Qu JX, Gu L, Pu ZH, Yu XM, Liu YM, Li R,
Wang YM, Cao B and Wang C: Beijing Network for Adult
Community-Acquired Pneumonia (BNACAP): Viral etiology of
community-acquired pneumonia among adolescents and adults with mild
or moderate severity and its relation to age and severity. BMC
Infect Dis. 15:892015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hocke M, Menges M, Topalidis T, Dietrich
CF and Stallmach A: Contrast-enhanced endoscopic ultrasound in
discrimination between benign and malignant mediastinal and
abdominal lymph nodes. J Cancer Res Clin Oncol. 134:473–480. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sugimoto S, Soh J, Maki Y, Kurosaki T,
Yamane M, Toyooka S, Oto T and Miyoshi S: Primary mediastinal
lymphoma; a clinicopathologic case series. Kyobu Geka. 65:527–531.
2012.(In Japanese). PubMed/NCBI
|
|
15
|
Knipe Henry Dr, Gaillard Frank Dr, et al:
Radiographic features. Mediastinal lymphoma.
|
|
16
|
Mehrian P and Ebrahimzadeh SA:
Differentiation between sarcoidosis and Hodgkin's lymphoma based on
mediastinal lymph node involvement pattern: Evaluation using spiral
CT scan. Pol J Radiol. 78:15–20. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Juanpere S, Cañete N, Ortuño P, Martínez
S, Sanchez G and Bernado L: A diagnostic approach to the
mediastinal masses. Insights Imaging. 4:29–52. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tomiyama N, Honda O, Tsubamoto M, Inoue A,
Sumikawa H, Kuriyama K, Kusumoto M, Johkoh T and Nakamura H:
Anterior mediastinal tumors: Diagnostic accuracy of CT and MRI. Eur
J Radiol. 69:280–288. 2009. View Article : Google Scholar : PubMed/NCBI
|