Introduction
Diabetes mellitus is a metabolism-related chronic
disease that affects individuals worldwide. Poorly controlled blood
glucose levels typically lead to various complications in organs
that are rich in microvasculature, including nephropathy (1). Diabetic nephropathy (DN) is a high risk
factor for vascular disease, and is common among patients with type
2 diabetes (2). DN is characterized
by albuminuria, hyperfiltration and hyperpermeability to
macromolecules, proteinuria and end-stage renal failure (3). Although the underlying mechanism of
type 2 DN (T2DN) development remains unclear, this multifactorial
disease may be associated with factors such as hyperglycemia,
hyperlipidemia, oxidative stress and inflammatory cytokines
(4,5).
Hyperglycemia causes oxidative stress and increases
the generation of reactive oxygen species (ROS) (4). ROS damage the cell membrane, inactivate
antioxidant enzymes, alter endogenous antioxidant gene expression
and contribute to the pathogenesis of DN (6–8).
Furthermore, ROS activate signal transduction cascades which induce
the expression of profibrotic factors, including fibronectin, lamin
and Collagen IV, which contribute to the accumulation of
extracellular matrix (ECM) and inflammatory gene expression, such
as IL-6. Furthermore, transforming growth factor (TGF)-β1
expression is activated by ROS, in combination with its downstream
effector connective tissue growth factor (CTGF), which contributes
to tissue fibrosis (9,10) and promotes cell proliferation and ECM
synthesis, which is one of the predominant pathological
characteristics of DN (11,12).
Metformin, which is an oral hypoglycemic diguanide
drug, has been widely used for several decades in the treatment for
type 2 diabetes mellitus (T2DM), particularly in patients with
obesity (13). Metformin reduces
diabetic complications by reducing glucose levels in the body
(13); and although the detailed
mechanism underlying these benefits is yet to be elucidated, it is
generally acknowledged that metformin restores the body's response
to insulin. It has been demonstrated that metformin reduces
gluconeogenesis in the liver and also inhibits sugar uptake in the
intestines (14); whereas another
previous study has demonstrated that it may reduce ROS generation
(15). Furthermore, metformin has
exhibited renal protective effects against a nephrotoxic agent in
some previous studies (16,17).
The present study aimed to explore the potential
renal protective effect of metformin on the progression of DN in
high-fat diet (HFD) and STZ-induced diabetic rats, and the
underlying mechanism.
Materials and methods
Regents
Metformin was purchased from Tianjin Pacific
Chemical & Pharmaceutical Co., Ltd., (Tianjin, China).
Captopril was purchased from Shanghai Pukang Pharmaceutical Co.,
Ltd., (Shanghai, China). Detection kits for total cholesterol (TC;
A111-1), triglyceride (TG; A110-1), high density
lipoprotein-cholesterol (HDL-c; A112-1), low density
lipoprotein-cholesterol (LDL-c; S113-1), serum creatinine (Scr),
blood urea nitrogen (BUN), superoxide dismutase (SOD; A001-1),
malondialdehyde (MDA; A003-1) and glutathione peroxidase (GSH-Px;
A005) were purchased from Nanjing Jiancheng Institute of
Biotechnology (Nanjing, China).
Animals and experimental design
A total of 80 male Wistar rats, aged 7 weeks and
weighing 160–180 g, were obtained from The Experimental Animal
Center at Jilin University (Jilin, China). Rats were housed in
normal cages under controlled conditions (25°C and a 12 h
light/dark cycle) with ad libitum access to a standard
pellet diet (SPD) and water. Experiments were performed in
accordance with the Guide for the Care and Use of Laboratory
Animals of Jilin University, and were approved by the Ethics
Committee. Following acclimatization for one week, rats were
divided into two groups, and were either fed with SPD or a HFD,
consisting of 10% fat, 20% sucrose, 10% protein and 60% pulverized
standard rat pellet, for eight weeks. Following overnight fasting,
the rats fed with HFD were intravenously (i.v) injected with a
single low-dose of STZ (30 mg/kg; Sigma-Aldrich, St. Louis, MO,
USA), whereas the rats in the control SFD group were treated with a
vehicle control buffer. Two weeks following STZ injection, fasting
blood glucose (FBG) levels were tested and the rats with high FBG
(>11.1 mol/l) were used for the subsequent experiments.
Diabetic rats were randomly divided into three equal
groups (n=20). Experimental groups were as follows: Control,
control group; model, diabetic control group; metformin, diabetic
group with metformin treatment (70 mg/kg); and captopril, diabetic
group with captopril treatment (10 mg/kg). Metformin and captopril
were administered intragastrically (i.g.) once a day for 13 weeks.
Simultaneously, the control and model groups were administered 0.5%
sodium carboxymethyl cellulose (i.g.; Sanpu Chemical Reagent Co.,
Ltd., Shanghai, China) as procedural control. FBG levels were
determined during treatment at 0, 3, 6, 9 and 13 weeks using a
glucometer (Eukare, Eumed Biotechnology Co., Ltd. Taiwan). In the
present study, captopril, which is an angiotensin converting enzyme
(ACE) inhibitor, was used as a positive control as it has been
demonstrated to prevent the progression of chronic kidney disease
(18).
Assessment of biochemical
parameters
Serum samples were collected to determine HDL-c,
LDL-c, TC, TG, SCr and BUN levels. Measurements were performed
according to the manufacturer's protocol for each kit. In brief,
after 13 weeks of administration the rats were anesthetized by
chloral hydrate. Blood samples were taken from the abdomen artery
into non-hepatinised tubes and were allowed to clot for 2 h at room
temperature, and were then centrifuged at 1,100xg for 15 min.
Assessment of urine parameters
The urinary creatinine and creatinine in plasma were
measured using an AU5800 automatic analyzer (Beckman Coulter, Inc.,
CA, USA). Creatinine clearance (CCr) and 24-h urinary albumin
excretion rate (UAER) were calculated according to the following
formulae: UAER=urinary albumin (µg/ml) × 24-h urine volume (ml);
and CCr=urinary creatinine (UCr) (mg/ml) × urine volume
(ml/kg)/creatinine in plasma (mg/ml) (19).
Determination of SOD, MDA and GSH-Px
levels
One small section (200 mg) of right kidney was
harvested from the rats and precisely weighed. Subsequently, saline
was added according to the tissue weight: Saline volume=1:9 (w/v).
Following homogenization at 4°C by a DY89-I electric homogenate
(Ningbo Scientz Biotechnology Co., Ltd., Ningbo, China), the
homogenates were centrifuged at 1,100xg for 15 min at room
temperature. SOD activity, MDA content and GSH-Px levels were
measured using commercially available kits, according to
manufacturer's protocol.
Histopathology and electron microscopy
examination
Kidney samples were fixed in 10% formalin,
paraffin-embedded, cut into 5-micron sections and stained with
hematoxylin and eosin (Sanpu Chemical Reagent Co., Ltd.). Slides
were examined under an Eclipse 80i light microscope (magnification,
×400; Nikon, Tokyo, Japan) by a pathologist who was blind to the
experimental profiles. For electron microscopy, kidney tissues were
cut into small cubes (2 mm/side), fixed in 4% glutaraldehyde and
examined by independent pathologists with a JEM-1200EX transmission
electron microscope (Japan Electronic Co., Ltd.) who were blinded
to the protocol of the present study.
Immunohistochemical analysis
Expression levels of TGF-β1 and CTGF in the kidney
sections were analyzed via immunochemical staining. Polyclonal
anti-rabbit TGF-β1 antibody (1:200; bs-7443R) and monoclonal
anti-rabbit CTGF antibody (1:500; bs-0743R) were purchased from
Boaosen (Wuhan, China). Brown/yellow granular deposits in the cells
or matrix were interpreted as positive. Semi-quantitative
evaluations of the images were carried out using Image Pro Plus 6.0
(Media Cybernetics, Inc., Rockville, MD, USA).
Statistical analysis
Data are presented as the mean ± standard error of
the mean. Statistical significance was determined by one-way
analysis of variance, followed by Dunnett's test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Metformin decreases FBG levels in T2DN
rats
Following STZ injection, the rats in the model group
exhibited the typical symptoms of diabetes, with FBG levels
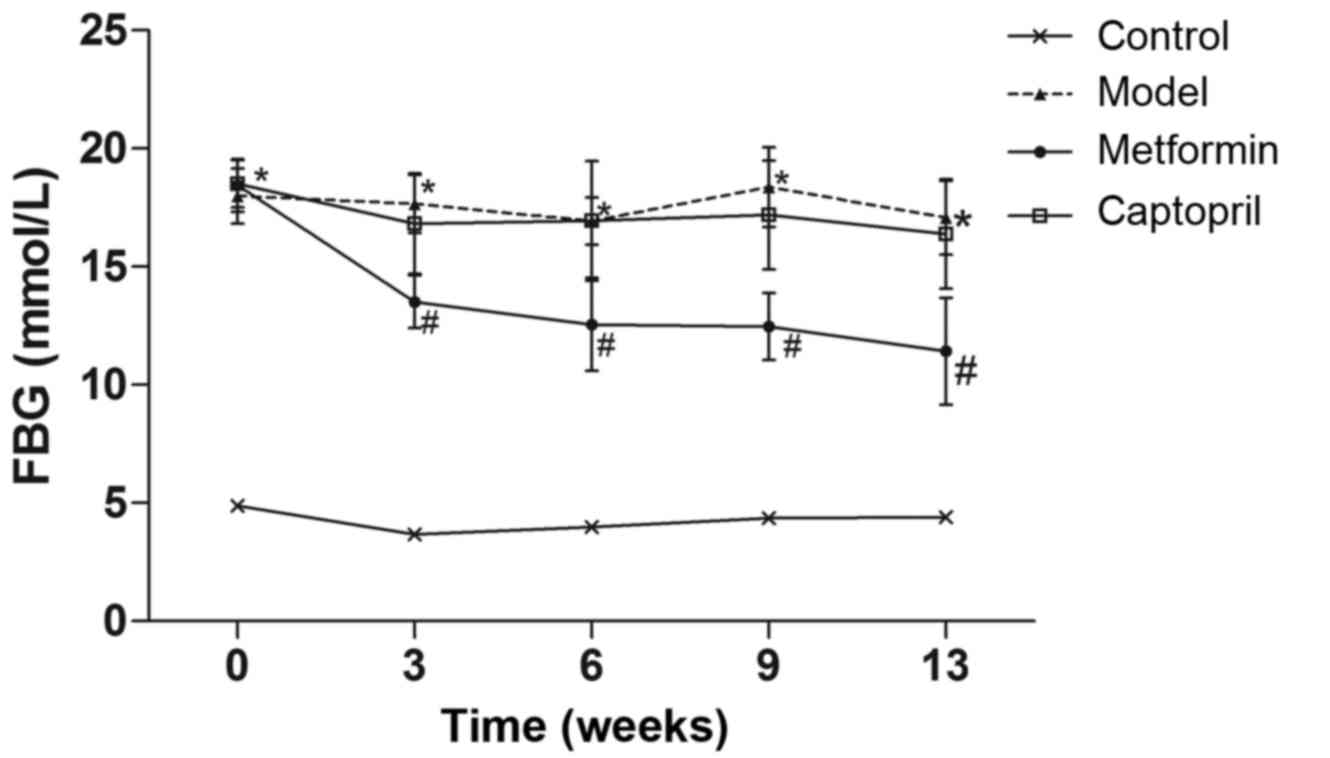
>11.1 mmol/l. As shown in Fig. 1,
the FBG levels in the model group significantly increased as the
experimental period increased. From the third week onwards, the
metformin group exhibited significantly decreased FBG levels
(P<0.05), whereas the captopril group exhibited no significant
differences in FBG. These results suggest that metformin decreases
FBG in T2DN rats.
Metformin protects the kidney function
in T2DN rats
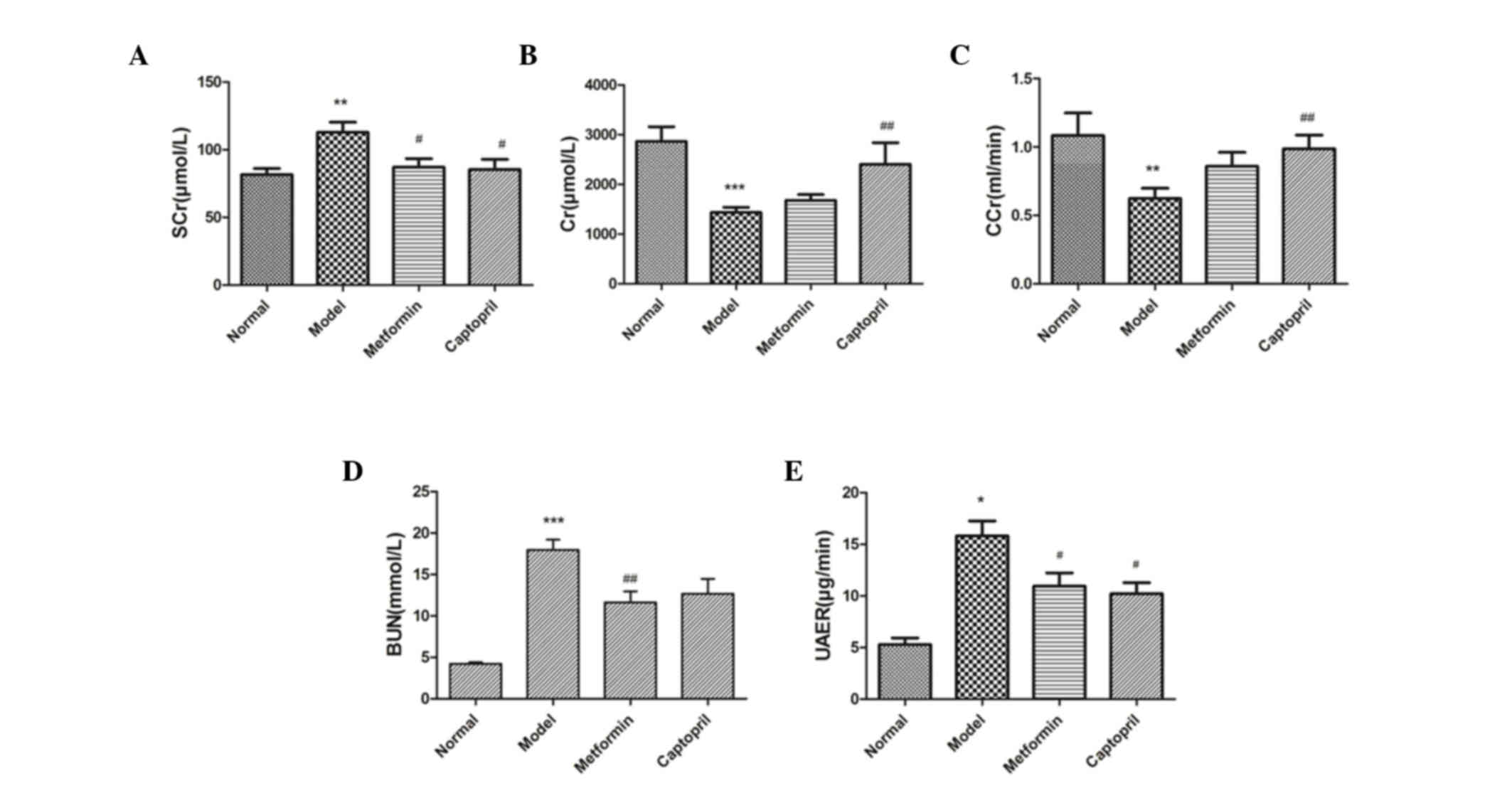
Following the induction of hyperglycemia via STZ,
significant increases in SCr (P<0.01), BUN (P<0.001) and UAER
levels were detected, accompanied by significant decreases in UCr
(P<0.001) and CCr (P<0.01), which indicated a significant
alternation in the kidney function of model rats, as compared with
the control rats (Figs. 2A-E).
Metformin treatment significantly reduced SCr (P<0.05) and BUN
(P<0.01) and UAER (P<0.05) levels in diabetic rats, as
compared with the model group. Metformin did not induce any
significant alterations in UCr and CCr levels; whereas UCr and CCr
levels were significantly increased following captopril treatment,
as compared with the model group (P<0.01). These results suggest
that metformin protects rental function in T2DN rats.
Metformin decreases blood lipids in
T2DN rats
Diabetic dyslipidemia was successfully established
in rats, as indicated by increased LDL-c (P<0.01), TG and TC
(both P<0.05) levels, and decreased HDL-c (P<0.01) levels.
Metformin treatment significantly counteracted the above mentioned
alterations in diabetic rats; serum LDL-c, TG and TC were reduced
(P<0.05) and HDL-c was increased (P<0.01). Captopril had no
significant effect on hyperlipidemia (Table I). These results suggest that
metformin decreases blood lipids in T2DN rats.
 | Table I.Effects of metformin on blood lipids
in rats with type 2 diabetes nephropathy. |
Table I.
Effects of metformin on blood lipids
in rats with type 2 diabetes nephropathy.
| Group | LDL-c (mmol/l) | HDL-c (mmol/l) | TG (mmol/l) | TC (mmol/l) |
|---|
| Control | 0.54±0.07 | 0.65±0.07 | 0.27±0.04 | 1.60±0.10 |
| Model |
1.02±0.09a |
0.42±0.04a |
0.42±0.04b |
2.12±0.15b |
| Metformin |
0.62±011c |
0.58±0.05d |
0.27±0.03c |
1.66±0.13c |
| Captopril | 0.80±0.10 | 0.55±0.05 | 0.39±0.07 | 1.68±0.23 |
Metformin decreases oxidative stress
in T2DN rats
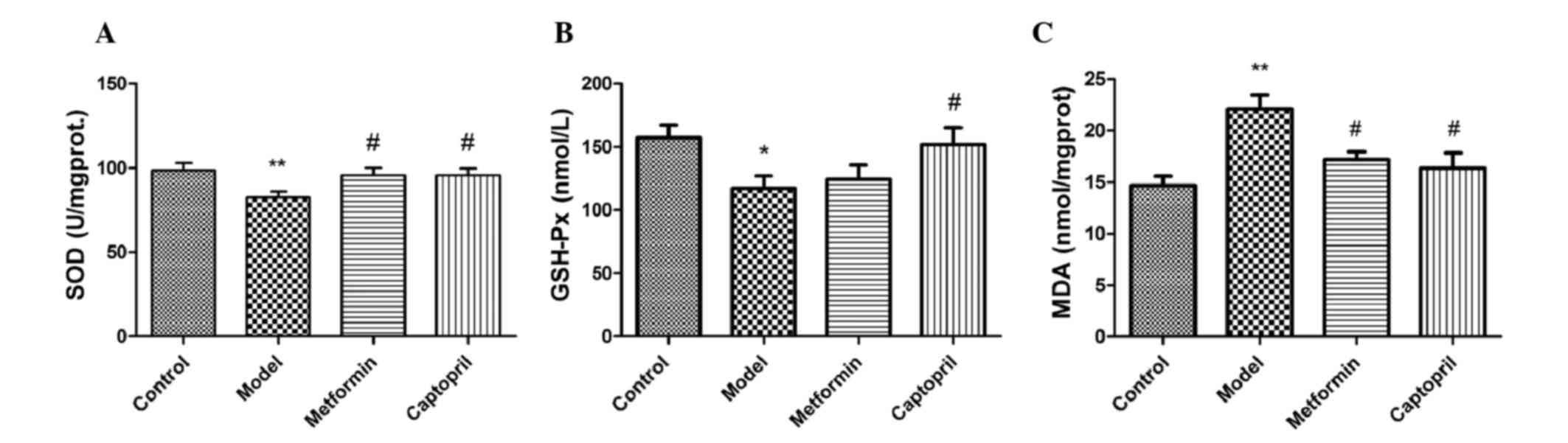
Diabetic rats exhibited significantly decreased
activities of SOD (P<0.01) and GSH-Px (P<0.05) (Figs. 3A and B), which was accompanied by a
significant increase in MDA levels (P<0.01) (Fig. 3C) in kidney tissue, as compared with
the control rats. Metformin treatment significantly increased the
activity of SOD (P<0.05) and decreased the level of MDA in
diabetic rats, as compared with the model group. However, the
activity of GSH-Px was only increased by captopril administration
(P<0.05), as compared with the model group. These results
suggest that metformin inhibits oxidative stress in T2DN rats.
Metformin protects histopathologcial
changes of kidney in T2DN rats
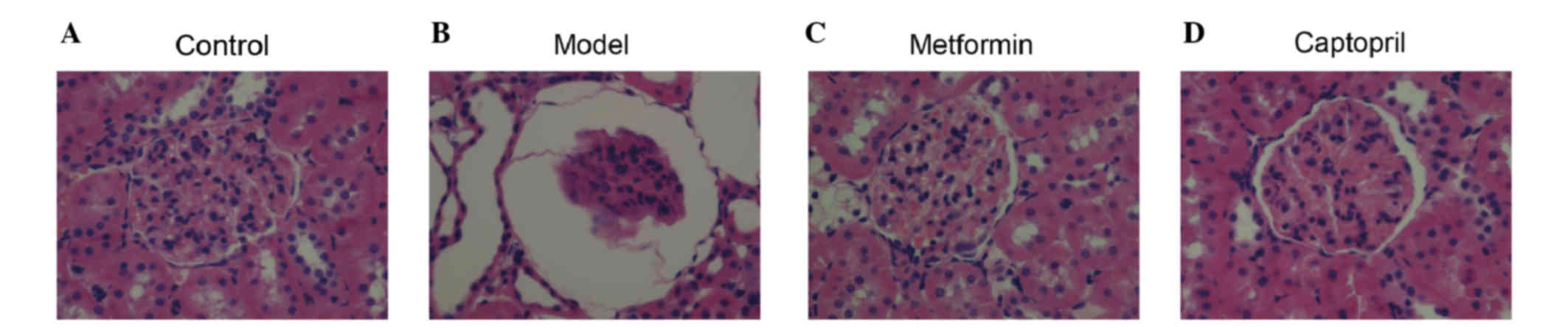
Fig. 4 shows the
morphology of the glomerulus, as detected by hematoxylin-eosin
staining. As compared with the control group (Fig. 4A), model rats exhibited reduced
glomerular tuft, increased Bowman's spaces, vacuolar degeneration,
and dilated renal capsule and kidney tubules (Fig. 4B). Metformin and captopril markedly
improved the renal lesions in diabetic rats (Figs. 4C and D, respectively).
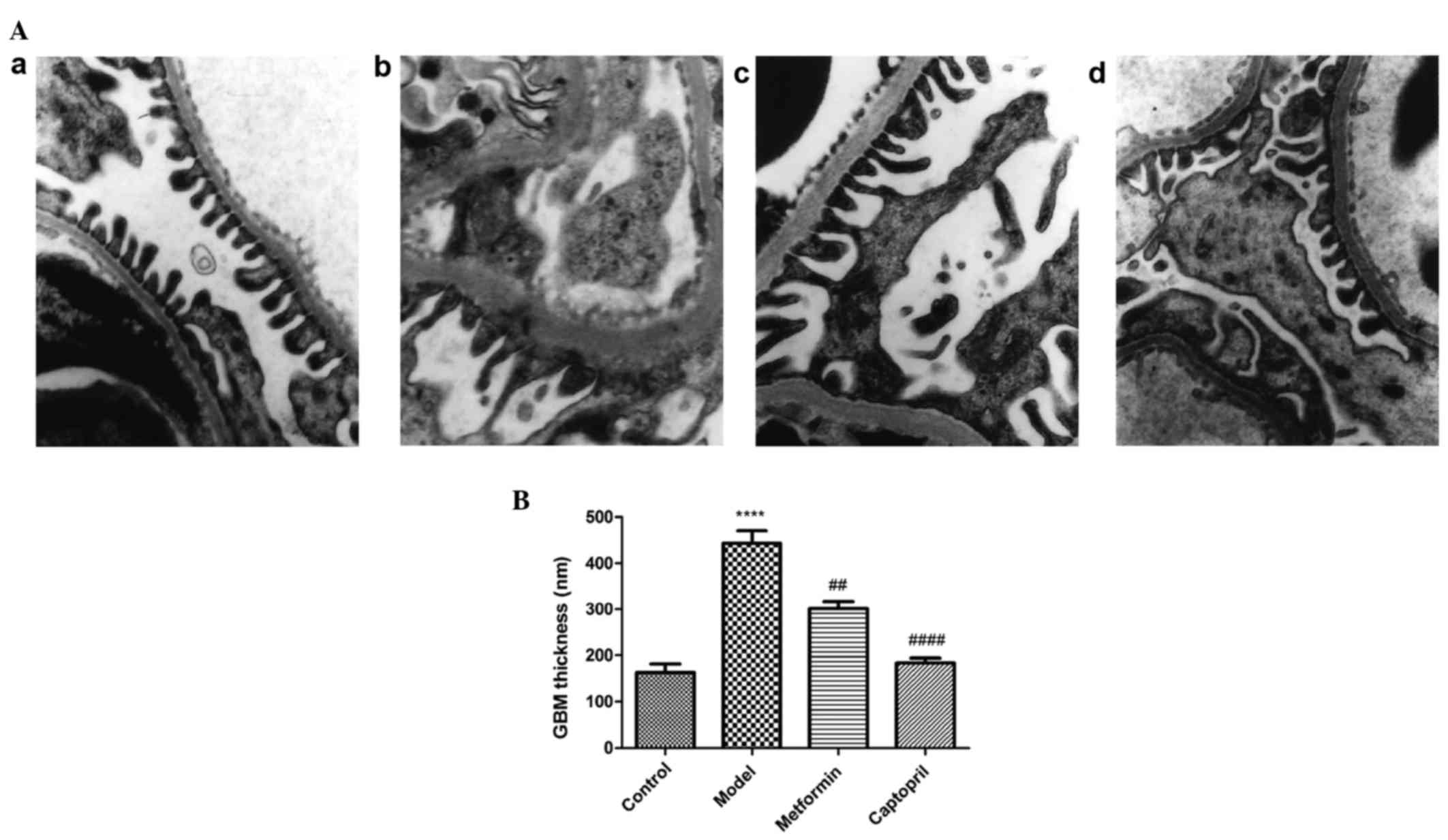
Representative images of the kidney cortices
acquired by transmission electron microscope are presented in
Fig. 5. Kidney cortices samples from
the control group exhibited normal structure of three layer of the
filtration barrier, with normal glomerular basement membrane (GBM)
thickness and equally distributed podocyte foot processes that form
foot-like structures (Fig. 5A-a). In
the model rats, the podocytes processes merged together in large
areas, and the filtration barrier was blurry and no longer clearly
distinguishable (Fig. 5A-b).
Furthermore, significant segmental thickening of the GBM was
detected (P<0.0001), as compared with the control group
(Fig. 5B). Treatment with metformin
and captopril ameliorated these ultrastructural changes in the
kidneys of diabetic rats (Figs. 5A-c
and 5A-d). Notably, GBM thickness
was significantly decreased in the metformin- and captopril-treated
groups, as compared with the model group (P<0.01 and
P<0.0001, respectively). These results suggest that metformin
protects against glomerular damage in the kidneys of T2DN rats.
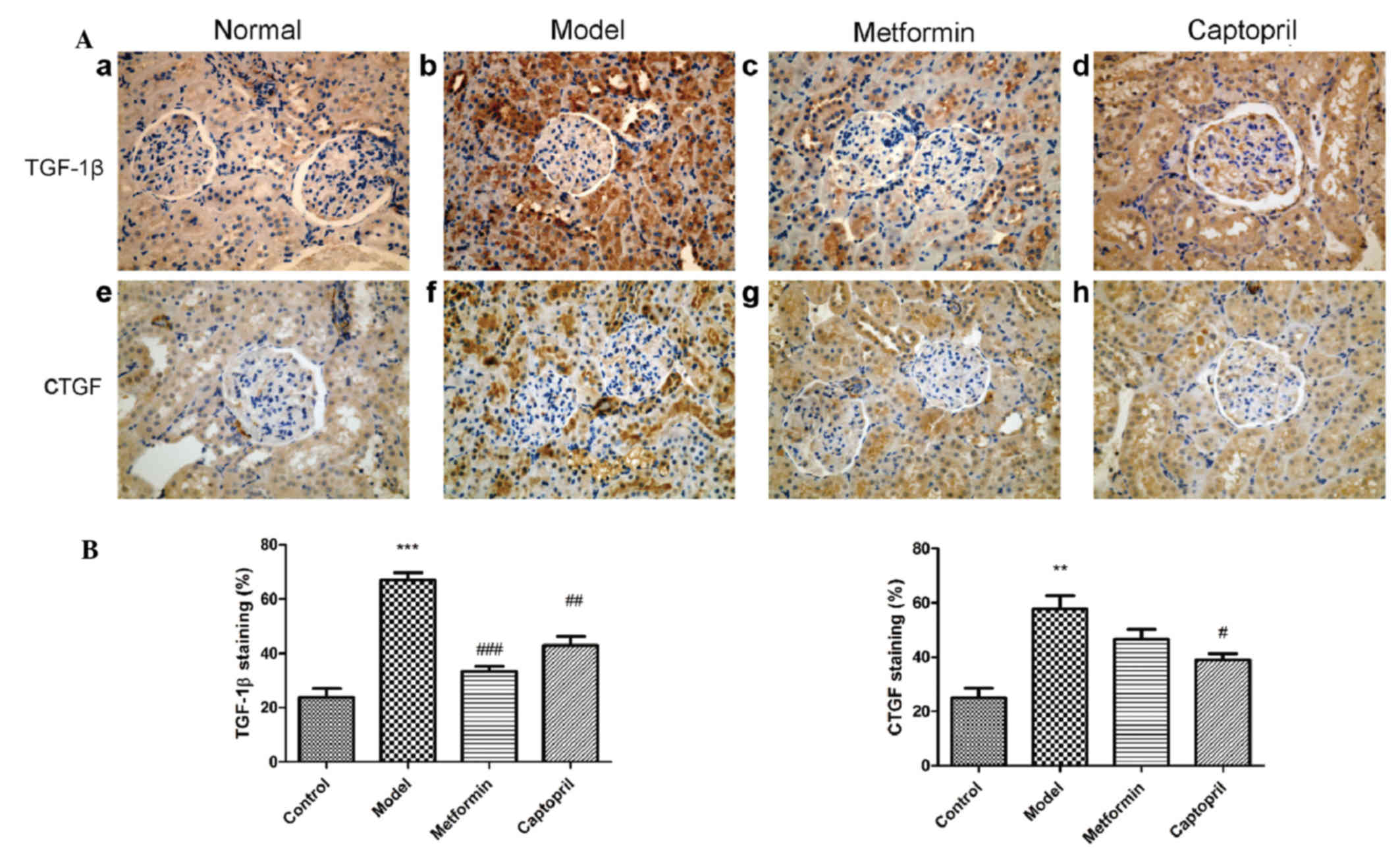
Metformin decreases TGF-β1 and CTGF
expression levels in T2DN rats
The effect of metformin treatment on the expression
levels of TGF-β1 and CTGF were examined by immunohistochemistry. As
shown in Fig. 6, positive staining
of TGF-β1 and CTGF in the proximal tubule and glomerular mesangial
area were significantly enhanced in the model group, as compared
with the control group. As compared with the model group, TGF-β1
expression levels were significantly reduced by metformin and
captorpil treatment (P<0.001 and P<0.01, respectively). Only
captopril administration was able to significantly reduce the
expression levels of CTGF, as compared with the model group
(P<0.05).
Semi-quantitative analysis of the positively stained
areas demonstrated that TGF-β1 and CTGF expression levels in the DN
rats were increased, whereas metformin treatment was able to
significantly reduce the expression of TGF-β1 (P<0.001; Fig. 6B). These results suggest that
metformin decreases TGF-β1 and CTGF expression levels in the
kidneys of T2DN rats.
Discussion
In the present study, the renoprotective effects of
metformin against T2DN were demonstrated in a high-fat diet,
low-dose STZ-induced rat model of T2DN. These results demonstrated
that merformin can markedly improve the renal lesions (Fig. 4) and ameliorate the GBM thickness of
the kidney (Fig. 5) in diabetic
rats. At the same time, merformin can decrease the FBG levels,
reduce TG and TC levels, decrease the TGF-β1 expression and
increase SOD activity. Therefore, treatment with metformin
indicated the importance of glycemic control, blood lipid control,
anti-oxidative and anti-inflammatory effects in the treatment of
T2DN.
STZ is widely used in studies investigating DM, as
it specifically targets β-cells and reduces blood insulin levels,
leading to hyperglycemia and mimicking DM pathology (20–22).
Dosages of STZ required in DM models remain controversial. In a
pervious mouse model, high-dose STZ induced direct nephrotoxicity,
making it unable to distinguish between the direct toxic effect of
STZ and the lesions that resulted from STZ-induced hyperglycemia
(20,23,24). In
the present study, insulin resistance was induced in a rat model
via a high-fat diet (25,26), followed by a single low dose of STZ
(30 mg/kg) to induce hyperglycemia for 2 weeks. Elevated glucose
levels after 13 weeks successfully induced renal lesions that were
similarly present in human patients with DN, hyperglycemia,
hyperlipidemia, oxidative stress and renal damage (20). According to previous diagnostic
criteria of DN outlined by Mogensen et al (27), the present study evaluated rats in DN
stages 3–4.
In the present STZ-induced DN model, kidney damage
was assessed via kidney function parameters, including elevated
SCr, UCr, BUN and UAER, and declined CCr levels. Presence of
albumin in the urine is a primary indicator of kidney damage in the
early onset of DN, and the UAER is typically measured in the clinic
to assess renal lesions in patients with DN (28,29).
Creatinine is a breakdown product of creatine phosphate in muscle
and its clearance rate from blood to urine (CCr) correlates with
glomerular filtration rate (30);
therefore, CCr can be used as an indicator for kidney function.
Kidney damage, as indicated by reduced UAER, was detected 13 weeks
after the initiation of STZ-induced hyperglycemia. In addition,
SCr, UCr and BUN kidney function parameters were significantly
increased in the model group, as compared with the control group.
Treatment with metformin alone ameliorated the majority of these
kidney dysfunctions, indicating the protective effects of metformin
administration in rats with T2DN. In the model group, morphological
and ultrastructural analysis indicated severe damage to the kidney
tissue, including reduced glomeruli, dilation of the renal capsule
and kidney tubules, and GBM thickening. Treatment with metformin
successfully counteracted these morphological alterations.
Hyperglycemia is considered to be the dominant
pathological characteristic of DM, as it causes the majority of the
symptoms associated with DM. Chronic hyperglycemia results in the
accumulation of advanced glycation end products (AGEs) in the body,
which further increase the risk for vascular complications in
patients with DM (31). A previous
study demonstrated that AGEs are always present in diabetic
individuals with kidney dysfunction, leading to the overproduction
of ROS (32). ROS produced by
hyperglycemia are capable of damaging cell membranes and
inactivating endogenous antioxidants, lipid and carbohydrate
(33,34), and are considered to be a predominant
cause of diabetic-related complications (35,36).
Endogenous antioxidant molecules, such as SOD and GSH-Px,
counteract ROS-mediated renal injury (37); however, they are severely decreased
in patients with T2DN, indicating oxidative stress (37,38). As
hyperglycemia has a dominant role at the beginning of the
ROS-mediated pathway, strict glucose modulation remains the major
therapeutic strategy, as this aids the amelioration of oxidative
stress (39–41). In the present study, elevated FBG
levels were significantly reduced by the well-characterized
hypoglycemic agent, metformin; whereas the ACE inhibitor,
captopril, induced no effect on FBG. These results indicated that
glycemic control is important for the metformin-mediated
renoprotective effect. Furthermore, the levels of SOD, GSH-Px and
MDA in kidney homogenates were determined. In the model group,
decreased levels of the SOD and GSH-Px antioxidants were
accompanied by an increase in MDA levels. Treatment with metformin
or captopril increased SOD levels and reduced MDA levels. These
results suggested that treatment with metformin or captopril exerts
a renoprotective effect via increasing SOD and reducing MDA.
Hyperlipidemia is a common symptom of DM (42–45).
Persistent filtration of lipids and lipid proteins contributes to
chronic and progressive renal injury (46), albuminuria and glomerulosclerosis
(46,47). Hyperlipidemia is considered as a risk
factor for DN as it may exacerbate glomerular injury through the
activation of various signaling pathways (48). The lipid profile of patients with DN
is as follows: High LDL-c, TC and TG, and low HDL-c (45,49).
This lipid profile has been termed ‘diabetic dyslipidemia’, and is
predominantly observed in patients with T2DM (49). Notably, it has been demonstrated that
these lipid abnormalities are associated with worsening kidney
function and urinary albumin excretion (49). In the present study, the model group
exhibited increased TC, TG and LDL-c, and decreased HDL-c.
Treatment with metformin, which is a hypoglycemic drug,
significantly attenuated these pathological alternations in blood
lipid concentrations; whereas captopril exhibited no significant
effect. This result implied that metformin may help ease DN
symptoms by modulating lipid metabolism and dyslipidemia.
There is a growing body of evidence suggesting the
involvement of inflammatory cytokines, including TGF-β1, CTGF and
IL-6, in the pathogenesis of DN (50,51).
Oxidative stress activates TGF-β1 and IL-6 by modulating multiple
pathways, and these cytokines contribute to glomerular mesangial
expansion and tubulointerstitial fibrosis (39,40,50).
CTGF expression is associated with oxidative stress and has been
established as the downstream effector of TGF-β1 (52). Together, CTGF and TGF-β1 contribute
to tissue fibrosis (9,10), promoting cell proliferation and ECM
synthesis (11). Furthermore, it has
previously been demonstrated that serum IL-6 levels were
significantly elevated in patients with T2DN, as compared with
hyperglycemic patients without nephropathy (53,54).
Elevation of IL-6 inflammatory cytokine levels in patients with DM
and nephropathy indicates that T2DN is a low-inflammatory disease
(51,55). Therefore, the use of agents with
anti-inflammatory effects may serve as an attractive strategy for
the treatment of renal dysfunction in patients with T2DM (40). In the present study, uncontrolled
nephropathy was detected in the model group, which was
characterized by significantly elevated expression levels of TGF-β1
and CTGF in the kidney. The results of the present study
demonstrated that metformin was capable of counteracting the
inflammation effect of DN and prevent chronic DN pathogenesis.
Therefore, the anti-inflammatory effect induced by metformin is
another important mechanism by which it protected rats from the
development of chronic T2DN in the present study.
In conclusion, the present study demonstrated the
renoprotective effects of metformin against T2DN in a high-fat
diet, low-dose STZ-induced rat model of T2DN. The successful
induction of T2DN in the rats was demonstrated by severe renal
dysfunction, hyperglycemia, dyslipidemia, a reduction in
antioxidants and increased expression levels of inflammatory
cytokines. Metformin treatment significantly attenuated the
pathological characteristics of T2DN, by reducing blood glucose,
protecting renal functions and retaining normal morphology. The
mechanism of this effect may be associated with glycemic control,
lipid metabolism, and anti-oxidative and anti-inflammatory
functions; however, further investigation is required to fully
elucidate the underlying mechanism.
References
|
1
|
Kashihara N, Haruna Y, Kondeti VK and
Kanwar YS: Oxidative stress in diabetic nephropathy. Curr Med Chem.
17:4256–4269. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yokoyama H, Araki S, Kawai K, Hirao K,
Oishi M, Sugimoto K, Sone H, Maegawa H and Kashiwagi A; Japan
Diabetes Clinical Data Management Study Group: Pioglitazone
treatment and cardiovascular event and death in subjects with type
2 diabetes without established cardiovascular disease (JDDM 36).
Diabetes Res Clin Pract. 109:485–492. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ritz E: Diabetic nephropathy. Saudi J
Kidney Dis Transpl. 17:481–490. 2006.PubMed/NCBI
|
|
4
|
Zou J, Yu X, Qu S, Li X, Jin Y and Sui D:
Protective effect of total flavonoids extracted from the leaves of
Murraya paniculata (L.) Jack on diabetic nephropathy in rats. Food
Chem Toxicol. 64:231–237. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gohda T, Mima A, Moon JY and Kanasaki K:
Combat diabetic nephropathy: From pathogenesis to treatment. J
Diabetes Res. 2014:2071402014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pan HZ, Zhang L, Guo MY, Sui H, Li H, Wu
WH, Qu NQ, Liang MH and Chang D: The oxidative stress status in
diabetes mellitus and diabetic nephropathy. Acta Diabetol. 47 Suppl
1:S71–S76. 2010. View Article : Google Scholar
|
|
7
|
Swaminathan S and Shah SV: Novel
approaches targeted toward oxidative stress for the treatment of
chronic kidney disease. Curr Opin Nephrol Hypertens. 17:143–148.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tabak O, Gelisgen R, Erman H, Erdenen F,
Muderrisoglu C, Aral H and Uzun H: Oxidative lipid, protein and DNA
damage as oxidative stress markers in vascular complications of
diabetes mellitus. Clin Invest Med. 34:E163–E171. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ho C, Lee PH, Hsu YC, Wang FS, Huang YT
and Lin CL: Sustained Wnt/β-catenin signaling rescues high glucose
induction of transforming growth factor-β1-mediated renal fibrosis.
Am J Med Sci. 344:374–382. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zorena K, Malinowska E, Raczyńska D,
Myśliwiec M and Raczyńska K: Serum concentrations of transforming
growth factor-Beta 1 in predicting the occurrence of diabetic
retinopathy in juvenile patients with type 1 diabetes mellitus. J
Diabetes Res. 2013:6149082013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen MM, Lam A, Abraham JA, Schreiner GF
and Joly AH: CTGF expression is induced by TGF-beta in cardiac
fibroblasts and cardiac myocytes: A potential role in heart
fibrosis. J Mol Cell Cardiol. 32:1805–1819. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li X, Cui X, Sun X, Li X, Zhu Q and Li W:
Mangiferin prevents diabetic nephropathy progression in
streptozotocin-induced diabetic rats. Phytother Res. 24:893–899.
2010.PubMed/NCBI
|
|
13
|
Nasri H and Rafieian-Kopaei M: Metformin:
Current knowledge. J Res Med Sci. 19:658–664. 2014.PubMed/NCBI
|
|
14
|
Kirpichnikov D, McFarlane SI and Sowers
JR: Metformin: An update. Ann Intern Med. 137:25–33. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Grossmann ME, Yang DQ, Guo Z, Potter DA
and Cleary MP: Metformin Treatment for the Prevention and/or
Treatment of Breast/Mammary Tumorigenesis. Curr Pharmacol Rep.
1:312–323. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rafieian-Kopaei M and Nasri H: Ginger and
diabetic nephropathy. J Renal Inj Prev. 2:9–10. 2013.PubMed/NCBI
|
|
17
|
Baradaran A: Lipoprotein(a), type 2
diabetes and nephropathy; the mystery continues. J Nephropathol.
1:126–129. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim CS, Sohn EJ, Kim YS, Jung DH, Jang DS,
Lee YM, Kim DH and Kim JS: Effects of KIOM-79 on hyperglycemia and
diabetic nephropathy in type 2 diabetic Goto-Kakizaki rats. J
Ethnopharmacol. 111:240–247. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kong LL, Wu H, Cui WP, Zhou WH, Luo P, Sun
J, Yuan H and Miao LN: Advances in murine models of diabetic
nephropathy. J Diabetes Res. 2013:7975482013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dupuis F, Atkinson J, Limiñana P and
Chillon JM: Captopril improves cerebrovascular structure and
function in old hypertensive rats. Br J Pharmacol. 144:349–356.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Szkudelski T: The mechanism of alloxan and
streptozotocin action in B cells of the rat pancreas. Physiol Res.
50:537–546. 2001.PubMed/NCBI
|
|
22
|
Lenzen S: The mechanisms of alloxan- and
streptozotocin-induced diabetes. Diabetologia. 51:216–226. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hall-Craggs M, Brenner DE, Vigorito RD and
Sutherland JC: Acute renal failure and renal tubular squamous
metaplasia following treatment with streptozotocin. Hum Pathol.
13:597–601. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tay YC, Wang Y, Kairaitis L, Rangan GK,
Zhang C and Harris DC: Can murine diabetic nephropathy be separated
from superimposed acute renal failure? Kidney Int. 68:391–398.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jiang X, Ma H, Wang Y and Liu Y: Early
life factors and type 2 diabetes mellitus. J Diabetes Res.
2013:4850822013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lee KM, Yang SJ, Kim YD, Choi YD, Nam JH,
Choi CS, Choi HS and Park CS: Disruption of the cereblon gene
enhances hepatic AMPK activity and prevents high-fat diet-induced
obesity and insulin resistance in mice. Diabetes. 62:1855–1864.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mogensen CE, Christensen CK and Vittinghus
E: The stages in diabetic renal disease. With emphasis on the stage
of incipient diabetic nephropathy. Diabetes. 32 Suppl 2:S64–S78.
1983. View Article : Google Scholar
|
|
28
|
Viberti G and Wheeldon NM;
MicroAlbuminuria Reduction With VALsartan (MARVAL) Study
Investigators, : Microalbuminuria reduction with valsartan in
patients with type 2 diabetes mellitus: A blood
pressure-independent effect. Circulation. 106:672–678. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang XL, Lu JM, Pan CY and Tian H: A study
comparing the prevalence of urinary albumin excretion and
microalbuminuria in pre-diabetes subjects. Zhonghua Nei Ke Za Zhi.
43:170–173. 2004.(In Chinese). PubMed/NCBI
|
|
30
|
Stirban A, Gawlowski T and Roden M:
Vascular effects of advanced glycation endproducts: Clinical
effects and molecular mechanisms. Mol Metab. 3:94–108. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sakai H, Jinde K, Suzuki D, Yagame M and
Nomoto Y: Localization of glycated proteins in the glomeruli of
patients with diabetic nephropathy. Nephrol Dial Transplant. 11
Suppl 5:S66–S71. 1996. View Article : Google Scholar
|
|
32
|
Rösen P, Nawroth PP, King G, Möller W,
Tritschler HJ and Packer L: The role of oxidative stress in the
onset and progression of diabetes and its complications: A summary
of a Congress Series sponsored by UNESCO-MCBN, the American
diabetes association and the german diabetes society. Diabetes
Metab Res Rev. 17:189–212. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
33
|
Iwasaki Y, Sawada T, Kijima H, Kosuge T,
Katoh M, Rokkaku K, Kita J, Shimoda M and Kubota K: Estimated
glomerular filtration rate is superior to measured creatinine
clearance for predicting postoperative renal dysfunction in
patients undergoing pancreatoduodenectomy. Pancreas. 39:20–25.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yan LJ: Analysis of oxidative modification
of proteins. Curr Protoc Protein Sci Chapter. 14:Unit14.42009.
|
|
35
|
Booth AA, Khalifah RG, Todd P and Hudson
BG: In vitro kinetic studies of formation of antigenic advanced
glycation end products (AGEs). Novel inhibition of post-Amadori
glycation pathways. J Biol Chem. 272:5430–5437. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Miyoshi H, Taguchi T, Sugiura M, Takeuchi
M, Yanagisawa K, Watanabe Y, Miwa I, Makita Z and Koike T:
Aminoguanidine pyridoxal adduct is superior to aminoguanidine for
preventing diabetic nephropathy in mice. Horm Metab Res.
34:371–377. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wagener FA, Dekker D, Berden JH,
Scharstuhl A and van der Vlag J: The role of reactive oxygen
species in apoptosis of the diabetic kidney. Apoptosis.
14:1451–1458. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Singh DK, Winocour P and Farrington K:
Oxidative stress in early diabetic nephropathy: Fueling the fire.
Nat Rev Endocrinol. 7:176–184. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Krishan P and Chakkarwar VA: Diabetic
nephropathy: Aggressive involvement of oxidative stress. J Pharm
Educ Res. 2:352011.
|
|
40
|
Mima A: Inflammation and oxidative stress
in diabetic nephropathy: New insights on its inhibition as new
therapeutic targets. J Diabetes Res. 2013:2485632013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Shao N, Kuang HY, Wang N, Gao XY, Hao M,
Zou W and Yin HQ: Relationship between oxidant/antioxidant markers
and severity of microalbuminuria in the early stage of Nephropathy
in type 2 diabetic Patients. J Diabetes Res. 2013:2324042013.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Grover HS and Luthra S: Molecular
mechanisms involved in the bidirectional relationship between
diabetes mellitus and periodontal disease. J Indian Soc
Periodontol. 17:292–301. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Iacopino AM: Periodontitis and diabetes
interrelationships: Role of inflammation. Ann Periodontol.
6:125–137. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Howard BV: Lipoprotein metabolism in
diabetes mellitus. J Lipid Res. 28:613–628. 1987.PubMed/NCBI
|
|
45
|
Ma Y, Wang Y, Huang Q, Ren Q, Chen S,
Zhang A, Zhao L, Zhen Q and Peng Y: Impaired β cell function in
Chinese newly diagnosed type 2 diabetes mellitus with
hyperlipidemia. J Diabetes Res. 2014:4930392014. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Moorhead JF, Chan MK, El-Nahas M and
Varghese Z: Lipid nephrotoxicity in chronic progressive glomerular
and tubulo-interstitial disease. Lancet. 2:1309–1311. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Krolewski AS, Warram JH and Christlieb AR:
Hypercholesterolemia-a determinant of renal function loss and
deaths in IDDM patients with nephropathy. Kidney Int Suppl.
45:S125–S131. 1994.PubMed/NCBI
|
|
48
|
Ravid M, Neumann L and Lishner M: Plasma
lipids and the progression of nephropathy in diabetes mellitus type
II: Effect of ACE inhibitors. Kidney Int. 47:907–910. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Rosario RF and Prabhakar S: Lipids and
diabetic nephropathy. Curr Diab Rep. 6:455–462. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Lee HB, Yu MR, Yang Y, Jiang Z and Ha H:
Reactive oxygen species-regulated signaling pathways in diabetic
nephropathy. J Am Soc Nephrol. 14 8 Suppl 3:S241–S245. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Choudhary N and Ahlawat RS: Interleukin-6
and C-reactive protein in pathogenesis of diabetic nephropathy: New
evidence linking inflammation, glycemic control and
microalbuminuria. Iran J Kidney Dis. 2:72–79. 2008.PubMed/NCBI
|
|
52
|
Branchetti E, Poggio P, Sainger R, Shang
E, Grau JB, Jackson BM, Lai EK, Parmacek MS, Gorman RC, Gorman JH,
et al: Oxidative stress modulates vascular smooth muscle cell
phenotype via CTGF in thoracic aortic aneurysm. Cardiovasc Res.
100:316–324. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Vestra M Dalla, Mussap M, Gallina P,
Bruseghin M, Cernigoi AM, Saller A, Plebani M and Fioretto P:
Acute-phase markers of inflammation and glomerular structure in
patients with type 2 diabetes. J Am Soc Nephrol. 16 Suppl
1:S78–S82. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Sekizuka K, Tomino Y, Sei C, Kurusu A,
Tashiro K, Yamaguchi Y, Kodera S, Hishiki T, Shirato I and Koide H:
Detection of serum IL-6 in patients with diabetic nephropathy.
Nephron. 68:284–285. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Chen FQ, Wang J, Liu XB, Ma XY, Zhang XB,
Huang T, Ma DW and Wang QY: Levels of inflammatory cytokines in
type 2 diabetes patients with different urinary albumin excretion
rates and their correlation with clinical variables. J Diabetes
Res. 2013:1389692013. View Article : Google Scholar : PubMed/NCBI
|