Introduction
Endogenous fungal chorioretinitis in newborn infants
is a rare condition that may lead to vision loss (1). To the best of our knowledge, a
Candida infection disseminating from the eye to the hip
joint in infants has not been previously reported. Early diagnosis
and aggressive treatment are essential to avoid vision loss. Ocular
candidiasis is a serious complication of candidemia, but little
information has been published on the optimal duration of
treatment. Based mainly on expert opinion, the Infectious Diseases
Society of America guidelines propose 4–6 weeks of treatment for
endophthalmitis with the duration being determined by the
stabilization or resolution of eye lesions (2). The current case report describes a case
of successfully treated fungal chorioretinitis and hip
osteoarthritis with systemic candidiasis, in a full term infant
following treatment with antibiotics.
Case report
A 39-week-gestation female infant was delivered by
caesarean section at The First Hospital of Jilin University
(Changchun, China) in September 2014. At day 6 postpartum, the
patient became febrile, with a temperature of 39°C and experienced
vomiting. The patient was diagnosed with septicemia and neonatal
meningitis. Following intravenous administration of cefepime (30
mg/kg) twice a day for 11 days, a prominent conjunctival infection
developed in the left eye. Cultures for Candida albicans in
the blood and cerebrospinal fluid tested positive. Other tests
include blood tests [white blood cells 0.9×109/l
(neutrophils 0.216×109/l, lymphocytes
0.684×109/l), red blood cells 5.25×1012/l,
hemoglobin 189 g/l, platelet 279×109/l] and
cerebrospinal fluid tests [Cl 121 mmol/l, Glu 0.8 mmol/l, protein
1.0 g/l, Pandy's test (−), white blood cells 20×106/l
(macropolycytes 8×106/l, monocytes 12×106/l),
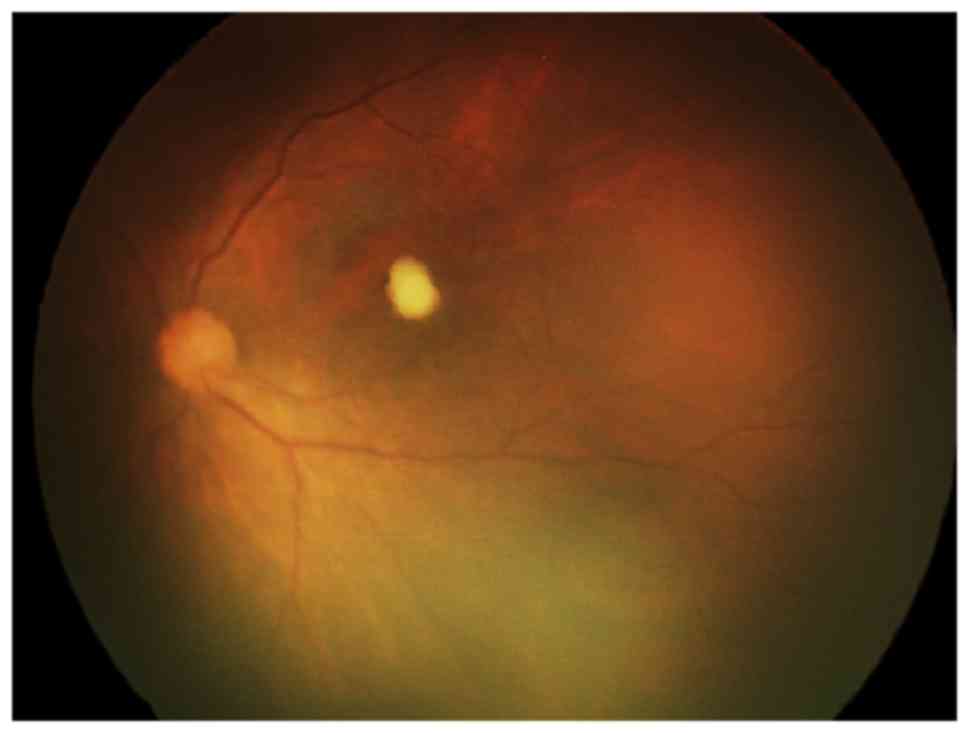
red blood cells 70×106/l]. Ophthalmic examination
indicated one yellow-white chorioretinal juxta foveal lesion in the
left eye, with neither vitreous haze nor cells (Fig. 1). Chest X-ray and tuberculin skin
test were normal. Intravenous fluconazole (6 mg/kg daily; Lunan
Pharmaceutical Group Co., Ltd., Linyi, China) administration was
begun instead of cefepime for the treatment of fungal infection.
The patient stopped vomiting and the temperature was 36.8°C
following the use of fluconazole for 20 days. Cultures for
Candida albicans in the blood and cerebrospinal fluid tested
negative. Subsequently, the patient was discharged.
However, 6 days after discharge, the patient was
referred to The First hospital of Jilin University with a 1-day
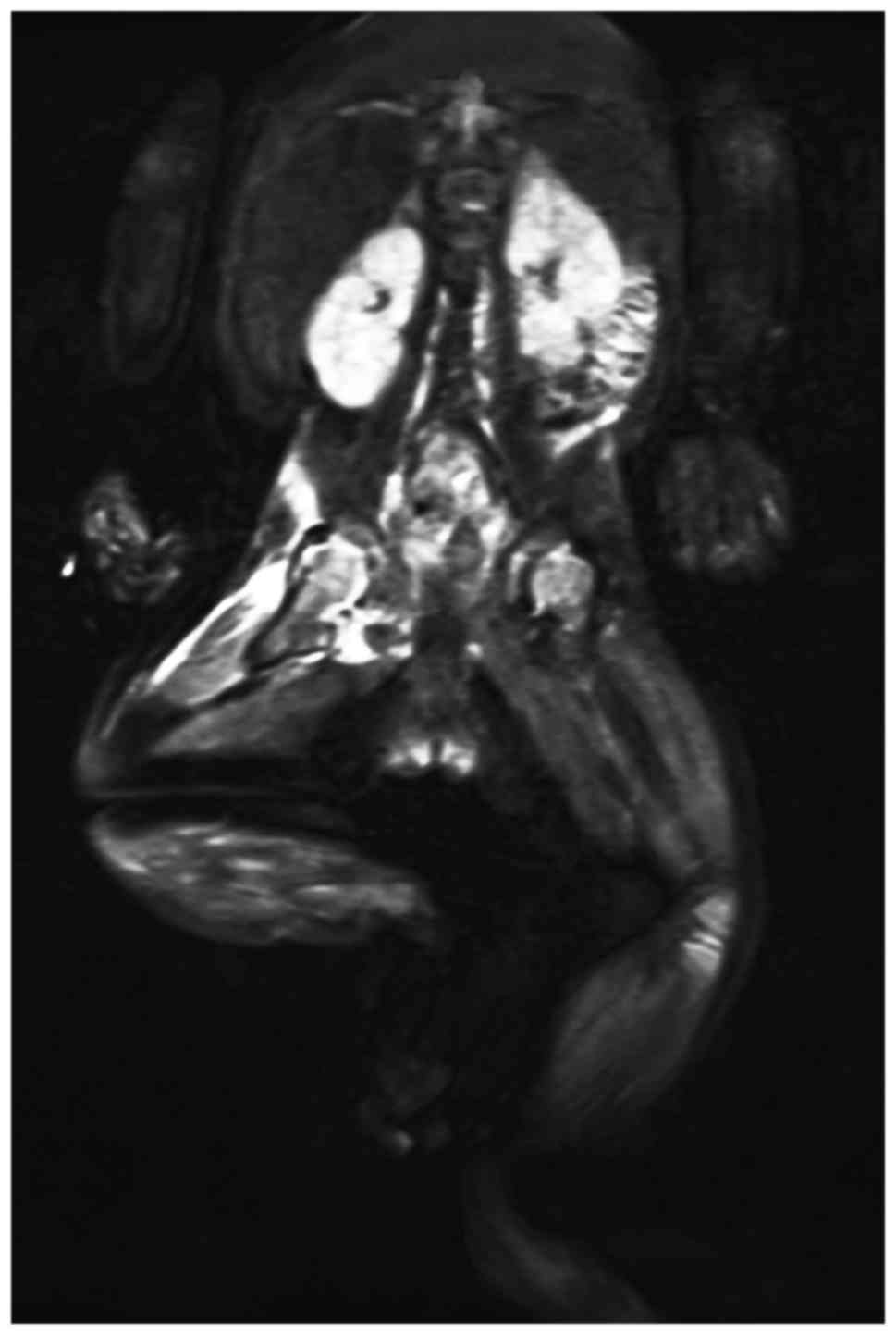
history of fever and limitation of motion in the right hip. A
diagnosis of hip osteoarthritis was established by magnetic
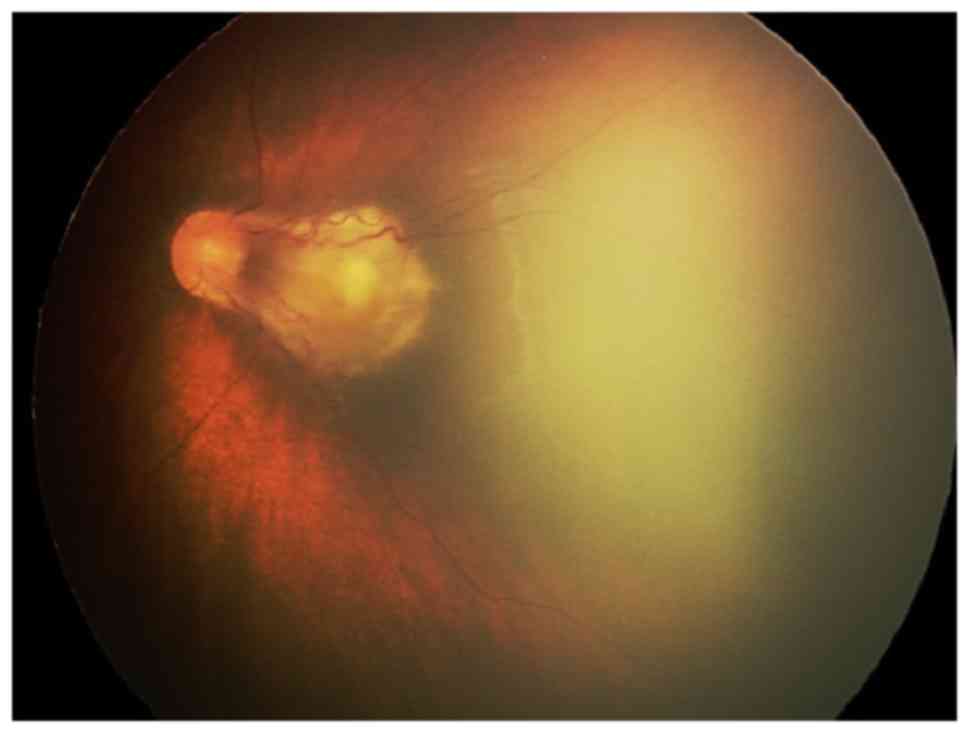
resonance imaging (Fig. 2). Fundus
examination indicated that the lesion had expanded and extended to
the inferior and superior temporal vascular arcades in the left eye
(Fig. 3). Following a further 4
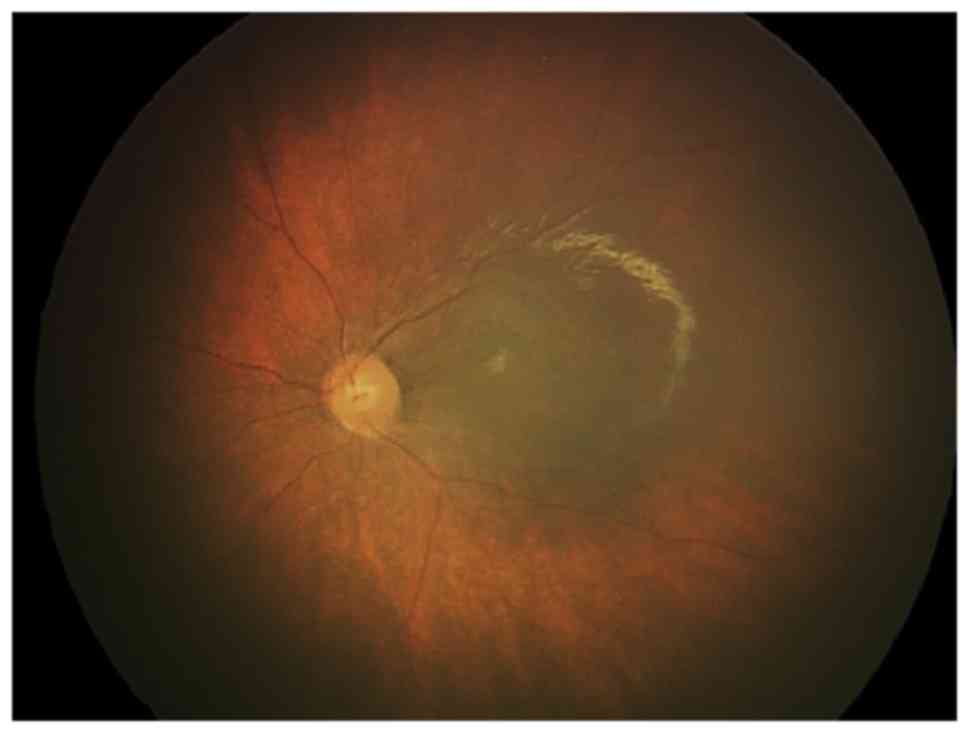
weeks of intravenous fluconazole administration (6 mg/kg daily), no
active chorioretinal lesions were observed in the fundus
examination (Fig. 4) and limitation
of motion in the right hip was completely resolved. The blood
culture for C. albicans was negative. Three months later,
the patient remained asymptomatic and fundus examination was
unremarkable.
Discussion
Fungal chorioretinitis is defined as the presence of
deep, focal, white chorioretinal lesions with no evidence of direct
vitreous involvement (3) and it is
rarely diagnosed in newborn infants due to high availability of
prophylactic antifungal therapy (1).
Those at risk of developing fungal chorioretinitis include
hospitalized patients with a history of a compromised immune
system, diabetes mellitus, intravenous drug use, chronic use of
indwelling catheters, use of broad spectrum intravenous antibiotics
or hyperalimentation (4,5). The risk factor for the patient in the
current study was treatment with broad spectrum antibiotics.
The most common causative species of candidemia
identified in fungal culture is C. albicans (41%), followed
by Candida parapsilosis (24%) and Candida glabrata
(13%). The most common organ of dissemination is the lung (58%),
followed by the liver (23%), kidney (16%), brain (12%), spleen
(8%), heart (8%) and eye (8%) (4).
The probability of fungus disseminating to a given organ seems be
correlated with the relative size and blood supply of that organ
(6). Of 38 heroin users treated for
systemic Candida infections, 10 had osteoarticular
involvement (vertebrae, costal cartilage, knees and sacroiliac)
(7). To the best of our knowledge,
this is the first report of Candida infection disseminating
from the eye to hip joint in an infant. Ophthalmologists should be
aware of this unusual complication when treating active
Candida chorioretinitis.
When treating patients with fungal chorioretinitis,
there is some debate over the appropriate duration of systemic
antifungal therapy. According to the most updated guidelines, the
duration of therapy for fungal chorioretinitis should be at least
four to six weeks and should ideally continue until all clinical
evidence of intraocular infection has been resolved (2). The current case is consistent with
these guidelines, supporting the proposal that four weeks of
antifungal treatment is necessary. Although the occurrence of
ocular infection is very low in newborns, close follow-up of
infants who survive fungemia remains essential, as in a minority of
cases, preterm infants with successfully treated fungemia may
develop a fungal abscess in the crystalline lens, as a result of
Candida sequestration (8).
In conclusion, in cases of fungal chorioretinitis,
early detection and rational duration of treatment using
fluconazole or other systemic antifungals may prevent severe ocular
involvement and avoid lifelong visual impairment. Particular care
should be taken to test for fungal chorioretinitis in the presence
of risk factors or external signs of intraocular inflammation
(3,9,10). To
the best of our knowledge, this is the first reported case of a
Candida infection disseminating from the eye to the hip
joint in an infant. The patient was successfully treated with
fluconazole, and the current results suggest that at least four to
six weeks of antifungal treatment should be administered in future
cases.
References
|
1
|
Dozier CC, Tarantola RM, Jiramongkolchai K
and Donahue SP: Fungal eye disease at a tertiary care center: The
utility of routine inpatient consultation. Ophthalmology.
118:1671–1676. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pappas PG, Kauffman CA, Andes D, Benjamin
DK Jr, Calandra TF, Edwards JE Jr, Filler SG, Fisher JF, Kullberg
BJ, Ostrosky-Zeichner L, et al: Clinical practice guidelines for
the management of candidiasis: 2009 update by the infectious
diseases society of America. Clin Infect Dis. 48:503–535. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Donahue SP, Greven CM, Zuravleff JJ, Eller
AW, Nguyen MH, Peacock JE Jr, Wagener MW and Yu VL: Intraocular
candidiasis in patients with candidemia. Clinical implications
derived from a prospective multicenter study. Ophthalmology.
101:1302–1309. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fraser VJ, Jones M, Dunkel J, Storfer S,
Medoff G and Dunagan WC: Candidemia in a tertiary care hospital:
Epidemiology, risk factors, and predictors of mortality. Clin
Infect Dis. 15:414–421. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tanaka M, Kobayashi Y, Takebayashi H,
Kiyokawa M and Qiu H: Analysis of predisposing clinical and
laboratory findings for the development of endogenous fungal
endophthalmitis. A retrospective 12-year study of 79 eyes of 46
patients. Retina. 21:203–209. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zaoutis TE, Greves HM, Lautenbach E,
Bilker WB and Coffin SE: Risk factors for disseminated candidiasis
in children with candidemia. Pediatr Infect Dis J. 23:635–641.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dupont B and Drouhet E: Cutaneous, ocular,
and osteoarticular candidiasis in heroin addicts: New clinical and
therapeutic aspects in 38 patients. J Infect Dis. 152:577–591.
1985. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Donahue SP, Hein E and Sinatra RB: Ocular
involvement in children with candidemia. Am J Ophthalmol.
135:886–887. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Brod RD, Flynn HW Jr, Clarkson JG,
Pflugfelder SC, Culbertson WW and Miller D: Endogenous Candida
endophthalmitis. Management without intravenous amphotericin B.
Ophthalmology. 97:666–674. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dellon AL, Stark WJ and Chetien PB:
Spontaneous resolution of endogenous Candida endophthalmitis
complicating intravenous hyperalimentation. Am J Ophthalmol.
79:648–654. 1975. View Article : Google Scholar : PubMed/NCBI
|