Introduction
Alzheimer's disease (AD), the most common form of
dementia, is a progressive neurodegenerative disease characterized
by a progressive decline in cognitive function, endangering a
growing proportion of the elderly population (1). Due to the lack of effective treatments,
the search for means of preventing/delaying the onset/progression
of AD remains a major research area (2). Exploration of methods for adjusting
risk factors is one direction to pursue in preventing/delaying AD.
Epidemiological studies have revealed that vascular factors are
involved in the increase of the incidence of AD, possibly resulting
in poor prognosis (3,4).
In general, vascular disease frequently coexists
with degenerative intracranial changes of patients with dementia,
which makes it difficult to identify risk factors associated with
cognitive decline and diagnose types of dementia. In a
population-based study on 308 patients with dementia, types of
dementia were re-evaluated in combination with data on vascular
lesions, as well as the incidence and progression of the disease
(5). Only 47% of those patients
initially diagnosed with AD were reclassified as pure AD, only 25%
of those diagnosed with vascular dementia (VD) were reclassified as
pure VD and most of the cases were of mixed dementia. There has
been a growing interest in the hypothesis that vascular diseases
are associated with AD and certain studies have revealed that
vascular system dysfunction may trigger the amyloid cascade
(6,7).
A previous study also found that vascular risk
factors accelerate the progression of AD (8). A consensus has now been reached that
early detection and treatment of classic vascular risk factors
reduce their impact on the epidemiology of dementia (9,10).
Although intimal medial thickness (IMT), a marker of early
atherosclerosis, is associated with cognitive decline and can be
used to measure subclinical vascular disease (11), previous studies have mainly focused
on community population samples with or without a history of stroke
(12–14). A longitudinal study on 66 patients
with AD showed a significant association between IMT and the
progression of cognitive impairment at 12-month follow-up (15). Although an increasing number of
studies investigated the association between vascular factors and
cognitive impairment in patients with AD, the findings showed
rather inconsistent and weak evidence of the association (16). Previous studies, most of which were
cross-sectional with a relatively small sample size, showed a weak
association between IMT and cognitive impairment, whereas a few
longitudinal studies revealed a rather significant association
(17,18). The lack of longitudinal research
design with a relatively large sample calls for a large sample
panel study on the association of vascular factors and cognitive
impairment in patients with AD. The present three-year prospective
study sought to establish whether carotid artery atherosclerosis
has a considerable impact on the acceleration of the progression of
cognitive decline in Chinese patients with early-stage AD, with a
focus on identifying the possible follow-up treatment, i.e.,
surgical procedure or medication.
Materials and methods
Study population
As the present study was a three-year panel study,
data were initially collected for 521 patients randomly selected
from 7 urban communities in the Chongqing metropolitan area (total
population, 35 million in Chongqing municipality, including 10
million urban residents), 437 of which remained after the
three-year follow-up. The sample was selected on the basis of the
following criteria: i) Diagnosis with probable AD according to the
National Institute of Neurological and Communicative Disorders and
Stroke and the Alzheimer's Disease and Related Disorders
Association criteria (19); and ii)
mild to moderate phase of the disease: 1–2 on the Clinical Dementia
Rating (CDR) scale (20). The
exclusion criteria were as follows: i) Clinical history of
cerebrovascular diseases, focal neurological signs, severe
subcortical leukoencephalopathy and/or cortical infarction
(21); ii) a Hachinski score
(22) of >4; iii) a diagnosis of
other types of dementia; iv) inability to comply with the study
assessment; v) mental illness; vi) alcohol or drug abuse; and vii)
relocation from the area or refusal to participate (8).
The clinical diagnosis of AD was made by a group of
highly qualified neurologists and psychiatrists. The present study
was approved by the Institutional Review Board of Third Military
Medical University (Chongqing, China) and all subjects provided
informed written consent according to the Declaration of
Helsinki.
Clinical assessment
On admission, all patients underwent a structured
interview for demographic data and medical history, as well as a
neurological examination and head imaging. The following data were
prospectively collected: Age, sex, educational level, cigarette
smoking, hypertension (previously diagnosed and treated or systolic
pressure >160 mmHg and/or diastolic pressure >90 mmHg
persistently observed during admission after the acute phase),
diabetes mellitus (previously diagnosed and treated or fasting
glucose >7 mmol/l in two blood samples after the acute phase),
and atrial fibrillation (diagnosed and treated previously or during
admission). All patients underwent magnetic resonance imaging
(MRI), brain scans as well as fluid-attenuated inversion recovery
(FLAIR). Among them, MRI sequences were used to detect infarction
and cerebral white matter lesions. Cerebral white matter lesions
were also defined as ill-defined periventricular hyper-intense
signals on T2 or FLAIR phase width an area of area ≥5 mm. Lesions
were quantitatively rated using the Wahlund scale (23).
Neuropsychological evaluation
Cognitive status was assessed using the Chinese
version of the Mini-Mental Status Examination (CMMS), which was
previously validated in elderly Chinese individuals as cognitive
screening measures (24), with a
scale ranging from 0–30 and with the boundary score of CMMS defined
as 17 (illiteracy), 20 (≤6 years of education) and 24 (>6 years
of education). Subjects who were abnormal according to CMMS
assessment were subjected to further neuropsychological tests,
including Alzheimer Disease Assessment Scale-cognitive subscale
(ADAS-cog) (25), CDR (20), Fuld Object Memory Evaluation (FOM)
(26), Rapid Verbal Retrieve (RVR)
(27), the Wechsler Adult
Intelligence Scale [Digit Span (DS) and Block Design (BD) subtests]
(28).
Functional ability to perform basic and instrumental
activities was evaluated using a modified Activities of Daily
Living (ADL) test (29), which
contained 20 basic and instrumental activities of daily living.
Each activity was rated on a 4-point scale: 1, no limitation; 2,
performs activities by oneself with certain difficulties; 3,
requires help with activities; and 4, unable to perform any
activity. Additive scores of ADL ranged from 20 to 80, with an ADL
score >20 indicating that the subject had certain difficulties
in self-care. The Hachinski Ischemic Scale (22) was used for evaluating significant
vascular disease.
Ultrasound examination
A high-resolution B-mode ultrasound examination of
the left and right carotid arteries was performed on 437 subjects
using an Aloka SSD-650 (Hitachi, Tokyo, Japan) with a 7.5- and
10-MHz transducer. Acquisition, processing and storage of B-mode
images were computer-assisted, utilizing the software specifically
designed for longitudinal studies (30). The examination involved scanning the
common carotid arteries, the carotid bifurcations and the first 2
cm of the internal carotid arteries. The IMT (31) (distance between the media-adventitia
interface and the lumen-intima interface) was automatically
measured twice on longitudinal B-mode images of the far wall of
each carotid artery. The value assigned corresponded to the maximum
thickness of the intima media of the carotid arteries. Most of the
examinations were performed by one examiner and all analyses of IMT
were made by the same skilled observer.
In a previous study, the association between carotid
artery stenosis and cognitive impairment was explored in a Chinese
population, revealing that the IMT value has more a significant
association with cognitive impairment than stenosis (32), leading to a major focus on the IMT
rather than stenosis in the present study.
Follow-up
Trained neurologists and psychiatry experts were
performed annual follow-up from November 2011 to November 2014.
Each follow-up procedure included CMMS, ADAS-cog, ADL, RVR, BD, DS
and FOM assessment. If new neurological signs of localization
suggested new brain lesions, a cranial MRI scan was performed.
Statistical analysis
Statistical analysis was performed using SPSS 19.0
for Windows (International Business Machines Corp., Armonk, NY,
USA). All variables including adjusting factors (e.g., age, sex,
education and vascular risk factors) as well as carotid IMT were
introduced into mixed-effect regression analyses for the three-year
panel data in order to investigate longitudinal associations of
carotid IMT with cognitive function. Mixed-effect regression adopts
fixed as well as random effects in the estimation and eliminates
the effects of confounding variables from unmeasured time-invariant
causes in the panel data (33). In
the mixed-effects regression analyses, each measure of cognitive
function was separately regressed on carotid IMT (i.e., overall
differences in carotid IMT over the three-year period), a battery
of adjusting variables, and an interaction term of carotid IMT with
age (i.e., changes in cognitive functions associated with carotid
IMT over time). Values are expressed as the mean ± standard
deviation (SD).
Results
The study included 521 patients with mild to
moderate AD, among which 45 patients did not comply with the
research assessment, 33 patients were lost to follow-up and 6
patients died, while the 437 patients remaining successfully
completed the 3-year follow-up study. The mean age of the subjects
at baseline was 69.2±10.5 years, 45.6% were male and the mean
education was 10.7 years. The mean carotid IMT was 2.3±1.2 mm
(range, 0.8–4.6 mm). Demographic data and the clinical baseline
characteristics are presented in Table
I.
 | Table I.Baseline characteristics of patients
with mild to moderate Alzheimer's disease. |
Table I.
Baseline characteristics of patients
with mild to moderate Alzheimer's disease.
| Variables | Mean (SD) | Range |
|---|
| Age (years) | 69.2 (10.5) | 58–88 |
| Gender (% male) | 45.6 |
|
| Education
(years) | 10.7 (3.5) | 6–17 |
| Mean arterial
pressure (mmHg) | 97.3 (14.8) | 64–165 |
| Total cholesterol
(mg/dl) | 201.4 (32.6) | 115–323 |
| Body mass index
(kg/m2) | 25.3 (4.2) | 16.7–38.4 |
| Cardiovascular
medication use (%) | 19.8 |
|
| Current smoking
habit (%) | 45.1 |
|
| Hachinski ischemic
scale | 2.3 (1.2) | 0–5 |
| Wahlund scale | 4.6 (4.5) | 0–14 |
| Mean carotid IMT
(mm) | 2.3 (1.2) | 0.8–4.6 |
First, mixed-effects regression analysis for CMMS
was performed in order to estimate the effect of carotid IMT and
other adjusting variables. As expected, the preliminary
mixed-effects regression estimate of the model (not presented here)
did not reveal any statistically significant effect of carotid IMT
on CMMS. In the subsequent mixed-effects regression estimation
(Table II), a series of
neuropsychological and functional test scores were regressed on the
carotid IMT value and other adjusting variables in all six models.
The results showed that carotid IMT had a statistically significant
effect in four of the models (ADAS-cog, FOM, DS, and RVR), while
the effect of carotid IMT was not significant in the ADL and BD
models. It was also found that the effects of the interaction
between carotid IMT and age (change over time) were statistically
significant in ADAS-cog (b=−0.676, P=0.036), FOM (b=−0.41,
P=0.023), DS (b=−1.35, P=0.034) and RVR (b=−1.52, P=0.038),
respectively.
 | Table II.Mixed-effects regression estimates of
neuropsychological test results and performance on carotid IMT and
covariates. |
Table II.
Mixed-effects regression estimates of
neuropsychological test results and performance on carotid IMT and
covariates.
|
| Carotid IMT | Carotid
IMTxAge |
|---|
|
|
|
|
|---|
| Neuropsychological
test | b | SE | b | SE |
|---|
| ADAS-cog | −35.2a | 14.3 | −0.68b | 0.31 |
| ADL |
1.46 |
0.98 | −0.03 | 0.01 |
| FOM | −23.5a | 11.7 | −0.41b | 0.18 |
| BD | −17.3 | 24.2 | −1.32 | 0.08 |
| DS | −46.2a | 29.2 | −1.35b | 0.53 |
| RVR | −65.2a | 32.4 | −1.52b | 0.52 |
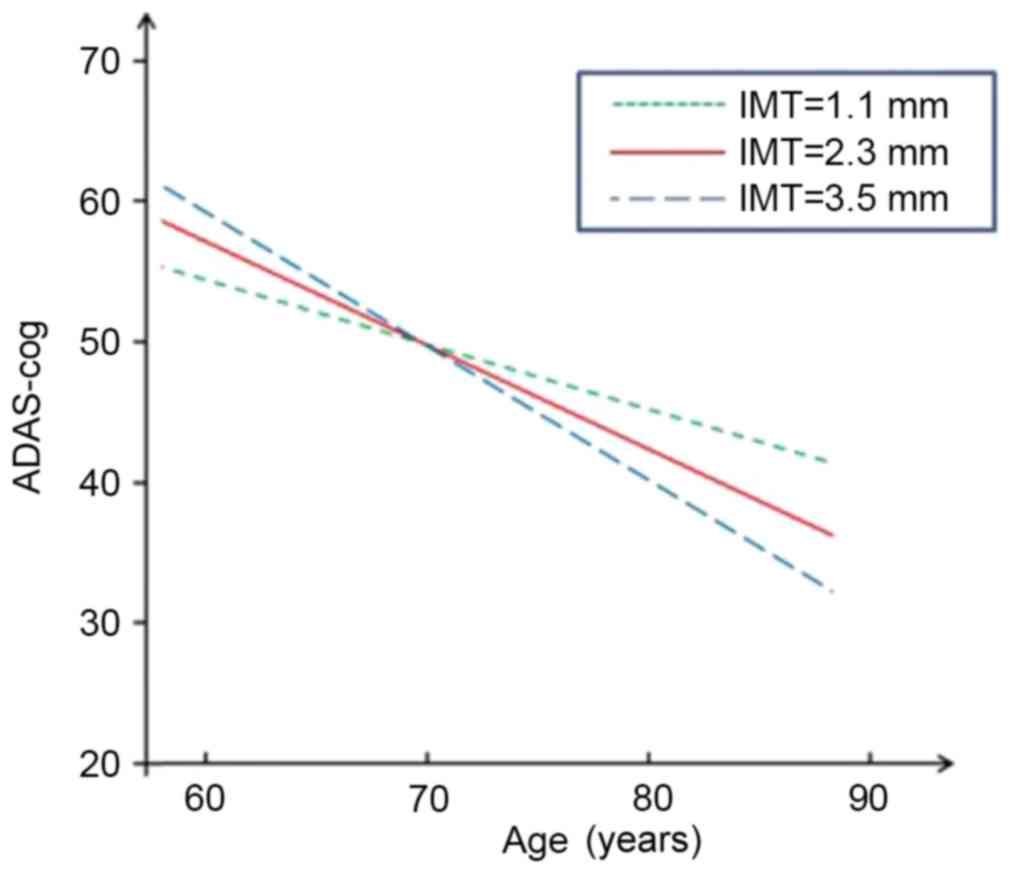
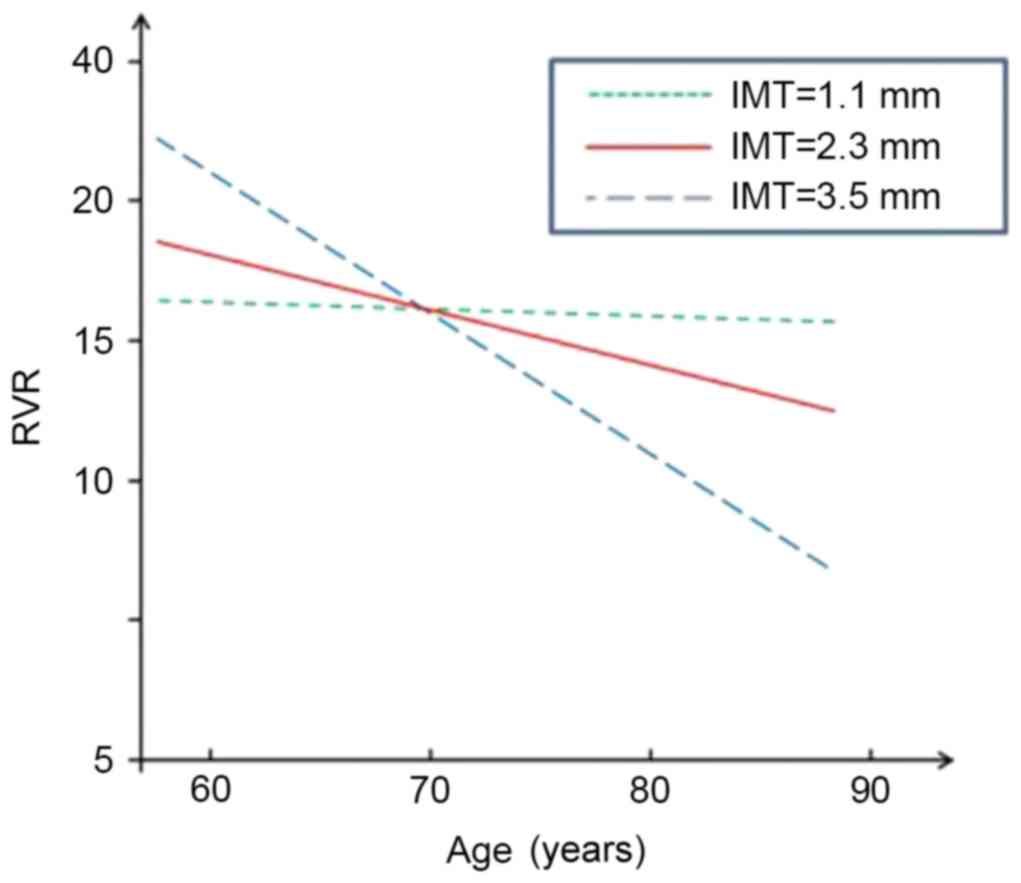
Figs. 1–4 present significant carotid IMTxAge
interactions for ADAS-cog, ADL, DS and RVR, respectively, and
visualize the nature of the significant interactions between
carotid IMT and age in the four regression models in Table II. Each fig. shows age-associated
changes in cognitive performance as a function of different levels
of carotid IMT (IMT=1.1, 2.3 and 3.5 mm), with all the covariates
adjusted in the analyses. The figures are based on the association
of mean value of carotid IMT ± SD and predictive cognitive values.
The figures clearly show that the higher the IMT value, the steeper
the decline in the four neuropsychological test scores as people
age.
Discussion
The present three-year prospective study
investigated the longitudinal change of cognitive function in
patients with mild to moderate AD in terms of different carotid
artery IMT values. During the follow-up period, patients with a
relatively high IMT showed a significantly greater prospective
decline in performance according to various cognitive measures,
including ADAS-cog, RVR, FOM and DS. Individuals with a greater
carotid IMT showed a faster prospective decline in cognitive
function, particularly in verbal fluency and memory for objects and
digits. The present findings are consistent with previous ones,
according to which cognitive decline in AD patients was associated
with subclinical vascular disease (15).
The results of the present study demonstrated that
carotid IMT is associated with a various types of cognitive
dysfunction, particularly verbal and non-verbal memory, semantic
fluency and executive function. Among the scales significantly
associated with IMTxAge, FOM is a group of neuropsychological tests
including memory, physical perception (touch discrimination),
visual naming, left-right orientation and learning features, while
RVR is applied to detect semantic memory storage function. FOM and
RVR can be used in combination to evaluate the degree of memory
impairment. In the present study, DS was adopted from the Wechsler
intelligence tests, and immediate memory and attention are major
measures of cognitive function in this test. By combining a battery
of neuropsychological tests, detailed information on cognitive
function in verbal and non-verbal memory, semantic fluency and
executive function was obtained.
Previous studies suggested several hypothetical
interpretations of the association between vascular risk factors
and AD. While it has been speculated that cerebrovascular disease
is not involved in an account of cerebral atrophy caused by
neurodegeneration, it has also been suggested that cerebral
vascular factors have a key role in inducing or maintaining the
pathological process of typical AD degeneration (34). Other studies reported that a lack of
cerebral blood flow may amplify or strengthen the influence of the
degeneration process, independently causing additional damage
(35). It was also suggested that
chronic cerebral hypoperfusion caused by severe carotid artery
atherosclerosis is one of the causes of cognitive impairment
(36). In a previous study, in which
cerebrovascular pathology appears to be, along with aging, a key
permissible factor for the development of dementia-associated
neurodegeneration, it was found that AD patients showed a
significantly higher prevalence of vascular pathology and
cerebrovascular disease than patients with α-synucleinopathy, prion
disease and frontotemporal lobar degeneration due to immunoreactive
inclusions of Tau and TAR DNA binding protein 43 (37).
A previous study suggested that vascular risk
factors are associated with mild cognitive impairment and AD
(38). Previous findings regarding
VD and AD patients also showed that vascular risk factors, brain
pathology and cognitive characteristics have a greater overlap than
previously known (39), and
particularly individuals with memory impairment have a risk of
various types of dementia. Moreover, it has been proposed that
atherosclerosis and AD share a common infectious/inflammatory
pathoetiology and individuals with atherosclerosis or AD are
neither merely ‘ill’ nor ‘old’, but that acquired
infection/inflammation and endocrine aging are rather likely to
have a joint role in causing these age-associated diseases
(40). Subclinical vascular diseases
may directly or indirectly affect cognitive function through
various mechanisms, and the measured values of carotid
atherosclerosis are associated with various cardiovascular risk
factors, including demographic, metabolic, immune and lifestyle
factors as well as cognitive decline (41). Other hypothetical mechanisms are
common genetic susceptibility (such as apolipoprotein E ε4 allele),
chronic cerebral hypoperfusion, asymptomatic cerebral infarction
and other associated brain structural changes, such as atrophy of
the cortex (42).
The present study clearly indicated that the
severity of carotid artery atherosclerosis accelerates cognitive
impairment and acts as a potential risk factor for AD. Loss of
cognition allegedly has a detrimental influence on individuals and
society, calling for active prevention or deceleration of its
progress. Considering the fact that the development of any specific
disease-modifying treatment for AD is unlikely in the near future,
the present study underscores the possibility that early
intervention to reduce atherosclerosis may be of clinical benefit
for AD. It further suggests that the application of various
treatments for carotid arterial atherosclerosis is worthwhile in
order to assess their effect on cognitive function in patients.
Considering the difficulty of identifying the
respective contributions of degenerative and vascular components to
morbidity and pathological processes in each patient, a more
rational approach to the problem may be a comprehensive and
consistent treatment to keep modifiable vascular risk factors at
their lowest level among patients with cognitive impairment,
regardless of whether they have been diagnosed as dementia
(43). A previous study revealed
that the treatment of vascular risk factors may slow down cognitive
decline in patients with AD (44).
However, it has rarely been reported whether treatments of IMT,
such as interventional operation, decelerate the progression of AD.
The present study confirmed that severe IMT greatly accelerates the
progress of AD, further suggesting that AD patients with high IMT
may benefit from aggressive endovascular treatment.
For the prevention and treatment of AD, it is
important to make a diagnosis as early as possible and to intervene
with risk factors that are pivotal for its progression (45). In either normal or cognitively
impaired population groups, asymptomatic carotid atherosclerotic
disease has an important role in accelerating cognitive damage
(46). It is noteworthy that the
present study was performed in a large Chinese metropolitan area
with 93% of the population being of Han Chinese ethnicity who have
similar cultural habits, including a relatively hig-fat diet, which
represents a risk factor for atherosclerosis.
In conclusion, while certain controversies remain
regarding the association between vascular factors and cognitive
impairment in patients with AD, the present 3-year prospective
study provided further evidence that carotid atherosclerosis is a
predictive or predisposing factor for the progression of cognitive
impairment in AD patients, particular that regarding verbal and
non-verbal memory, semantic fluency and executive function. The
combined application of widely used neuropsychological measurement
scales and the use of time-varying covariates are highlighted in
this study. However, the limitations of the present study were that
only patients with mild to moderate AD were selected as the study
sample, and that the carotid artery IMT was used as a single
parameter to resemble carotid atherosclerosis in the assessment. In
addition, it should be noted that among previous studies, the use
of inconsistent study samples as well as different follow-up
periods and neuropsychological scales may also lead to the
contradictory and inconsistent findings in this field. Therefore,
the association of carotid artery IMT with the accelerated decline
of cognitive function and even other types of cognitive impairment
should be further studied after adjusting these covariate
factors.
Acknowledgements
Funding for this study was provided by the Program
for Innovation Team Building at Institutions of Higher Education in
Chongqing (grant no. KJTD201301).
References
|
1
|
Breteler MM: Vascular risk factors for
Alzheimer's disease: An epidemiologic perspective. Neurobiol Aging.
21:153–160. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhu CW, Scarmeas N, Torgan R, Albert M,
Brandt J, Blacker D, Sano M and Stern Y: Longitudinal study of
effects of patient characteristics on direct costs in Alzheimer
disease. Neurology. 67:998–1005. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gorelick PB: Risk factors for vascular
dementia and Alzheimer disease. Stroke. 35 11 Suppl 1:S2620–S2622.
2004. View Article : Google Scholar
|
|
4
|
Viticchi G, Falsetti L, Vernieri F,
Altamura C, Bartolini M, Luzzi S, Provinciali L and Silvestrini M:
Vascular predictors of cognitive decline in patients with mild
cognitive impairment. Neurobiol Aging. 33:1127.e1–9. 2012.
View Article : Google Scholar
|
|
5
|
Aguero-Torres H, Kivipelto M and von
Strauss E: Rethinking the dementia diagnosis in a population-based
study: What is Alzheimer's disease and what is vascular dementia? A
study from the Kungsholmen project. Dement Geriatr Cogn Disord.
22:244–249. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Grammas P, Yamada M and Zlokovic B: The
cerebromicrovasculature: A key player in the pathogenesis of
Alzheimer's disease. J Alzheimers Dis. 4:217–123. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Humpel C and Marksteiner J:
Cerebrovascular damage as a cause for Alzheimer's disease. Curr
Neurovasc Res. 2:341–347. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li J, Zhang M, Xu ZQ, Gao CY, Fang CQ,
Deng J, Yan JC, Wang YJ and Zhou HD: Vascular risk aggravates the p
rogression of Alzheimer's disease in a Chinese cohort. J Alzheimers
Dis. 20:491–500. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Luzzi S, Vella L, Bartolini M, Provinciali
L and Silvestrini M: Atherosclerosis in the evolution of
Alzheimer's disease: Can treatment reduce cognitive decline? J
Alzheimers Dis. 20:893–901. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
López-Olóriz J, López-Cancio E, Arenillas
JF, Hernández M, Jiménez M, Dorado L, Barrios M, Soriano-Raya JJ,
Miralbell J, Cáceres C, et al: Asymptomatic cervicocerebral
atherosclerosis, intracranial vascular resistance and cognition:
The AsIA-neuropsychology study. Atherosclerosis. 230:330–335. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lorenz MW, Markus HS, Bots ML, Rosvall M
and Sitzer M: Prediction of clinical cardiovascular events with
carotid intima-media thickness: A systematic review and
meta-analysis. Circulation. 30:459–467. 2007. View Article : Google Scholar
|
|
12
|
Johnston SC, O'Meara ES, Manolio TA,
Lefkowitz D, O'Leary DH, Goldstein S, Carlson MC, Fried LP and
Longstreth WT Jr: Cognitive impairment and decline are associated
with carotid artery disease in patients without clinically evident
cerebrovascular disease. Ann Intern Med. 140:237–247. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Komulainen P, Kivipelto M, Lakka TA,
Hassinen M, Helkala EL, Patja K, Nissinen A and Rauramaa R: Carotid
intima-media thickness and cognitive function in elderly women: A
population-based study. Neuroepidemiology. 28:207–213. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Muller M, Grobbee DE, Aleman A, Bots M and
van der Schouw YT: Cardiovascular disease and cognitive performance
in middle aged and elderly men. Atherosclerosis. 190:143–149. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Silvestrini M, Gobbi B, Pasqualetti P,
Bartolini M, Baruffaldi R, Lanciotti C, Cerqua R, Altamura C,
Provinciali L and Vernieri F: Carotid atherosclerosis and cognitive
decline in patients with Alzheimer's disease. Neurobiol Aging.
30:1177–1183. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Urbanova B, Tomek A, Mikulik R, Magerova
H, Horinek D and Hort J: Neurosonological examination: A
non-invasive approach for the detection of cerebrovascular
impairment in AD. Front Behav Neurosci. 8:42014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tachibana H, Washida K, Kowa H, Kanda F
and Toda T: Vascular function in Alzheimer's disease and vascular
dementia. Am J Alzheimers Dis Other Demen. 31:437–442. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Heinzel S, Liepelt-Scarfone I, Roeben B,
Nasi-Kordhishti I, Suenkel U, Wurster I, Brockmann K, Fritsche A,
Niebler R, Metzger FG, et al: A neurodegenerative vascular burden
index and the impact on cognition. Front Aging Neurosci.
9:1612014.
|
|
19
|
McKhann G, Drachman D, Folstein M, Katzman
R, Price D and Stadlan EM: Clinical diagnosis of Alzheimer's
disease: Report of the NINCDS-ADRDA work group under the auspices
of department of health and human services task force on
Alzheimer's disease. Neurology. 34:939–944. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hughes CP, Berg L, Danziger WL, Coben LA
and Martin RL: A new clinical scale for staging of dementia. Br J
Psychiatry. 140:566–572. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Román GC, Tatemichi TK, Erkinjuntti T,
Cummings JL, Masdeu JC, Garcia JH, Amaducci L, Orgogozo JM, Brun A,
Hofman A, et al: Vascular dementia: Diagnostic criteria for
research studies. Report of the NINDS-AIREN International Workshop.
Neurology. 43:250–260. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hachinski VC, Iliff LD, Zilhka E, Du
Boulay GH, McAllister VL, Marshall J, Russell RW and Symon L:
Cerebral blood flow in dementia. Arch Neurol. 32:632–637. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wahlund LO, Barkhof F, Fazekas F, Bronge
L, Augustin M, Sjögren M, Wallin A, Ader H, Leys D, Pantoni L, et
al: A new rating scale for age-related white matter changes
applicable to MRI and CT. Stroke. 32:1318–1322. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhou HD, Wang JY, Li J, Deng J, Gao C and
Chen M: Study on frequency and predictors of dementia after
ischemic stroke: The Chongqing stroke study. J Neurol. 251:421–427.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rosen WG, Mohs RC and Davis KL: A new
rating scale for Alzheimer's disease. Am J Psychiatry.
141:1356–1364. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fuld PA, Masur DM, Blau AD, Crystal H and
Aronson MK: Object-memory evaluation for prospective detection of
dementia in normal functioning elderly: Predictive and normative
data. J Clin Exp Neuropsychol. 12:520–528. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang M: Prevalence study on dementia and
Alzheimer disease. Zhonghua Yi Xue Za Zhi. 70424–428. (430)1990.(In
Chinese). PubMed/NCBI
|
|
28
|
Welsh KA, Butters N, Hughes JP, Mohs RC
and Heyman A: Detection and staging of dementia in Alzheimer's
disease. Use of the neuropsychological measures developed for the
consortium to establish a registry for Alzheimer's disease. Arch
Neurol. 49:448–452. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Katz S, Downs TD, Cash HR and Grotz RC:
Progress in development of the index of ADL. Gerontologist.
10:20–30. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Touboul PJ, Prati P, Scarabin PY, Adrai V,
Thibout E and Ducimetière P: Use of monitoring software to improve
the measurement of carotid wall thickness by B-mode imaging. J
Hypertens. 10 Suppl:S37–S41. 1992. View Article : Google Scholar
|
|
31
|
Dubey AK, Varma Y, Dubey S, Singh G, Dubey
AK, Sharma V and Grade S: PW195 lipid profile and carotid intimal
medial thickness in different stages of chronic kidney disease.
Global Heart. 9:e2972014. View Article : Google Scholar
|
|
32
|
Xiang J, Zhang T, Yang QW, Liu J, Chen Y,
Cui M, Yin ZG, Li L, Wang YJ, Li J and Zhou HD: Carotid artery
atherosclerosis is correlated with cognitive impairment in an
elderly urban Chinese non-stroke population. J Clin Neurosci.
20:1571–1575. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Firebaugh G, Warner C and Massoglia M:
Fixed effects, random effects and hybrid models for causal
analysisMorgan SL: Handbook of Causal Analysis for Social Research.
Springer Science+Business Media Dordrecht; pp. 113–132. 2013,
View Article : Google Scholar
|
|
34
|
Schneider JA, Wilson RS, Bienias JL, Evans
DA and Bennett DA: Cerebral infarctions and the likelihood of
dementia from Alzheimer disease pathology. Neurology. 62:1148–1155.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Snowdon DA, Greiner LH, Mortimer JA, Riley
KP, Greiner PA and Markesbery WR: Brain infarction and the clinical
expression of Alzheimer disease: The Nun study. JAMA. 227:813–817.
1997. View Article : Google Scholar
|
|
36
|
Ruitenberg A, den Heijer T, Bakker SL, van
Swieten JC, Koudstaal PJ, Hofman A and Breteler MM: Cerebral
hypoperfusion and clinical onset of dementia: The Rotterdam Study.
Ann Neurol. 57:789–794. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Toledo JB, Arnold SE, Raible K,
Brettschneider J, Xie SX, Grossman M, Monsell SE, Kukull WA and
Trojanowski JQ: Contribution of cerebrovascular disease in autopsy
confirmed neurodegenerative disease cases in the National
Alzheimer's Coordinating Centre. Brain. 136:2697–2706. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Stampfer MJ: Cardiovascular disease and
Alzheimer's disease: Common links. J Intern Med. 260:211–223. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
de la Torre JC: Is Alzheimer's disease a
neurodegenerative or a vascular disorder? Data, dogma, and
dialectics. Lancet Neurol. 3:184–190. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lathe R, Sapronova A and Kotelevtsev Y:
Atherosclerosis and Alzheimer-diseases with a common cause?
Inflammation, oxysterols, vasculature. BMC Geriatr. 21:14–36.
2014.
|
|
41
|
Devereux RB and Alderman MH: Role of
preclinical cardiovascular disease in the evolution from risk
factor exposure to development of morbid events. Circulation.
88:1444–1455. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bots ML, van Swieten JC, Breteler MM, de
Jong PT, van Gijn J, Hofman A and Grobbee DE: Cerebral white matter
lesions and atherosclerosis in the Rotterdam study. Lancet.
341:1232–1237. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Viswanathan A, Rocca WA and Tzourio C:
Vascular risk factors and dementia. How to move forward? Neurology.
72:368–374. 2009.PubMed/NCBI
|
|
44
|
Deschaintre Y, Richard F, Leys D and
Pasquier F: Treatment of vascular risk factors is associated with
slower decline in Alzheimer disease. Neurology. 73:674–680. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Morris JC, Storandt M, Miller JP, McKeel
DW, Price JL, Rubin EH and Berg L: Mild cognitive impairment
represents early-stage Alzheimer disease. Arch Neurol. 58:397–405.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Silvestrini M, Vernieri F, Pasqualetti P,
Matteis M, Passarelli F, Troisi E and Caltaqirone C: Impaired
cerebral vasoreactivity and risk of stroke in patients with
asymptomatic carotid artery stenosis. JAMA. 283:2122–2127. 2000.
View Article : Google Scholar : PubMed/NCBI
|