Introduction
With the rapid development of industrialization and
an increasing number of traffic accidents, the incidence rate of
spinal fractures is constantly rising, reaching as high as 5–6% of
full-body fractures, of which the thoracolumbar fracture is the
most common. Thoracolumbar vertebral fracture refers to the state
that bone cortical continuity is impaired by an external force
(1), which is manifested by local
pain. Without prompt treatment, nerve damage (motion and sense
dysfunctions of double lower limbs, excretion dysfunction) may
occur, thereby causing more serious complications (2). The traditional open osteosynthesis
shows increased trauma, massive bleeding, long length of hospital
stay and multiple complications (3).
Moreover, the ischemic necrosis and fibrosis of muscles caused by
extensive detachment and repeated sustained traction of tissues
adjacent to the vertebral body (fascia muscularis, muscle and
anadesma) can seriously affect the prognosis of patients, which may
lead to the intractable stiffness of the waist and back. As early
as the 1980s, through using percutaneous pedicle screws
osteosynthesis, Magerl (4) created
the minimally invasive technique for the treatment of spinal
trauma. The clinical application of minimally invasive percutaneous
pedicle screws osteosynthesis has gradually been popularized in
recent years (5). In this study, 70
patients who suffered from spinal fractures and received treatment
at our hospital from January 2014 to June 2016 were selected. The
minimally invasive percutaneous pedicle screws osteosynthesis and
traditional open surgery were used for treatment, which achieved
satisfactory clinical effects.
Materials and methods
Sample selection
Seventy patients, who suffered from thoracolumbar
vertebra fracture with no nerve damage and received treatment at
our hospital from January 2014 to June 2016, were selected and
randomly divided into either the minimally invasive percutaneous
pedicle screws osteosynthesis group (MIPPSO group) or the
traditional open pedicle screws osteosynthesis group (TOPSO group)
with 35 cases in each group. The selected patients or their
families signed written informed consent form, and the study was
approved by the Ethics Committee at Xuzhou Hospital.
The inclusion criteria were as follows: a) the
patient was diagnosed with a thoracolumbar vertebra fracture, b)
the patient suffered from Type-A, Grade-E single segmental
fracture, with no need for spinal canal decompression, and c) the
patient who suffered from fresh fracture within two weeks. The
exclusion criteria were as follows: a) the patient with
thoracolumbar vertebra fracture who needed spinal canal
decompression to relieve nervous symptoms; and b) pathological
and/or old fracture (Table I).
 | Table I.Comparison of general conditions of
two groups of patients. |
Table I.
Comparison of general conditions of
two groups of patients.
| Item | MIPPSO group | TOPSO group | P-value |
|---|
| Sex (Male/Female,
n) | 23/12 | 24/11 | >0.05 |
| Age (mean ± SD,
years) | 36.89±7.21 | 37.01±6.83 | >0.05 |
| Weight (mean ± SD,
kg) | 63.26±9.27 | 64.54±8.65 | >0.05 |
| Denis typing (n) |
|
| >0.05 |
| Simple
compression fracture | 8 | 9 |
|
| Blowout
fracture | 27 | 26 |
|
| Injured segment
(n) |
|
| >0.05 |
| T11 | 2 | 1 |
|
| T12 | 7 | 6 |
|
| L1 | 20 | 21 |
|
| L2 | 6 | 7 |
|
Materials
The percutaneous pedicle screw system, which was
purchased from Changzhou Kanghui Medical Innovation Co., Ltd.
(Changzhou, China), has good biocompatibility, no obvious allergic
reaction and no effect on magnetic resonance examination.
Methods
Patients in the MIPPSO group were treated as
follows. The patient assumed the position of prone hyperextension,
thereby suspending the abdomen. The injured vertebra and the
projection of upper and lower vertebral pedicle center on the body
surface was orientated and marked by using a C-arm X-ray machine
(Siemens, Frankfurt, Germany). The towels were routinely
sterilized, and then a total of four longitudinal incisions, 2.0 cm
in length, were made along with the orientation under general
anesthesia with endotracheal intubation. The tissue was cut open
layer by layer via a blunt separation to expose the operative
field. According to the perspective of the C-arm machine, the screw
was kept in parallel with the end plate, keeping a 10–15° angle of
sagittal orientation towards the inside; then, the screw was placed
into vertebral pedicle. It was ensured that the inner cortex was
not broken through the screw and the position was placed well under
the perspective of the C-arm machine. The same method was adopted
to place other vertebral pedicle screws. Then, the fixation rods
were installed. The pre-curved fixation rods were successively
placed into the upper and lower pedicle screw tail grooves via a
subcutaneous muscular tunnel. The injured vertebra was reset
supporting by the distracter. After confirming the satisfactory
reduction, all the nuts were tightened. With no placement of a
drainage strip, the incision was sutured layer by layer. In the
TOPSO group, surgery was conducted in accordance with the
traditional method.
Main observation indexes
The main observation indexes were outlined as
follows:
Pre-operative parameters
The pre-operative parameters include the length of
surgical incision, duration of operation, bleeding during operation
and length of hospital stay of patients in both groups.
Pain assessment
Pain assessment was conducted using the visual
analog scale (VAS) scoring system (6). The corresponding point of pain
intensity, which the patient felt on the 10 cm line, was confirmed.
The VAS scores of patients in both groups were compared before the
operation and on the post-operative 1st, 3rd and 5th day,
respectively.
Inflammation-related indexes
Through the respective detection of CRP levels and
CK activities in peripheral blood before operation and at
post-operative 24 and 48 h, the changes in levels of serum CRP
levels and CK activities of pre-operation and post-operation of
patients in both groups were compared.
Imaging indexes
Through the pre-operative X-ray examination and
conducting re-examinations on the post-operative 3rd day and in the
1st year, the changes of Cobb's angles of pre-operation and
post-operation of patients in both groups were compared. The
anterior margin height of injured vertebra = Actual
height/Reference height × 100%. Reference height = the sum of upper
and lower anterior margin height of injured vertebra/2 × 100%. The
measure of Cobb's angle and sagittal index (SI) referred to the
literature (7).
Statistical analysis
The SPSS 18.0 software (SPSS Inc., Chicago, IL, USA)
was used for statistical analysis. All data were expressed as mean
± SD. The t-test and Chi-square test were used to compare the data.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparisons of perioperative
parameters of two groups of patients
The length of surgical incision, duration of
operation, bleeding volume of operation and length of hospital stay
of patients in both groups were compared. The MIPPSO group had the
advantages of small incision, short duration of operation, less
bleeding and short hospital stay, and there was a statistically
significant difference in each parameter between the groups of data
(P<0.05) (Table II).
 | Table II.Comparisons of perioperative
parameters of two groups of patients (mean ± SD, n=35). |
Table II.
Comparisons of perioperative
parameters of two groups of patients (mean ± SD, n=35).
| Item | MIPPSO group | TOPSO group | P-value |
|---|
| Length of incision
(cm) |
2.04±1.32 |
9.57±1.02 | <0.05 |
| Duration of operation
(min) |
59.46±7.28 |
123.16±4.65 | <0.05 |
| Bleeding volume of
operation (ml) |
21.31±9.76 |
162.35±30.64 | <0.05 |
| Length of hospital
stay (days) |
5.28±3.50 |
10.37±2.33 | <0.05 |
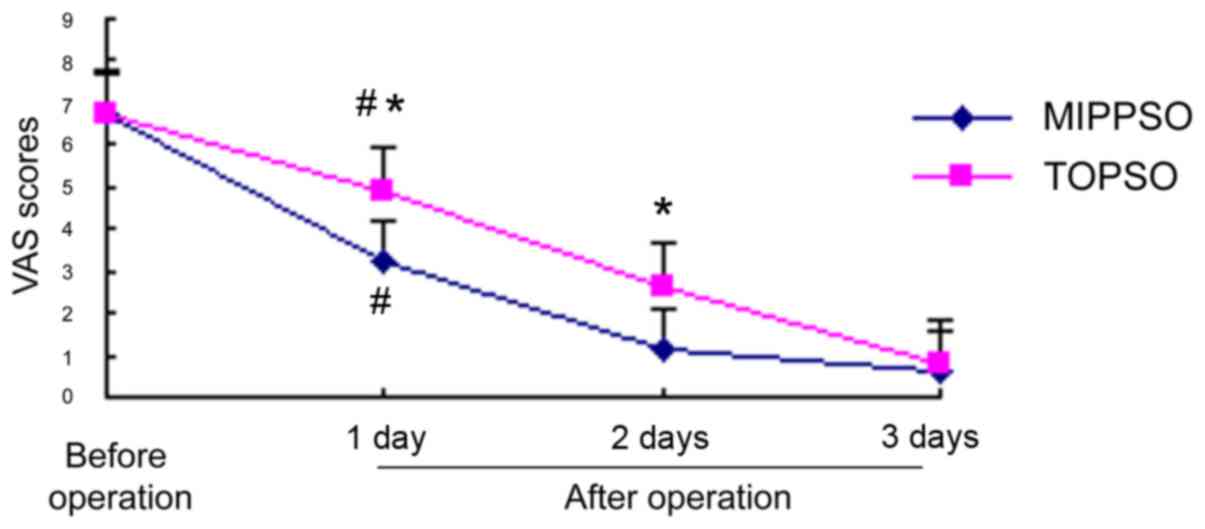
Comparisons of VAS pain scores of the
groups of patients
The pre-operative VAS pain scores of patients in the
MIPPSO group and the TOPSO group were 6.76±1.80 and 6.69±2.01,
respectively, which showed no statistically significant difference
(P>0.05). The scores on the post-operative 1st and 3rd day in
the MIPPSO group were, respectively 3.23±1.50 and 1.14±1.37, while
the scores on the post-operative 1st and 3rd day in the TOPSO group
were 4.91±1.52 and 2.66±1.14, respectively. The pain of both groups
on the post-operative 1st and 3rd day were relieved when compared
to levels pre-operation, with a statistically significant
difference (P<0.05). Compared to the TOPSO group, the ease of
pain in the MIPPSO group was more obvious, and the difference was
statistically significant (P<0.05). The pain scores of both
groups on the post-operative 5th day were 0.58±0.54 and 0.81±1.06,
and there was no statistically significant difference (P>0.05)
(Fig. 1).
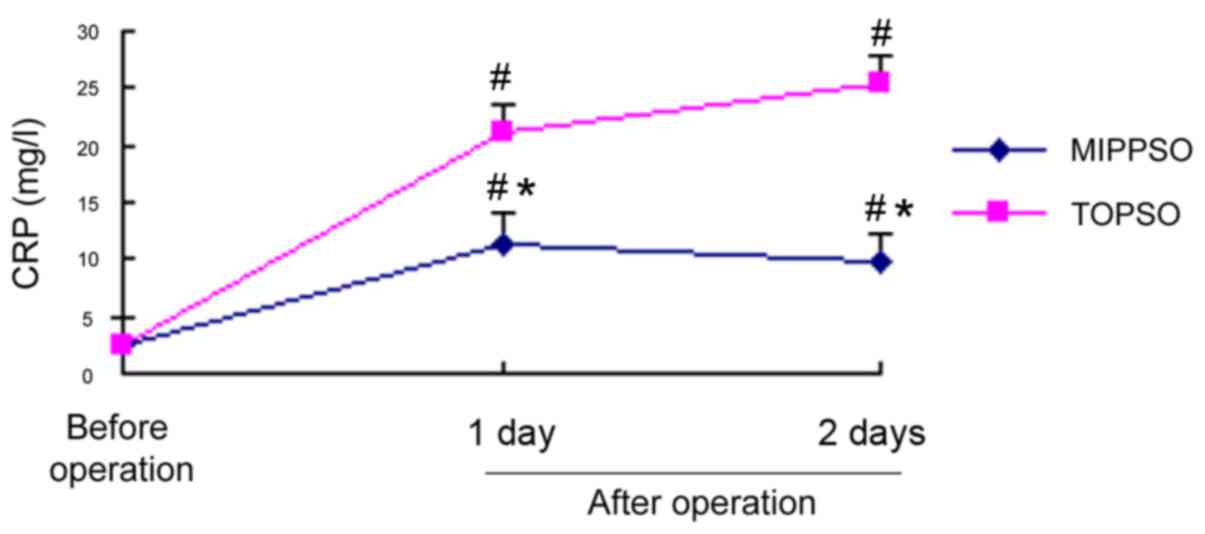
Changes of pre-operative and
post-operative inflammatory indexes (serum CRP and CK) of both
groups of patients
Comparison of changes of pre-operative and
post-operative serum CRP of both groups of patients
The baseline serum CRPs of patients in both groups
before the operation were comparable. The serum CRPs of patients in
the MIPPSO group and the TOPSO group were 11.43±5.01 mg/l and
21.16±5.72 mg/l at post-operative 24 h, respectively. The
concentrations in the MIPPSO group and the TOPSO group were
respectively 9.67±6.25 mg/l and 25.39±2.86 mg/l at post-operative
48 h. The serum CRPs of both groups at 24 and 48 h after operation
were significantly increased when compared to the pre-operation
levels (P<0.05). Moreover, the serum CRPs in the TOPSO group at
post-operative 24 and 48 h were significantly higher than those in
the MIPPSO group (P<0.05) (Fig.
2).
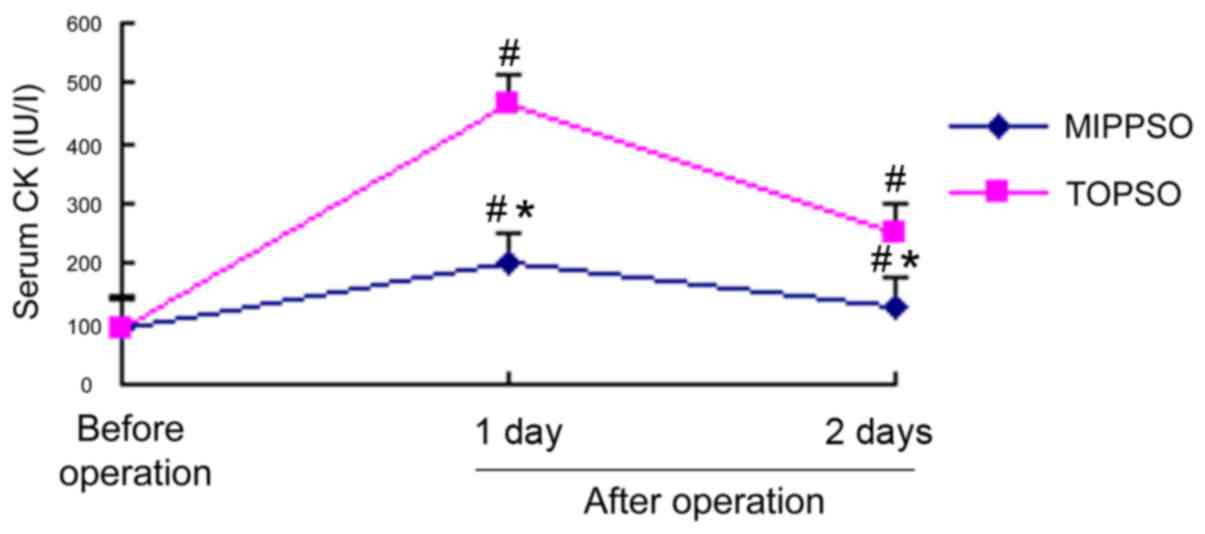
Comparisons of the changes of pre-operative and
post-operative serum CK of both groups of patients
The baseline serum CKs of patients in both groups
before the operation were comparable. The serum CKs of patients in
the MIPPSO group and TOPSO group were 201.34±45.96 IU/l and
465.61±45.27 IU/l at post-operative 24 h, respectively. The
concentrations were 129.67±56.25 IU/l and 252.39±42.65 IU/l at
post-operative 48 h, respectively. The serum CKs of both groups at
24 h post-operation were all significantly increased when compared
to the pre-operation (P<0.05). The concentrations were decreased
at post-operative 48 h but still higher than the pre-operation
(P<0.05). The serum CKs in the TOPSO group were significantly
higher than those in the MIPPSO group at post-operative 24 and 48 h
(P<0.05) (Fig. 3).
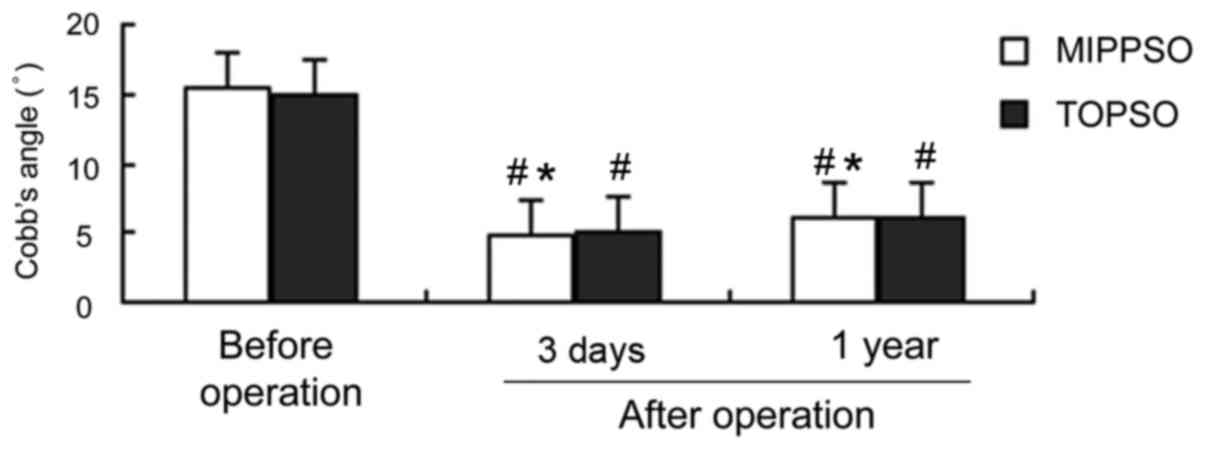
Changes of pre-operative and
post-operative imaging indexes (Cobb's angle and anterior margin
height of vertebral body) of both groups of patients
Comparisons of the changes of pre-operative and
post-operative Cobb's angle of two groups of patients
The Cobb's angles of patients in both groups before
the operation were 15.5±5.3° and 14.9±5.6°, respectively, which
were comparable (P>0.05). The Cobb's angles in the MIPPSO group
and the TOPSO group were 4.8±3.5° and 5.0±3.3° on the
post-operative 3rd day, and 6.1±2.9° and 6.2±2.7° in the
post-operative 1st year, respectively. The Cobb's angles of
patients in both groups on the 3rd day and in the 1st year
post-operation were all significantly decreased when compared to
pre-operation (P<0.05), but there were no statistically
significant differences between the groups (P>0.05) (Fig. 4).
Comparison of changes of the pre-operative and
post-operative anterior margin height of the vertebral body of both
groups of patients
The anterior margin heights of the vertebral body of
patients in both groups before the operation were 64.3±11.2% and
65.9±9.5%, respectively, which were comparable (P>0.05). The
anterior margin heights of vertebral body in the MIPPSO group and
TOPSO group were 90.1±3.0% and 89.5±3.75% on the post-operative 7th
day, and 88.2±2.3% and 87.6±2.9% in the post-operative 1st year,
respectively. The anterior margin heights of the vertebral body of
patients in both groups on the 7th day and in the 1st year
post-operation were all significantly increased when compared to
pre-operation (P<0.05), but there were no statistically
significant differences between the groups (P>0.05) (Fig. 5).
Post-operative complications
There was no orientation error, osteosynthesis
failure, cerebrospinal fluid leakage and iatrogenic nerve injury in
either group after operation. Seventy patients were treated and
discharged.
Discussion
The thoracolumbar vertebra fracture is often caused
by high-energy violent injuries, which are closely correlated with
the anatomy of the spine. T10-L2, which is a relatively small area
of thoracolumbar segment, is the region where thoracic kyphosis
gradually turns into the lumbar lordosis. Due to a lack of
protection of costovertebral structure, stress cannot be
transmitted to a larger sagittal articular surface, which makes it
easier to cause a spinal injury (8).
Surgery is the best therapy in the treatment of spinal injury
(9,10). Currently, there are three pathways of
surgery which include the anterior approach, posterior approach and
anterior and posterior combined approach, of which the most
commonly used mode is the posterior pedicle screw internal
fixation. However, the open reduction and internal fixation has a
large trauma, in which loose nails and broken nails as well as
post-operative complications such as a loss of correction can
easily occur (11). With the
enhancement in the quality of life and aesthetic requirements,
minimally invasive percutaneous pedicle screws osteosynthesis has
gradually highlighted its superiority in clinical practice.
With strong axial stress and significant effect of
distraction, the pedicle screw system can make the anterior and
posterior ligament fully extended, which is conducive to the
recovery of the height of injured vertebral body in order to
produce the effect of clamping plate between the ligament and soft
tissue in order to achieve indirect decompression, as well as to
correct kyphosis deformity, thereby achieving reduction, fixation
and early functional exercise. In the study of Palmisani et
al (12), minimally invasive
percutaneous pedicle screws osteosynthesis were used to treat 51
patients with a thoracolumbar vertebra fracture.
During the follow-up within 1–2 years, results
showed that the recovery of patients who received osteosynthesis
surgery was rapid, with fewer complications, and obtained
satisfactory clinical and functional effects. The results of this
study revealed that the pain of patients in both groups on
post-operative 1st and 3rd day were relieved when compared to the
pre-operation (P<0.05), of which the ease of pain in the MIPPSO
group was more significant (P<0.05). The use of minimally
invasive percutaneous osteosynthesis, which has a small surgical
incision, can effectively reduce the muscle stripping surface of
the waist and back, alleviate soft tissue injury, further avoid
post-operative back pain and reduce the pain of patients, thereby
improving the clinical effects. With the shortest fusion segment,
the strong pedicle screw osteosynthesis system can achieve the
effect of good orthopedics and maintain a three-dimensional
position of spine in order to further retain the motion segment
(13). The differences of the Cobb's
angle and anterior margin height of vertebral body of patients in
both groups before the operation were not statistically significant
and were therefore comparable (P>0.05). When comparing each
group to itself between the pre-operation and post-operation, the
Cobb's angles and anterior margin heights of vertebral body were
significantly ameliorated (P<0.05). However, there were no
statistically significant differences between the groups, whether
pre-operation or post-operation (P>0.05), which are consistent
with reports in literature (14).
The results indicate that minimally invasive percutaneous pedicle
screws osteosynthesis in the treatment of thoracolumbar vertebra
fracture is beneficial in order to correct the posterior convex
angle and recover the vertebral height of injured vertebra, so that
the gastrointestinal, cardiac and cerebral function abnormalities,
infection, spinal deformity and other complications can be reduced
and the pain can be relieved effectively.
In this study, the length of surgical incision,
duration of operation, bleeding volume of operation and length of
hospital stay of patients in both groups were compared, and we
found that the MIPPSO group had advantages of small incision, short
duration of operation, less bleeding and shorter hospital stay,
which shows a statistically significant difference in each
parameter between the groups of data (P<0.05). Percutaneous
pedicle screw osteosynthesis is characterized by not only a simple
operation, a shorter operation time and less bleeding but also a
strong fixation. In addition, it allows patients to get out of bed
early, which helps avoiding multiple complications caused by a
long-term bed rest, which is conducive to the early functional
rehabilitation training of patients.
The body produces a special form of trauma-stress
response during the process of surgery, which can cause local
injury and organ dysfunction; thus, surgeons try to reduce the
trauma of surgery. Currently, TNF-α, IL-6 and other cytokines, as
well as CRP and CK, are the main indicators in the evaluation of
trauma stress. Early in the 1930s, C-reactive protein (CRP) was
discovered as a type of protein that can react with the
pneumococcal capsular component C polysaccharide. The serum CRP
concentration is relatively low in the normal human body, however,
in inflammation, burns, surgery, trauma and other stress states,
the CRP concentration can be increased within 6 h after tissue
trauma, reaching a peak in one to three days (15,16),
which is 2,000 times higher than the normal physiological value. As
a specific stress marker, CRP is one of the most sensitive acute
phase proteins produced by the stress response. The change in serum
CRP concentration is positively correlated to the degree of
surgical trauma, which is a relatively sensitive item that reflects
the degree of tissue injury (17).
None of the patients in this study showed signs of infection, which
suggests that the elevated serum CRP was mainly caused by surgical
trauma stress. The post-operative serum CRP levels of both groups
were higher compared to the pre-operation (P<0.05), which was
more significant in the TOPSO group (P<0.05). The CK content is
most abundant in skeletal muscle, which is also found in the
myocardium, brain and other tissues.
Generally, it is difficult for creatine kinase to
pass through the cell membrane, and if it is released into the
blood then there is the possibility that the cell membrane is
damaged. The concentration of creatine kinase, which is low in
normal human blood circulation, is released into the blood in the
case that muscle cell membrane is injured and cell permeability is
increased by mechanical agents such as ischemia, hypoxia and other
factors. The increase in creatine kinase activity in serum is
correlated with the degree of muscle stripping, the range and the
time. Thus, creatine kinase is a better indicator in the assessment
of muscle injury (18–24). Our results demonstrate that creatine
kinase activities post-operation in both groups were significantly
higher than those pre-operation (P<0.05). In addition, the serum
creatine kinase activities were higher in the TOPSO group than the
MIPPSO group at post-operative 24 and 48 h, suggesting that
minimally invasive surgery could relieve the degree of
post-operative pain of waist and back via a reduction in the trauma
to paravertebral muscle, which has obtained an ideal clinical
effect.
In conclusion, the effect of minimally invasive
percutaneous pedicle screws osteosynthesis is similar to that of
the traditional open surgery. However, the technique of MIPPSO has
the advantages of small trauma, less bleeding, short duration of
operation, rapid post-operative recovery, light pain, less economic
cost, and better aesthetic effect, and is therefore worthy of
clinical promotion.
References
|
1
|
Zairi F, Aboukais R, Marinho P, Allaoui M
and Assaker R: Minimally invasive percutaneous stabilization plus
balloon kyphoplasty for the treatment of type A thoraco lumbar
spine fractures: Minimum 4 year's follow-up. J Neurosurg Sci.
58:169–175. 2014.PubMed/NCBI
|
|
2
|
Alizadeh M, Kadir MR, Fadhli MM,
Fallahiarezoodar A, Azmi B, Murali MR and Kamarul T: The use of
X-shaped cross-link in posterior spinal constructs improves
stability in thoracolumbar burst fracture: A finite element
analysis. J Orthop Res. 31:1447–1454. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim DY, Lee SH, Chung SK and Lee HY:
Comparison of multifidus muscle atrophy and trunk extension muscle
strength: Percutaneous versus open pedicle screw fixation. Spine.
30:123–129. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Magerl F: External skeletal fixation of
the lower thoracic and the lumbar spineCurrent Concepts of External
Fixation of Fractuers. Unthoff HK and Stahl E: Spring Verlag; New
York, NY: pp. 353–366. 1982, View Article : Google Scholar
|
|
5
|
Grossbach AJ, Dahdaleh NS, Abel TJ, Woods
GD, Dlouhy BJ and Hitchon PW: Flexion-distraction injuries of the
thoracolumbar spine: Open fusion versus percutaneous pedicle screw
fixation. Neurosurg Focus. 35:E22013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Huskisson EC: Measurement of pain. Lancet.
2:1127–1131. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huang QS, Chi YL, Wang XY, Mao FM, Lin Y,
Ni WF and Xu HZ: Comparative percutaneous with open pedicle screw
fixation in the treatment of thoracolumbar burst fractures without
neurological deficit. Zhonghua Wai Ke Za Zhi. 46:112–114. 2008.(In
Chinese). PubMed/NCBI
|
|
8
|
Smith HE, Anderson DG, Vaccaro AR, Albert
TJ, Hilibrand AS, Harrop JS and Ratliff JK: Anatomy, biomechanics,
and classification of thoracolumbar injuries. Semin Spine Surg.
22:2–7. 2010. View Article : Google Scholar
|
|
9
|
Gu Y, Zhang F, Jiang X, Jia L and McGuire
R: Minimally invasive pedicle screw fixation combined with
percutaneous vertebroplasty in the surgical treatment of
thoracolumbar osteoporosis fracture. J Neurosurg Spine. 18:634–640.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gu YT, Zhu DH, Liu HF, Zhang F and McGuire
R: Minimally invasive pedicle screw fixation combined with
percutaneous vertebroplasty for preventing secondary fracture after
vertebroplasty. J Orthop Surg. 10:312015. View Article : Google Scholar
|
|
11
|
Park HY, Lee SH, Park SJ, Kim ES, Lee CS
and Eoh W: Minimally invasive option using percutaneous pedicle
screw for instability of metastasis involving thoracolumbar and
lumbar spine : A case series in a single center. J Korean Neurosurg
Soc. 57:100–107. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Palmisani M, Gasbarrini A, Brodano GB, De
Iure F, Cappuccio M, Boriani L, Amendola L and Boriani S: Minimally
invasive percutaneous fixation in the treatment of thoracic and
lumbar spine fractures. Eur Spine J. 18 Suppl 1:71–74. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gaines RW Jr: The use of pedicle-screw
internal fixation for the operative treatment of spinal disorders.
J Bone Joint Surg Am. 82:1458–1476. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ni WF, Huang YX, Chi YL, Xu HZ, Lin Y,
Wang XY, Huang QS and Mao FM: Percutaneous pedicle screw fixation
for neurologic intact thoracolumbar burst fractures. J Spinal
Disord Tech. 23:530–537. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hildebrand F, Pape HC and Krettek C: The
importance of cytokines in the posttraumatic inflammatory reaction.
Unfallchirurg. 108:793–794, 796–803. 2005.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Baez Laporta Y, Rodriguez Palomero MA, De
Vicente Sánchez JC, Carretero Sanabria P, Al Kassam Martínez D,
Ferrer Pérez A, Villoria Muriel C and Rodríguez Gilsanz F:
C-reactive protein in the diagnosis of postoperative infection in
pediatric patients: A prospective observational study of 103
patients. J Pediatr Surg. 46:1726–1731. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kragsbjerg P, Holmberg H and Vikerfors T:
Serum concentrations of interleukin-6, tumour necrosis
factor-alpha, and C-reactive protein in patients undergoing major
operations. Eur J Surg. 161:17–22. 1995.PubMed/NCBI
|
|
18
|
Pokora I, Kempa K, Chrapusta SJ and
Langfort J: Effects of downhill and uphill exercises of equivalent
submaximal intensities on selected blood cytokine levels and blood
creatine kinase activity. Biol Sport. 31:173–178. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bagai A, Schulte PJ, Granger CB, Mahaffey
KW, Christenson RH, Bell G, Lopes RD, Green CL, Lincoff AM,
Armstrong PW, et al: Prognostic implications of creatine kinase-MB
measurements in ST-segment elevation myocardial infarction patients
treated with primary percutaneous coronary intervention. Am Heart
J. 168:503–511. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim S, Um TH, Cho CR and Jeon JS:
False-positive elevation of creatine kinase MB mass concentrations
caused by macromolecules in a patient who underwent nephrectomy for
renal cell carcinoma. Ann Lab Med. 34:405–407. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nnadi E, Manafa P, Okocha E, Chukwuma G
and Aneke J: Evaluation of creatine kinase activity and inorganic
phosphate concentration in adult nigerian homozygous and
heterozygous hemoglobin phenotypes. Ann Med Health Sci Res.
4:697–700. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Johnsen SH, Lilleng H and Bekkelund SI:
Creatine kinase as predictor of blood pressure and hypertension. Is
it all about body mass index? A follow-up study of 250 patients. J
Clin Hypertens (Greenwich). 16:820–826. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Laoutidis ZG and Kioulos KT:
Antipsychotic-induced elevation of creatine kinase: A systematic
review of the literature and recommendations for the clinical
practice. Psychopharmacology (Berl). 231:4255–4270. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Behringer M, Montag J, Kilian Y, Mccourt M
and Mester J: The repeated bout effect: Is the blunted creatine
kinase response an effect of an altered enzyme inactivation
kinetic? J Sports Med Phys Fitness. 55:1431–1437. 2015.PubMed/NCBI
|