Introduction
Ischemic heart disease is a major cause of mortality
and disability globally. According to the World Health
Organization, it is predicted to become the primary global cause of
mortality by the year 2020 (1). It
accounts for 1.4 million cases of mortality in developed countries
and 5.7 million in developing countries (2). Many risk factors, including smoking,
obesity, hypertension, hyperlipidemia and hyperglycemia, may induce
ischemic heart disease, which subsequently lead to congestive heart
failure, myocardial infarction and even cardiac arrest (3,4). Timely
reperfusion is currently the most effective method of treating
ischemic heart disease (5). However,
abrupt reperfusion causes ischemia/reperfusion (I/R) injury
(6). Apoptosis serves an important
role in the progression of myocardial I/R injury (7,8) and it
has been demonstrated that the mitochondria are the center of
regulation for apoptosis (9,10). As the primary apoptotic pathway, the
mitochondria-induced intrinsic pathway is initiated by I/R and
increases the size of mitochondrial permeability transition pores
(MPTP), which in turn induces the release of apoptogenic factors
and activation of the downstream apoptotic cascade reaction
(11).
Penehyclidine hydrochloride (PHC) may be used during
surgery; however, it has also recently been identified as a new
type of anticholinergic drug (12).
PHC selectively acts on nicotinic and muscarinic (muscarinic 1 and
muscarinic 3 subtypes) receptors, which induces anticholinergic
effects (13). The major benefit of
PHC compared with other anticholinergic drugs is that it does not
cause muscarinic 2 receptor-associated cardiovascular side effects
(14). PHC stabilizes the heart rate
without autonomic nervous modulation (15). Our previous study demonstrated that
PHC pre-treatment reduces myocardial apoptosis in rat hearts in
vivo (16); however, its
mechanism of action remains unclear. Furthermore, ischemic heart
disease is unpredictable in most cases; thus, post-conditioning
treatment is clinically more significant than pre-conditioning
treatment. Therefore, the present study aimed to investigate the
effects of PHC post-conditioning on myocardial cell apoptosis in a
rat model of myocardial I/R and to determine whether the
mitochondrial-induced pathway is involved.
Materials and methods
Animal model
The present study was approved by the Ethics
Committee of Capital Medical University (Beijing, China). The rats
were cared for following the National Institutes of Health Guide
for the Care and Use of Laboratory animals (17). A total of 24 8-week old Wistar rats
(male; 220–250 g) were provided by Beijing Vital River Laboratory
Animal Technology Co., Ltd. (Beijing, China). Rats had free access
to food and water and were housed in standard cages (22°C, 50%
humidity, 12:12 h light/dark cycle). An animal model was induced
following a previously described protocol (16). All rats were anesthetized by
intraperitoneal injection of 10% chloral hydrate (300 mg/kg; Yulong
Algae Co., Ltd., Qingdao, China). Following thoracotomy, the rat
heart was exposed. Myocardial I/R was induced by occlusion of the
left anterior descending coronary artery and the coronary artery
was subjected to 30 min ischemia followed by 3 h reperfusion. Rats
in the sham operation group underwent the same procedure with no
ligation. Rats were subsequently euthanized by injection of
potassium chloride at the end of the experiment.
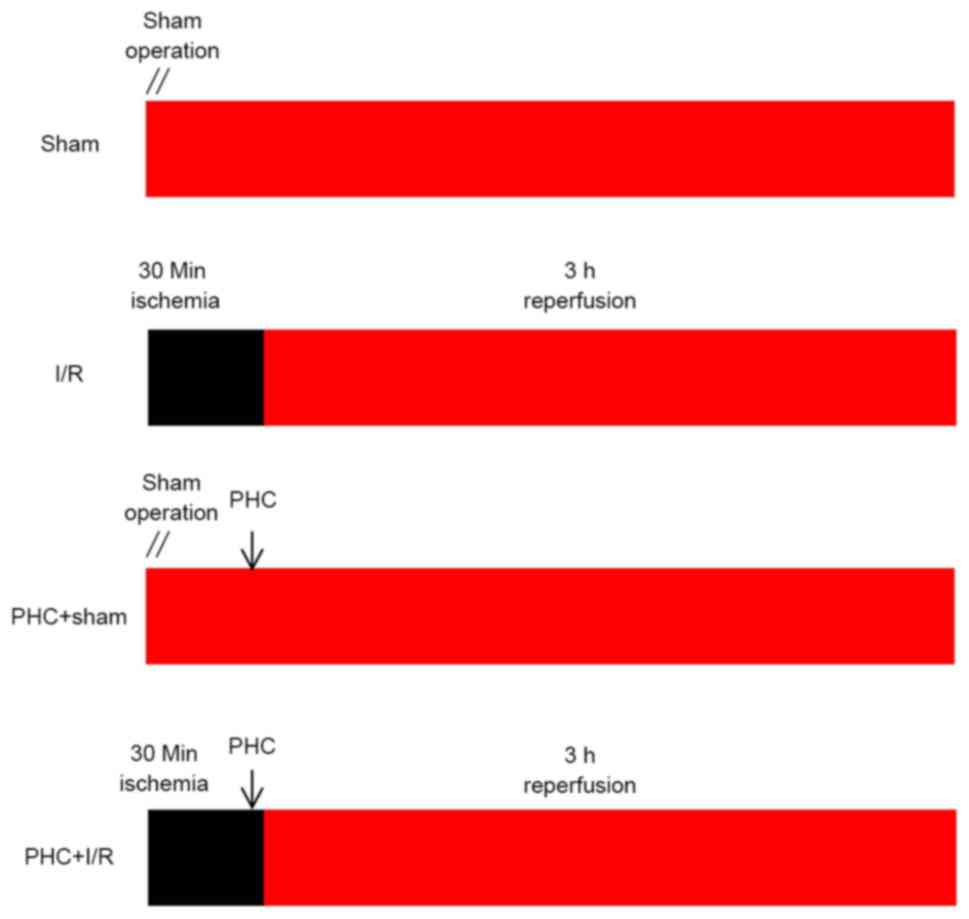
Experimental design
PHC injections were obtained from Chengdu List
Pharmaceutical Co., Ltd. (Chengdu, China). They were sealed for
preservation and stored in cool, dry place (20°C). PHC was prepared
immediately prior to the start of the experiment. PHC (1 mg/ml) was
diluted in normal saline. The 24 healthy male Wistar rats were
randomly and evenly categorized into 4 experimental groups as
follows: i) Sham group consisting of rats undergoing sham surgery;
ii) I/R group consisting of rats subjected to 30 min myocardial
ischemia followed by 3 h reperfusion; iii) PHC+sham group
consisting of rats injected with PHC (1 mg/kg) via the tail vein,
25 min following sham surgery; and iv) PHC+I/R group consisting of
rats subjected to 30 min myocardial ischemia, treated with PHC (1
mg/kg) via the tail vein 25 min following ischemia and then
undergoing 3 h reperfusion. The experimental design is presented in
Fig. 1.
Flow cytometry
Apoptotic cells were analyzed by flow cytometry, as
previously described (18).
Following 3 h reperfusion, rat hearts were removed and myocardial
tissue sections from frozen samples were shredded, digested and
washed. The myocardial tissue was centrifuged for 10 min at 160 × g
at 4°C and the precipitate was collected. The precipitate was
washed twice with PBS and centrifuged for 10 min at 160 × g at 4°C.
The precipitate was then resuspended in binding buffer containing 5
µl Annexin V-fluorescein isothiocyanate (FITC; BD Biosciences,
Franklin Lakes, NJ, USA) and 5 µl propidium iodide staining
solution (BD Biosciences). The solution was incubated for 15 min at
37°C in the dark. Apoptosis (%) was quantified using the Annexin
V-FITC and propidium iodide apoptosis detection kit (BD
Biosciences) by flow cytometry as previously described (BD
Biosciences) (18). The result was
analyzed with CellQuest Pro software version 5.2 (BD
Biosciences).
Terminal
deoxynucleotidyltransferase-mediated dUTP nick end labelling
(TUNEL) staining
TUNEL staining was used to measure the rate of
apoptosis, as previously described (16). Following 3 h reperfusion, rat hearts
were removed. Myocardial tissue sections were dehydrated in
ascending series of ethanol, cleared in xylene and embedded in
paraffin. Paraffin-embedded myocardial tissues were cut into
sections 5-µm thick, dewaxed with xylene and stained for TUNEL
analysis. Sections were penetrated for 8 min with 0.1% Triton X-100
(50 µl; Beyotime Institute of Biotechnology, Haimen, China) and
washed 3 times for 5 min each in PBS at 37°C. Sections were then
blocked for 10 min by 3% H2O2 and washed 3
times for 5 min each in PBS at 37°C. TUNEL reaction mixture was
added to the sections, which were then incubated for 60 min at 37°C
in a dark in a humidified environment. Sections were washed 3 times
in PBS for 5 min each at 37°C. Converter-POD (50 µl; Roche
Diagnostics, Basel, Switzerland) was added to the sections and
incubated for 30 min in a humid environment at 37°C. Sections were
washed 3 times for 5 min each in PBS at 37°C. Sections were
incubated with DAB substrate for 10 min at 15°C and washed 3 times
for 5 min each in PBS at 37°C. Finally, sections were stained by
hematoxylin for 3 min at 37°C and fixed by neutral balata.
TUNEL-positive cells were counted using a fluorescent microscope
(Olympus, Tokyo, Japan) at a magnification of ×400.
JC-1 staining
Following 3 h reperfusion, rat hearts were removed
and myocardial tissue sections were shredded, centrifuged and
stained using the JC-1 staining method, as previously described
(19). Myocardial tissue sections
were homogenized in mitochondrial isolation buffer and centrifuged
at 1,000 × g for 5 min at 4°C. The supernatant was centrifuged at
11,000 × g for 10 min at 4°C and the precipitate was collected. The
precipitate was resuspended in JC-1 solution (×200 JC-1 stock
solution, X5 JC-1 staining buffer, ddH2O; Keygenbio,
Nanjing, China) and incubated for 20 min at 37°C. A Lumat LB9507
chemic luminous instrument (Berthold Technologies, Bad Wildbad,
Germany) was used to detect the absorbency of the samples. The
ratio of red/green absorbency represents mitochondrial membrane
potential (MMP).
Western blot analysis
Following 3 h reperfusion, rat hearts were removed.
Apoptosis-related proteins were extracted and measured using
western blot analysis, as previously described (20). Bax, Bcl-2 cytosol cytochrome c
(cyt-c) and cleaved caspase-3 proteins were extracted by
using a cytosol extraction kit (Wanleibio Co., Ltd., Shanghai,
China). Voltage-dependent anion-selective channel protein 1 (VDAC1)
protein was extracted by using a mitochondria extraction kit
(Wanleibio Co., Ltd.). The expression of Bax, Bcl-2, VDAC1, cyt-c
and cleaved caspase-3 was measured using a BCA Protein assay kit
(Beyotime Institute of Biotechnology). The proteins (40 µg) were
separated by 12% SDS-PAGE and transferred onto polyvinylidene
fluoride membranes. Following blocking with 5% non-fat milk for 1 h
and washing with TTBS (150 mM NaCl, 20 mM Tris, 0.1% Tween-20, pH
7.6) for 5 min, membranes were incubated with specific Bcl-2
antibody (1:500; cat. no/WL01556), Bax antibody (1:500; cat. no.
WL01637; both from Wanleibio Co., Ltd.), VDAC1 antibody (1:500,
cat. no. bs-1461R; Bioss, Beijing, China), β-actin antibody
(1:1,000, WL01845), COX IV (1:500, WL01794) or cyt-c
antibody (1:500, WL01571) (all from Wanleibio Co., Ltd.) overnight
at 4°C and then with goat anti-rabbit immunoglobulin G conjugated
to horseradish peroxidase (1:5,000, cat. no. WLA023a; Wanleibio
Co., Ltd.) for 45 min at 37°C. An ECL western blotting detection
system (Wanleibio Co., Ltd.) was used to determine protein bands.
Image software GeneTools 4.3.7 (Syngene, Frederick, MD, USA) was
used to quantify the band intensities. The band densities were
normalized to β-actin or COX IV.
Statistical analysis
The results were obtained from 6 different samples
and all data were expressed as the mean ± standard deviation. SPSS
13.0 (SPSS, Inc., Chicago, IL, USA) was used for analysis. The
differences between data were evaluated using a two-way analysis of
variance followed by Bonferroni post hoc testing. P<0.05 was
considered to indicate a statistically significant difference.
Results
Effect of PHC on cardiomyocyte
apoptosis
Following 3 h reperfusion, apoptotic cells were
analyzed using flow cytometry (Fig.
2A). There was a decreased proportion of apoptotic cells in the
PHC+sham group compared with the Sham group; however, this
difference was not significant (5.52±2.32% vs. 6.20±2.93%). The
proportion of apoptotic cells in the I/R group was significantly
increased compared with the Sham group (25.12±5.92% vs. 6.20±2.93%)
and significantly decreased in the PHC+I/R group compared with the
I/R group (7.35±3.42% vs. 25.12±5.92%, both P<0.001; all
Fig. 2A).
 | Figure 2.Effect of PHC on cardiomyocyte
apoptosis. (A) Representative images of flow cytometry. Cell
populations were regarded, respectively, as early-stage apoptotic
in the LR quadrant, living in the LL quadrant, late-stage apoptotic
in the UR quadrant and necrotic in the UL quadrant. (B)
Representative images of myocardial TUNEL staining. TUNEL-positive
cells were regarded as apoptotic and counted using a microscope at
×400 magnification. Cells in the nucleus contained brown granules
suggesting positive staining and are indicated by red arrows.
Normal cell nuclei were stained blue with hematoxylin. (C) The
cardiomyocyte apoptotic rate was expressed as a ratio of
TUNEL-positive cells (apoptotic cells) to the total number of
cardiomyocytes. Data were expressed as the mean ± standard
deviation (n=6 each group). Scale bar, 20 µm.
##P<0.01 vs. sham; **P<0.01 vs. I/R. ns, not
significant (P>0.05); I/R, ischemia/reperfusion; PHC,
penehyclidine hydrochloride; TUNEL, terminal
deoxynucleotidyltransferase-mediated dUTP nick end labelling; LL,
lower left; UL, upper left; LR, lower right; UR, upper right; FITC,
fluorescein isothiocyanate. |
Following 3 h reperfusion, TUNEL staining was
performed (Fig. 2B) to measure the
rate of apoptosis as the proportion of apoptotic cells in the
sample. The difference in the apoptotic rate of cardiomyocytes in
the PHC+sham group compared with the Sham group was not significant
(3.62±1.5% vs. 2.95±1.4%; Fig. 2C).
The apoptotic rate was significantly increased in the I/R group
compared with the Sham group (58.09±6.2% vs. 2.95±1.4%) and
significantly decreased in the PHC+I/R group compared with the I/R
group (15.84±2.6% vs. 58.09±6.2%, both P<0.01; Fig. 2C).
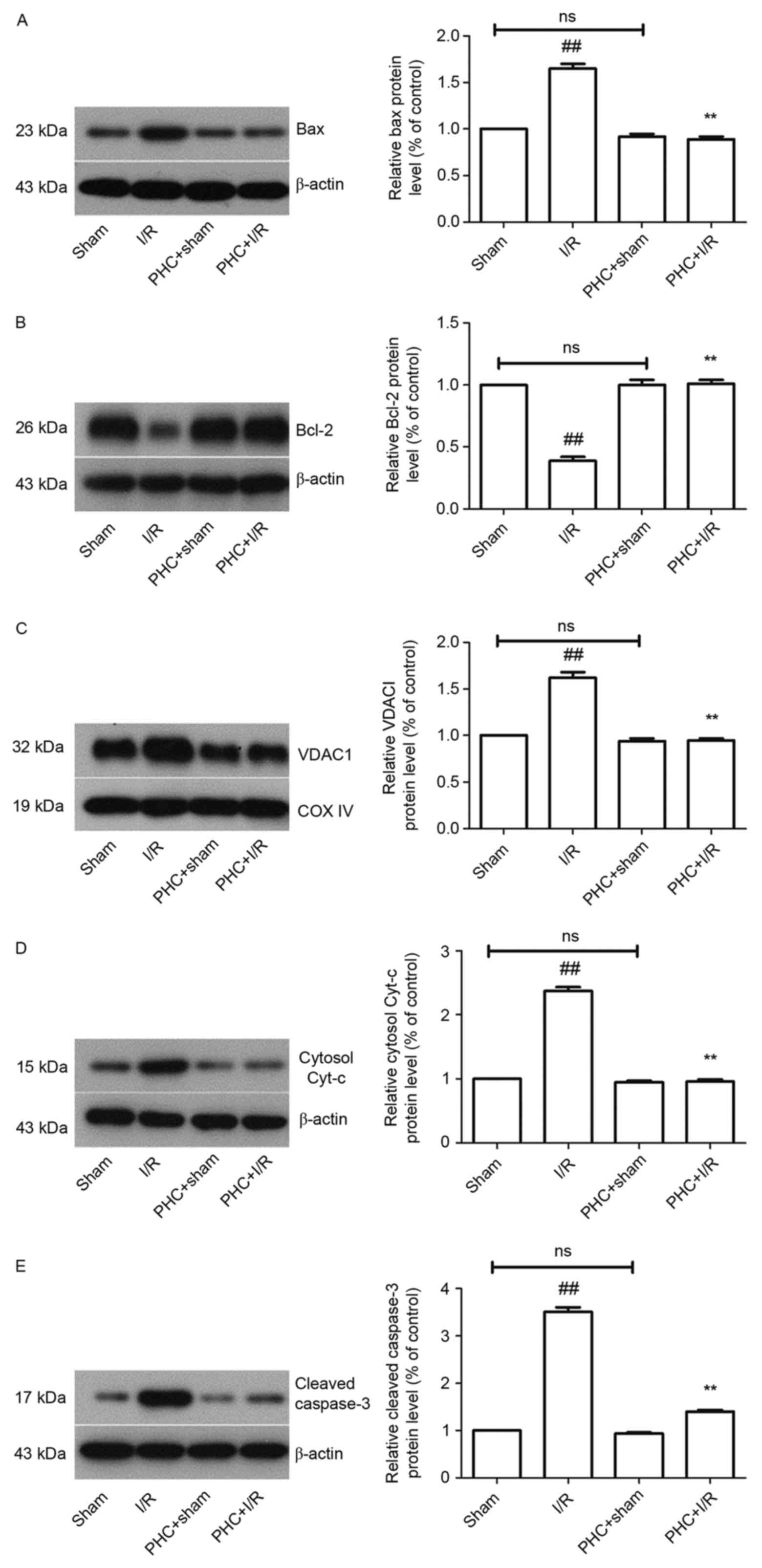
Effect of PHC on the expression of
apoptotic regulatory proteins
The expression of the apoptotic regulatory proteins
Bax and Bcl-2 following 3 h reperfusion was measured using western
blotting (Fig. 3A and B). The
difference in the expression of Bax (0.92±0.03 vs. 1.00; Fig. 3A) and Bcl-2 (1.0±0.04 vs. 1.00;
Fig. 3B) in the PHC+sham group
compared with the Sham group were not significant. The expression
of Bax was significantly increased in the I/R group compared with
sham group (1.65±0.05 vs. 1.00) and significantly decreased in the
PHC+I/R group compared with the I/R group (0.89±0.03 vs. 1.65±0.05,
both P<0.01; Fig. 3A). The
expression of Bcl-2 was significantly decreased in the I/R group
compared with the Sham group (0.39±0.03 vs. 1.00) and significantly
increased in the PHC+I/R group compared with the I/R group
(1.01±0.03 vs. 0.39±0.03, both P<0.01; both Fig. 3B).
Effect of PHC treatment on
apoptosis-related protein expression
The expression of the apoptosis-related proteins
VDAC1, cytosol cyt-c and cleaved caspase-3 was measured
using western blotting following 3 h reperfusion.
The difference between the expression of VDAC1 in
the PHC+sham group and the sham group was not significant
(0.94±0.03 vs. 1.00). The expression of VDAC1 was significantly
increased in the I/R group compared with the sham group (1.62±0.06
vs. 1.00) and significantly decreased in the PHC+I/R group compared
with the I/R group (0.95±0.02 vs. 1.62±0.06, both P<0.01;
Fig. 3C).
The difference between the expression of cytosol
cyt-c in the PHC+sham group and the sham group was not
significant (0.95±0.02 vs. 1.00). The expression of cytosol
cyt-c was significantly increased in the I/R group compared
with the Sham group (2.37±0.06 vs. 1.00) and significantly
decreased in the PHC+I/R group compared with the I/R group
(0.96±0.03 vs. 2.37±0.06, both P<0.01; Fig. 3D).
The difference between the expression of cleaved
caspase-3 in the PHC+sham group and the Sham group was not
significant (0.94±0.02 vs. 1.00). The expression of cleaved
caspase-3 was significantly increased in the I/R group compared
with the sham group (3.51±0.1 vs. 1.00) and significantly decreased
in the PHC+I/R group compared with the I/R group (1.40±0.03 vs.
3.51±0.1, both P<0.01; all Fig.
3E).
Effect of PHC treatment on MMP
The cellular MMP was measured using a JC-1 staining
method following 3 h reperfusion. The difference in MMP (0.99±0.03
vs. 1.00±0.03) between the PHC+sham group and the Sham group was
not significant. The I/R group exhibited a significantly decreased
MMP compared with the sham group, (0.36±0.01 vs. 1.00±0.03) and MMP
was significantly increased in the PHC+I/R group compared with the
I/R group (0.73±0.08 vs. 0.36±0.01, both P<0.01; all Fig. 4).
Discussion
During the course of reperfusion therapy in ischemic
heart disease, there may be a rapid and severe onset of I/R injury.
Thus, the focus of current studies in the field is to identify
therapies that attenuate myocardial I/R injury.
The pathogenesis of I/R injury includes oxidative
stress, cellular apoptosis, Ca2+ overload and an
inflammatory response (21).
Previous studies have demonstrated that myocardial apoptosis serves
an important role in I/R injury (22–24).
Apoptosis leads to a reduction in myocardial cells and cardiac
function (25). Therapeutic
strategies that inhibit the apoptosis of myocardial cells attenuate
I/R injury (26). There are a number
of apoptotic pathways, including the mitochondria-induced intrinsic
pathway, the death receptor-induced extrinsic pathway and the
endoplasmic reticulum stress-induced pathway (27–29). The
initiation of the mitochondria-induced intrinsic pathway by
pro-apoptotic signaling leads to the opening of MPTP, the release
of apoptogenic factors and the activation of the apoptotic cascade
reaction (11). Yu et al
(30) demonstrated that PHC
attenuates apoptosis in focal cerebral I/R and exhibits a
neuroprotective effect. Lin et al (16) indicated that pretreatment with PHC
reduces myocardial apoptosis in rat hearts in vivo. The
results of the aforementioned studies demonstrate that I/R induces
cell apoptosis, whereas PHC reduces cell apoptosis. Central
components of the mitochondria-induced intrinsic pathway include
Bcl-2 family members, MMP, MPTP, apoptogenic factor and caspase
family members (9,11,31). The
proportion of apoptotic cells, the apoptotic rate, the expression
of apoptotic regulatory proteins Bax and Bcl-2, MMP, expression of
MPTP via VDAC1, expression of the apoptogenic factor cytosol
cyt-c and expression of the caspase family member cleaved
caspase-3 were examined in the present study to determine whether
PHC post-conditioning inhibits myocardial apoptosis via the
mitochondria-induced intrinsic pathway. The present study
demonstrated that rats undergoing I/R exhibit significantly
increased numbers of apoptotic cardiomyocytes and an increased
apoptotic rate, whereas PHC post-conditioning significantly
decreased the number of apoptotic cardiomyocytes and the apoptotic
rate. Thus, the results of the present study are consistent with
the results of studies conducted by Yu et al (30) and Lin et al (16), as it was demonstrated that PHC
treatment attenuates I/R injury by inhibiting apoptosis.
Furthermore, the present study indicated that PHC post-conditioning
effectively protects rats against I/R-induced myocardial apoptosis.
The application of post-conditioning has more clinical significance
than preconditioning, as ischemic heart disease is unpredictable in
most cases (32).
The Bcl-2 family proteins pro-apoptotic Bax and
anti-apoptotic Bcl-2 serve a key role in regulating the
mitochondrial apoptotic process (33). It has been demonstrated that the
balance between Bax and Bcl-2 is associated with apoptotic
suppression or activation (34). Bax
increases the size of MPTPs, whereas Bcl-2 decreases the size of
MPTPs during apoptosis (35). The
present study demonstrated that I/R significantly increased the
expression of Bax but significantly decreased the expression of
Bcl-2. Following treatment with PHC, the expression of Bax was
significantly decreased, while the expression of Bcl-2 was
significantly increased. These results indicate that PHC
post-conditioning protects against I/R injury by regulating the
balance between Bax and Bcl-2.
The MMP mediates mitochondrial activity and cellular
survival (36) and I/R disrupts the
MMP, which induces myocardial apoptosis (37). A decrease in the MMP is characterized
as a key factor in the activation of apoptotic pathways. The
present study demonstrated that myocardial I/R injury was
accompanied by a decrease in the MMP. Treatment with PHC leads to a
partial but significant recovery of the MMP. Thus, the results
indicate that PHC post-conditioning maintains the MMP, which
attenuates I/R-induced myocardial apoptosis.
MPTPs are complex protein channels in the inner
mitochondrial membrane and their opening leads to a decrease in the
MMP and the onset of mitochondrial swelling (38). VDAC is an important component of
MPTPs located in the mitochondrial outer membrane (39). VDAC1 is the major form of VDAC and is
a gatekeeper in MPTPs, and its expression serves an important role
in mediating mitochondrial apoptosis (40). It has been previously demonstrated
that an increase in VDAC1 expression leads to an increase in
mitochondria membrane permeability (40). The present study demonstrated that
there was a significant increase in VDAC1 expression following I/R,
whereas PHC post-conditioning significantly decreased the
expression of VDAC1. These results indicate that PHC may stabilize
the mitochondrial membrane, inhibit the opening of MPTPs and
protect mitochondrial activity against I/R-induced cardiomyocyte
apoptosis.
The mitochondrial apoptogenic factor cyt-c is
released from the mitochondrial inter-membrane space into the
cytosol during reperfusion and induces the apoptotic process
(41). Cytosol cyt-c combines
with other apoptosis factors to form an apotosome, thus triggering
a further apoptotic cascade (42).
The present study demonstrated that I/R significantly increased the
expression of cytosol cyt-c protein, whereas PHC
post-conditioning significantly decreased the expression of cytosol
cyt-c protein. These results indicate that PHC
post-conditioning protects against cardiomyocyte apoptosis by
inhibiting the release of cyt-c from the mitochondria into
the cytosol.
Caspase-3 exhibits a high propensity and catalytic
turnover to cleave substrates and is therefore a key executioner
protease (43). Cleaved caspase-3
induces irreversible and intense apoptosis (44). The present study demonstrated that
I/R significantly increased levels of cleaved caspase-3, whereas
PHC post-conditioning significantly decreased cleaved caspase-3
levels in the cytosol. These results indicate that PHC
post-conditioning decreases I/R-induced apoptosis by attenuating
the activation of caspase-3.
In conclusion, the present study demonstrated that
PHC post-conditioning protects cardiomyocytes against apoptosis in
a rat model of myocardial I/R. PHC served an important role in
inhibiting myocardial apoptosis through the mitochondria-induced
intrinsic pathway. Its anti-apoptotic mechanisms consist of
suppressing of Bax expression, activating Bcl-2, promoting the
recovery of MMP and inhibiting VDAC1, cytosol cyt-c and
cleaved caspase-3 in myocardial I/R. The present study indicated
that a PHC post-conditioning approach may be developed as a novel
therapeutic strategy for treating I/R-induced myocardial apoptosis.
However, the anti-apoptotic mechanism of action of PHC
post-conditioning remains unclear and requires further study.
Acknowledgements
The present study was supported by the National
Nature Science Foundation of China (grant no. 81471902).
References
|
1
|
Ostadal B: The past, the present and the
future of experimental research on myocardial ischemia and
protection. Pharmacol Rep. 61:3–12. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pagidipati NJ and Gaziano TA: Estimating
deaths from cardiovascular disease: A review of global
methodologies of mortality measurement. Circulation. 127:749–756.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Patel AV and Bangalore S: Challenges with
evidence-based management of stable ischemic heart disease. Curr
Cardiol Rep. 19:112017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cordero A, Galve E, Bertomeu-Martinez V,
Bueno H, Fácila L, Alegria E, Cequier Á, Ruiz E and
González-Juanatey JR: Trends in risk factors and treatments in
patients with stable ischemic heart disease seen at cardiology
clinics between 2006 and 2014. Rev Esp Cardiol (Engl Ed).
69:401–407. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chi HJ, Chen ML, Yang XC, Lin XM, Sun H,
Zhao WS, Qi D, Cai J and Dong JL: Progress in therapies for
myocardial ischemia reperfusion injury. Curr Drug Targets. Apr
1–2016.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Barrere-Lemaire S, Nargeot J and Piot C:
Delayed postconditioning: Not too late? Trends Cardiovas Med.
22:173–179. 2012. View Article : Google Scholar
|
|
7
|
Qiao Y, Zhao Y, Liu Y, Ma N, Wang C, Zou
J, Liu Z, Zhou Z, Han D, He J, et al: miR-483-3p regulates
hyperglycaemia-induced cardiomyocyte apoptosis in transgenic mice.
Biochem Biophys Res Commun. 477:541–547. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Eefting F, Rensing B, Wigman J, Pannekoek
WJ, Liu WM, Cramer MJ, Lips DJ and Doevendans PA: Role of apoptosis
in reperfusion injury. Cardiovasc Res. 61:414–426. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Desagher S and Martinou JC: Mitochondria
as the central control point of apoptosis. Trends Cell Biol.
10:369–377. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Teringova E and Tousek P: Apoptosis in
ischemic heart disease. J Transl Med. 15:872017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kroemer G, Galluzzi L and Brenner C:
Mitochondrial membrane permeabilization in cell death. Physiol Rev.
87:99–163. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhan J, Xiao F, Li JJ, Zhang ZZ, Chen K,
Wang YP and Wang YL: Penehyclidine hydrochloride decreases
pulmonary microvascular permeability by upregulating beta arrestins
in a murine cecal ligation and puncture model. J Surg Res.
193:391–398. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang YA, Zhou WX, Li JX, Liu YQ, Yue YJ,
Zheng JQ, Liu KL and Ruan JX: Anticonvulsant effects of
phencynonate hydrochloride and other anticholinergic drugs in soman
poisoning: Neurochemical mechanisms. Life Sci. 78:210–223. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ma TF, Zhou L, Wang Y, Qin SJ, Zhang Y, Hu
B, Yan JZ, Ma X, Zhou CH and Gu SL: A selective M1 and M3 receptor
antagonist, penehyclidine hydrochloride, prevents postischemic LTP:
Involvement of NMDA receptors. Synapse. 67:865–874. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Liu XB, Pan S, Yang XG, Li ZW, Sun QS,
Zhao Z, Ma HC and Cui CR: Effect of penehyclidine hydrochloride on
heart rate variability in hysteroscopy. Exp Ther Med. 10:181–186.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lin D, Ma J, Xue Y and Wang Z:
Penehyclidine hydrochloride preconditioning provides
cardioprotection in a rat model of myocardial Ischemia/Reperfusion
injury. PLoS One. 10:e1380512015. View Article : Google Scholar
|
|
17
|
Research NRCU: Guide for the Care and Use
of Laboratory Animals. National Academies Press (US); Washington
(DC): 1996
|
|
18
|
Li T, Xu XH, Tang ZH, Wang YF, Leung CH,
Ma DL, Chen XP, Wang YT, Chen Y and Lu JJ: Platycodin D induces
apoptosis and triggers ERK- and JNK-mediated autophagy in human
hepatocellular carcinoma BEL-7402 cells. Acta Pharmacol Sin.
36:1503–1513. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Koka S, Das A, Salloum FN and Kukreja RC:
Phosphodiesterase-5 inhibitor tadalafil attenuates oxidative stress
and protects against myocardial ischemia/reperfusion injury in type
2 diabetic mice. Free Radic Biol Med. 60:80–88. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Reifschneider NH, Goto S, Nakamoto H,
Takahashi R, Sugawa M, Dencher NA and Krause F: Defining the
mitochondrial proteomes from five rat organs in a physiologically
significant context using 2D blue-native/SDS-PAGE. J Proteome Res.
5:1117–1132. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sharma V, Bell RM and Yellon DM: Targeting
reperfusion injury in acute myocardial infarction: A review of
reperfusion injury pharmacotherapy. Expert Opin Pharmaco.
13:1153–1175. 2012. View Article : Google Scholar
|
|
22
|
Zhu T, Yao Q, Wang W, Yao H and Chao J:
iNOS induces vascular endothelial cell migration and apoptosis via
autophagy in ischemia/reperfusion injury. Cell Physiol Biochem.
38:1575–1588. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang X, Cao Y, Shen M, Wang B, Zhang W,
Liu Y, He X, Wang L, Xia Y, Ding M, et al: DIDS reduces
ischemia/reperfusion-induced myocardial injury in rats. Cell
Physiol Biochem. 35:676–688. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sima N, Lü W and Xie X: Early proteins E6
and E7 of human papillomavirus may attenuate ischemia-reperfusion
injury. Med Hypotheses. 76:607–609. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhang S, Li G, Fu X, Qi Y, Li M, Lu G, Hu
J, Wang N, Chen Y, Bai Y and Cui M: PDCD5 protects against cardiac
remodeling by regulating autophagy and apoptosis. Biochem Biophys
Res Commun. 461:321–328. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fliss H and Gattinger D: Apoptosis in
ischemic and reperfused rat myocardium. Circ Res. 79:949–956. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Park YJ, Choi C, Chung KH and Kim KH:
Pharbilignan C induces apoptosis through a mitochondria-mediated
intrinsic pathway in human breast cancer cells. Bioorg Med Chem
Lett. 26:4645–4649. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wang J, Wang QL, Nong XH, Zhang XY, Xu XY,
Qi SH and Wang YF: Oxalicumone A, a new dihydrothiophene-condensed
sulfur chromone induces apoptosis in leukemia cells through
endoplasmic reticulum stress pathway. Eur J Pharmacol. 783:47–55.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lee HP, Li TM, Tsao JY, Fong YC and Tang
CH: Curcumin induces cell apoptosis in human chondrosarcoma through
extrinsic death receptor pathway. Int Immunopharmacol. 13:163–169.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yu C and Wang J: Neuroprotective effect of
penehyclidine hydrochloride on focal cerebral ischemia-reperfusion
injury. Neural Regen Res. 8:622–632. 2013.PubMed/NCBI
|
|
31
|
Palchaudhuri R, Lambrecht MJ, Botham RC,
Partlow KC, van Ham TJ, Putt KS, Nguyen LT, Kim SH, Peterson RT,
Fan TM and Hergenrother PJ: A small molecule that induces intrinsic
pathway apoptosis with unparalleled speed. Cell Rep. 13:2027–2036.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Weintraub WS and Boden WE: Reexamining the
efficacy and value of percutaneous coronary intervention for
patients with stable ischemic heart disease. JAMA Intern Med.
176:1190–1194. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Brenner D and Mak TW: Mitochondrial cell
death effectors. Curr Opin Cell Biol. 21:871–877. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Xia A, Xue Z, Li Y, Wang W, Xia J, Wei T,
Cao J and Zhou W: Cardioprotective effect of betulinic Acid on
myocardial ischemia reperfusion injury in rats. Evid Based
Complement Alternat Med. 2014:5737452014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lindsay J, Esposti MD and Gilmore AP:
Bcl-2 proteins and mitochondria-specificity in membrane targeting
for death. Biochim Biophys Acta. 1813:532–539. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lyon AR, Joudrey PJ, Jin D, Nass RD, Aon
MA, O'Rourke B and Akar FG: Optical imaging of mitochondrial
function uncovers actively propagating waves of mitochondrial
membrane potential collapse across intact heart. J Mol Cell
Cardiol. 49:565–575. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kadenbach B, Ramzan R, Moosdorf R and Vogt
S: The role of mitochondrial membrane potential in ischemic heart
failure. Mitochondrion. 11:700–706. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Xiao-Feng L, Wen-Ting Z, Yuan-Yuan X,
Chong-Fa L, Lu Z, Jin-Jun R and Wen-Ya W: Protective role of
6-Hydroxy-1-H-Indazole in an MPTP-induced mouse model of
Parkinson's disease. Eur J Pharmacol. 791:348–354. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Shoshan-Barmatz V and Ben-Hail D: VDAC, a
multi-functional mitochondrial protein as a pharmacological target.
Mitochondrion. 12:24–34. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shoshan-Barmatz V, De Pinto V,
Zweckstetter M, Raviv Z, Keinan N and Arbel N: VDAC, a
multi-functional mitochondrial protein regulating cell life and
death. Mol Aspects Med. 31:227–285. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Marenzi G, Giorgio M, Trinei M, Moltrasio
M, Ravagnani P, Cardinale D, Ciceri F, Cavallero A, Veglia F,
Fiorentini C, et al: Circulating cytochrome c as potential
biomarker of impaired reperfusion in ST-segment elevation acute
myocardial infarction. Am J Cardiol. 106:1443–1449. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Lee HJ, Lee HJ, Lee EO, Ko SG, Bae HS, Kim
CH, Ahn KS, Lu J and Kim SH: Mitochondria-cytochrome
c-caspase-9 cascade mediates isorhamnetin-induced apoptosis.
Cancer Lett. 270:342–353. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Demon D, Van Damme P, Vanden Berghe T,
Deceuninck A, Van Durme J, Verspurten J, Helsens K, Impens F, Wejda
M, Schymkowitz J, et al: Proteome-wide substrate analysis indicates
substrate exclusion as a mechanism to generate caspase-7 versus
caspase-3 specificity. Mol Cell Proteomics. 8:2700–2714. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Cao L, Duanmu W, Yin Y, Zhou Z, Ge H, Chen
T, Tan L, Yu A, Hu R, Fei L and Feng H: Dihydroartemisinin exhibits
anti-glioma stem cell activity through inhibiting p-AKT and
activating caspase-3. Pharmazie. 69:752–758. 2014.PubMed/NCBI
|