Introduction
Deep vein thrombosis (DVT) is a type of venous
thromboembolism disease that is common in the clinic and typically
occurs following surgery for lower extremity bone trauma and other
diseases, including diabetes and gestational hypertension (1,2). The
incidence of DVT is >0.1% and has increased in recent years
(3). The primary pathological
characteristic of lower extremity venous thrombosis is abnormal
blood coagulation in the lower extremity deep vein that obstructs
the lumen and causes venous reflux obstacles (4). Lesions in the limb induce different
degrees of swelling and pain and in some severe cases may cause
limb gangrene. Following the detachment of thrombi, patients may
experience pulmonary embolism and respiratory distress (5,6).
Furthermore, DVT may progress to post-thrombotic syndrome, which
seriously affects patient quality of life and may cause pain
(7).
At present, early diagnosis of DVT is clinically
significant for the treatment and prognosis of patients. The
current gold standard for the clinical diagnosis of DVT is lower
extremity venous imaging. However, this is a type of invasive
examination and increases the risk of complications occurring,
including thrombus detachment, allergic reactions and increased
thrombosis severity, which limits its application in the clinic
(8). Recent studies have
demonstrated that biomarkers including C-reactive protein (CRP),
D-dimer and interleukin (IL)-6, exhibit beneficial clinical value
in the early diagnosis of DVT; however, these biomarkers are still
not a substitute for lower extremity venous imaging (9–11). At
present, the mechanism of DVT is unclear, which greatly limits
screening for DVT diagnostic markers. Therefore, it is important to
determine the mechanism of DVT in order to identify potential
biomarkers.
Micro (mi)RNAs are endogenous, small noncoding RNAs
that are approximately 20–22 nucleotides long and found in
eukaryotes (12). Mature miRNA binds
to the 3′-untranslated (UTR) region of its target mRNA, forming
silencing complexes and inducing the degradation of target mRNA or
inhibiting its translation (13,14).
miRNAs are stable molecules that may be developed as biomarkers for
various diseases and their levels are high in the peripheral blood
(15). In addition, miRNAs are
involved in almost all pathological and physiological processes in
eukaryotic cells, including cancer, cardiovascular disease,
Alzheimer's disease and inflammation (16–18).
In the present study, the diagnosis value of
microRNA (miR)-26a in DVT was assessed. The role and mechanism of
miR-26a in DVT was also analyzed and discussed.
Patients and methods
Patients
A total of 45 patients (27 males and 18 females;
mean age, 53±8.63 years old) who had suffered from bone trauma were
diagnosed with lower extremity DVT between May 2013 and April 2015
at the Xiangya Second Hospital of Central South University
(Xiangya, China) and were enrolled in the present study. All
patients were diagnosed by lower extremity venous imaging (19). Patients had experienced DVT for
between 2 and 15 years. Clinical symptoms included pain and
swelling of the lower limbs and difficulty walking. Among the 45
patients, 6 patients also had pulmonary embolism (PTE). For
comparison, 40 healthy individuals were also enrolled. Peripheral
whole blood was collected from the upper limb veins of 45 patients
and 40 healthy individuals to extract total DNA. Prior written and
informed consent was obtained from all individuals recruited in the
current study and ethical approval was granted by the Ethics Review
Board of Central South University.
Cell culture and reagents
Human umbilical vein endothelial cells (HUVECs)
(Sciencell Research Laboratories, Inc., San Diego, CA, USA) were
maintained in RPMI 1640 medium supplemented with 10% fetal bovine
serum (FBS) (BD Biosciences, Franklin Lakes, NJ, USA) and cultured
at 37°C in an atmosphere containing 0.5% CO2. TRIzol LS
reagent and Lipofectamine 2000 transfection reagent were purchased
from Invitrogen; Thermo Fisher Scientific, Inc. (Waltham, MA, USA).
Mouse anti-human GAPDH monoclonal antibody (AG019) and enhanced
chemiluminescence substrate were purchased from Beyotime Institute
of Biotechnology (Shanghai, China). Rabbit anti-human protein
kinase C δ (PRKCD) polyclonal antibody (ab86800) and rabbit
anti-nuclear factor (NF)-κB polyclonal antibody (ab16502) were
purchased from Abcam (Cambridge, UK). The Takara PrimeScript RT and
Regent SYBR PrimeScript RT-PCR kits were purchased from Takara
Biotechnology Co., Ltd. (Dalian, China).
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA from whole blood cells was extracted using
TRIzol LS reagent. Reverse transcription was performed using a
Takara PrimeScript RT kit according to the manufacturer's
instructions. qPCR was performed to measure the levels of miR-26a,
CCL2 mRNA and CCL7 mRNA and the Regent SYBR PrimeScript RT-PCR kit
was used to perform qPCR following the manufacturer's instructions.
U6 was used as a reference gene for miR-26a and GAPDH was used as a
reference gene for CCL2 and CCL7. Primer sequences are listed in
Table I. The reaction system
consisted of the following: cDNA (2 µl), Buffer Mix (containing
enzymes, 10 µl), forward primer (0.5 µl), reverse primer (0.5 µl)
and 17 µl H2O. To detect miR-26a, CCL2 and CCL7, PCR was
performed under the following cycling conditions: 95°C for 10 min,
followed by 40 cycles of denaturing at 95°C for 30 sec and primer
annealing at 60°C for 30 sec. Levels of miR-26a, CCL2 mRNA and CCL7
mRNA were calculated using the 2−ΔΔCq method (20).
 | Table I.Primers used in reverse
transcription-quantitative polymerase chain reaction. |
Table I.
Primers used in reverse
transcription-quantitative polymerase chain reaction.
| Primer | Direction | Primer sequences
(5′-3′) |
|---|
| miR-26a | Forward |
CAAGUAAUCCAGGAUAGG |
|
| Reverse |
GGCCAACCGCGAGAAGATGTTTTTTTTT |
| CCL2 | Forward | CCA
ACTCCTGCCTCCGCTCTA |
|
| Reverse |
TGCAGATCTGGGTTGTGGAG |
| CCL7 | Forward |
CTGACCCCACACAGAAGTGG |
|
| Reverse |
CCCCATGAGGTAGAGAAGGGA |
| U6 | Forward |
CTCGCTTCGGCAGCACA |
|
| Reverse |
AACGCTTCACGAATTTGCGT |
| GAPDH | Forward |
CGGAGTCAACGGATTTGGTCGTAT |
|
| Reverse |
AGCCTTCTCCATGGTGGTGAAGAC |
Transfection in HUVECs
HUVECs were seeded in 24-well plates at a density of
2×105 cells/well 24 h at 37°C prior to transfection.
Cells were transfected with 0.5 µg of GV227-PRKCD-Neo-EGFP and 25
pmol of miR-26a mimics (Hanbio, Shanghai, China). Transfection was
performed using Lipofectamine 2000 according to the manufacturer's
instructions and cells were harvested 48 h later.
PRKCD small interfering (si)RNA was purchased from
Shanghai Genechem Co., Ltd. (Shanghai, China). PRKCD siRNA was
transfected into HUVECs using Lipofectamine 2000 according to the
manufacturer's instructions. Follow-up experiments were performed
48 h later. Cells were observed using an inverted fluorescent
microscope (IX 73; Olympus Corp., Tokyo, Japan).
Western blot analysis
HUVECs were lysed in radio immunoprecipitation assay
buffer (Beyotime Institute of Biotechnology). Protein was
determined by BCA assay, and 20 µg protein was separated by 12.5%
SDS-PAGE and subsequently transferred to polyvinylidene difluoride
membranes. Membranes were blocked with 5% non-fat dry milk in
Tris-buffered saline with Tween 20 for 1 h at room temperature and
subsequently incubated with antibodies against PRKCD (1:800) or
GAPDH (1:5,000) overnight at 4°C. Subsequently, membranes were
incubated with a secondary antibody horseradish
peroxidase-conjugated goat anti-mouse immunoglobulin (Ig)G antibody
(cat. no. BS12478; 1:5,000; Bioworld Technology, Inc., St. Louis
Park, MN, USA) for 1 h at room temperature and washed with PBST 5
min three times. The protein chemiluminescence was then detected
using enhanced chemiluminescence substrate and analyzed by Quantity
one V 4.6.2 (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Dual-luciferase reporter gene
assay
The target gene of miR-26a was predicted using
TargetScan (http://www.targetscan.org/). The miR-26a binding
sequence and mutation region sequence in 3′-UTR of PRKCD were
synthesized according to bioinformatic analysis (21) and then cloned into pMIR-REPORT
plasmids (Thermo Fisher Scientific, Inc.). The two types of
constructed plasmids and miR-26a mimics were respectively
co-transfected into HEK293 cells using Lipofectamine 2000 (Thermo
Fisher Scientific, Inc.). The fluorescence value of each group was
detected 24 h later using the dual-luciferase reporter gene system
(Promega Corporation; Madison, WI, USA) according to the
manufacturer's instructions and was compared with Renilla
luciferase activity for normalization.
Statistical analysis
Data were expressed as the mean + standard
deviation. Statistical analyses were performed using the two-tailed
Student's t-test (paired) and SPSS 16.0 software (SPSS, Inc.,
Chicago, IL, USA). The clinical value of miR-26a in the diagnosis
of DVT was evaluated using a receiver operating characteristic
(ROC) curve. In addition, Spearman's rank correlation analysis was
conducted to determine the correlation between miR-26a and CCL2 and
CCL7 levels. P<0.05 was considered to indicate a statistically
significant difference.
Results
Expression of miR-26 in the peripheral
blood of patients with DVT
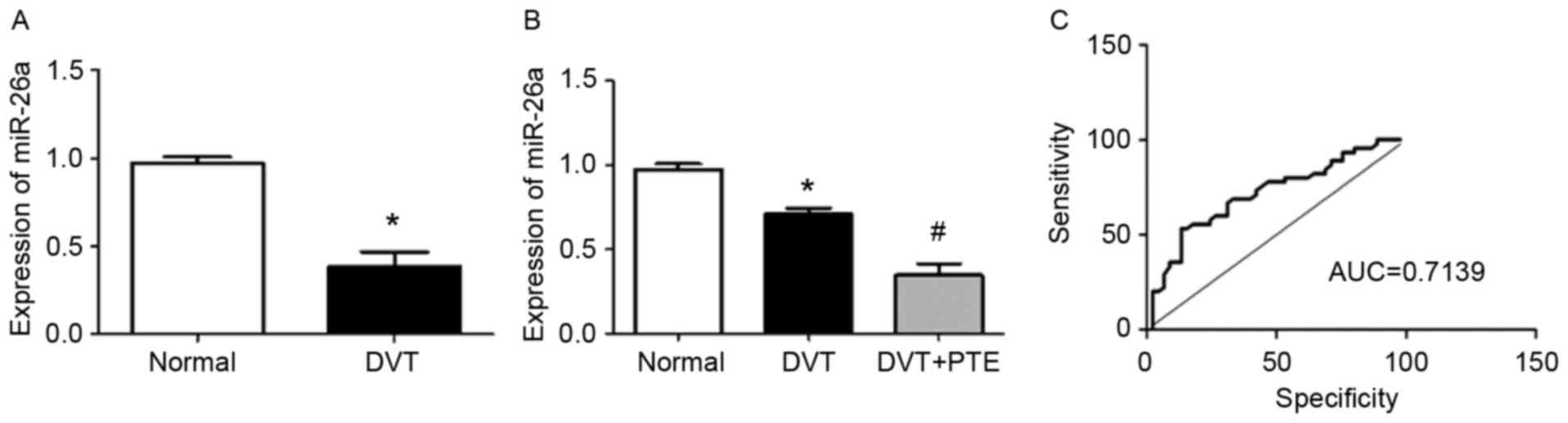
The results of RT-qPCR indicated that levels of
miR-26a were significantly downregulated in the peripheral blood of
patients with DVT compared with normal controls (P<0.05;
Fig. 1A). In addition, levels of
miR-26a in the peripheral blood of patients with DVT complicated
with pulmonary embolism (DVT + PTE) were significantly lower than
in patients with DVT alone (P<0.05; Fig. 1B). These results demonstrate that the
downregulated expression of miR-26a may be associated with DVT.
Analysis of ROC curve
To determine the role of miR-26a in the diagnosis of
DVT, a ROC curve was generated. The results of the ROC curve
analysis revealed that the largest area under the curve (AUC) was
0.7136 (P<0.01; Fig. 1C),
suggesting that miR-26a may be useful in the clinical diagnosis of
DVT.
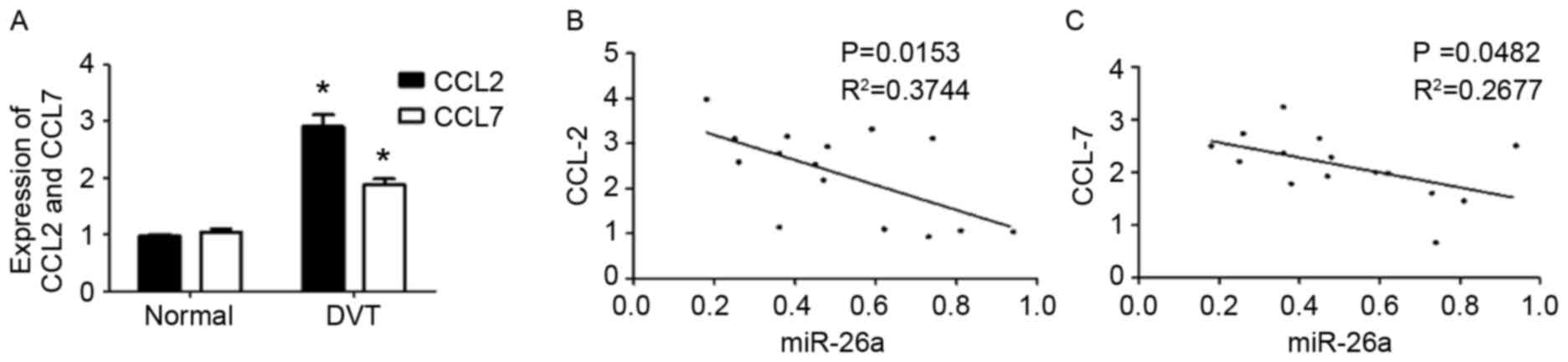
Correlation of CCL2 and CCL7 mRNA
levels with miR-26a
CCL2 and CCL7 are important inflammatory chemokines
that recruit monocytes to specified lesions, promote the release of
local inflammatory factors and aggravate the inflammatory response
(22,23). In the present study, the results from
RT-qPCR suggested that levels of CCL2 and CCL7 mRNA were
significantly increased in the peripheral blood of patients with
DVT compared with the controls (P<0.05; Fig. 2A). Spearman's rank correlation
analysis results indicated that the expression of miR-26a was
negatively correlated with levels of CCL2 and CCL7 mRNA in the
peripheral blood of patients with DVT (P<0.05; Fig. 2B and C, respectively). These results
indicate that miR-26a may be involved in the regulation of CCL2 and
CCL7 mRNA levels.
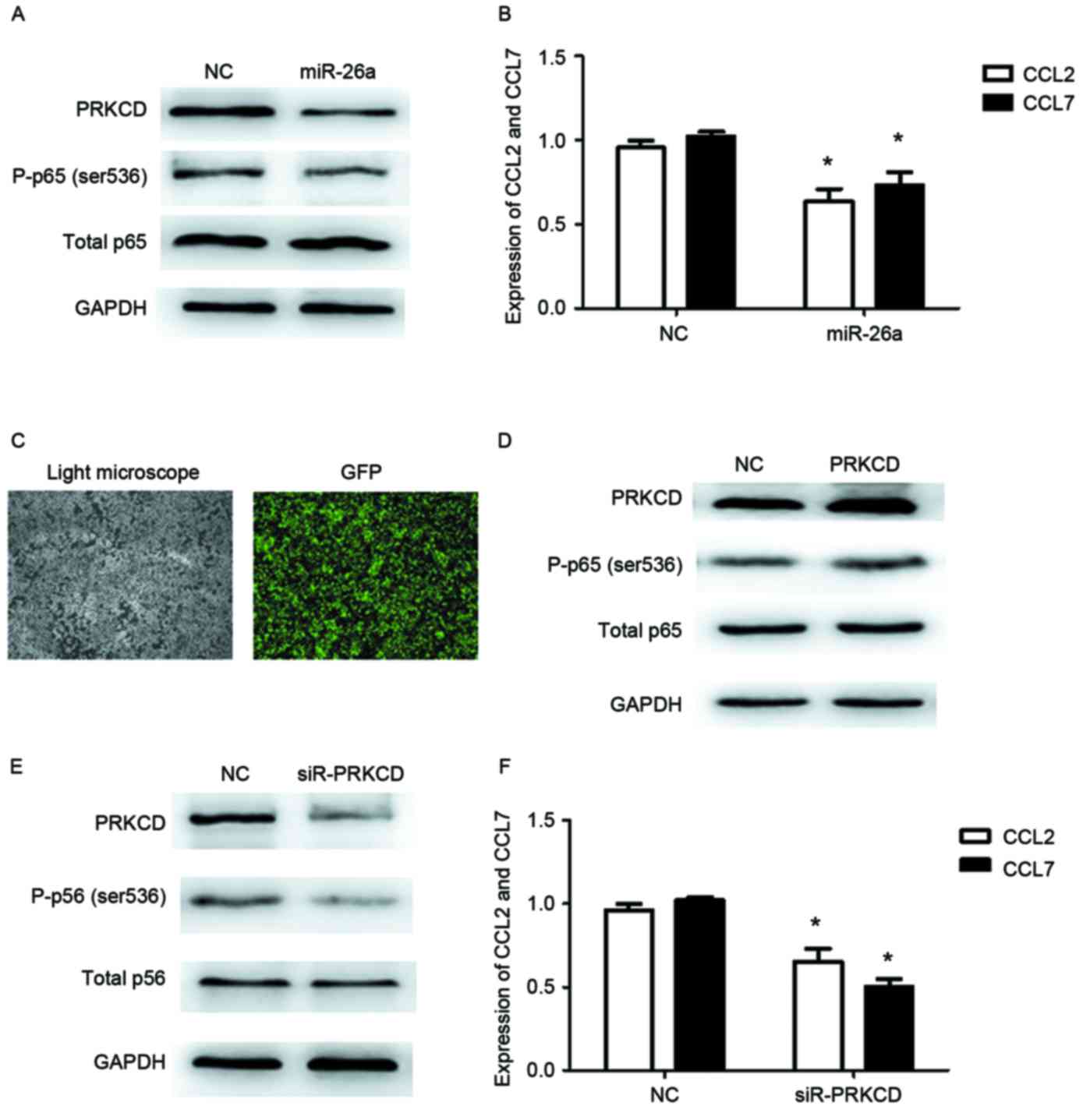
miR-26a-PRKCD-NF-κB signaling pathway
regulates the expression of CCL2 and CCL7
Bioinformatics analysis revealed that there was a
conservative binding domain of miR-26a in the 3′-UTR of PRKCD mRNA,
indicating that miR-26a may regulate the expression of PRKCD. It
has been demonstrated that PRKCD activates the NF-κB signaling
pathway, promotes the expression and release of CCL2 and CCL7 and
increases the local inflammatory response (24). Furthermore, it has been demonstrated
that the inflammatory response is associated with the occurrence of
DVT (25). Therefore, the effects of
miR-26a on PRKCD, NF-κB-related protein and levels of CCL2 and CCL7
mRNA were examined in the current study (Fig. 3). The results determined that the
expression of PRKCD was markedly decreased following the
overexpression of miR-26a in HUVECs (Fig. 3A). In addition, levels of CCL2 and
CCL7 mRNA were significantly decreased in miR-26a-overexpressed
HUVECs compared with the control (P<0.05; Fig. 3B). The phosphorylation of p65 protein
was markedly decreased in miR-26a-overexpressed HUVECs compared
with the control (Fig. 3A),
suggesting that the NF-κB signaling pathway was inactivated.
However, overexpression of PRKCD in HUVECs attenuated the effects
of miR-26a on p65 phosphorylation (Fig.
3D). Green fluorescence indicated the transfection efficiency
(Fig. 3C). These results suggest
that miR-26a may suppress the expression of PRKCD and inhibit the
NF-κB signaling pathway, thus inhibiting CCL2 and CCL7
expression.
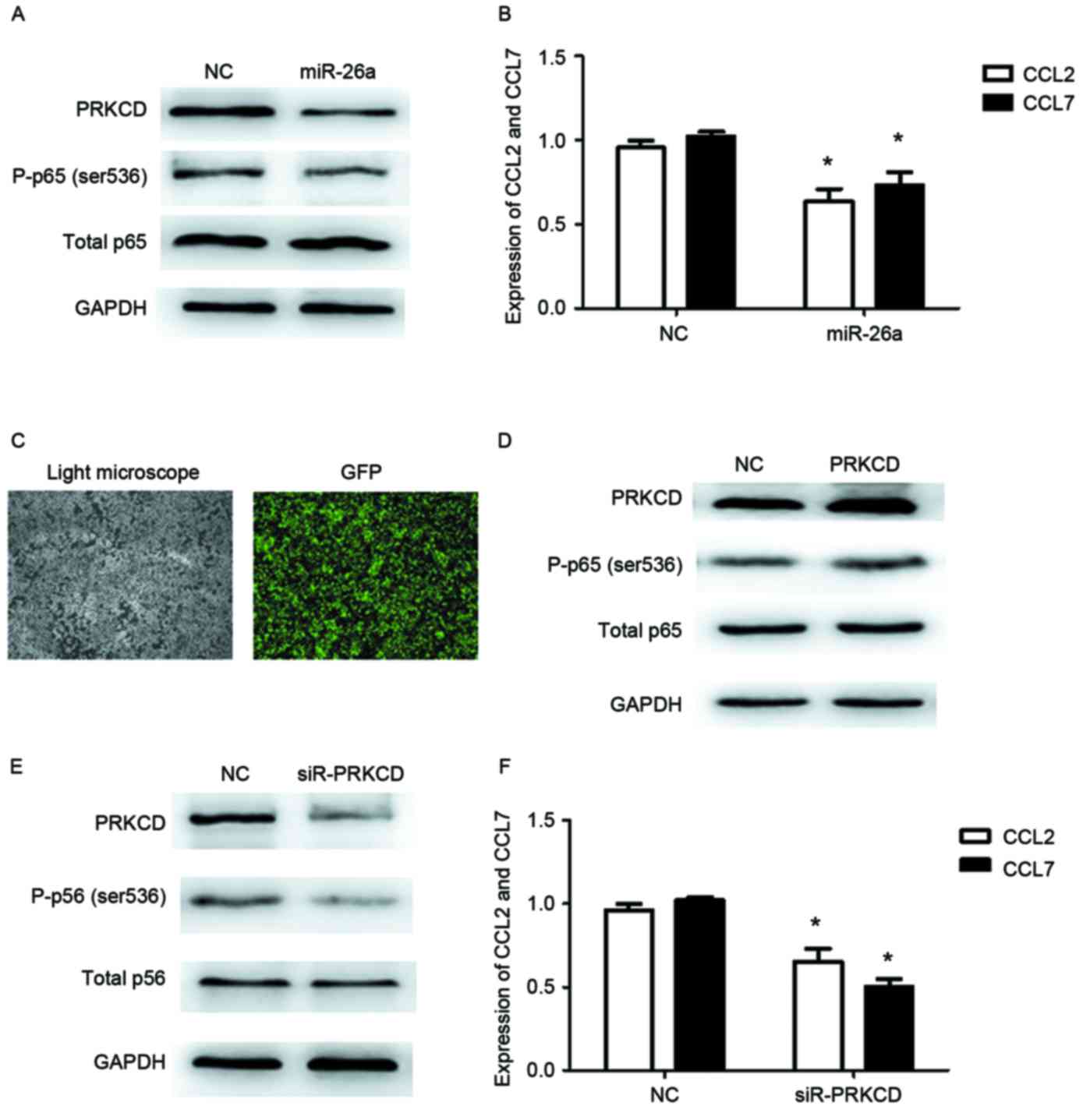 | Figure 3.miR-26a regulates the expression of
PRKCD, CCL2, CCL7 and p65. (A) Effect of miR-26a on the expression
of PRKCD and p-p65 was assessed using western blotting. GAPDH was
used as an internal control. (B) The effect of miR-26a on the
levels of CCL2 and CCL7 mRNA was detected by RT-qPCR. (C)
Fluorescence was detected following transfection with PRKCD
expression vector. Magnification, ×400. (D) Effect of PRKCD
overexpression on the phosphorylation of p65 was detected by
western blotting. (E) Effect of PPKCD knockdown on the expression
of p65 and p-p65 was assessed by western blotting. GAPDH was used
as an internal control. (F) Effect of PRKCD knockdown on the levels
of CCL2 and CCL7 mRNA was detected by RT-par. *P<0.05 vs. NC.
NC, negative control; p-p65, phosphorylated p65; miR-26,
microRNA-26; CCL, chemokine C-C motif ligand 2; PRKCD, protein
kinase C δ; GFP, green fluorescent protein; siR, small interfering
RNA; RT-qPCR, reverse transcription-quantitative polymerase chain
reaction. |
siR-PRKCD inhibits the activation of
NF-κB
To further determine the effect of PRKCD on the
NF-κB signaling pathway, PRKCD expression was reduced by siRNA.
Western blotting indicated that the expression of PRKCD was
markedly decreased following the transfection of siR-PRKCD
(Fig. 3E). Similarly, the
phosphorylation of p65 was markedly downregulated following a
decrease in the expression of PRKCD (Fig. 3E), suggesting that the NF-κB
signaling pathway was inhibited. Furthermore, levels of CCL2 and
CCL7 mRNA were significantly decreased in siR-PRKCD-treated HUVECs
compared with the control (P<0.05; Fig. 3F). These results suggest that PRKCD
regulates the NF-κB signaling pathway and decreases the expression
of CCL2 and CCL7.
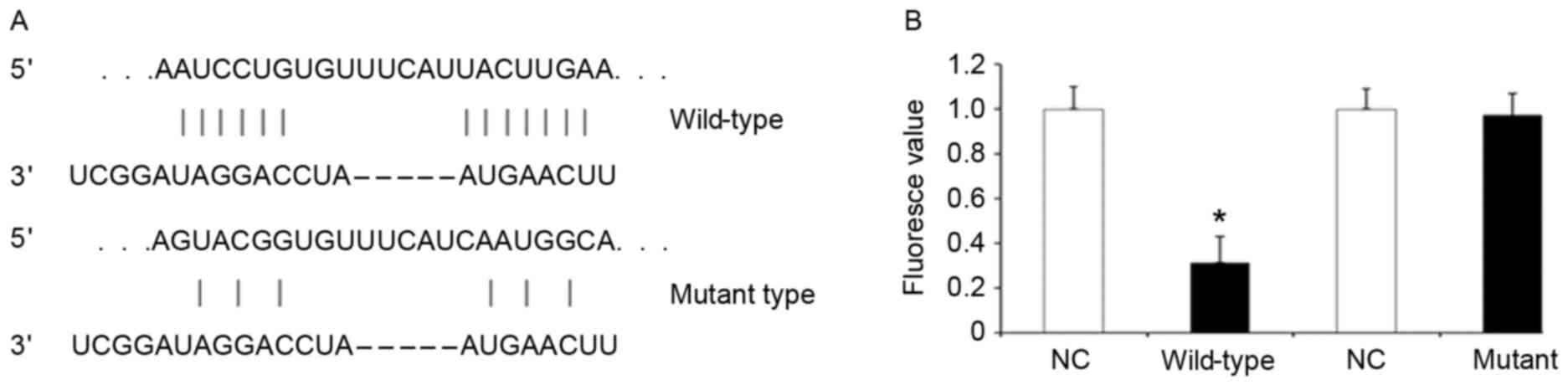
Dual-luciferase reporter gene
assay
The results of the dual-luciferase reporter gene
assay (Fig. 4) demonstrated that
fluorescence was significantly reduced following co-transfection of
miR-26a mimic and luciferase reporter gene plasmid
pMIR-REPORT-wild-type (P<0.01; Fig.
4B). However, there was no difference in fluorescence following
co-transfection of miR-26a mimic and pMIR-REPORT-mutant (Fig. 4B). These results suggest that miR-26a
is able to bind the specific domain in the 3′-UTR of PRKCD
mRNA.
Discussion
In the present study, the expression of miR-26a was
significantly downregulated in the peripheral blood of patients
with DVT. The AUC of the ROC curve was 0.7136, suggesting that
miR-26a may be valuable in the clinical diagnosis of DVT.
Furthermore, the results of the present study indicated that
miR-26a targeted PRKCD mRNA and inhibited the activation of the
NF-κB signaling pathway, thus downregulating the expression of CCL2
and CCL7 mRNA and attenuating the local inflammatory response.
Therefore, it was hypothesized that the reduction of miR-26a levels
may increase levels of inflammatory cytokines in the peripheral
blood of patients with bone trauma and increase the risk of
DVT.
DVT is a common clinical disease and its incidence,
morbidity and mortality rates have increased in recent years
(26). Clinical manifestations of
DVT are primarily lower limb swelling, ulceration and necrosis,
which may seriously limit patient quality of life (27). Detachment of thrombi may cause
pulmonary embolism and lead to patient mortality (21). Inflammation is a major of the risk
factors of DVT (28,29). Various studies have demonstrated that
levels of inflammatory cytokines and chemokines are increased in
the peripheral blood of patients with DVT. Du and Tan (10) identified that certain inflammatory
factors including IL-6, CRP and NF-κB are closely associated with
DVT. Krieger et al (30)
suggested that changes in CRP levels and the erythrocyte
sedimentation coefficient may induce acute lower extremity DVT.
miRNAs are post-transcription regulating factors and therefore may
serve an important role in inflammation. It was reported by Sawant
et al (31) that miR-21
targets B-cell lymphoma 6 mRNA and promotes the differentiation of
T helper 2 cells. Lu et al (32) demonstrated that miR-376b regulates
the expression of IL-6. Furthermore, it was determined that miR-26a
is involved in the differentiation of T cells and regulation of the
NF-κB signaling pathway (33). The
present study indicated that levels of miR-26a were significantly
downregulated in the peripheral blood of patients with DVT and
negatively correlated with CCL2 and CCL7 expression. Additionally,
bioinformatics analysis identified that miR-26a regulated the
expression of PRKCD. Previous results demonstrated that PRKCD
activates the NF-κB signal pathway and promotes the expression and
release of inflammatory cytokines (23). Therefore, it was hypothesized that
the downregulation of miR-26a in the peripheral blood of patients
with DVT may be associated with inflammation.
To investigate this hypothesis, miR-26a was
overexpressed in HUVECs and the expression of PRKCD was markedly
decreased. In addition, levels of CCL2 and CCL7 mRNA were
significantly decreased. The results from western blotting
suggested that miR-26a was able to inhibit activation of the NF-κB
signaling pathway. Reduction of PRKCD expression by siRNA also
attenuated activation of the NF-κB signaling pathway. A previous
study demonstrated that activation of NF-κB promoted the expression
and release of CCL2 and CCL7 (34).
CCL2 and CCL7 are able to recruit inflammatory cells to specific
lesions, promote the release of local inflammatory factors and
aggravate the inflammatory response (35). The results of the dual-luciferase
reporter gene assay conducted in the current study indicated that
miR-26a was able to bind to the 3′-UTR of PRKCD, demonstrating that
PRKCD is a target gene of miR-26a. This suggests that the
downregulation of miR-26a increased PRKCD expression, activating
the NF-κB signaling pathway and promoting the expression of CCL2
and CCL7.
In conclusion, the current study demonstrated that
miR-26a may be valuable in the clinical diagnosis of DVT as novel
biomarker. miR-26a may inactivate the NF-κB signaling pathway by
binding PRKCD mRNA and may reduce the risk of DVT by inhibiting the
inflammatory response.
References
|
1
|
van Hylckama Vlieg A and Baglin TP: The
risk of a first and a recurrent venous thrombosis associated with
an elevated D-dimer level and an elevated thrombin potential:
Results of the THE-VTE study: Reply. J Thromb Haemost.
13:2286–2287. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Van der Hulle T, den Exter PL, Planquette
B, Meyer G, Soler S, Monreal M, Jiménez D, Portillo AK, O'Connell C
and Liebman HA: Risk of recurrent venous thromboembolism and major
hemorrhage in cancer-associated incidental pulmonary embolism
amongst treated and untreated patients: A pooled analysis of 926
patients. J Thromb Haemost. 14:105–113. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hossam Abdel-Hamid, Jonathan Miles,
Richard W J. Carrington, Alister Hart, Alex Loh, John A and
Skinner: Combined vascular and orthopedic approach for a
pseudotumor causing deep vein thrombosis after metal-on-metal hip
resurfacing arthroplasty. Case Rep Orthop.
2015:9262632015.PubMed/NCBI
|
|
4
|
Hattab Y, Küng S, Fasanya A, Ma K, Singh
AC and DuMont T: Deep venous thrombosis of the upper and lower
extremity. Crit Care Nurs Q. 40:230–236. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cho SY, Youn HJ, Park MY, Shim BJ, Lee SJ,
Kim JH, Park JK, Oh CY, Ahn SH and Cho WH: Post-operative multiple
thrombosis associated with patent foramen ovale: Embolic stroke,
right atrial thrombi, pulmonary embolism and deep vein thrombosis.
J Cardiovasc Ultrasound. 23:177–180. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ahn S, Kim MH, Jun KW, Hwang JK, Park SC,
Moon IS and Kim JI: The incidence and risk factors of deep vein
thrombosis after kidney transplantation in Korea: Single center
experience. Clin Transplant. 29:1181–1186. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Alderman BE, de Boisanger J and Bottomley
T: Hypoplasia of the inferior vena cava in a young man presenting
with extensive deep venous thrombosis. BMJ Case Rep 2015. pii
bcr2015211849. 2015. View Article : Google Scholar
|
|
8
|
Park SI, Lee M, Lee MS, Kim MD, Won JY and
Lee DY: Single-session aspiration thrombectomy of lower extremity
deep vein thrombosis using large-size catheter without
pharmacologic thrombolysis. Cardiovasc Intervent Radiol.
37:412–419. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gholami K, Talasaz AH, Entezari-Maleki T,
Salarifar M, Hadjibabaie M, Javadi MR, Dousti S, Hamishehkar H and
Maleki S: The effect of high-dose vitamin D3 on soluble p-selectin
and hs-crp level in patients with venous thromboembolism: A
randomized clinical trial. Clin Appl Thromb Hemost. 22:483–489.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Du T and Tan Z: Relationship between deep
venous thrombosis and inflammatory cytokines in postoperative
patients with malignant abdominal tumors. Braz J Med Biol Res.
47:1003–1007. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Entezari-Maleki T, Talasaz A Hajhossein,
Salarifar M, Hadjibabaie M, Javadi MR, Bozorgi A, Jenab Y,
Boroumand MA and Gholami K: Plasma VITAMIN D status and its
correlation with risk factors of thrombosis, P-selectin and hs-CRP
level in patients with venous thromboembolism; the first study of
Iranian population. Iran J Pharm Res. 13:319–327. 2014.PubMed/NCBI
|
|
12
|
Stypińska B and Paradowska-Gorycka A:
Cytokines and MicroRNAs as candidate biomarkers for systemic lupus
erythematosus. Int J Mol Sci. 16:24194–24218. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhu W, Qian J, Ma L, Ma P, Yang F and Shu
Y: MiR-346 suppresses cell proliferation through SMYD3 dependent
approach in hepatocellular carcinoma. Oncotarget. May 22–2017.doi:
10.18632/oncotarget.18060. (Epub ahead of print).
|
|
14
|
Iwakawa HO and Tomari Y: The functions of
MicroRNAs: mRNA decay and translational repression. Trends Cell
Biol. 25:651–665. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huang YK and Yu JC: Circulating microRNAs
and long non-coding RNAs in gastric cancer diagnosis: An update and
review. World J Gastroenterol. 21:9863–9886. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
He Y, Lin J, Kong D, Huang M, Xu C, Kim
TK, Etheridge A, Luo Y, Ding Y and Wang K: Current state of
circulating MicroRNAs as cancer biomarkers. Clin Chem.
61:1138–1155. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Libânio D, Dinis-Ribeiro M and
Pimentel-Nunes P: Helicobacter pylori and microRNAs: Relation with
innate immunity and progression of preneoplastic conditions. World
J Clin Oncol. 6:111–132. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sakimoto T and Ishimori A:
Anti-inflammatory effect of topical administration of tofacitinib
on corneal inflammation. Exp Eye Res. 145:110–117. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schaefer JK, Jacobs B, Wakefield TW and
Sood SL: New biomarkers and imaging approaches for the diagnosis of
deep venous thrombosis. Curr Opin Hematol. 24:274–281. May;2017.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-tie quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim JH, Jeon S and Shin BA: MicroRNA-29
family suppresses the invasion of HT1080 human fibrosarcoma cells
by regulating matrix metalloproteinase 2 expression. Chonnam Med J.
53:161–167. May;2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bardina SV, Michlmayr D, Hoffman KW, Obara
CJ, Sum J, Charo IF, Lu W, Pletnev AG and Lim JK: Differential
roles of chemokines CCL2 and CCL7 in monocytosis and leukocyte
migration during west nile virus infection. J Immunol.
195:4306–4318. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cummings R, Zhao Y, Jacoby D, Spannhake
EW, Ohba M, Garcia JG, Watkins T, He D, Saatian B and Natarajan V:
Protein kinase Cdelta mediates lysophosphatidic acid-induced
NF-kappaB activation and interleukin-8 secretion in human bronchial
epithelial cells. J Biol Chem. 279:41085–41094. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Abdalla G, Matuk R Fawzi, Venugopal V,
Verde F, Magnuson TH, Schweitzer MA and Steele KE: The diagnostic
accuracy of magnetic resonance venography in the detection of deep
venous thrombosis: A systematic review and meta-analysis. Clin
Radiol. 70:858–871. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Friedmann DP, Liolios AM, Wu DC, Goldman
MP and Eimpunth S: A randomized, double-blind, placebo-controlled
study of the effect of a high-potency topical corticosteroid after
sclerotherapy for reticular and telangiectatic veins of the lower
extremities. Dermatol Surg. 41:1158–1163. Oct;2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gómez-Outes A, Suárez-Gea ML, Lecumberri
R, Terleira-Fernández AI and Vargas-Castrillón E: Direct oral
anticoagulants in the treatment of venous thromboembolism, with a
focus on patients with pulmonary embolism: An evidence-based
review. Vasc Health Risk Manag. 10:627–639. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Olszewski WL, Zaleska M, Stelmach E,
Swoboda-Kopec E, Jain P, Agrawal K, Gogia S, Gogia A, Andziak P and
Durlik M: Cryptic bacteria of lower limb deep tissues as a possible
cause of inflammatory and necrotic changes in ischemia, venous
stasis and varices and lymphedema. Surg Infect (Larchmt).
16:313–322. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Saghazadeh A, Hafizi S and Rezaei N:
Inflammation in venous thromboembolism: Cause or consequence? Int
Immunopharmacol. 28:655–665. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jenkins JS and Michael P: Deep venous
thrombosis: An interventionalist's approach. Ochsner J. 14:633–640.
2014.PubMed/NCBI
|
|
30
|
Krieger E, Van der Loo B, Amann-Vesti BR,
Rousson V and Koppensteiner R: C-reactive protein and red cell
aggregation correlate with late venous function after acute deep
venous thrombosis. J Vasc Surg. 40:644–649. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sawant DV, Wu H, Kaplan MH and Dent AL:
The Bcl6 target gene microRNA-21 promotes Th2 differentiation by a
T cell intrinsic pathway. Mol Immunol. 54:435–442. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lu S, Jiao H, Xu J, Zheng Y, Sun Y and
Chen H: Downregulation of IL6 targeted MiR-376b may contribute to a
positive IL6 feedback loop during early liver regeneration in mice.
Cell Physiol Biochem. 37:233–242. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Xie Q, Wei M, Kang X, Liu D, Quan Y, Pan
X, Liu X, Liao D, Liu J and Zhang B: Reciprocal inhibition between
miR-26a and NF-κB regulates obesity-related chronic inflammation in
chondrocytes. Biosci Rep. 35:pii e002042015.
|
|
34
|
Bauer D, Redmon N, Mazzio E, Taka E,
Reuben JS, Day A, Sadrud-Din S, Flores-Rozas H, Soliman KF and
Darling-Reed S: Diallyl disulfide inhibits TNFα induced CCL2
release through MAPK/ERK and NF-Kappa-B signaling. Cytokine.
75:117–126. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Gao X, Huang W, Zhang X, Du S, Wang J,
Wang W, Zhou M, Chen S, Li X and Jonas JB: Chemokine (C-C motif)
ligand 2 and chemokine (C-C motif) ligand 7 in angle-closure
glaucoma. Acta Ophthalmol. 94:e220–e224. 2016. View Article : Google Scholar : PubMed/NCBI
|