Introduction
Presently, approximately 10% of couples are plagued
by reproduction-related issues mainly caused by environmental
factors and stress. Since the advent of assisted reproductive
technology such as the in vitro fertilization-embryo
transfer, artificial insemination, and ovulation induction
techniques, provided great opportunity for infertile patients to
coup with their problem.
However, it has been reported that IVF technology
may have certain undesirable side effects, such as OHSS and
hypertensive disorders in pregnancy, possibly due to use of drugs
and operational intervention (1,2).
Hypertensive disorders in pregnancy have an insidious onset with a
fast progressive course, which may cause serious challenges
(3), and may threaten maternal and
neonatal health. Studying the connection between IVF procedures and
hypertensive disorders in pregnancy can contribute to early
prevention and treatment. In this study, correlation of
hypertensive disorders in pregnancy with different procedures of
in vitro fertilization was explored, and pregnancy outcomes
of patients were evaluated.
Patients and methods
Subjects
From February 2012 to February 2016, a total of 658
maternity patients who conceived through in vitro
fertilization in our hospital's assisted reproductive center and
gave birth in Maternal and Child Health Hospital of Wuxi and had
completed clinical records were enrolled in this study. This study
was approved by the Ethics Committee of Maternal and Child Health
Hospital of Wuxi. Signed written informed consents were obtained
from the patients' guardians. Inclusion criteria: Patients with no
history of hypertension prior to pregnancy; patient with complete
clinical data in our hospital's assisted reproductive center and
obstetric department; pregnancy outcomes were either live single
birth or live twin births (including embryo reduction in the early
stage of multiple pregnancy); patients delivered no less than 25
gestational weeks with a birth weight of no less than 700 grams. A
specialized physician performed the whole process of ovulation
induction, egg retrieval, IVF and embryo transfer. All patients had
an average infertility duration of 4.3±3.5 years, with 242 patients
in primary infertility and 416 patients in secondary infertility.
Patients who were diagnosed with other conditions included 39 cases
of gestational diabetes, 76 cases of hepatitis B virus carriers and
hepatitis B patients with symptoms, 57 cases of uterine fibroids, 9
cases with history of tuberculosis, 3 cases with history of
syphilis, and 10 cases with history of thyroid disease. Patients
were divided into two groups according to different fertilization
procedures: i) the routine in vitro fertilization-embryo
transfer group (IVF-ET group, 377 cases) and ii) the
intra-cytoplasmic sperm injection-embryo transfer group (ICSI-ET
group, 281 cases). Patients were also divided into two groups
according to different embryo transfer cycles: the fresh embryo
transfer group (F-ET group, 446 cases) and the frozen-thawed embryo
transfer group (T-ET group, 212 cases). Patients' general data in
different groups are presented in Table
I. No significant differences between the two groups
(P>0.05) in comparison of infertility years, gestational weeks,
pregnancy outcomes (single/twins), birth weight and delivery mode
were detected. All corresponding data were comparable. If
P<0.05, the difference was considered statistically
significant.
 | Table I.General data of patients in different
groups (mean ± SD). |
Table I.
General data of patients in different
groups (mean ± SD).
|
|
|
|
| Pregnancy
outcome |
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|---|
| Group | N | Infertility
years | Gestational
weeks | Single | Twin | Birth weight (g) | Natural labor | BMI
(kg/m2) |
|---|
| IVF-ET | 377 | 4.2±3.6 | 27.8±7.1 | 261 | 116 | 2802.7±754.1 | 19 | 21.8±2.7 |
| ICSI-ET | 281 | 4.4±3.3 | 28.0±6.7 | 198 | 83 | 2789.2±800.9 | 16 | 21.5±3.1 |
|
t-value/χ2 |
| 1.125 | 1.076 | 0.968 | 1.324 | 1.401 | 1.434 |
| P-value |
| 0.611 | 0.612 | 0.664 | 0.087 | 0.081 | 0.075 |
| F-ET | 446 | 4.3±3.5 | 27.6±6.9 | 307 | 139 | 2792.6±746.8 | 24 | 21.9±2.5 |
| T-ET | 212 | 4.5±3.2 | 27.9±7.0 | 152 | 60 | 2787.5±781.3 | 11 | 21.6±2.9 |
|
t-value/χ2 |
| 1.123 | 1.254 | 1.106 |
| 1.076 | 1.365 | 1.563 |
| P-value |
| 0.598 | 0.058 | 0.421 |
| 0.587 | 0.088 | 0.069 |
Methods
Diagnostic criteria for hypertensive disorders in
pregnancy were based on the Gynecological Guidelines introduced by
the American Association of Obstetricians and Gynecologists in
2004.
Procedures performed on patients in
the IVF-ET group
Follicles were prepared using hormone replacement
therapy (HRT), micro-stimulation, natural cycle and various
controlled superovulation schemes. When the follicle diameter
reached 18–20 mm, appropriate amount of human chorionic
gonadotropin (HCG) was injected at night to trigger ovulation. Eggs
were retrieved 36 h later through type-B ultrasound-guided needle
puncture. Sperms were collected via masturbation, or surgical
extraction from testicular tissue or epididymis. Best sperms and
eggs were selected and put together in a culture dish allowing them
combined to form fertilized eggs. After 2–5 days, the fertilized
eggs in the culture dish grew to early embryos which were
transferred into the patient's uterine cavity, aiming for a
successful pregnancy and childbirth.
Procedures performed on patients in
the ICSI-ET group
Procedures of ovulation induction, egg retrieval and
sperm collection were the same as described for patients in the
IVF-ET group, but the fertilization mode was different. Under a
microscope, a microinjection needle was used to manually pierce
through the zona pellucida and egg cell membrane to inject a single
sperm into the cytoplasm for fertilization. Compared with routine
IVF, ICSI had a higher success rate of pregnancy. ICSI was
beneficial to patients suffering from infertility due to serious
male oligoasthenoteratozoospermia, obstructive azoospermia, and
nonfertilization after routine IVF.
Procedures performed on patients in
the F-ET group
Fresh embryos were transferred into the patient's
uterine cavity after 2–5 days following fertilization under
above-mentioned fertilization modes.
Procedures performed on patients in
the T-ET group
In some patients, fresh embryo transfer was given up
due to OHSS, peak level of progesterone or other reasons. After
this cycle, frozen-thawed embryo transfer was performed.
Statistical method
Statistical analysis was performed using SPSS 18.0
software (SPSS Inc., Chicago, IL, USA). Measurement data were
expressed as mean ± SD, and compared using t inspection. Ratios and
rates of two groups and above were compared using the exact
probability test of a contingency table. The binary regression
model was used to calculate uncorrected odds ratio (OR) and
confidence interval (CI), as well as corrected OR and CI by
multiple factors. Interference of confounding factors was avoided
as far as possible. Difference was considered statistically
significant when P<0.05.
Results
Characteristics of patients who
conceived through assisted reproductive technology
Single or multiple births in different
groups
For single birth, 261 cases (56.86%) and 198 cases
(43.14%) were recorded in the IVF-ET and ICSI-ET group,
respectively, while 307 cases (66.88%) and 152 cases (33.12%) were
recorded in the F-ET and T-ET group, respectively. For twin births,
116 cases (58.29%) and 83 cases (41.71%) were recorded in the
IVF-ET and ICSI-ET group, respectively, and 139 cases (69.85%) and
60 cases (30.15%) were recorded, respectively. There were no
statistically significant differences between single births or twin
births in the corresponding groups (P>0.05) (Table II).
 | Table II.Single or multiple births in different
groups (n, %). |
Table II.
Single or multiple births in different
groups (n, %).
|
| Fertilization
mode | Transfer cycles |
|---|
|
|
|
|
|---|
| Births | IVF-ET group | ICSI-ET group | F-ET group | T-ET group |
|---|
| Single | 261 (56.86) | 198 (43.14) | 307 (66.88) | 152 (33.12) |
| Twin | 116 (58.29) | 83
(41.71) | 139 (69.85) | 60
(30.15) |
| t-value | 1.256 | 1.387 | 1.439 | 1.402 |
| P-value | 0.713 | 0.621 | 0.589 | 0.615 |
Child-bearing age of patients in different
groups
Patients' child-bearing ages in different groups
were divided into 5 age ranges with five-year intervals. The number
of patients in the 30–34 years old range was the largest, with
44.03% (166 cases) in the IVF-ET group, 46.26% (130 cases) in the
ICSI-ET group, 45.07% (201 cases) in the F-ET group, and 45.28% (96
cases) in the T-ET group. The differences between groups were not
statistically significant (P>0.05). There were no significant
differences between groups in the other age ranges (P>0.05)
(Table III).
 | Table III.Child-bearing age of patients in
different groups (n, %). |
Table III.
Child-bearing age of patients in
different groups (n, %).
| Age range | IVF-ET group | ICSI-ET group | F-ET group | T-ET group |
χ2-value | P-value |
|---|
| 20–24 | 6 (1.60) | 4 (1.42) | 8 (1.79) | 3 (1.42) | 1.865 | 0.726 |
| 25–29 | 89 (23.60) | 74 (26.33) | 103 (23.09) | 46 (21.70) | 2.013 | 0.613 |
| 30–34 | 166 (44.03) | 130 (46.26) | 201 (45.07) | 96 (45.28) | 1.432 | 0.941 |
| 35–39 | 84 (22.28) | 57 (20.28) | 100 (22.42) | 47 (22.17) | 1.648 | 0.827 |
| 40–45 | 32 (8.49) | 16 (5.69) | 34 (7.62) | 20 (9.43) | 2.369 | 0.525 |
Causes of infertility for patients in different
groups
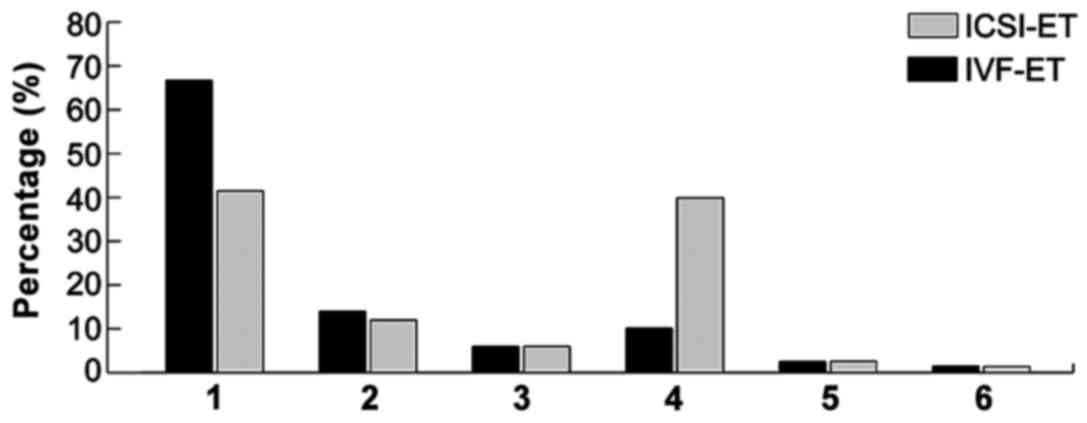
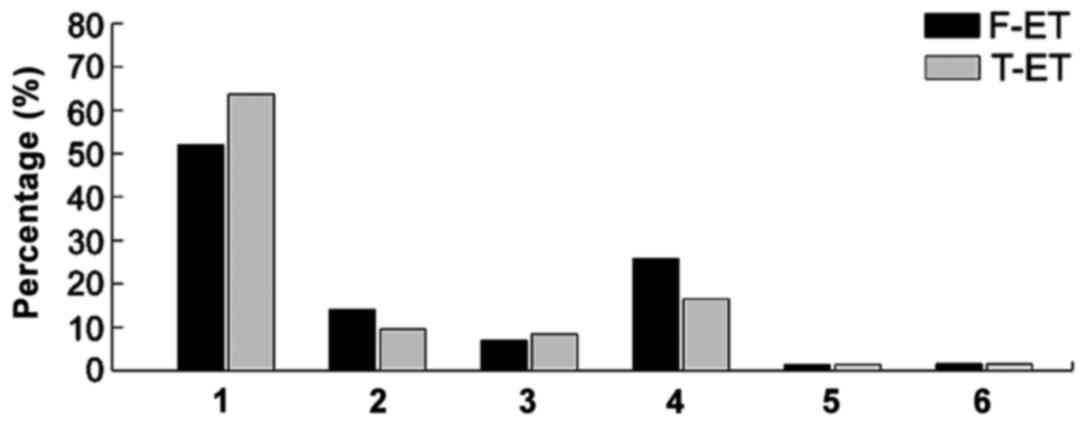
Among 658 patients with infertility, 366 cases were
infertile due to tubal problems (congenital anomalies of the
fallopian tubes, tubal inflammation, and history of tubal
ligation), 83 cases due to endometriosis, 44 cases due to ovulation
disorders, 150 cases due to male sperm abnormalities
(oligoasthenoterazoospermia, necrospermia, and azoospermia), 8
cases due to other factors (abnormal chromosome, and congenital
malformation of genital tract), and 7 cases due to unknown causes.
Tubal problems ranked the first cause of infertility in all groups,
accounting for 66.7% in the IVF-ET group, 41.5% in the ICSI-ET
group, 52.1% in the F-ET group, and 63.7% in the T-ET group. Male
sperm abnormalities accounted for 39.86% (112 cases) in the ICSI-ET
group, 10.08% (38 cases) in the IVF-ET group, 25.78% (115 cases) in
the F-ET group, and 16.51% (35 cases) in the T-ET group.
Apparently, the majority of patients in the ICSI-ET group suffered
from male sperm abnormalities (Figs.
1 and 2).
Correlation of different fertilization modes with
hypertensive disorders in pregnancy
Among all the 658 maternity patients who conceived
through IVF, there were 56 cases (8.51%) of hypertensive disorders
in pregnancy, including 21 cases (3.19%) of gestational
hypertension, 34 cases (5.17%) of pre-eclampsia and 1 case (0.15%)
of eclampsia. Among the 459 single-birth patients, there were 30
cases (6.54%) of hypertensive disorders in pregnancy, including 11
cases (2.40%) of gestational hypertension, 19 cases (4.14%) of
pre-eclampsia and no eclampsia. Among the 199 twin-birth patients,
there were 26 cases (13.07%) of hypertensive disorders in
pregnancy, including 10 cases (5.03%) of gestational hypertension,
15 cases (7.54%) of pre-eclampsia and 1 case (0.50%) of
eclampsia.
Correlation of different fertilization modes with
hypertensive disorders in pregnancy
Among the 377 patients in the IVF-ET group, there
were 26 cases (6.90%) of hypertensive disorders in pregnancy,
including 8 cases (2.12%) of gestational hypertension, 18 cases
(4.77%) of pre-eclampsia and no eclampsia. Among the 281 patients
in the ICSI-ET group, there were 30 cases (10.68%) of hypertensive
disorders in pregnancy, including 13 cases (4.63%) of gestational
hypertension, 16 cases (5.69%) of pre-eclampsia and 1 case (0.36%)
of eclampsia.
The odds ratio (OR) of gestational hypertension in
the comparison between the ICSI-ET and the IVF-ET groups was 2.01
(0.81–4.74), and was reduced to 1.69 (0.70–4.02) after correction.
There were significant differences in the correlation. The odds
ratio of pre-eclampsia in the comparison between the ICSI-ET and
IVF-ET groups was 1.36 (0.42–4.18), and was reduced to 1.17
(0.36–3.62) after correction. There were no significant differences
in the correlation. The differences of OR of gestational
hypertension or pre-eclampsia in twin-birth patients of the two
groups were statistically significant, but the differences in
single-birth patients were not statistically significant (Table IV).
 | Table IV.Correlation of different
fertilization modes with hypertensive disorders in pregnancy (n,
%). |
Table IV.
Correlation of different
fertilization modes with hypertensive disorders in pregnancy (n,
%).
|
| Gestational
hypertension | Pre-eclampsia |
|---|
|
|
|
|
|---|
| Group | All | Single birth | Twin births | All | Single birth | Twin births |
|---|
| IVF-ET | 8
(2.12) | 6 (2.30) | 2 (1.72) | 18 (4.77) | 11 (4.21) | 7 (6.03) |
| ICSI-ET | 13 (4.63) | 5 (2.53) | 8 (9.64) | 16 (5.69) | 8
(4.04) | 8 (9.64) |
| OR | 2.01 | 1.23 | 6.24 | 1.36 | 0.87 | 2.21 |
|
| 0.81–4.74 | 0.35–3.39 | 1.02–27.5 | 0.42–4.18 | 0.25–2.06 | 0.59–5.26 |
| Corrected
ORa | 1.69 | 0.96 | 5.46 | 1.17 | 0.8 | 2.15 |
|
| 0.70–4.02 | 0.29–3.01 | 0.82–23.6 | 0.36–3.62 | 0.26–2.00 | 0.52–4.78 |
Correlation of different embryo transfer cycles
with hypertensive disorders in pregnancy
Among the 466 patients in the F-ET group, there were
40 cases (8.97%) of hypertensive disorders in pregnancy, including
17 cases (3.81%) of gestational hypertension, 23 cases (5.16%) of
pre-eclampsia and no eclampsia. Among the 212 patients in the T-ET
group, there were 15 cases (7.08%) of hypertensive disorders in
pregnancy, including 4 cases (1.89%) of gestational hypertension,
11 cases (5.19%) of pre-eclampsia and 1 case (0.47%) of
eclampsia.
The odds ratio (OR) of gestational hypertension in
the comparison between the F-ET and T-ET groups was 0.44
(0.13–1.34), and became 0.49 (0.15–1.51) after correction. The odds
ratio of pre-eclampsia in the comparison between the F-ET and T-ET
groups was 0.93 (0.42–1.96), and became 0.98 (0.44–2.12) after
correction. There were no significant differences in the
correlation. The differences of OR of gestational hypertension or
pre-eclampsia in single-birth or twin-birth patients of the two
groups were not statistically significant (Table V).
 | Table V.Correlation of different embryo
transfer cycles with hypertensive disorders in pregnancy (n,
%). |
Table V.
Correlation of different embryo
transfer cycles with hypertensive disorders in pregnancy (n,
%).
|
| Gestational
hypertension | Pre-eclampsia |
|---|
|
|
|
|
|---|
|
|
|
|
|---|
| F-ET | 17 (3.81) | 9 (2.93) | 8 (5.76) | 23 (5.16) | 15 (4.89) | 8 (5.76) |
|---|
| T-ET | 4
(1.89) | 2 (1.32) | 2 (3.33) | 11 (5.19) | 4
(2.63) | 7
(11.67) |
| OR | 0.44 | 0.33 | 0.68 | 0.93 | 0.52 | 1.86 |
|
| 0.13–1.34 | 0.05–1.47 | 0.15–3.32 | 0.42–1.96 | 0.20–1.61 | 0.64–5.61 |
| Corrected OR | 0.49 | 0.41 | 0.6 | 0.98 | 0.61 | 1.98 |
|
| 0.15–1.51 | 0.09–1.98 | 0.13–3.15 | 0.44–2.12 | 0.22–1.84 | 0.73–6.43 |
Discussion
In the past 30 years, with commercialization of
assisted reproductive technology and vigorous development of its
derived technologies, the assisted reproductive technology has
advanced from IVF-ET to ICSI-ET, preimplantation genetic diagnosis
(PGD), and frozen-thawed embryo transfer. Nevertheless, the
test-tube baby technology was considered to be a double-edged
sword; on one hand, it was great news for patients suffering from
infertility, but at the same time it was plagued with its potential
safety risks. Results obtained from prior studies showed that the
increase in the number of test-tube babies has led to an upsurge in
the number of babies with birth defects (4–6). In
addition, maternity health at different stages of pregnancy has
been adversely affected (7).
Patient characteristics in successful cases of IVF
technology. In terms of age, the average maternal age for patients
participated in this study was higher than the average in China. In
our society, more and more women start pregnancy and give birth at
advanced maternal age. Advanced maternal age might be a leading
factor for poor outcomes for both mother and newborns. In this
study, we discovered that in most cases we had a single birth
(69.76%), and patients who successfully gave twin births were
mostly young with good ovarian response, and who provided more eggs
and thus more transferable embryos. In terms of mode of delivery,
the rate of spontaneous labor was 5.32% among those patients who
conceived successfully through IVF in our hospital's assisted
reproductive center. This rate was apparently lower than that of
natural pregnancy in China. In this study, we also found that the
rate of caesarean section among patients who conceived through IVF
was significantly higher than that among patients who conceive
naturally. This finding was similar to results reported in prior
studies (8,9). This phenomenon can be explained by the
fact that in most cases, older patients are those who usually opt
for assisted reproductive technology. In view of many potential
complications due to advanced maternal age, medical practitioners
may relax the cesarean section indications appropriately in their
real work. Moreover, those patients who feel a desperate need to
have a baby may proactively ask for a caesarean birth.
Causes of infertility for patients who conceived
through IVF. The number of patients suffering from infertility is
increasing. It has been shown that the first three causes of
infertility for patients who conceived through IVF are tubal
problems, male sperm abnormalities and endometriosis. The tubal
problems include congenital tubal abnormalities, tubal non-specific
inflammation, and history of tubal ligation of the fallopian tube.
Male sperm abnormalities include azoospermia, necrospermia,
teratozoospermia, asthenospermia, and oligospermia. This was
followed by endometriosis, ovulation disorder, and other causes of
infertility (including chromosome abnormalities, male ejaculation
disorder, and congenital malformation of genital tract) (10). In this study, we had only few cases
(5.83%) with ovulation disorder conceived through fresh embryo
transfer. The reason can be explained by the fact that patients
with ovulation disorder were often with polycystic ovary syndrome
(PCOS) and susceptible to ovarian hyperstimulation syndrome (OHSS).
For these patients, frozen-thawed embryo transfer could achieve
higher live birth rate in comparison with fresh embryo transfer.
Additionally, risk of OHSS and incidence of unexpected abortion
were also low (11).
Correlation of procedures of in vitro
fertilization with hypertensive disorders in pregnancy. Different
from natural pregnancy, maternity patients who conceived through
IVF may experience adverse pregnancy outcomes such as hypertensive
disorders in pregnancy due to biological, medical and sociological
factors. Hypertensive disorders in pregnancy usually occur during
pregnancy with unknown pathogenesis, and in recent years, the
incidence rate of these disorders is on the rise (12), and is one of the top five causes
leading to maternal death. According to an incomplete statistic,
approximately 60,000 pregnant women die every year because of
pre-eclampsia and eclampsia (13).
Currently it is widely accepted that hypertensive disorders in
pregnancy may be related to inflammatory factors, genetic factors,
placental dysfunction, immune system dysfunction and other
mechanisms (14). According to
published literature, risk factors include family history, advanced
maternal age, history of hypertension, first birth, metabolic
syndrome, and twin pregnancy (15).
Whether or not the assisted reproductive technology increases the
incidence of hypertensive disorders in pregnancy remained
contentious in literature.
Mukhopadhaya and Arulkumaran (16) and Sibai (17) believe that the IVF technology
increase the risk of adverse pregnancy outcomes such as maternal
pre-eclampsia and gestational hypertension. While Sun et al
(18) as well as Isaksson et
al (19) offer an opposite
opinion. In this study, we discovered that incidence of
hypertensive disorders in pregnancy was 8.51%, which indicated the
IVF technology might affect occurrence and progression of
hypertensive disorders in pregnancy at different levels. Other
studies showed that age was one of the most important risk factors.
Maternity patients at advanced maternal age experienced a high risk
of developing hypertensive disorders in pregnancy in comparison
with patients at normal maternal age (20). Patients who conceived through IVF
usually had an infertility history, and were extremely nervous.
This nervousness may lead to anxiety or depression during
pregnancy. The stress experienced by patients may increase
resistance of the uterine artery, which is one of the factors
leading to pre-eclampsia (21).
The procedure of superovulation as part of IVF
technology was not able to fully simulate the physiological state
of hormone. It was reported that onset of pre-eclampsia may be
related to the unusually high levels of HCG on the trigger day
which activated the renin-angiotensin-aldosterone system (22). HCG-induced high hormone levels post
the trigger day also played a role in occurrence of pre-eclampsia.
Moreover, one of the most common complications related to the IVF
technology is the multiple pregnancy. A multiple pregnancy often
increase uterine pressure to an unusually high level, which cause
severe placental ischemia and hypoxia, resulting in vascular
endothelial cell damage and dysfunction. Thus, a multiple pregnancy
is a risk factor for hypertensive disorders in pregnancy (23). It is also arguable that the embryos
obtained from donated eggs were allogeneic to the pregnant mother,
thus immune system attacks inflict damage to the body, and increase
the risk of hypertensive disorders in pregnancy (24).
In this study, the incidence of hypertensive
disorders in pregnancy was higher in the ICSI-ET group than that in
the IVF-ET group. The difference was statistically significant, and
the difference was even more significant in the comparison of twins
in the two groups. This indicates that the ICSI-ET technology, to a
certain extent, increases the risk of hypertensive disorders in
pregnancy. Unlike the routine IVF-ET technology, following the
ICSI-ET protocol, a single normal sperm was placed in a fine needle
under a microscope using external force, followed by piercing of
the zona pellucida and the egg membrane with the needle tip and
injection of the sperm into the follicle pulp to complete
fertilization. In this process of fertilization, the invasive
procedure can create some unfavorable conditions that may impact
the implantation of the embryos and change the endometrial
microenvironment, which can affect the health of the offspring
(25).
In this study, we discovered that frozen-thawed
embryo transfer did not increase the risk of developing
hypertensive disorders in pregnancy. Unlike the fresh embryo
transfer technology, following the frozen-thawed embryo transfer
protocol, the early embryos were frozen for storage, and were
resuscitated before transfer. This technique can increase the
cumulative pregnancy rate of a single ovulation induction/egg
retrieval process. It also allows recovery of the ovary and reduces
patients suffering from multiple periods of egg retrieval, and
therefore it is convenient and economical to patients.
We concluded that the risk of onset of hypertensive
disorders in pregnancy has a certain correlation with the ICSI
fertilization technology, however no apparent correlation with
transfer cycles was detected.
Acknowledgements
This study was supported by the National Natural
Science Fund 8160060698.
References
|
1
|
Myers ER, McCrory DC, Mills AA, Price TM,
Swamy GK, Tantibhedhyangkul J, Wu JM and Matchar DB: Effectiveness
of assisted reproductive technology (ART). Evid Rep Technol Assess
(Full Rep). 167:1–195. 2008.
|
|
2
|
Pinborg A: IVF/ICSI twin pregnancies:
Risks and prevention. Hum Reprod Update. 11:575–593. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ahmad AS and Samuelsen SO: Hypertensive
disorders in pregnancy and fetal death at different gestational
lengths: A population study of 2 121 371 pregnancies. BJOG.
119:1521–1528. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Paoloni-Giacobino A: Epigenetics in
reproductive medicine. Pediatr Res. 61:R51–R57. 2007. View Article : Google Scholar
|
|
5
|
Kanyó K and Konc J: A follow-up study of
children born after diode laser assisted hatching. Eur J Obstet
Gynecol Reprod Biol. 110:176–180. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Halliday J, Oke K, Breheny S, Algar EJ and
Amor D: Beckwith-Wiedemann syndrome and IVF: A case-control study.
Am J Hum Genet. 75:526–528. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang YA, Chughtai AA, Farquhar CM, Pollock
W, Lui K and Sullivan EA: Increased incidence of gestational
hypertension and preeclampsia after assisted reproductive
technology treatment. Fertil Steril. 105:920–926.e2. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hammarberg K, Fisher JR and Rowe HJ:
Women's experiences of childbirth and post-natal healthcare after
assisted conception. Hum Reprod. 23:1567–1573. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Baxi A and Kaushal M: Outcome of twin
pregnancies conceived after assisted reproductive techniques. J Hum
Reprod Sci. 1:25–28. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kintiraki E, Papakatsika S, Kotronis G,
Goulis DG and Kotsis V: Pregnancy-induced hypertension. Hormones
(Athens). 14:211–223. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen ZJ, Shi Y, Sun Y, Zhang B, Liang X,
Cao Y, Yang J, Liu J, Wei D, Weng N, et al: Fresh versus frozen
embryos for infertility in the polycystic ovary syndrome. N Engl J
Med. 375:523–533. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kuklina EV, Ayala C and Callaghan WM:
Hypertensive disorders and severe obstetric morbidity in the United
States. Obstet Gynecol. 113:1299–1306. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jido TA and Yakasai IA: Preeclampsia: A
review of the evidence. Ann Afr Med. 12:75–85. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Stern JE, Luke B, Tobias M, Gopal D,
Hornstein MD and Diop H: Adverse pregnancy and birth outcomes
associated with underlying diagnosis with and without assisted
reproductive technology treatment. Fertil Steril. 103:1438–1445.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Owiredu W, Ahenkorah L, Turpin CA, Amidu N
and Laing EF: Putative risk factors of pregnancy-induced
hypertension among Ghanaian pregnant women. J Med Biomed Sci.
1:62–76. 2012.
|
|
16
|
Mukhopadhaya N and Arulkumaran S:
Reproductive outcomes after in-vitro fertilization. Curr Opin
Obstet Gynecol. 19:113–119. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sibai BM: Subfertility/infertility and
assisted reproductive conception are independent risk factors for
pre-eclampsia. BJOG. 122:9232015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sun LM, Walker MC, Cao HL, Yang Q, Duan T
and Kingdom JC: Assisted reproductive technology and
placenta-mediated adverse pregnancy outcomes. Obstet Gynecol.
114:818–824. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Isaksson R, Gissler M and Tiitinen A:
Obstetric outcome among women with unexplained infertility after
IVF: A matched case-control study. Hum Reprod. 17:1755–1761. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tabcharoen C, Pinjaroen S, Suwanrath C and
Krisanapan O: Pregnancy outcome after age 40 and risk of low birth
weight. J Obstet Gynaecol. 29:378–383. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kurki T, Hiilesmaa V, Raitasalo R, Mattila
H and Ylikorkala O: Depression and anxiety in early pregnancy and
risk for preeclampsia. Obstet Gynecol. 95:487–490. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mikat B, Zeller A, Scherag A,
Drommelschmidt K, Kimmig R and Schmidt M: βhCG and PAPP-A in first
trimester: Predictive factors for preeclampsia? Hypertens
Pregnancy. 31:261–267. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Miyake H, Iwasaki N, Nakai A, Suzuki S and
Takeshita T: The influence of assisted reproductive technology on
women with pregnancy-induced hypertension: A retrospective study at
a Japanese Regional Perinatal Center. J Nippon Med Sch. 77:312–317.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pecks U, Maass N and Neulen J: Oocyte
donation: a risk factor for pregnancy-induced hypertension: a
meta-analysis and case series. Dtsch Arztebl Int. 108:23–31.
2011.PubMed/NCBI
|
|
25
|
Buzzi PJ, Zappacosta MP, Auge L, Isa L,
Obejero EY and Bello A: Beneficial effect of local injury to the
endometrium in intracytoplasmic sperm injection (ICSI) patients
with recurrent implantation failure. Fertil Steril. 102:e2932014.
View Article : Google Scholar
|