Introduction
Retinitis pigmentosa (RP) is an inherited retinal
disease caused by the degeneration of photoreceptors and retinal
pigment epithelium (RPE) within the eye (1). RP is a major cause of acquired
blindness in adults worldwide, occurring in 1 out of every 4,000
individuals (2). RP is characterized
by nyctalopia, progressive visual field contraction and,
ultimately, central visual field loss (3). A clinical diagnosis of RP is largely
based on characteristic fundus changes, decreased
electroretinography (ERG) responses and optical coherence
tomography (OCT) examinations. Previous histological studies have
determined that the death of RPE cells and photoreceptors is the
common progression for all patients with RP. However, while certain
patients with RP lose their vision at a young age, others maintain
central vision for their entire lives without treatment (3). The RP patients with central vision are
able to maintain a relatively normal macular area for an extended
period of time, which is defined as the ‘macular-sparing area’
throughout the present study. Visual field function is associated
with the type of macular lesion the patient has (4) and may be assessed by the observation of
preserved outer retinal lines (5).
With the introduction of spectral domain (SD)-OCT,
it has been possible to obtain structural information on retinal
anatomical abnormalities in patients with RP (6). Previous studies have demonstrated that
three highly reflective lines, including the external limiting
membrane (ELM), the ellipsoid zone (EZ) and the interdigitation
zone in the outer retina are important predictors of visual acuity
(7,8), which is highly correlated with visual
field function (9). However,
patients with RP often have complications, including cataracts,
epiretinal membranes (ERM) and macular edema (10,11),
which makes it difficult to acquire useful information from
traditional fundus images or ophthalmoscopy.
Heidelberg Engineering GmbH (Heidelberg, Germany)
introduced a novel combined instrument, the Spectralis SD-OCT,
which enables the recording of confocal scanning laser
ophthalmoscope (cSLO) and SD-OCT images simultaneously (12). Multicolor imaging uses a cSLO with
three laser wavelengths to acquire reflective images (blue
reflectance, 488 nm; green reflectance, 515 nm; infrared (IR)
reflectance, 820 nm). The Spectralis SD-OCT is able to obtain
detailed structural information and localize pathologic
abnormalities more precisely than previously available instruments.
The present study evaluated the effectiveness of the Spectralis
SD-OCT in defining the macular-sparing area by multicolor imaging
compared with traditional fundus photography. The potential
correlations between the macular-sparing area and the best
corrected visual acuity (BCVA), the visual field and subfoveal
choroidal thickness (SFCT) were also analyzed.
Materials and methods
Inclusion of patients
Between January 2015 and June 2017, 25 patients with
RP (RP group; n=50 eyes) and 35 healthy individuals (control group;
n=70 eyes) were enrolled in the present study at Shanghai Tenth
People's Hospital Affiliated to Tongji University School of
Medicine (Shanghai, China). All participants in the present study
underwent a complete ophthalmic examination, including a BCVA test,
slit lamp biomicroscopy, an intraocular pressure test, a dilated
fundus examination and SD-OCT. Patients with RP were further tested
with full-field ERG, and central visual field and muticolor
imaging.
Patients with RP were diagnosed based on the
presence of nyctalopia, characteristic funduscopic appearance,
constricted visual field and a reduction in full-field ERG.
Individuals with significant media opacities and other intraocular
diseases were excluded from the current study. BCVA is expressed as
the logarithm of the minimum angle of resolution (logMAR). For
calculations, the BCVA of finger counts and hand movement were
designated as 1.6 and 2.0, as previously described (13). The control group participants had a
visual acuity of ≥20/20, ametropic value of <-3.00 D and no
ocular or systemic diseases.
Written informed consent was obtained from all
participants. Procedures followed the tenets of the Declaration of
Helsinki and the present study was approved by the Institutional
Review Board of Shanghai Tenth People's Hospital.
Multicolor imaging
All patients with RP underwent multicolor imaging
using the Spectralis SD-OCT (version 6.0.9) within the central 30
degrees of the visual field. Multicolor imaging uses multiple
colored lasers to selectively capture information on different
retinal structures. The blue laser reflectance produces detailed
views of the retinal nerve fiber layers and epiretinal
abnormalities. The green laser reflectance provides information on
the retinal vasculature and intra-retinal structures, while the IR
laser penetrates into the deepest retinal layers, providing images
of the choroid, RPE cells and photoreceptors (14). Multicolor images are composed of the
reflective images acquired by the three different colored lasers.
SD-OCT scanning combined with multicolor imaging was performed
simultaneously by the Spectralis SD-OCT.
Macular-sparing area measurement
The macular-sparing areas were traced independently
by two physicians. The built-in measurement software programs
within the Spectralis SD-OCT subsequently converted the pixels
selected in the IR images to mm2. The average data from
the results was used for analysis.
SFCT measurement
Enhanced depth imaging scans were used to assess the
SFCT. Single line scans composed of 100 averaged images were
captured to achieve a high quality image. A horizontal scan across
the fovea was selected for the RP and control group, since this is
a precise method for measuring subfoveal choridal thickness
(15). Two experienced OCT readers
measured the SFCT from the inner border of the sclera to the outer
border of the RPE. Detailed information, including serial number,
name, sex and date of birth, was recorded to ensure that individual
participants could be identified following data collection.
Visual field
Static automated perimetry (central 30-2 threshold
program with spot size III; Humphrey 750i; Carl Zeiss Meditec,
Dublin, CA, USA) was performed on patients with RP to determine
their visual field function. The visual field test was performed
once per eye prior to the baseline test to minimize practice
effects. To decrease the duration of the examination a Swedish
interactive threshold algorithm fast strategy was used. Mean
deviation (MD) and pattern standard deviation (PSD) data were
obtained to assess the function of the visual field. MD represents
the average deviation of sensitivity from age-corrected threshold
values, while PSD represents the contiguous irregularities and the
increased value with more irregularities (16).
Statistical analysis
All data were analyzed using SPSS software (version
20.0; IBM Corp., Armonk, NY, USA). An independent samples t-test
was used for comparison of SFCT between the patients with RP and
the controls. The associations between the macular-sparing area and
BCVA, visual field and SFCT were measured using a Spearman's rank
correlation test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Participant inclusion within the
study
In total, 25 patients with RP (50 eyes) underwent
ophthalmic examinations. There were 4 eyes excluded due to
nystagmus and 2 eyes excluded due to severe cataracts. Overall, 44
eyes of 24 patients with RP (14 male and 10 female; age, 26–80
years; mean age, 51.11±13.15 years) were analyzed in the present
study. A total of 70 eyes from 35 healthy participants (20 male and
15 female; age, 25–71 years; mean age, 57.51±10.19 years) were
examined as the control group. No significant differences were
identified in age and gender between the RP group and the control
group. All patients in the RP group had concentric constrictions of
the visual field. The mean MD and PSD were −28.40±4.01 dB and
6.32±3.62 dB, respectively.
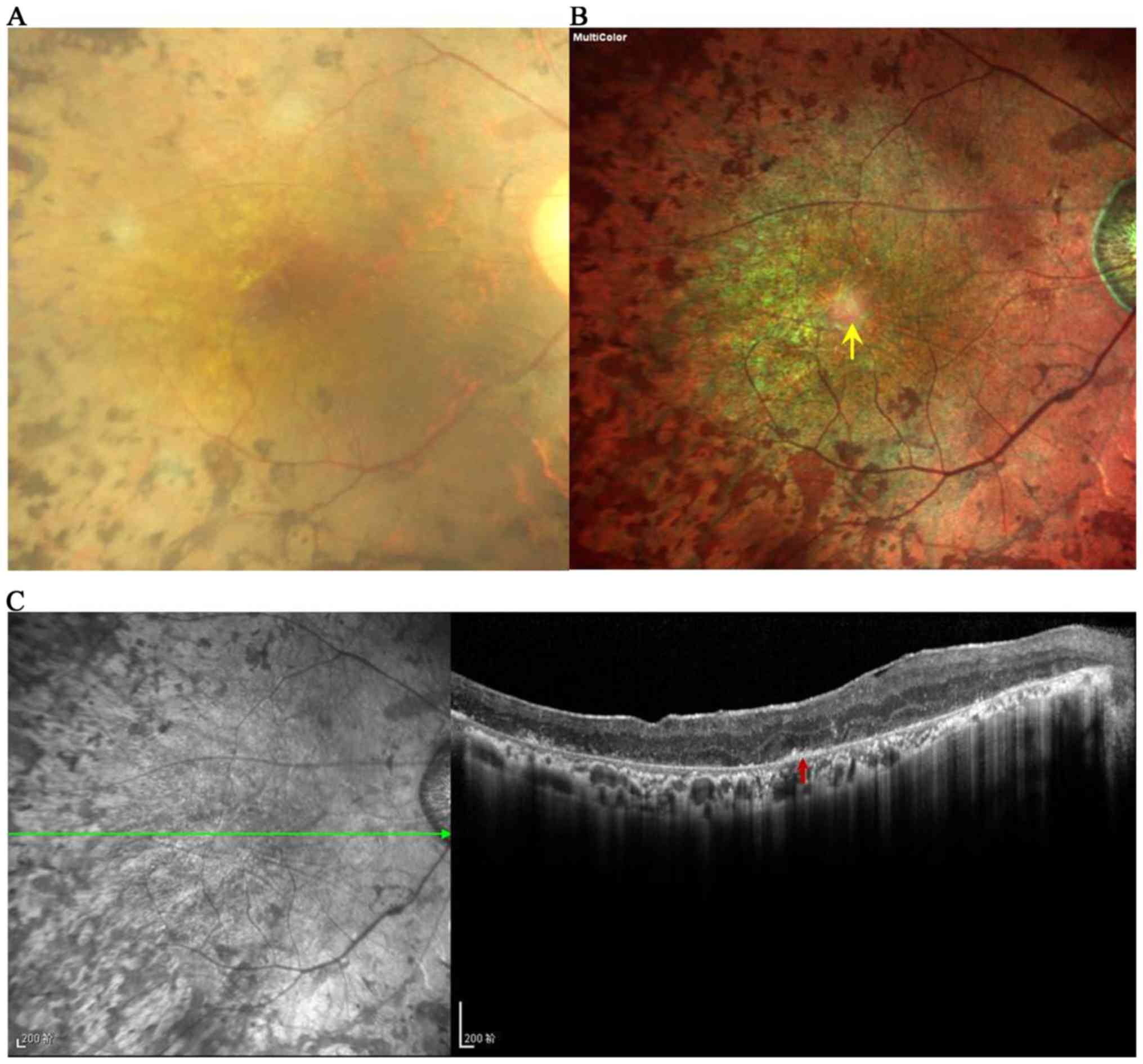
Use of multicolor imaging in the
evaluation of the macular area of a patient with RP with an
ERM
Traditional fundus photography (Fig. 1A) was used to identify the abnormal
macular area, however, the retinal aberrations were difficult to
detect due to the presence of moderate cataracts. Conversely, the
multicolor cSLO image clearly revealed the presence of an ERM and
macular aberrations (Fig. 1B). The
multicolor cSLO image exposed a green macular area with regular
elliptical shape boundaries, indicating the thickening of the
macular retina. Spicule-shaped pigment deposits were also
identified surrounding the macular area. The multicolor image
demonstrates the radiating retinal folds in the ERM and a
moderately healthy macular fovea within the area. A horizontal OCT
B-scan corresponding to the multicolor image is presented in
Fig. 1C, which revealed the ERM, an
irregular RNFL layer, thickening of the macular fovea, a preserved
RPE layer and outer retinal lines.
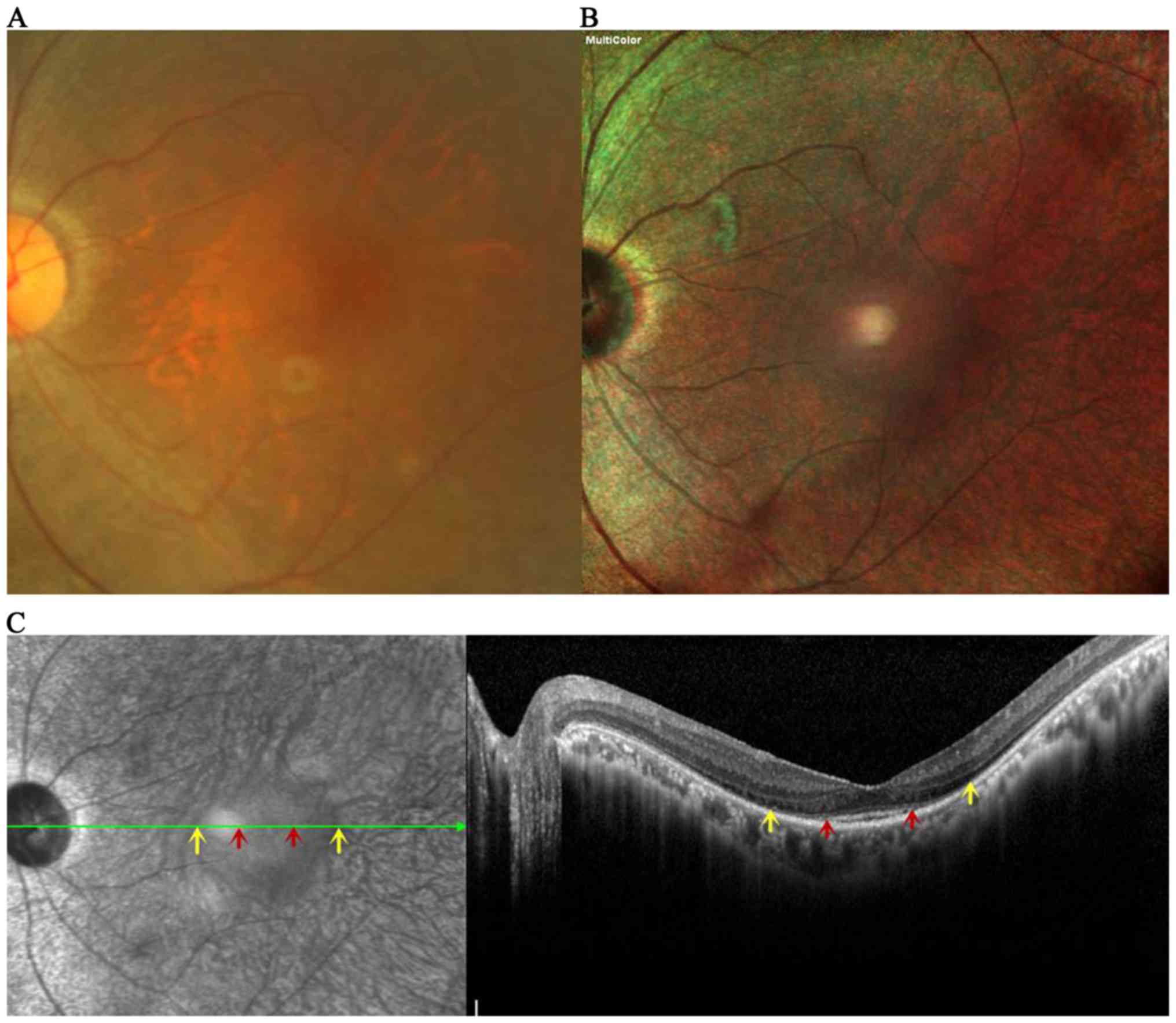
Multicolor imaging for the evaluation
of the macular-sparing area of a patient with RP with a mild
cataract
An individual from the RP group with a regular
macular area and a mild cataract was selected to evaluate the
structural changes of RP using multicolor imaging. In the image
captured using fundus photography it was difficult to distinguish
the exact border of the macular-sparing area due to the cataract
and tissue overlay (Fig. 2A). By
contrast, multicolor imaging is able to acquire structural
information from different layers, and the oblong margins of the
area are well defined on the multicolor image (Fig. 2B). The green line on the IR image
(Fig. 2C) reveals the location of
the horizontal cross-sectional SD-OCT image corresponding to the
adjacent image. The red arrowheads indicate the horizontal
boundaries of the normal reflective area, while the borders of the
hyporeflective ring are shown between the yellow arrowheads on the
IR image. The same anatomical locations of the normal reflective
area indicate the region of the EZ band, while the hyporeflective
ring is characterized by the disrupted ELM line on the SD-OCT
image. While the ELM length was significantly longer than EZ length
within the area, the ELM and EZ lines were absent outside of the
hyporeflective ring.
Multimodal imaging for the evaluation
of the macular-sparing area of a patient with RP
When compared with the fundus photography image in
Fig. 3A, the margins of the
macular-sparing area were well visualized on the multicolor image
and disrupted RPE changes with leopard-spot pigment deposits can be
clearly observed in the periphery of the retina (Fig. 3B). The multicolor image reveals a
normal reflective area surrounded by a hyperreflective ring. The
horizontal OCT exhibits the continuous outer retinal lines (EZ and
ELM) within the normal reflective area, while the hyperreflective
ring corresponds to a thickening ELM area, and the hyporeflective
area coincides with the disrupted ELM line and invisible EZ line
(Fig 3C). Multicolor imaging was
able to provide high resolution images of the macular-sparing area
and visualize more details relating to retinal alterations,
particularly the outer retinal changes, compared with fundus
photography.
Multicolor imaging for the evaluation
of macular features in a patient with RP with irregular
margins
Multimodal images depict features of the fundus. The
macular-sparing area is characterized by a green area on the
multicolor image (Fig. 4A), which
indicates a thickening retina or relatively preserved RPE layer.
The IR reflectance image exhibited a high intergraded agreement of
hyporeflective area with the multicolor image (Fig 4B). The image also revealed abrupt
margins in the nasal and superonasal quadrants, and increased
choroidal signals because of the disruption and loss of
photoreceptors and RPE cells. The outer retinal features are
moderately visualized on the green and blue reflectance images
(Fig. 4C and D). The macular-sparing
area was better outlined on the infrared reflectance image. Within
the macular fovea, the heterogeneous reflectance images indicated
the irregular outer retinal structures. Surrounding the macular
area, bone spicule-shaped pigment deposits could be observed on all
reflectance images (Fig. 4).
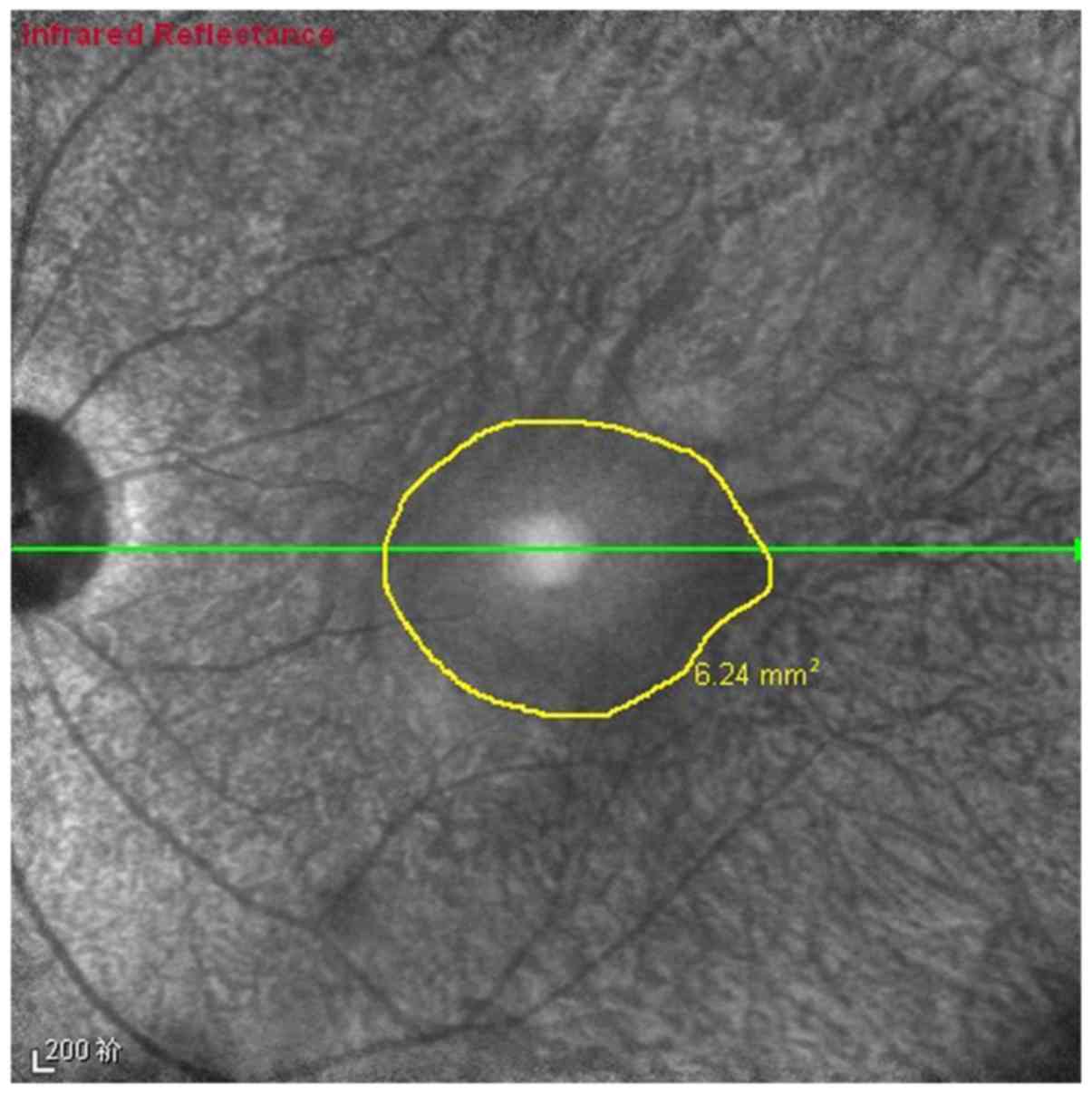
Macular-sparing area measurements
The macular-sparing area was traced independently by
two observers on the IR images (Fig.
5) using built-in measurement software. The size of the area
was calculated by an automatic conversion of pixels to
mm2. The mean size of the area was 18.80±17.72
mm2 in the RP group (data not shown). The size in male
patients was 15.99±16.55 mm2, while in female patients
it was 22.32±19.03 mm2 (data not shown). These results
demonstrate that female patients exhibited a larger macular area,
but that the difference was not significant (data not shown).
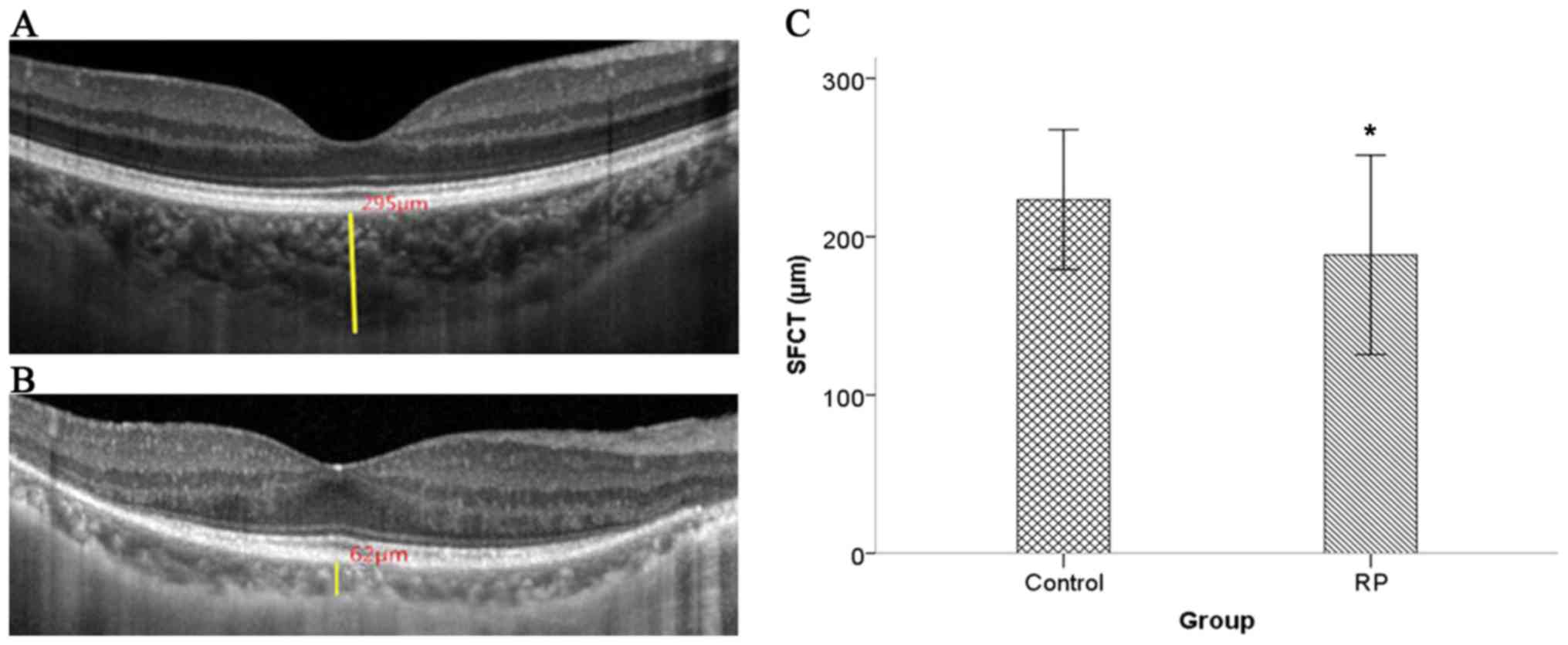
SFCT measurements
SFCT was measured from the inner border of the
sclera to the outer border of the RPE vertically. Images
representing a typical eye from the control and RP groups are
presented in Fig. 6A and B,
respectively. The SFCT measurements were obtained from the OCT
images using a linear measurement tool. The mean SFCT of the
control group was 225.47±60.52 µm, while the mean SFCT of the RP
group was 193.82±62.55 µm (Fig. 6C).
The SFCT was significantly thinner in eyes from the RP group when
compared with the control group (P<0.001).
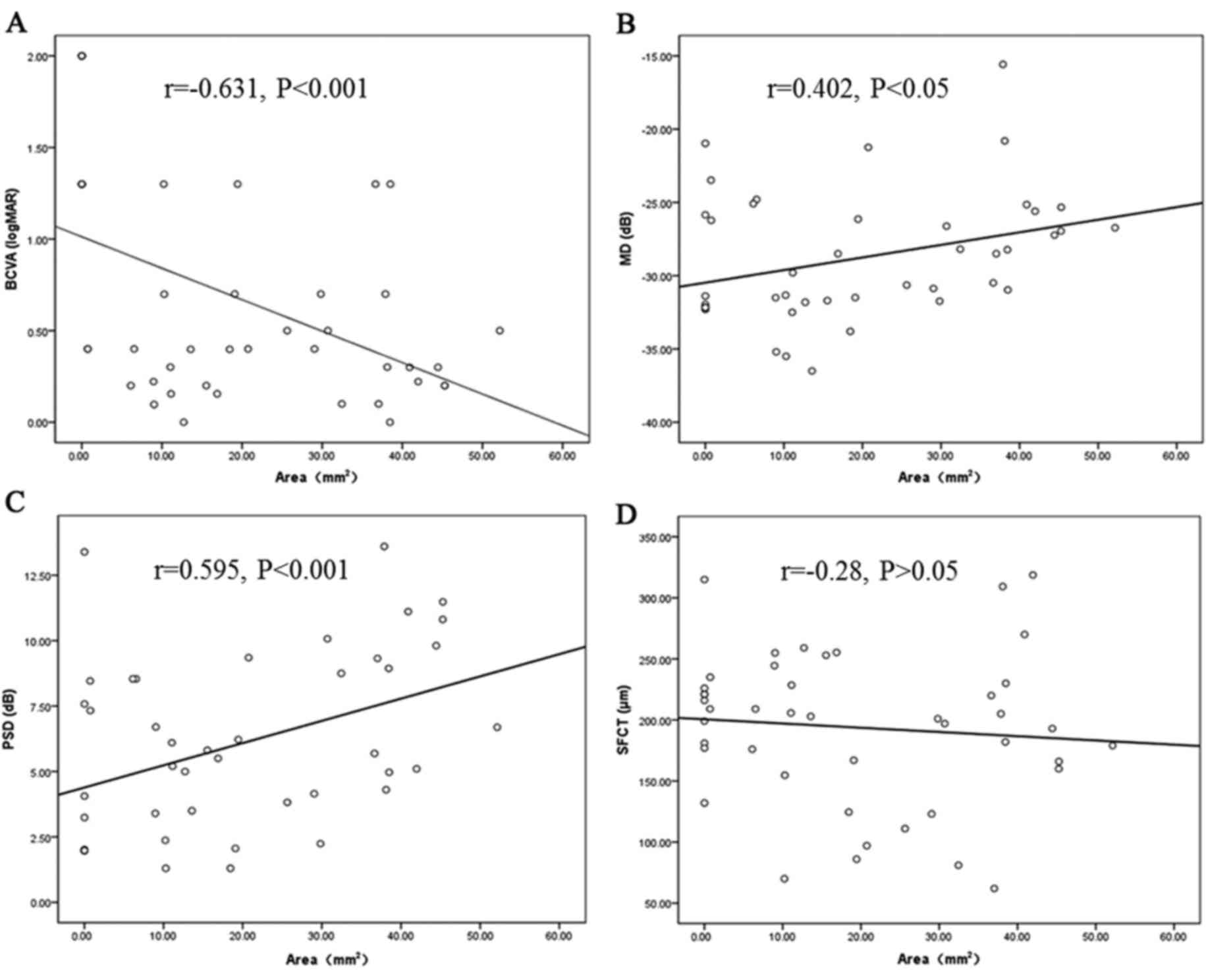
Correlations between the
macular-sparing area size and BCVA, visual field and SFCT
The correlations between the macular-sparing area
and the BCVA, visual field and SFCT were analyzed using a
Spearman's rank correlation test (Fig.
7). There was a significant positive correlation between the
size of the macular-sparing area and BCVA (r=−0.631; P<0.001),
and the visual field in terms of MD (r=0.402; P<0.05) and PSD
(r=0.595; P<0.001). However, no significant correlation was
identified between the macular-sparing area and SFCT (r=−0.28;
P>0.05). These results indicate that the size of the
macular-sparing area is an effective parameter by which to assess
visual function.
Discussion
In clinical practice, certain patients with RP are
able to maintain a relatively normal macular area for an extended
period of time. This normal region has been defined as the
‘macular-sparing area’ throughout the present study. As patients
with RP often have complications, including cataracts (17), ERMs (18) and macular edema (19), it can be difficult to acquire useful
details on the fundus from regular fundus photography.
Improvements in technology may lead to advancements
within the field of ophthalmic imaging; the present study
introduces multicolor imaging as a novel modality that offers
improved visualization of macular clinical features in patients
with RP. Multicolor imaging utilizes multiple colored lasers to
obtain information originating from different retinal structures
simultaneously; it is able to reveal topographic changes within
different retinal layers. It is difficult to demonstrate these
detailed alterations using traditional fundus photography due to
refractive stroma turbidity. In the present study, the potential of
multicolor imaging as a means for evaluating the clinical features
of the macular-sparing area and complications in patients with RP
was investigated. To the best of our knowledge, this is the first
time Spectralis SD-OCT has been used to observe the characteristics
of RP.
In the present study multicolor imaging was used to
visualize the macular-sparing area and variable macular changes in
patients with RP with various complications, including an ERM and
cataracts. Multicolor cSLO imaging demonstrated the radiating
retinal folds and traction retinal area despite the presence of
cataracts. While the margins of the macular-sparing area were
relatively indistinct on traditional fundus photography, the oblong
margins of the area were well defined on the multicolor images.
Multicolor images also depicted the macular-sparing area with a
normal reflective area surrounded by a hyporeflective or
hyperreflective ring, which coincided with the outer retinal
changes. Multicolor imaging was revealed to possess marked
advantages over traditional fundus photography, as it revealed
detailed information about retinal structural changes and depicted
retinal alterations at a high resolution.
The IR reflectance laser provides detailed images of
the choroid, RPE and photoreceptors, which may be used to enhance
understanding of retinal degenerative diseases (20). The Spectralis SD-OCT is a novel
technology that has been confirmed as an excellent tool for the
evaluation of geographic atrophy secondary to age-related macular
degeneration (21). The present
study identified that the IR reflectance laser image was able to
visualize irregular macular alterations, while they were poorly
discerned on the blue and green laser reflectance images.
The normal reflective area was identified as being
surrounded by either a hyporeflective or hyperreflective ring on
the multicolor SLO images. This suggests that certain
microstructure anomalous changes may lead to the different
appearances of retinal alterations. The present study demonstrated
that continuous outer retinal lines were responsible for the normal
reflective area. A disrupted ELM line, combined with an invisible
EZ line may be presented as a hyporeflective ring surrounding the
healthy macular fovea. ELM line thickening as a result of EZ
disruption may be associated with the hyperreflective ring, which
suggests that ELM remolding occurs to increase the ELM thickness.
Outside of the hyporeflective or hyperreflective ring, ELM and EZ
lines were absent. A morphologic association between the features
on multicolor images and the outer retinal changes on the OCT scans
has been identified. Thus, multicolor imaging may be a useful
method of detecting subtle changes and providing structural
information that could previously only be revealed through an OCT
examination.
As the macular-sparing area reflects the outer
retinal line changes, it was hypothesized that an association
between the macular-sparing area and visual function exists. The
results of the present study revealed a significant correlation
between the size of macular-sparing area and BCVA. This is
consistent with the results of previous studies, where ELM and EZ
lines were identified as being significantly correlated with BCVA
(5,22,23).
Patients with advanced RP without outer retinal lines exhibit
poorer BCVA. However, certain patients with RP who have
disorganized segments exhibit abnormal changes in the outer retinal
lines as well as the inner retinal layers (8). This influences the BCVA, resulting in a
moderate association between the macular-sparing area and BCVAs.
The results of the present study demonstrated that multicolor
imaging of the macular-sparing area may be another useful parameter
by which to evaluate the visual function of patients with RP.
The visual field is associated with OCT parameters
(24) and represents another
important method of diagnosing RP. The results of the present study
demonstrated that the MD and PSD of the visual field were
positively correlated with the size of the macular-sparing area;
thus indicating that a larger healthy macular area represents a
wider visual field. These results are consistent with previous
studies, which concluded that the thickness of the photoreceptor
outer segments decreased linearly with the loss of visual field
(25,26). However, the visual field is
influenced by a number of other factors, including RNFL thickness
and patient compliance (27). This
means that the correlation between the macular-sparing area and the
visual field needs to be investigated in a larger number of
individuals with RP to confirm the findings of the present
study.
RP is characterized by the degeneration of
photoreceptors and RPE cells, in addition to variable choroid
atrophy (28). The IR laser was able
to penetrate the deepest retinal layers and provide detailed
information on choroidal changes. The outer retinal layers are
supplied by choroidal capillaries and it was hypothesized that
there may be an association between SFCT and the size of the
macular-sparing area. However, while SFCT was identified as being
reduced in all individuals within the RP group, there was no
significant correlation identified between the SFCT and the size of
the macular-sparing area. RPE-derived vascular endothelial growth
factor is one of the most important factors involved in the
maintenance of normal choriocapillaris (29,30),
however, the subfoveal choroidal thickness may be maintained for an
extended period of time while the macular-sparing area exists. The
outer retinal layers may be mainly associated with the
choriocapillary layer as opposed to the whole choroid thickness
(31), so a device that is able to
measure choriocapillary thickness is required. Further research to
measure additional sites and the choriocapillary layer is required
to confirm the association between choroidal thickness and the size
of the macular-sparing area.
In conclusion, the results of the present study
indicate that multicolor imaging is an effective, novel approach to
defining the macular-sparing area and visualizing macular
aberrations in patients with RP. Multicolor imaging is able to
identify more subtle retinal alterations, and more objective and
quantitative information compared with traditional fundus
photography. Multicolor imaging is also able to visualize the
intact outer retinal structures regardless of complications,
including cataracts and ERM. Therefore, multicolor imaging
represents a useful tool to investigate macular structural changes
and their association with visual function in patients with RP. It
was also identified that there is a significant positive
correlation between the size of the macular-sparing area and visual
field function and BCVA.
Acknowledgements
The present study was supported by the Shen Kang
Hospital Development Center (grant no. SHDC12010207).
References
|
1
|
Mrejen S, Audo I, Bonnel S and Sahel JA:
Retinitis pigmentosa and other dystrophies. Dev Ophthalmol.
58:191–201. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hartong DT, Berson EL and Dryja TP:
Retinitis pigmentosa. Lancet. 368:1795–1809. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Berson EL: Long-term visual prognoses in
patients with retinitis pigmentosa: The ludwig von sallmann
lecture. Exp Eye Res. 85:7–14. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Flynn MF, Fishman GA, Anderson RJ and
Roberts DK: Retrospective longitudinal study of visual acuity
change in patients with retinitis pigmentosa. Retina. 21:639–646.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aizawa S, Mitamura Y, Hagiwara A, Sugawara
T and Yamamoto S: Changes of fundus autofluorescence, photoreceptor
inner and outer segment junction line, and visual function in
patients with retinitis pigmentosa. Clin Exp Ophthalmol.
38:597–604. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Drexler W, Sattmann H, Hermann B, Ko TH,
Stur M, Unterhuber A, Scholda C, Findl O, Wirtitsch M, Fujimoto JG
and Fercher AF: Enhanced visualization of macular pathology with
the use of ultrahigh-resolution optical coherence tomography. Arch.
Ophthalmol. 121:695–706. 2003.
|
|
7
|
Sun LW, Johnson RD, Langlo CS, Cooper RF,
Razeen MM, Russillo MC, Dubra A, Connor TB Jr, Han DP, Pennesi ME,
et al: Assessing photoreceptor structure in retinitis pigmentosa
and usher syndrome. Invest Ophthalmol Vis Sci. 57:2428–2442. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu G, Li H, Liu X, Xu D and Wang F:
Structural analysis of retinal photoreceptor ellipsoid zone and
postreceptor retinal layer associated with visual acuity in
patients with retinitis pigmentosa by ganglion cell analysis
combined with OCT imaging. Medicine (Baltimore). 95:e57852016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fischer MD, Fleischhauer JC, Gillies MC,
Sutter FK, Helbig H and Barthelmes D: A new method to monitor
visual field defects caused by photoreceptor degeneration by
quantitative optical coherence tomography. Invest Ophthalmol Vis
Sci. 49:3617–3621. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chan TCY, Lam SC, Mohamed S and Wong RLM:
Survival analysis of visual improvement after cataract surgery in
advanced retinitis pigmentosa. Eye (Lond). Aug 4–2017.(Epub ahead
of print). doi: 10.1038/eye.2017.164. View Article : Google Scholar
|
|
11
|
Ikeda Y, Yoshida N, Murakami Y, Nakatake
S, Notomi S, Hisatomi T, Enaida H and Ishibashi T: Long-term
surgical outcomes of epiretinal membrane in patients with
retinitis. Sci Rep. 5:130782015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pang CE and Freund KB: Ghost maculopathy:
An artifact on near-infrared reflectance and multicolor imaging
masquerading as chorioretinal pathology. Am J Ophthalmol.
158:171–178. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wen Y, Klein M, Hood DC and Birch DG:
Relationships among multifocal electroretinogram amplitude, visual
field sensitivity, and SD-OCT receptor layer thicknesses in
patients with retinitis pigmentosa. Invest Ophthalmol Vis Sci.
53:833–840. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sergott RC: Retinal segmentation using
multicolor laser imaging. J Neuroophthalmol. 34 Suppl:S24–S28.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zeng J, Li J, Liu R, Chen X, Pan J, Tang S
and Ding X: Choroidal thickness in both eyes of patients with
unilateral idiopathic macular hole. Ophthalmology. 119:2328–2333.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lemke S, Cockerham GC, Glynn-Milley C, Lin
R and Cockerham KP: Automated perimetry and visual dysfunction in
blast-related traumatic brain injury. Ophthalmology. 123:415–424.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Andjelic S, Drašlar K, Hvala A and Hawlina
M: Anterior lens epithelium in cataract patients with retinitis
pigmentosa - scanning and transmission electron microscopy study.
Acta Ophthalmol. 95:e212–e220. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fujiwara K, Ikeda Y, Murakami Y, Nakatake
S, Tachibana T, Yoshida N, Nakao S, Hisatomi T, Yoshida S,
Yoshitomi T, et al: Association between aqueous flare and
epiretinal membrane in retinitis pigmentosa. Invest Ophthalmol Vis
Sci. 57:4282–4286. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Strong S, Liew G and Michaelides M:
Retinitis pigmentosa-associated cystoid macular oedema:
Pathogenesis and avenues of intervention. Br J Ophthalmol.
101:31–37. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Semoun O, Guigui B, Tick S, Coscas G,
Soubrane G and Souied EH: Infrared features of classic choroidal
neovascularisation in exudative age-related macular degeneration.
Br J Ophthalmol. 93:182–185. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ben Moussa N, Georges A, Capuano V, Merle
B, Souied EH and Querques G: MultiColor imaging in the evaluation
of geographic atrophy due to age-related macular degeneration. Br J
Ophthalmol. 99:842–847. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yoon CK and Yu HG: The structure-function
relationship between macular morphology and visual function
analyzed by optical coherence tomography in retinitis pigmentosa. J
Ophthalmol. 2013:8214602013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Smith TB, Parker M, Steinkamp PN, Weleber
RG, Smith N and Wilson DJ: VPA Clinical Trial Study Group; EZ
Working Group: Structure-function modeling of optical coherence
tomography and standard automated perimetry in the retina of
patients with autosomal dominant retinitis pigmentosa. PLoS One.
11:e01480222016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fischer MD, Fleischhauer JC, Gillies MC,
Sutter FK, Helbig H and Barthelmes D: A new method to monitor
visual field defects caused by photoreceptor degeneration by
quantitative optical coherence tomography. Invest Ophthalmol Vis
Sci. 49:3617–3621. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wakabayashi T, Sawa M, Gomi F and
Tsujikawa M: Correlation of fundus autofluorescence with
photoreceptor morphology and functional changes in eyes with
retinitis pigmentosa. Acta Ophthalmol. 88:e177–e183. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wen Y and Birch DG: Outer segment
thickness predicts visual field response to QLT091001 in patients
with RPE65 or LRAT mutations. Transl Vis Sci Technol. 4:82015.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rao HL, Raveendran S, James V, Dasari S,
Palakurthy M, Reddy HB, Pradhan ZS, Rao DA, Puttaiah NK and Devi S:
Comparing the performance of compass perimetry with humphrey field
analyzer in eyes with glaucoma. J Glaucoma. 26:292–297. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Miyata M, Hata M, Ooto S, Ogino K, Gotoh
N, Morooka S, Hasegawa T, Hirashima T, Sugahara M, Kuroda Y, et al:
Choroidal and retinal atrophy of bietti crystalline dystrophy
patients with CYP4V2 mutations compared to retinitis pigmentosa
patients with eys mutations. Retina. 37:1193–1202. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Saint-Geniez M, Kurihara T, Sekiyama E,
Maldonado AE and D'Amore PA: An essential role for RPE-derived
soluble VEGF in the maintenance of the choriocapillaris. Proc Natl
Acad Sci USA. 106:pp. 18751–18756. 2009, View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ohlmann A, Scholz M, Koch M and Tamm ER:
Epithelial-mesenchymal transition of the retinal pigment epithelium
causes choriocapillaris atrophy. Histochem Cell Biol. 146:769–780.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Adhi M, Regatieri CV, Branchini LA, Zhang
JY, Alwassia AA and Duker JS: Analysis of the morphology and
vascular layers of the choroid in retinitis pigmentosa using
spectral-domain OCT. Ophthalmic Surg Lasers Imaging Retina.
44:252–259. 2013. View Article : Google Scholar : PubMed/NCBI
|