Introduction
The incidence of diabetes is alarmingly high and has
shown no signs of decreasing its upward trend. Beyond the burden of
disease that diabetes itself presents, complications of diabetes
can also seriously affect a patient's health. Among complications
of diabetes, diabetic retinopathy is the most serious eye disease
as it may cause blindness. The primary cause of diabetic
retinopathy is long-term hyperglycemia; that is, diabetic
retinopathy is correlated with the severity and duration of
hyperglycemia (1). It is predicted
that the number of patients with diabetes in the United States will
reach 25 million by 2030, and the number of patients with diabetic
retinopathy by then will reach 300 million worldwide (2).
Development of diabetic retinopathy is related to a
variety of factors, including neovascularization, in which vascular
endothelial growth factor (VEGF) plays a pivotal role in every step
(3,4). VEGF can promote the migration, division
and proliferation of endothelial cells; improve the activity of
plasma plasminogen activators; and can activate gene expression in
endothelial cells, leading to neovascularization (5,6). Studies
have shown that matrix metalloproteinase-9 (MMP-9) also plays an
important role in neovascularization. In addition, monocyte
chemoattractant protein-1 (MCP-1) plays essential roles in the
progression of various complications of diabetes (7–9).
Based on the pathogenesis of diabetic retinopathy, a
variety of drugs have been developed, such as antioxidants, aldose
reductase inhibitors, antiplatelet drugs, and drugs that can
inhibit the formation of advanced glycation end products; however,
the application of these drugs are still challenged by the medical
community due to uncertain efficacy and adverse side effects
(10). The treatment of diabetes has
a long history in Chinese medicine. Studies have shown that Chinese
medicine can significantly improve diabetes and its related
complications. Pharmacological studies on traditional Chinese
medicine also provide a reference for further use of traditional
Chinese medicine in treatment of diabetes (11). Quercetin, as a component of
traditional Chinese medicine, functions as an antioxidant and in
aldose reductase inhibition. In this study, the effects of
quercetin on rats with diabetic retinopathy were investigated by
assessing its influence on various molecular factors implicated in
the pathogenesis of the disease.
Materials and methods
Materials and reagents
Quercetin and streptozotocin (STZ) were purchased
from Sigma (New York, NY, USA); MCP-1, MMP-9, VEGF and an
enzyme-linked immunosorbent assay (ELISA) kit were purchased from
Nanjing Jiancheng Bioengineering Institute (Nanjing, China); rabbit
anti-rat primary polyclonal antibodies of MCP-1, MMP-9 and VEGF
(dilution, 1:500; cat. nos. 10194-1-AP, 14552-1-AP and 19003-1-AP)
and Goat anti-rabbit HRP-labeled secondary polyclonal antibody were
purchased from Proteintech (Wuhan, China) (dilution, 1:2,000; cat.
no. SA00001-2); primer synthesis, reverse transcription kit and a
real-time PCR kit were purchased from Takara (Dalian, China); and a
BCA protein quantitation kit and cell lysate was purchased from
Beyotime (Nantong, China).
Experimental animal grouping and
sample collection
Thirty healthy male Sprague-Dawley rats (180–220 g)
were used in the study (SLAC Laboratory Animal Co., Ltd., Shanghai,
China). Twenty of the rats were randomly selected and fasted for 24
h, followed by intraperitoneal injection of STZ dissolved in a 2%
citric acid buffer (60 mg/kg dosage). Blood was extracted from the
tail vein 72 h later and all 20 rats showed a blood glucose level
>16.7 mmol/l, indicating successfully established diabetes. The
other 10 rats were treated with an intraperitoneal injection of the
same amount of 2% citric acid buffer to serve as a control. The 20
rats with diabetes were further divided randomly into 2 groups,
including a model group and a quercetin group, with 10 rats in each
group. Rats in the quercetin group were treated with an
intragastric injection of quercetin (150 mg/kg), while the same
amount of sodium carboxymethyl cellulose (CMCNa) was used for rats
in the model group and the control group. Treatment was performed
once per day. Blood samples were extracted from the tail vein of
rats in each group at 0, 10 and 20 weeks after the first treatment
and a blood glucose meter was used to measure blood glucose. After
treatment for 20 weeks, the rats were anesthetized with 10% chloral
hydrate (3 mg/kg). Blood was extracted from the inferior cava vein
and the rats were then sacrificed. Eyeballs were collected and the
ocular anterior segment and retina were removed and stored at −80°C
to be used later for RT-PCR and western blot analysis. The right
eyeball was fixed in 4% paraformaldehyde solution, followed by
dehydration by passing over a series of graded ethanol
concentrations. Dehydrated eyeballs were then treated with xylene
to make them transparent. After paraffin embedding, the eyeballs
were cut into sections for H&E staining. The study was approved
by the Ethics Committee of Renmin Hospital of Wuhan University
(Hubei, China).
ELISA to detect levels of MCP-1, MMP-9
and VEGF in serum of rats
The levels of MCP-1, MMP-9 and VEGF in the serum of
each group were detected by ELISA. All operations were performed in
strict accordance with the instructions of the kit. Each sample was
tested three times with two technique repetitions performed each
time.
RT-PCR to detect expression of MCP-1,
MMP-9 and VEGF mRNA in rat retina
Retinal tissue of the rats was collected and total
RNA was extracted. Concentration and purity of RNA were measured
and only the samples with a ratio of A260/A280 between 1.8 and 2.0
were used. Reverse transcription was performed according to the
instructions of the kit and the synthesized cDNA was used as a
template for RT-PCR reaction. All primer sequences are listed in
Table I. PCR reaction conditions
were as follows: 94°C for 5 min, followed by 30 cycles of 94°C for
30 sec, then 57°C for 30 sec, 72°C for 30 sec and 72°C for 5 min.
Ct values were processed using the 2−ΔCt method: ΔCt
(target gene) = Ct (target gene)-Ct (control gene).
 | Table I.Primers for MCP-1, MMP-9 and VEGF used
in RT-PCR. |
Table I.
Primers for MCP-1, MMP-9 and VEGF used
in RT-PCR.
| Genes | Primer sequences |
|---|
| VEGF | F:
5-TTTCGGGAACTAGACCTCTCACC-3 |
|
| R:
5-CTTCATGTCAGGCTTTCTGGATT-3 |
| MMP-9 | F:
5-CCCCCGAGACCTGAAAACCT-3′ |
|
| R:
5-TGATGTTATGATGGTGCCACTTGA-3 |
| MCP-1 | F:
5-CCCACTCACCTGCTGCTACTC-3 |
|
| R:
5-AGAAGTGCTTGAGGTGGTTGTG-3 |
| GAPDH | F:
5-GCACCGTCAAGGCTGAGAAC-3 |
|
| R:
5-TGGTGAAGACGCCAGTGGA-3 |
Western blot analysis to detect the
expression of MCP-1, MMP-9 and VEGF in rat retina
Frozen rat retinal tissue was used to extract total
protein content. Protein concentration was then measured. After
processing, protein samples (50 µg) were subjected to SDS-PAGE
electrophoresis, followed by transfer to a PVDF membrane. The
membrane was blocked with blocking solution at room temperature for
1 h, followed by incubation with the primary antibody overnight at
4°C. After washing with TTBS, the membrane was incubated with the
secondary antibody (1:2,000) at room temperature for 1 h. After
washing with TTBS, color development was performed and images were
taken.
Statistical analysis
The data are expressed as mean ± standard deviation
and processed using SPSS 17.0 (IBM Corp., New York, NY, USA).
Comparisons between 2 groups were performed using t-test and
P<0.05 was considered to be statistically significant.
Results
Effects of quercetin on blood glucose
in rats with diabetes
The changes in blood glucose in each group are shown
in Table II. Compared with the
control group, blood glucose was significantly increased in the
model group and the quercetin group (P<0.01). During the whole
experiment, no significant difference in blood glucose levels was
found between the model group and the quercetin group (P>0.05),
indicating that quercetin has no effects on blood glucose
levels.
 | Table II.Changes in blood glucose levels
(mmol/l) in each group. |
Table II.
Changes in blood glucose levels
(mmol/l) in each group.
| Time (weeks) | Control group | Model group | Quercetin group |
|---|
| 0 | 4.68±0.21 | 4.75±0.16 | 4.81±0.12 |
| 10 | 4.71±0.14 |
23.33±3.15a |
22.92±3.9a |
| 20 |
4.82±0.19a |
24.22±2.9a |
24.17±3.4a |
Effects of quercetin on histological
changes of rat retina
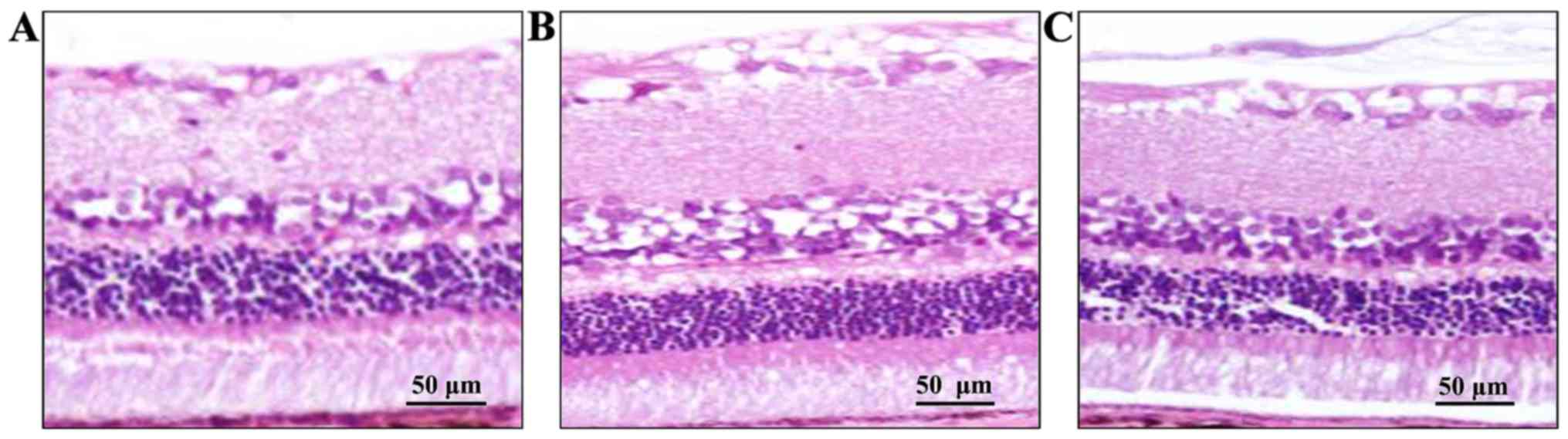
Retinal tissue was observed under optical microscope
(Olympus, Tokyo, Japan). As shown in Fig. 1 retinal tissue in the control group
was intact and the layers of retina were clear and regularly
arranged. Retinal tissue in the model group was thinner than that
of the control group and the structure was loose and cell
vacuolization was observed. Compared with the model group,
histological changes of the retina were improved in the quercetin
group, while edema and cell vacuolization were still observed
compared with the control group.
Effects of quercetin on serum levels
of MCP-1, MMP-9 and VEGF
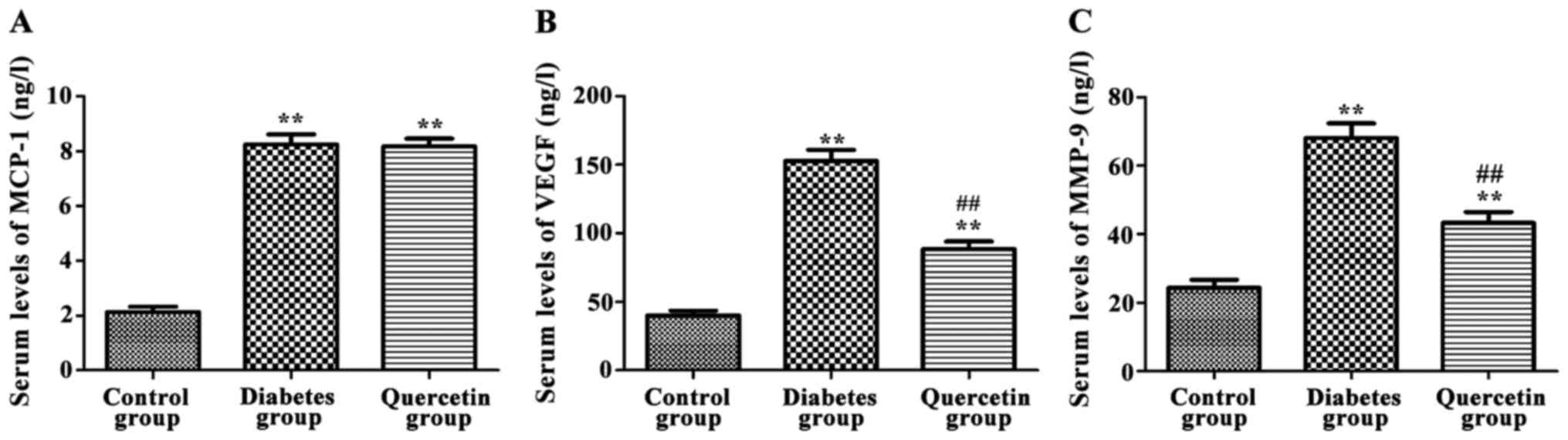
As shown in Fig. 2,
compared with control group, serum levels of MCP-1, MMP-9 and VEGF
were significantly increased in the model group (P<0.01).
Compared with the model group, serum levels of MMP-9 and VEGF were
significantly decreased in the quercetin group (P<0.01), but no
significant changes in serum levels of MCP-1 were observed
(P>0.05), indicating that quercetin could significantly decrease
serum levels of MMP-9 and VEGF, but not MCP-1.
Effects of quercetin on expression of
MCP-1, MMP-9 and VEGF mRNA in rat retina
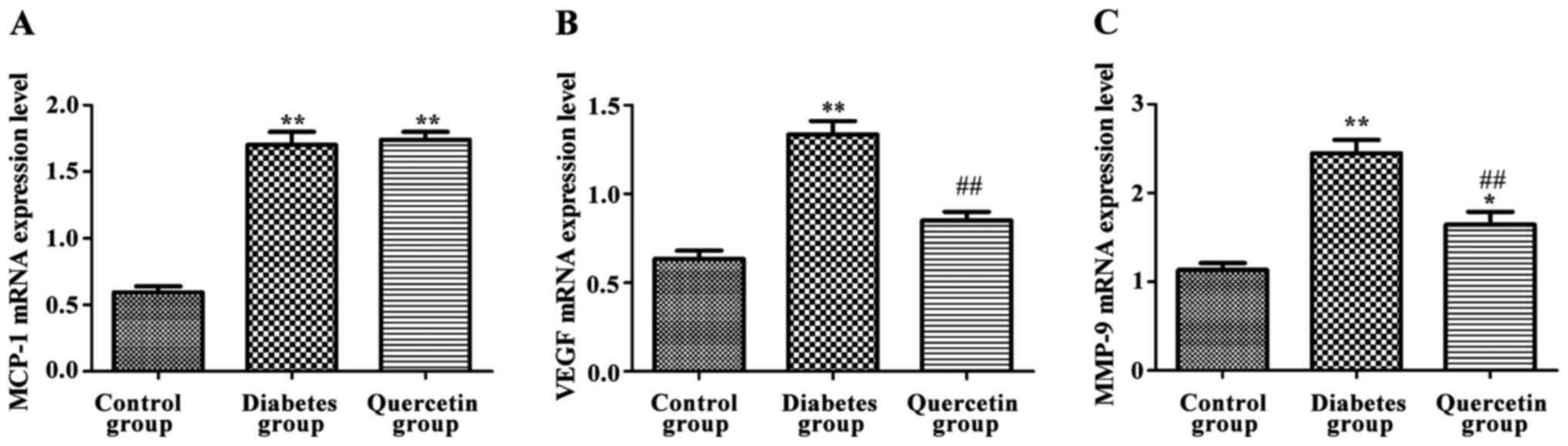
As shown in Fig. 3,
compared with the control group, expression of MCP-1, MMP-9 and
VEGF mRNA of the retina were significantly increased in the model
group (P<0.01). Compared with the model group, the expression
levels of MMP-9 and VEGF mRNA were significantly decreased in the
quercetin group (P<0.01), but no significant changes in the
expression level of MCP-1 was observed (P>0.05), indicating that
quercetin could significantly decrease the expression of MMP-9 and
VEGF mRNA, but not MCP-1 mRNA.
Effects of quercetin on the expression
of MCP-1, MMP-9 and VEGF protein in rat retina
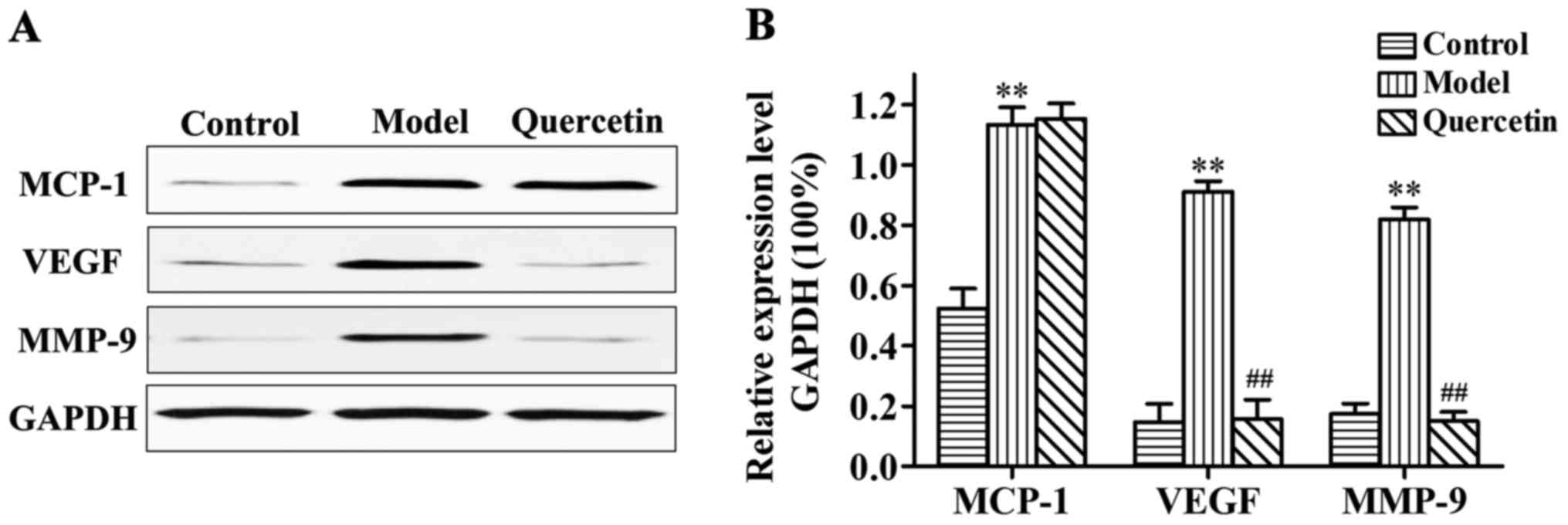
As shown in Fig. 4,
compared with control group, the expression of MCP-1, MMP-9 and
VEGF protein in retina were significantly increased in the model
group (P<0.01). Compared with the model group, expression levels
of MMP-9 and VEGF protein were significantly decreased in the
quercetin group (P<0.01), but no significant changes in the
expression levels of MCP-1 were observed (P>0.05), indicating
that quercetin could significantly decrease the expression levels
of MMP-9 and VEGF protein, but not the inflammatory mediator
protein, MCP-1.
Discussion
Diabetic retinopathy is one of the most common and
severe complications of diabetes. It has been shown that diabetic
retinopathy is the main cause of blindness in developed countries.
The disease is characterized by early high perfusion that can cause
significant expansion and deformation of capillaries, leading to
damage to the retina barrier. Progression of the disease is
characterized by capillary occlusion, bleeding and even the
formation of new blood vessels (12). Extensive research into the
pathogenesis, clinical treatment and other aspects of diabetic
retinopathy has been conducted by researchers. However, the
pathogenesis of diabetic retinopathy caused by early diabetes is
still unclear and effective clinical treatment is still lacking
(13).
In the course of diabetes progression, disorders of
glyco-metabolism are the leading causes of diabetic retinopathy.
Other molecular factors, such as MMPs, inflammatory mediators
(e.g., MCP-1) and VEGF are also involved (14–16). The
main process of neovascularization includes the degradation of
extracellular matrix by vascular endothelial cells, migration and
proliferation of endothelial cells and the synthesis of new matrix
components (17). Formation of new
blood vessels, which plays a pivotal role in the progression of
diabetic retinopathy, can also fundamentally affect the development
of the body, wound healing and reproduction (18). In addition, degradation of the
basement membrane is also an important step in the formation of new
blood vessels. MMP plays an important role in the reconstruction of
the basement membrane. According to the different structures, MMP
can be divided into two categories: membrane-type MMP and
secreted-type MMP. There are three types of secreted-type MMP,
including matrixase, such as MMP-3 and MMP-10, collagenase, such as
MMP-1 and MMP-8, and gelatinase, such as MMP-2 and MMP-9. Studies
have shown that MMP plays an important role in the formation of
neovascularization, especially MMP-9, which is involved in the
formation of vascular endothelial cells during the development of
new blood vessels (19,20). MCP-1, as a member of the family of
inflammatory factors and chemokines, exerts its roles mainly
through paracrine and autocrine. MCP-1 can induce the migration and
infiltration of macrophages and monocytes and plays an important
role in the activation of mononuclear phagocytic cells and
inflammation (21). Studies have
shown that MCP-1 expression is increased in the vitreous, retinal
vessel wall and related cells in diabetic retinopathy. In addition,
expression levels of TNF-α are positively correlated with MCP-1
expression (22).
In this study, STZ was used to establish a diabetic
rat model and increased blood glucose levels indicate the
successful establishment of the model. The aim of this study was to
investigate the effects of quercetin on the expression of MCP-1,
MMP-9 and VEGF in rats with diabetic retinopathy. Results showed no
significant differences in blood glucose levels between the model
group and the quercetin group, indicating that quercetin has no
effects in reducing blood glucose. Therefore, the effects of
quercetin on diabetic retinopathy were not achieved by reducing the
level of blood glucose. Histological results from this study found
that quercetin can reduce the pathological changes caused by
diabetes, such as retinal tissue edema and cell vacuolization.
ELISA results showed that, compared with rats in the control group,
serum levels of MCP-1, MMP-9 and VEGF were significantly increased
in the model group. Compared with the model group, serum levels of
MMP-9 and VEGF were significantly decreased in the quercetin group,
but no significant differences in serum levels of MCP-1 were found
between these two groups. RT-PCR and western blot analysis showed
that, compared with the control group, the expression of MCP-1,
MMP-9 and VEGF mRNA and protein in the retina were significantly
increased in the model group. Compared with the model group,
expression levels of MMP-9 and VEGF mRNA and protein were
significantly decreased in quercetin group, but no significant
differences in the expression of MCP-1 mRNA and protein were found
between these two groups.
In conclusion, the findings of this study indicate
that quercetin can protect rats from the damage caused by
STZ-induced diabetic retinopathy, and its effects may be achieved
by down-regulating expression levels of MMP-9 and VEGF, but not
MCP-1.
References
|
1
|
Funatsu H, Yamashita H, Nakamura S, Mimura
T, Eguchi S, Noma H and Hori S: Vitreous levels of pigment
epithelium-derived factor and vascular endothelial growth factor
are related to diabetic macular edema. Ophthalmology. 113:294–301.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Qaum T, Xu Q, Joussen AM, Clemens MW, Qin
W, Miyamoto K, Hassessian H, Wiegand SJ, Rudge J, Yancopoulos GD,
et al: VEGF-initiated blood-retinal barrier breakdown in early
diabetes. Invest Ophthalmol Vis Sci. 42:2408–2413. 2001.PubMed/NCBI
|
|
3
|
Kant S, Seth G and Anthony K: Vascular
endothelial growth factor-A (VEGF-A) in vitreous fluid of patients
with proliferative diabetic retinopathy. Ann Ophthalmol (Skokie).
41:170–173. 2009.PubMed/NCBI
|
|
4
|
Eichler W, Yafai Y, Keller T, Wiedemann P
and Reichenbach A: PEDF derived from glial Müller cells: A possible
regulator of retinal angiogenesis. Exp Cell Res. 299:68–78. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jorge R, Costa RA, Calucci D, Cintra LP
and Scott IU: Intravitreal bevacizumab (Avastin) for persistent new
vessels in diabetic retinopathy (IBEPE study). Retina.
26:1006–1013. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang SX, Wang JJ, Gao G, Parke K and Ma
JX: Pigment epithelium-derived factor downregulates vascular
endothelial growth factor (VEGF) expression and inhibits VEGF-VEGF
receptor 2 binding in diabetic retinopathy. J Mol Endocrinol.
37:l–12. 2006. View Article : Google Scholar
|
|
7
|
Kim JO, Lee GD, Kwon JH and Kim KS:
Anti-diabetic effects of new herbal formula in neonatally
streptozotocin-induced diabetic rats. Biol Pharm Bull. 32:421–426.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Forsyth PA, Wong H, Laing TD, Rewcastle
NB, Morris DG, Muzik H, Leco KJ, Johnston RN, Brasher PM,
Sutherland G, et al: Gelatinase-A (MMP-2), gelatinase-B (MMP-9) and
membrane type matrix metalloproteinase-1 (MT1-MMP) are involved in
different aspects of the pathophysiology of malignant gliomas. Br J
Cancer. 79:1828–1835. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Robison WG Jr, Laver NM, Jacot JL,
Chandler ML, York BM and Glover JP: Efficacy of treatment after
measurable diabetic-like retinopathy in galactose-fed rats. Invest
Ophthalmol Vis Sci. 38:1066–1073. 1997.PubMed/NCBI
|
|
10
|
Joussen AM, Poulaki V, Mitsiades N,
Kirchhof B, Koizumi K, Döhmen S and Adamis AP: Nonsteroidal
anti-inflammatory drugs prevent early diabetic retinopathy via
TNF-alpha suppression. FASEB J. 16:438–440. 2002.PubMed/NCBI
|
|
11
|
Zhang TT and Jiang JG: Active ingredients
of traditional Chinese medicine in the treatment of diabetes and
diabetic complications. Expert Opin Investig Drugs. 21:1625–1642.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aiello LP: Angiogenic pathways in diabetic
retinopathy. N Engl J Med. 353:839–841. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim JH, Kim JH, Yu YS, Cho CS and Kim KW:
Blockade of angiotensin II attenuates VEGF-mediated blood-retinal
barrier breakdown in diabetic retinopathy. J Cereb Blood Flow
Metab. 29:621–628. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Adamiec-Mroczek J, Oficjalska-Młyńczak J
and Misiuk-Hojło M: Proliferative diabetic retinopathy - The
influence of diabetes control on the activation of the intraocular
molecule system. Diabetes Res Clin Pract. 84:46–50. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Noda K, Ishida S, Inoue M, Obata K, Oguchi
Y, Okada Y and Ikeda E: Production and activation of matrix
metalloproteinase-2 in proliferative diabetic retinopathy. Invest
Ophthalmol Vis Sci. 44:2163–2170. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
EI-Asrar AM: Missotten L and Geboes K:
Expression of cyclo-xygenase-2 and downstream enzymes in diabetic
fibrovaseular epiretinal membranes. Br J Ophthalmol. 92:1534–1539.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Watanabe D: Erythropoietin as a retinal
angiogenic factor in proliferative diabetic retinopathy. Nippon
Ganka Gakkai Zasshi. 111:892–898. 2007.(In Japanese). PubMed/NCBI
|
|
18
|
Siekmann AF and Lawson ND: Notch
signalling limits angiogenic cell behaviour in developing zebrafish
arteries. Nature. 445:781–784. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Du Y, Sarthy VP and Kern TS: Interaction
between NO and COX pathways in retinal cells exposed to elevated
glucose and retina of diabetic rats. Am J Physiol Regul Integr Comp
Physiol. 287:R735–R741. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kern TS: Contributions of inflammatory
processes to the development of the early stages of diabetic
retinopathy. Exp Diabetes Res. 2007:951032007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wakabayashi Y, Usui Y, Okunuki Y, Kezuka
T, Takeuchi M, Iwasaki T, Ohno A and Goto H: Increases of vitreous
monocyte chemotactic protein 1 and interleukin 8 levels in patients
with concurrent hypertension and diabetic retinopathy. Retina.
31:1951–1957. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dong N, Li X, Xiao L, Yu W, Wang B and Chu
L: Upregulation of retinal neuronal MCP-1 in the rodent model of
diabetic retinopathy and its function in vitro. Invest Ophthalmol
Vis Sci. 53:7567–7575. 2012. View Article : Google Scholar : PubMed/NCBI
|