Introduction
Sudden cardiac death is the leading cause of death
in the world. Statistics show that in China, the number of sudden
cardiac death per year is 544,000 (1). Cardiopulmonary resuscitation (CPR) is
the most effective way to save the lives of patients. However, CPR
still failed to achieve satisfactory results in the treatment of
cardiac arrest (CA). The literature reported that 40% of patients
undergoing CPR treatment achieved return of spontaneous circulation
(ROSC), 10–30% of patients were completely cured and discharged,
and the remaining patients died of disease (2). However, patients with successful rescue
can often have a variety of complications, such as permanent
neurological complications, including cognitive disorders and
dyskinesia (3); post-resuscitation
cardiac dysfunction is also an important reason leading to poor
prognosis of patients (4), it
manifests as systemic ischemia and reperfusion syndrome. At the
same time, due to the sharp increase of a variety of deregulation
cytokines in the blood 3 h after CA, such as endotoxin releasing
into the plasma, there will be severe sepsis, leading to tissue
damage (5–7). Therefore, it is of important clinical
significance to explore an effective treatment in order to improve
the CPR postoperative prognosis.
In this experiment, we selected ulinastatin (UTI).
UTI is derived from human urinary protease inhibitors (8). It has been proved to have
anti-inflammatory, inhibiting neutrophil elastase, inhibiting
chemokine release and penetration effects (9). In addition, UTI protects mitochondrial
function by reducing calcium overload in cells, playing a role in
the protection of heart, lung, liver, kidney ischemia-reperfusion
injury (10). However, few studies
have evaluated the effect of UTI on cardiac dysfunction after CPR.
In the present study, we adopted continuous renal replacement
therapy (CRRT) at the same time, analyzed the role of UTI + CRRT in
early CPR, to provide some theoretical basis for clinical treatment
and improving the prognosis of CA.
Materials and methods
Clinical data
A total of 70 patients who were treated for CPR in
Ganzhou People's Hospital from October 2016 to March 2017 were
selected as the subjects. All patients or their families signed
informed consent, all procedures were in accordance with the
principles set out in the Helsinki Declaration. A total of 70
patients were randomly divided into control group (n=35, male 18,
female 17, mean age: 53.71±5.41 years) and UTI combined with CRRT
group (UTI + CRRT, n=35, male 19, female 16, mean age: 54.64±14.72
years). According to the American Heart Association guidelines, CPR
was performed, if necessary, chest compression and defibrillation
was given in reference to Advanced Cardiac Life Support Protocol.
The study was approved by the Ethics Committee of Ganzhou People's
Hospital.
Successful recovery was defined as patients showing
significant pulse and electrocardiography rhythm as well as
ventricular tachycardia or fibrillation. In the control group,
patients were treated with conventional symptomatic therapy. In the
UTI + CRRT group, patients were treated with intravenous injection
of UTI immediately after ROSC (Guangdong Tianpu Biochemical
Pharmaceutical Co., Ltd., Guangzhou, China; SFDA approval no.
H9990134) (300,000 U dissolved in 20 ml NaCl solution), once every
12 h. At the same time, CRRT treatment was performed with Diapact
CRRT (B. Braun Melsungen AG, Melsungen, Germany), 3 times for each
patient: Once per day for 3 days, 8 h for each treatment. All
patients underwent preoperative and post-resuscitation APACHE II
scoring by the same physician.
Sample collection and testing
The whole blood samples of the patients were
collected at 4 time points (0, 3, 6 and 12 h) after CPR. After
collecting them in the sodium citrate anticoagulant tube, the cells
were centrifuged for 5 min at 1,500 × g, then preserved at −80°C
immediately. After all the samples were collected, tumor necrosis
factor-α (TNF-α), IL-6, malondialdehyde (MDA) and cardiac troponin
I (cTnI) were measured in all samples. Blood samples from patients
were analyzed for pH, SO2, HCO3−
and lactic acid (LAC) using i-STAT System 300 (Abbott Laboratories
Inc., NY, USA). The cTnI concentration was measured using the
Abbott AXSYM system. The MDA content was determined by the kit
(Sigma; Merck KGaA, Darmstadt, Germany).
Detection of serum TNF-α and IL-6 by
ELISA
The levels of TNF-α and IL-6 in the serum of the
patients were determined by the ELISA kit (Abcam, Cambridge, MA,
USA). The reaction was carried out according to the kit
instructions. The reaction product was measured at 450 nm
wavelength and the OD values were measured, the expression was
analyzed.
Detection of toll-like receptor 4
(TLR4) expression by RT-PCR
The lymphocytes in the blood were extracted using
the TBD lymphocyte extraction kit (Tiangen Biotech Co., Ltd.,
Beijing, China), and RNA was extracted using TRIzol reagent
(Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA). The
concentration of extracted RNA was measured using a
spectrophotometer, 1 µg of RNA was taken for reverse transcription
(Takara Bio, Inc., Otsu, Japan). The mRNA levels of each indicators
were determined using SYBR-Green fluorescent reagent (Toyobo Life
Science, Osaka, Japan). TLR4 gene primers were synthesized by
Sangon Biotech Shanghai Co., Ltd. (Shanghai, China). Sequences:
Upstream 5′-CGTCTAGTCTAGAGCATCATC-3′; downstream
5′-GAGAAATGAGGAAGTAAGGG-3′; internal reference GAPDH: Upstream
5′-AGGTCGGTGTGAACGGATTTG-3′; downstream
5′-TGTAGACCATGTAGTTGAGGTCA-3′. The relative expression level of
each index is 2-ΔCq [ΔCq = Cq (target gene) - Cq (GAPDH)].
Statistical analysis
The results were analyzed using GraphPad Prism
software (Version 5.01; GraphPad Software, Inc., San Diego, Chile).
The differences of the indicators between the two groups were
compared by independent sample t-test. The expression of each
indicator at four time points was measured using the variance
analysis of repeated measurements. A P<0.05 was considered to
indicate a statistically significant difference.
Results
The basic physiological variables of
the control and the experimental group
There was no significant difference in body
temperature, heart rate, mean arterial pressure, cardiac
defibrillation and basic life support between the two groups
(P>0.05) (Table I).
 | Table I.Baseline physiology and resuscitation
related variables (mean ± SD). |
Table I.
Baseline physiology and resuscitation
related variables (mean ± SD).
| Item | Control (n=35) | UTI + CRRT
(n=35) | t-test | P-value |
|---|
| Age | 46.54±7.62 | 48.02±9.33 | 2.473 | 0.883 |
| Sex |
|
|
|
|
| Male | 17 | 19 | 3.234 | 0.673 |
|
Female | 18 | 16 | 3.667 | 0.594 |
| Body temperature
(°C) | 37.7±0.4 | 37.5±0.6 | 0.968 | 0.753 |
| HR (times/min) | 263±20 | 270±22 | 0.889 | 0.832 |
| MAP (mm/Hg) | 85±9 | 87±11 | 0.802 | 0.477 |
| DF (times) | 3±1 | 3±1 | 0.661 | 0.482 |
| BLS (min) | 3.7±2.0 | 3.6±1.8 | 0.539 | 0.724 |
Evaluation of the difference between
the biochemical indicators at different time points between the two
groups of patients
The levels of pH and SaO2 in the two
groups were not significantly different at any time point
(P>0.05). Compared with the control group, the levels of
HCO3− and LAC in the CRRT + UTI group was
downregulated significantly at 3 h after ROSC (Table II).
 | Table II.Comparison of biochemical indicators
in two groups (mean ± SD). |
Table II.
Comparison of biochemical indicators
in two groups (mean ± SD).
|
|
| ROSC |
|---|
|
|
|
|
|---|
| Groups | Index | 0 h | 3 h | 6 h | 12 h | F-value | P-value |
|---|
| Control | pH | 7.25±0.04 | 7.26±0.05 | 7.28±0.07 | 7.25±0.04 | 1.352 | 0.236 |
| (n=35) | SaO2
(%) | 94±2 | 94±3 | 93±4 | 93±3 | 1.023 | 0.991 |
|
|
HCO3− | 34±3 | 30±3 | 27±4 | 23±5 | 0.420 | 0.621 |
|
| (mmol/l) | 7.46±2.15 | 6.04±2.02 | 5.53±2.68 | 3.92±2.66 | 0.524 | 0.268 |
|
| Lac (mmol/l) |
|
|
|
|
|
|
| CRRT + UTI | pH | 7.24±0.04 | 7.25±0.06 | 7.26±0.08 | 7.24±0.05 | 1.0839 | 0.738 |
| group (n=35) | SaO2
(%) | 95±3 | 94±4 | 95±4 | 93±4 | 0.832 | 0.651 |
|
|
HCO3− | 34±4 | 25±4a | 19±5b | 17±4a | 7.453 | 0.0326 |
|
| (mmol/l) | 7.51±2.42 |
4.06±1.83a | 3.08±1.7a |
2.74±1.50a | 6.883 | 0.0192 |
|
| Lac (mmol/l) |
|
|
|
|
|
|
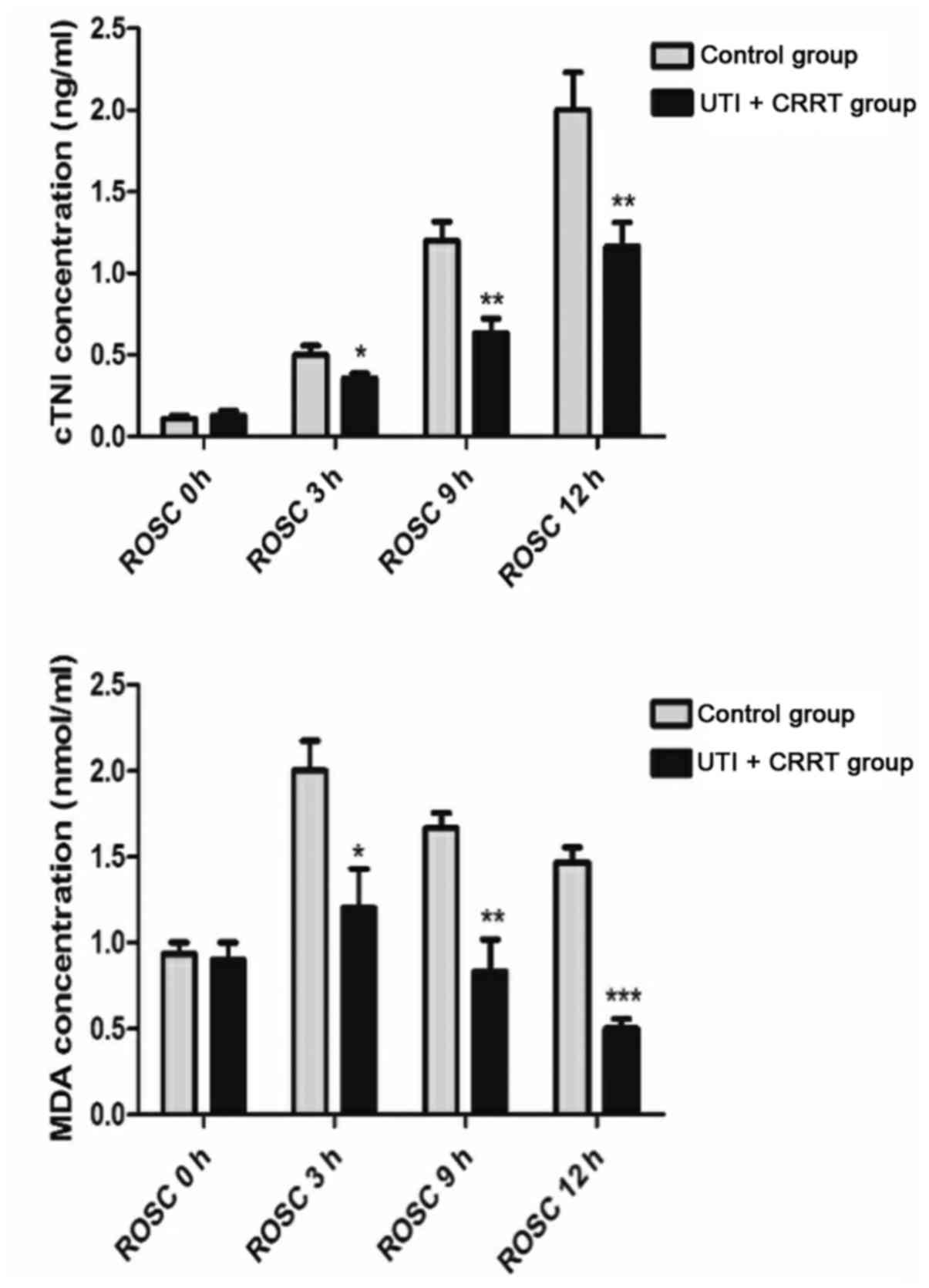
Serum cTnI and plasma MDA
expression
After CPR, the cTnI in the blood of the two groups
showed a continuous upward trend, and MDA reached the peak at 3 h
of ROSC. Starting from ROSC 3 h, UTI combined with CRRT
significantly reduced the expression of cTnI and MDA (P<0.05)
(Fig. 1).
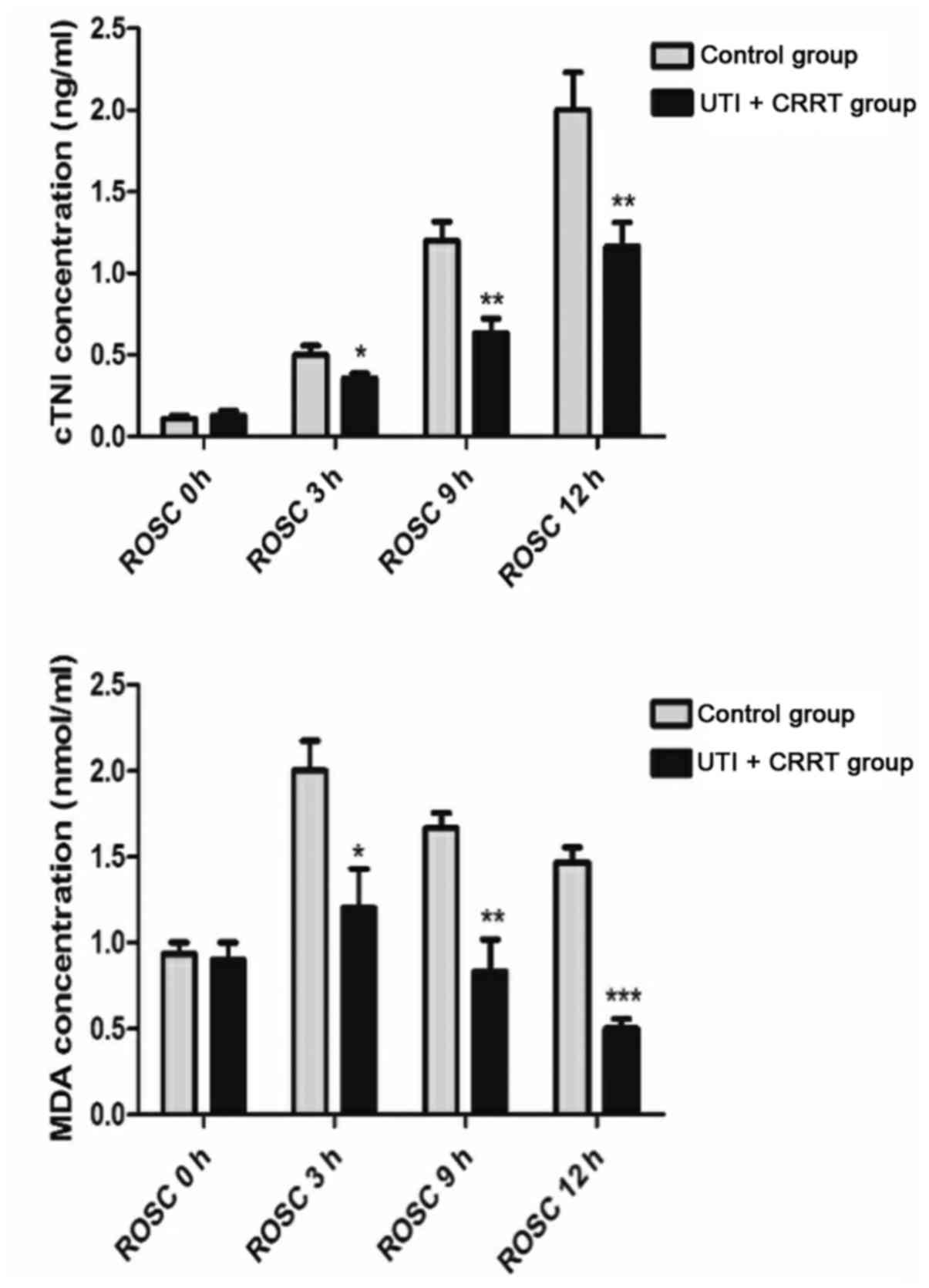 | Figure 1.Serum expression of cTnI and plasma.
After CPR, cTnI in the blood of the two groups continued to
increase, and MDA peaked at 3 h after ROSC. The expression of cTnI
and MDA in UTI + CRRT group was significantly lower than that in
control group from ROSC 3 h. UTI + CRRT vs. control group,
*P<0.05, **P<0.01, ***P<0.001. cTnI, cardiac troponin I;
CPR, cardiopulmonary resuscitation; MDA, malondialdehyde; UTI,
ulinastatin; CRRT, continuous renal replacement theraphy; ROSC,
return of spontaneous circulation. |
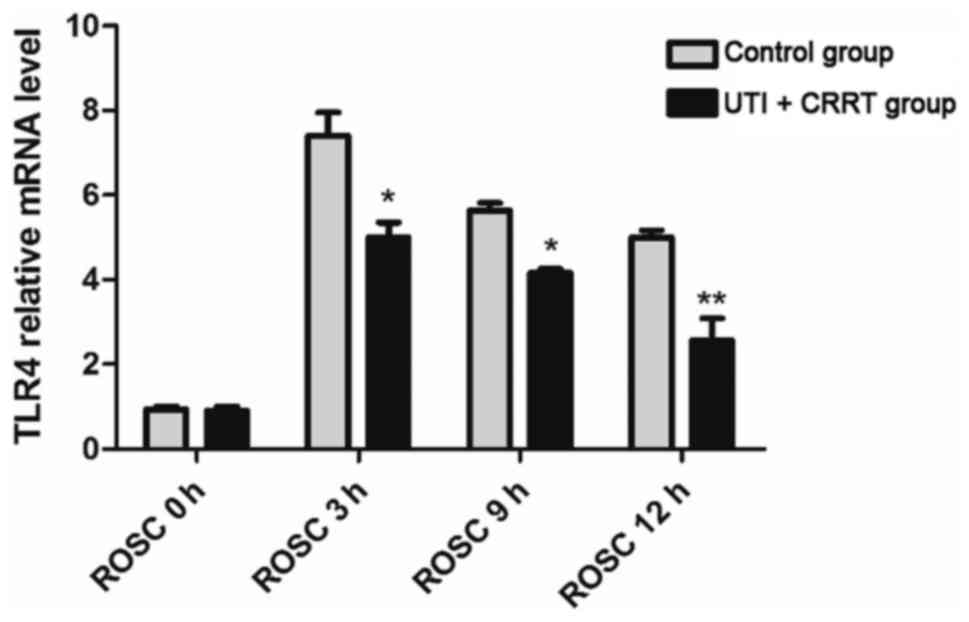
RT-PCR detection of TLR4 mRNA
levels
The patient's TLR4 mRNA expression reached the peak
3 h after the CPR, and then decreased. The expression levels of
TLR4 mRNA in the CRRT + UTI group were lower than those in the
control group at four time points (0, 3, 9, and ROSC 12 h)
(P<0.05) (Fig. 2).
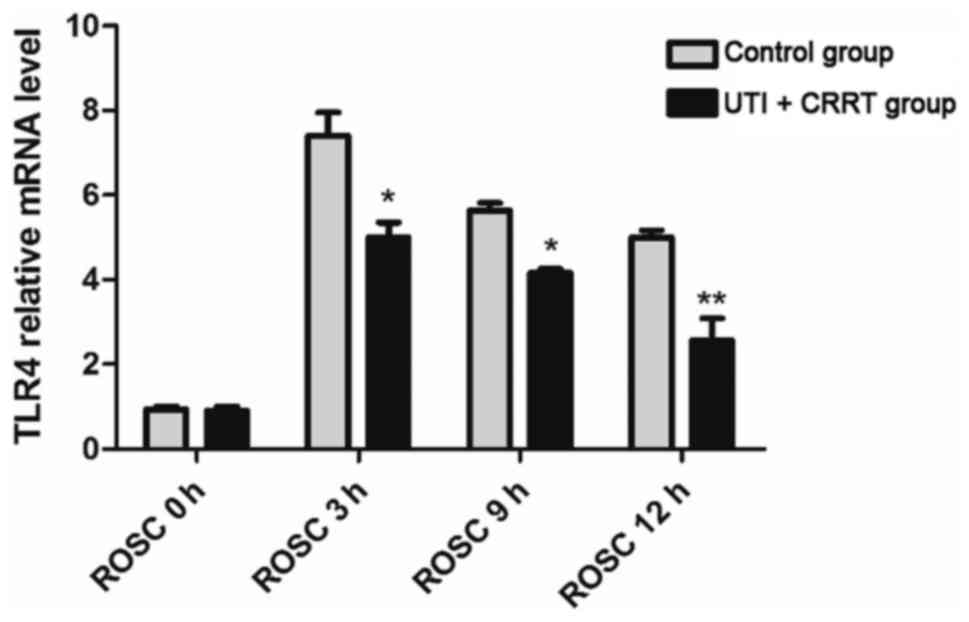 | Figure 2.RT-PCR detection of TLR4 mRNA levels.
The patient's TLR4 mRNA expression reached the peak 3 h after the
CPR, and then decreased. The expression levels of TLR4 mRNA in the
CRRT + UTI were lower than those in the control group at four time
points (0 h, 3 h, 9 h and ROSC 12 h) (P<0.05). UTI + CRRT vs.
control group, *P<0.05, **P<0.01. RT-PCR, reverse
transcription-polymerase chain reaction; TLR4, toll-like receptor
4; CPR, cardiopulmonary resuscitation; CRRT, continuous renal
replacement therapy; UTI, ulinastatin; ROSC, return of spontaneous
circulation. |
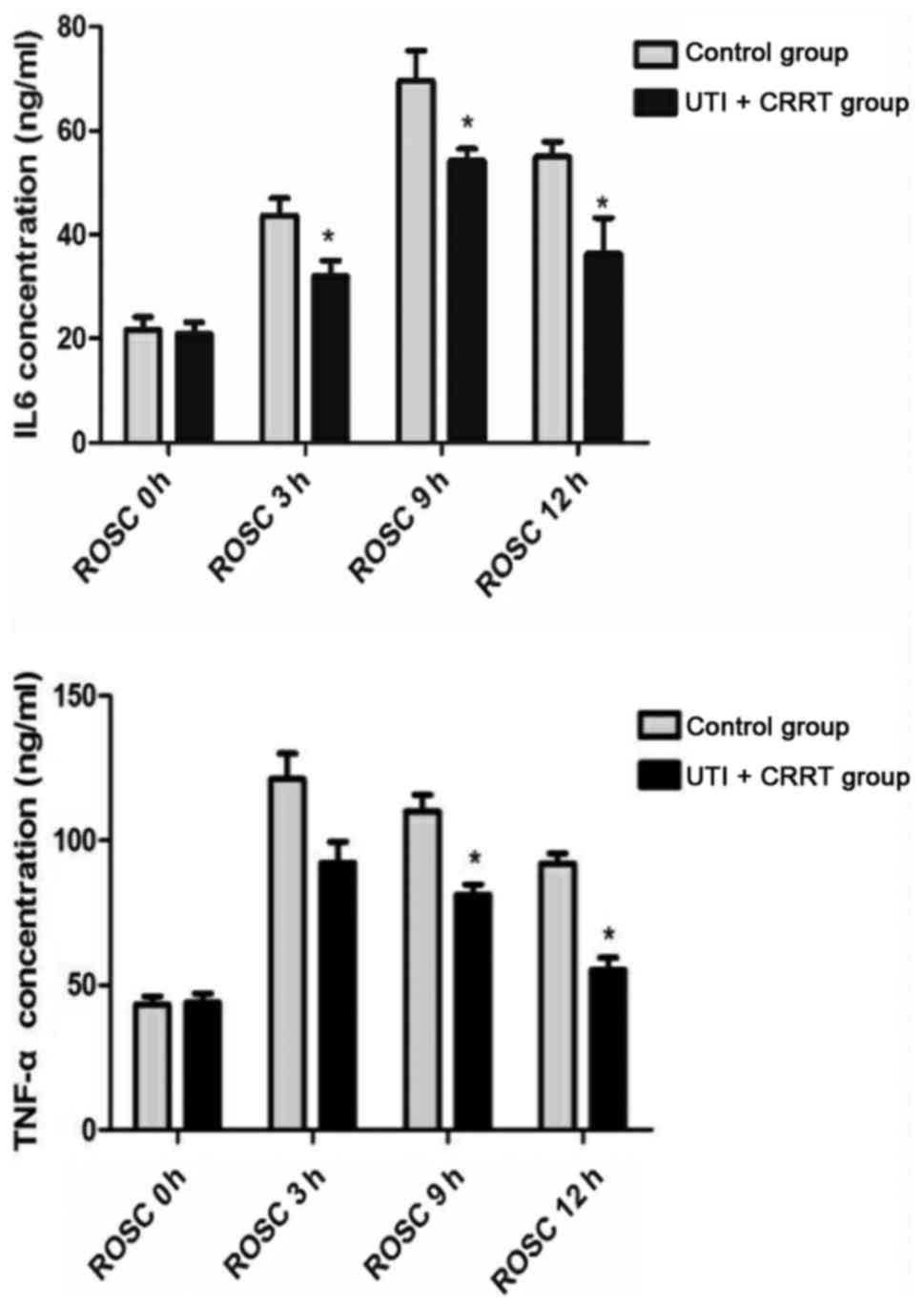
Detection of the expression of IL-6
and TNF-α by ELISA
After CPR, the levels of IL-6 and TNF-α in the blood
of the two groups reached the peak at 9 h and 3 h of ROSC,
respectively. However, the levels of IL-6 and TNF-α in UTI + CRRT
were significantly lower than those in the control group
(P<0.05) (Fig. 3).
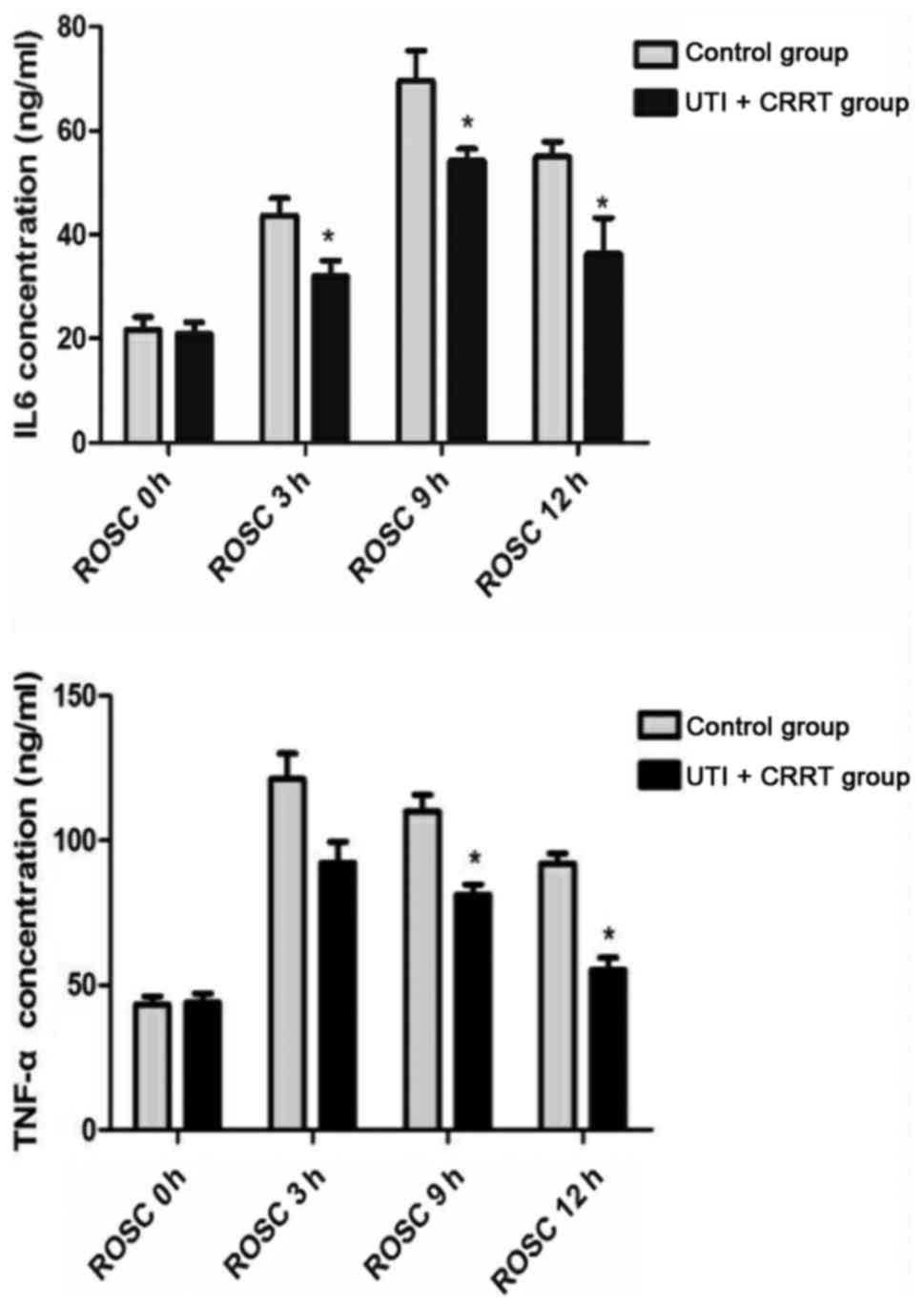 | Figure 3.ELISA detection of IL-6, and TNF-α
expression. After CPR, the levels of IL-6 and TNF-α in the blood of
the two groups reached the peak at 9 h and 3 h of ROSC,
respectively. However, the levels of IL-6 and TNF-α in UTI + CRRT
group were significantly lower than those in control group. UTI +
CRRT group vs. control group, *P<0.05. TNF-α, tumor necrosis
factor-α; IL-6, interleukin-6, CPR, cardiopulmonary resuscitation;
ROSC, return of spontaneous circulation; UTI, ulinastatin; CRRT,
continuous renal replacement theraphy. |
Average recovery time of consciousness
and spontaneous breathing after CPR
The average recovery time of consciousness and
spontaneous breathing for the patients in UTI combined with CRRT
was significantly shorter than the control group (P<0.05)
(Table III).
 | Table III.The time of recovery of consciousness
and spontaneous breathing (h) (mean ± SD). |
Table III.
The time of recovery of consciousness
and spontaneous breathing (h) (mean ± SD).
| Groups | n | Average recovery
time of spontaneous breathing | Average recovery
time of consciousness | t-test | P-value |
|---|
| Control | 35 | 15±7.2 |
| 36±11.2 |
|
| CRRT + UTI | 35 | 33±8.5b |
52±12.5a | 2.604 | 0.0204 |
APACHE II score of two groups
APACHE II scores were assessed by designated
physicians before and 24 h after CPR. UTI combined with CRRT
significantly reduced APACHE II scores (Table IV).
 | Table IV.APACHE II score (mean ± SD). |
Table IV.
APACHE II score (mean ± SD).
|
| APACHE II score
(points) |
|---|
|
|
|
|---|
| Groups | n | Before | After |
|---|
| Control | 35 | 24.41±4.41 | 21.34±6.23 |
| UTI + CRRT | 35 | 24.57±5.34 |
16.60±8.49a |
Discussion
After CA occurs in patients, it can lead to various
pathological situations, such as inflammation, oxidative stress,
myocardial damage and heart damage. In the present study, we
analyzed multiple biomarkers at multiple time points after CPR
treatment, including cTnI, MDA, TLR4, TNF-α, and IL-6. CTnI is a
specific marker of myocardial injury (11). Early myocardial injury can be
detected by serum cTnI levels (12).
In the present study, serum cTnI was continuously elevated in both
groups, but the level of UTI + CRRT was significantly lower than
that of the control group. Changes in cTnI suggest that CA will
inevitably lead to myocardial injury in patients, but the use of
UTI + CRRT can reduce the damage to a certain extent.
It has been shown that oxidative stress is
associated with lipid peroxidation and is one of the mechanisms of
neuronal injury induced by ischemia-reperfusion (13,14).
MDA, as the final product of lipid oxidation, can cause
cross-linked polymerization of protein, nucleic acid and other
macromolecules, and has cytotoxicity, it is often used as a marker
of oxidative stress after ischemia-reperfusion (15,16). In
the present study, plasma MDA levels in both groups increased
significantly, reached a peak at 3 h after CPR treatment, and
combination of UTI + CRRT significantly decreased MDA content,
indicating that UTI and CRRT have protective effects on myocardium
after CPR.
Organ damage CA after successful CRP is considered
to associate with systemic inflammatory response; various cytokines
and lipopolysaccharide (LPS) levels have been proved to have risen
significantly in patients with successful resuscitation (17,18).
TLR4 recognizes LPS, which promotes the production of a variety of
inflammatory cytokines (IL-6 and TNF-α), leading to sepsis-like
syndrome (19). Activated TLR4
promotes nuclear factor expression during cerebral ischemia and
hypoxia, and induces the production of cytokines such as TNF-α and
IL-6, causing inflammation and nerve damage (20). Therefore, we speculate that TLR4
signaling pathway may inhibit the inflammatory response and nerve
damage by hypoxic preconditioning, thus protecting brain function.
In addition, previous studies have shown that UTI can reduce lung
and kidney damage caused by LPS inhibiting the inflammatory
response of these organs (21). In
this study, TLR4 gene was significantly upregulated in both groups
after CPR, and TNF-α and IL-6 were also upregulated. UTI combined
with CRRT significantly lowered these indicators and shortened the
recovery time of consciousness and spontaneous breathing, reduced
the APACHE II score.
In conclusion, we found that UTI combined with CRRT
can protect against ischemia/reperfusion injury caused by early
CPR, and can inhibit the inflammatory response induced by TLR4
after early CPR.
References
|
1
|
Zhang S: Sudden cardiac death in China:
Current status and future perspectives. Europace. 17:14–18. 2015.
View Article : Google Scholar
|
|
2
|
de Vreede-Swagemakers JJ, Gorgels AP,
Dubois-Arbouw WI, van Ree JW, Daemen MJ, Houben LG and Wellens HJ:
Out-of-hospital cardiac arrest in the 1990's: A population-based
study in the Maastricht area on incidence, characteristics and
survival. J Am Coll Cardiol. 30:1500–1505. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Peters R and Boyde M: Improving survival
after in-hospital cardiac arrest: The Australian experience. Am J
Crit Care. 16:240–246. 2007.PubMed/NCBI
|
|
4
|
Kim RJ, Wu E, Rafael A, Chen EL, Parker
MA, Simonetti O, Klocke FJ, Bonow RO and Judd RM: The use of
contrast-enhanced magnetic resonance imaging to identify reversible
myocardial dysfunction. N Engl J Med. 343:1445–1453. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carden DL and Granger DN: Pathophysiology
of ischaemia-reperfusion injury. J Pathol. 190:255–266. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hernandez LA and Grisham MB: Role of
neutrophils in ischemia reperfusion induced microvascular injury.
Am J Physiol Heart Circ Physiol. 3:699–703. 2006.
|
|
7
|
Hausenloy DJ and Yellon DM: Myocardial
ischemia-reperfusion injury: A neglected therapeutic target. J Clin
Invest. 123:92–100. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Koga Y, Fujita M, Tsuruta R, Koda Y,
Nakahara T, Yagi T, Aoki T, Kobayashi C, Izumi T, Kasaoka S, et al:
Urinary trypsin inhibitor suppresses excessive superoxide anion
radical generation in blood, oxidative stress, early inflammation,
and endothelial injury in forebrain ischemia/reperfusion rats.
Neurol Res. 32:925–932. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang G, Wen J, Wilbur RR, Wen P, Zhou SF
and Xiao X: The effect of somatostatin, ulinastatin and Salvia
miltiorrhiza on severe acute pancreatitis treatment. Am J Med
Sci. 346:371–376. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pang XY, Fang CC, Chen YY, Liu K and Song
GM: Effects of ulinastatin on perioperative inflammatory response
and pulmonary function in cardiopulmonary bypass patients. Am J
Ther. 23:e1680–e1689. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kruzan RM, Herzog CA, Wu A, Sang Y, Parekh
RS, Matsushita K, Hwang S, Cheng A, Coresh J, Powe NR, et al:
Association of NTproBNP and cTnI with outpatient sudden cardiac
death in hemodialysis patients: The choices for healthy outcomes in
caring for ESRD (CHOICE) study. BMC Nephrol. 17:182016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hu CL, Wei HY, Liu ZY, Li X, Liao XX, Li
YJ, Zhan H, Jing XL, Xiong Y, Liu YY, et al: Investigation of the
relationship between venticular fibrillation duration and
cardiac/neurological damage in a rabbit model of electrically
induced arrhythmia. J Trauma. 69:1442–1447. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Murdolo G, Piroddi M, Luchetti F,
Tortoioli C, Canonico B, Zerbinati C, Galli F and Iuliano L:
Oxidative stress and lipid peroxidation by-products at the
crossroad between adipose organ dysregulation and obesity-linked
insulin resistance. Biochimie. 95:585–594. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Martindale JJ and Metzger JM: Uncoupling
of increased cellular oxidative stress and myocardial ischemia
reperfusion injury by directed sarcolemma stabilization. J Mol Cell
Cardiol. 67:26–37. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li XY and Chow CK: An improved method for
the measurement of malondialdehyde in biological samples. Lipids.
29:73–75. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Esterbauer H, Schaur RJ and Zollner H:
Chemistry and biochemistry of 4-hydroxynonenal, malonaldehyde and
related aldehydes. Free Radic Biol Med. 11:81–128. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Neumar RW, Nolan JP, Adrie C, Aibiki M,
Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC,
et al: Post-cardiac arrest syndrome: Epidemiology, pathophysiology,
treatment, and prognostication. A consensus statement from the
International Liaison Committee on Resuscitation (American Heart
Association, Australian and New Zealand Council on Resuscitation,
European Resuscitation Council, Heart and Stroke Foundation of
Canada, InterAmerican Heart Foundation, Resuscitation Council of
Asia, and the Resuscitation Council of Southern Africa); the
American Heart Association Emergency Cardiovascular Care Committee;
the Council on Cardiovascular Surgery and Anesthesia; the Council
on Cardiopulmonary, Perioperative, and Critical Care; the Council
on Clinical Cardiology; and the Stroke Council. Circulation.
118:2452–2483. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Erenler AK, Çelik S, Baydin A, Tomak L,
KoSargelir M and Yasti AÇ: Outcomes of cardiopulmonary
resuscitation in trauma patients in the emergency department. Eur
Rev Med Pharmacol Sci. 19:2567–2571. 2015.PubMed/NCBI
|
|
19
|
Janssen E, Ozcan E, Liadaki K, Jabara HH,
Manis J, Ullas S, Akira S, Fitzgerald KA, Golenbock DT and Geha RS:
TRIF signaling is essential for TLR4-driven IgE class switching
(IRM5P. 707). J Immunol. 192:2651–2658. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Blanco AM, Vallés SL, Pascual M and Guerri
C: Involvement of TLR4/type I IL-1 receptor signaling in the
induction of inflammatory mediators and cell death induced by
ethanol in cultured astrocytes. J Immunol. 175:6893–6899. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen J, Wang J, Su C, Qian W, Sun L, Sun
H, Chen J, Zhang H and Zhang J: Urinary trypsin inhibitor
attenuates LPS-induced endothelial barrier dysfunction by
upregulation of vascular endothelial-cadherin expression. Inflamm
Res. 65:213–224. 2016. View Article : Google Scholar : PubMed/NCBI
|