Introduction
Industrial pollution and traffic emissions have
increased the smog phenomenon. This coupled with vulnerable airway
barrier of the under-age children further increase the incidence of
asthma in children (1). Asthma in
children has become a public health problem that has attracted the
global concern regarding the disease. Various epidemiological
studies have shown that the global prevalence of asthma in children
ranges from 3 to 29% (2). The
occurrence of asthma in children can be caused by many factors,
including environmental, gender, genetic, ethnic factors and
socioeconomic status (3). In recent
years, studies have shown that vitamin D (VitD) levels and the
incidence of asthma were closely related. Relevant studies have
suggested that the VitD may be involved in the development of
asthma or the lack of lung compliance will lead to immune
dysfunction, thereby triggering the factors for asthma in children
(4).
There has been a growing interest in the potential
role of VitD in asthma management, because it might help to reduce
upper respiratory infections (such as the common cold) that can
lead to exacerbations of asthma. Several clinical trials have
tested whether taking VitD as a supplement has an effect on asthma
attacks, symptoms and lung function in children and adults with
asthma. VitD supplementation can regulate the body's immune
function, reduce inflammation and initiate repair functions in the
body (5). It has been reported that
the VitD has a protective effect on the respiratory tract (6). In the present study, VitD levels in
normal children and children with asthma were detected and the
correlation between the VitD levels and asthma attacks were
investigated. Atomization inhalation of budesonide combined with
albuterol and VitD supplement was used to treat asthma. This study
provided a theoretical basis for effective prevention and treatment
of asthma in children.
Materials and methods
General information
The total sample size was comprised of 96 children
with diagnosis of asthma. The data were collected from the time
period of May 2015 to April 2016. At the same time, a total of 96
healthy children were also selected from the physical examination
center. The study was approved by the Ethics Committee of Jingzhou
Maternal and Child Health-Care Hospital and informed consents were
signed by the guardians.
The inclusion criteria for the study was as
followed: i) patients who meet the asthma diagnostic criteria
established by Chinese Medical Association were included in the
samples; ii) age between 0 and 14 years were the only children that
were included in the samples; iii) the patients presenting with
clinical manifestations of cough, chest tightness, lung wheezing,
night and/or early morning onset or exacerbate; and iv) the parents
had signed informed consent. The exclusion criteria that were taken
for the study was as follows: i) the children without history of
recurrent respiratory tract infections and recent history of
wheezing were excluded from the sample size; ii) those children
that were allergic to the drugs which were used in this study were
also excluded; and iii) those children who were on hormonal drugs
during the previous 30 days.
The asthmatic patients were further randomly
subdivided into two groups i.e. observation group and control group
based on the treatment protocol. Each group comprised of 48 cases.
The patients in the control group were treated with the only
budesonide therapy. The patients in the observation group were
treated with atomization inhalation of budesonide combined with
salbutamol and VitD supplementation. The general information of the
both groups are given in Table
I.
 | Table I.Comparison of the general information
between asthmatic groups. |
Table I.
Comparison of the general information
between asthmatic groups.
| Items | Control group
(n=48) | Observation group
(n=48) | t/χ2 | P-value |
|---|
| Sex
(male/female) | 21/27 | 25/23 | 0.376 | 0.539 |
| Age (years) | 0–13 | 0–14 |
|
|
| Mean age (years) | 6.48±1.27 | 6.56±1.38 | 0.296 | 0.768 |
| Weight (kg) | 16.73±3.24 | 17.07±3.33 | 0.507 | 0.613 |
| History of allergies
(n, %) | 31 (64.58) | 33 (68.75) | 0.001 | 0.998 |
| Combined with
mycoplasma pneumoniae infection (n, %) | 16 (33.33) | 18 (37.50) | 0.047 | 0.827 |
| Eosinophil count in
peripheral blood | 0.47±0.26 | 0.45±0.24 | 0.392 | 0.696 |
| Childhood Asthma
Control Test Score (C-ACT) | 16.26±1.25 | 16.14±1.34 | 0.454 | 0.651 |
Determination of VitD levels and IgE
content
The venous blood of 3 ml was extracted from the all
samples including the healthy subjects. After the centrifugation at
the rate of 3000 r/min for 20 min, the separated serum was placed
in an EP tube and stored at −80°C. The levels of serum VitD were
determined by ELISA. The serum VitD levels were determined
according to the instructions of 25(OH)D3 kit (R&D
Systems, Inc., Minneapolis, MN, USA). After adding samples,
incubation, washing, enzyme addition, again incubation and washing,
the color development and the stop solution was added within 15
min. The OD of each well was measured by a microplate reader (450
nm wavelength) and the VitD level was calculated. The total serum
IgE level was measured by immunoturbidimetry according to the
instructions of IgE kit (Weifang Kanghua Biotechnology Co., Ltd.,
Weifang, China).
Treatment of asthmatic children
The children in the control group were given only
budesonide nasal spray (AstraZeneca AB, Södertälje, Sweden;
National medical license number: J20040082) inhalation therapy.
Children that were younger than 6 years were given a dose of 100 µg
and children aged 6 years or above were given a dose of 200 µg,
twice a day. Besides budesonide treatment, the patients in the
observation group were given salbutamol aerosol inhalation solution
(Shanghai Xinyi Jinzhu Pharmaceutical Co., Ltd., Shanghai, China;
National medical license number: H19990233) and with further
supplementation of vitamin D (Qingdao Shuangjing Pharmaceutical
Co., Ltd., Qingdao, China; National medical license number:
H20113033). The dosage of salbutamol therapy was as followed:
children who were under the age of 6 were given 100 µg, twice a day
and the dosage was doubled in cases of severe sign and symptoms.
Children who were aged 6 years or above were given a dose of 200
µg, twice a day, the drug was given once every 6 h for severe
symptom, 200 µg each time. The dosage of VitD was as followed:
children under the age of 6 were given 200 IU per day and children
over the age of 6 were given 400 IU per day.
Detection of the indicators
Pulmonary function was detected by children's
pulmonary function monitor (Master Screen Paed, CareFusion Corp.,
Höchberg, Germany). While testing, the respiratory tract was kept
unobstructed. Ring finger and fifth finger was used to hold up the
jaw of the children to put the mask, so that it covered both the
nose and mouth. The indicators which were used in the study were:
forced expiratory volume 1 (FEV1), forced vital capacity (FVC),
FEV1/FVC ratio, maximum expiratory flow at 25% (MEF25) and maximum
expiratory flow at 50% (MEF50). These tests were measured under
quiet breathing.
After 3 months of treatment, again the venous blood
samples were taken at early morning (8 h fasting), and the serum
was separated by centrifugation. IL-2, IL-4, IL-6 and IFN-γ levels
were determined by ELISA in strict accordance with the instructions
(Aikang Biology Co., Ltd., Shaoxing, China). Concentrations of
IL-2, IL-4, IL-6 and IFN-γ were calculated by reading the OD values
using a microplate reader (450 nm wavelength). All patients were
followed up for 6 months. The asthma control rate, reoccurrence
rate and re-hospitalization rate were statistically analyzed.
Follow-up
The control rate, reoccurrence rate and
re-hospitalization rate were compared between the groups 6 months
after the discharge. The standard criteria which were set for both
groups are as follows: Asthma control rate, no recurrence of asthma
within half a year. Recurrence rate, at least one acute attack
within six months. Re-hospitalization rate, hospitalization with
six months due to asthma recurrence.
Statistical analysis
Data were processed using SPSS software version 19.0
(SPSS, Inc., Chicago, IL, USA). Measurement data were expressed as
mean ± SD and were analyzed by the t-test. The count data were
expressed in terms of rate and were analyzed by the χ2.
Pearson correlation coefficient analysis was used to analyze the
correlation between VitD levels and pulmonary function, IgE.
P<0.05 was considered to be statistically significant.
Results
Comparison of VitD and IgE levels in
both groups of children
The levels of serum VitD in children with asthma
were significantly lower than those in the normal children. The
serum IgE levels in children with asthma were significantly higher
than those in normal children, and this was statistically
significant at P<0.05 (Table
II).
 | Table II.Comparison of VitD and IgE levels in
both groups of children. |
Table II.
Comparison of VitD and IgE levels in
both groups of children.
| Groups | Cases | VitD (ng/ml) | IgE (IU/ml) |
|---|
| Children with
asthma | 96 | 18.89±3.63 | 375.13±64.34 |
| Normal children | 96 | 32.74±3.67 | 286.79±54.45 |
| t-value |
| 26.289 | 10.269 |
| P-value |
| <0.001 | <0.001 |
Correlation between VitD levels, IgE
and pulmonary function
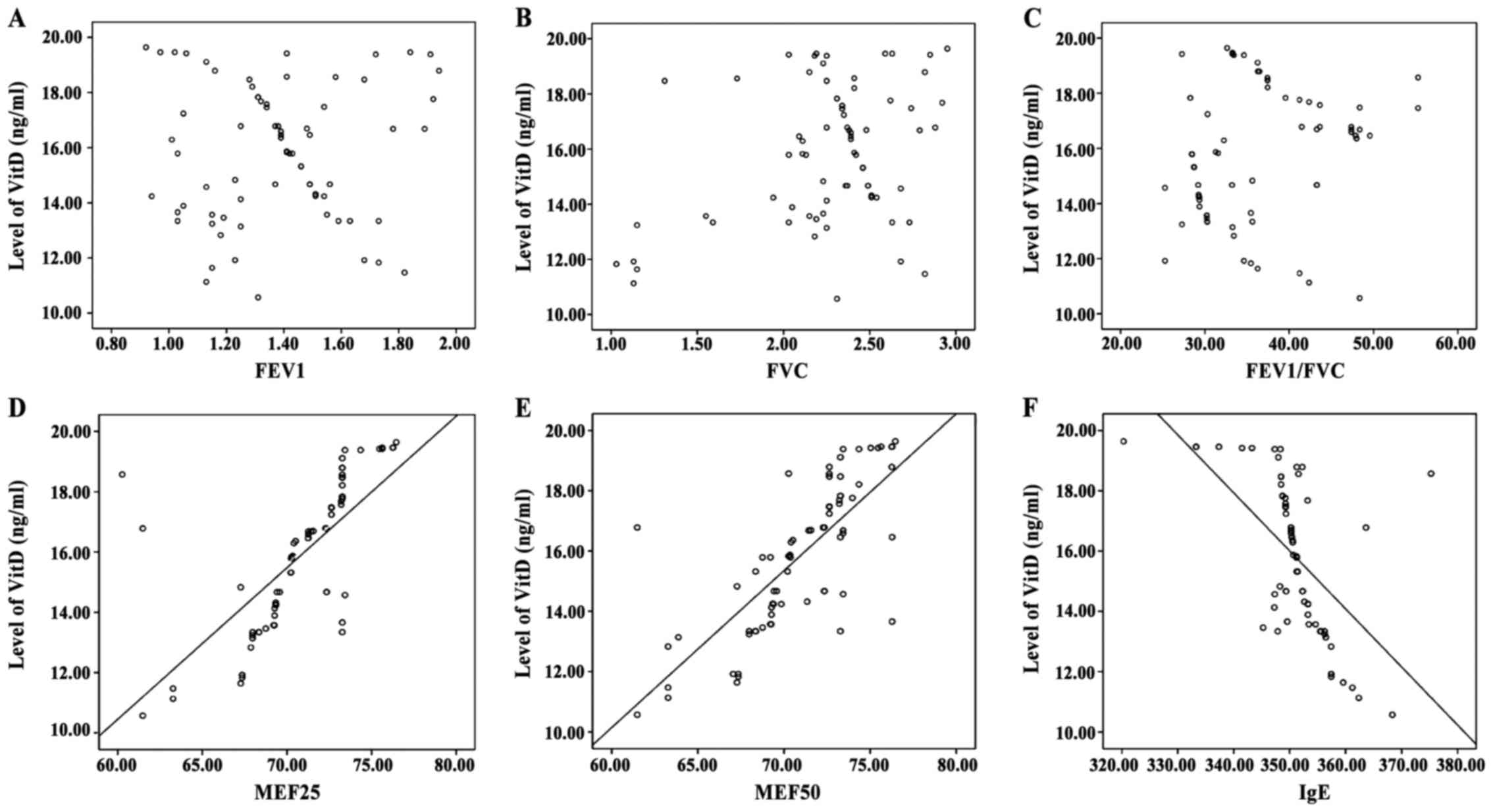
Pearson correlation coefficient analysis showed that
VitD levels were not significantly correlated with FEV1, FVC,
FEV1/FVC, but positively correlated with MEF25 and MEF50. The
analysis also revealed that VitD levels were negatively correlated
with IgE and were statistically significant at P<0.05 (Table III and Fig. 1).
 | Table III.Correlation between VitD levels, IgE
and pulmonary function. |
Table III.
Correlation between VitD levels, IgE
and pulmonary function.
| Items | Correlation
coefficient | P-value |
|---|
| FEV1 | −0.568 | 0.103 |
| FVC | 0.601 | 0.214 |
| FEV1/FVC | 0.345 | 0.317 |
| MEF25 | 0.679 | 0.005 |
| MEF50 | 0.457 | 0.016 |
| IgE | −0.568 | 0.024 |
Comparison of pulmonary function in
the asthmatic groups of children
After 3 months of treatment, the FVC, FEV1,
FEV1/FVC, MEF25 and MEF50 levels in observation group were
significantly higher than the control group with significance at
P<0.05 (Table IV).
 | Table IV.Comparison of pulmonary function in
asthmatic groups of children. |
Table IV.
Comparison of pulmonary function in
asthmatic groups of children.
| Groups | N (cases) | FVC (L) | FEV1 (L) | FEV1/FVC (%) | MEF25 (%) | MEF50 (%) |
|---|
| Control group | 48 | 2.35±0.73 | 1.19±0.37 | 41.35±8.34 | 65.14±7.48 | 65.34±3.15 |
| Observation
group | 48 | 2.69±0.87 | 1.46±0.42 | 49.53±7.76 | 78.28±7.24 | 79.48±3.38 |
| t-value |
| 1.933 | 3.342 | 4.957 | 8.745 | 21.203 |
| P-value |
| 0.041 | 0.001 | <0.001 | <0.001 | <0.001 |
The comparison of cytokine indexes
between the asthmatic groups after the treatment
The level of IL-2 and IFN-γ in the observation group
were significantly higher than those in the control group
(P<0.05). The level of IL-4 and IL-6 in the observation group
was significantly lower than that in the control group with
statistical significance at P<0.05 (Table V).
 | Table V.The comparison of cytokine indexes
between the asthmatic groups after the treatment. |
Table V.
The comparison of cytokine indexes
between the asthmatic groups after the treatment.
| Groups | N (cases) | IL-2 (µmol/) | IL-4 (µmol/) | IL-6 (µmol/l) | IFN-γ (µmol/) |
|---|
| Control group | 48 | 56.57±4.13 | 24.45±3.54 | 19.72±5.46 | 18.57±6.34 |
| Observation
group | 48 | 51.36±4.38 | 31.64±3.38 | 23.48±5.57 | 14.25±6.73 |
| t-value |
| 5.966 | 10.178 | 3.340 | 3.237 |
| P-value |
| <0.001 | <0.001 | 0.001 | 0.001 |
Comparison of therapeutic effect
observed 6 months after discharge in the asthmatic groups
The asthma recurrence rate and re-hospitalization
rate were significantly lower in the observation group than those
in the control group. The asthma control rate in the observation
group was significantly higher than that in the control group with
statistical significance at P<0.05 (Table VI).
 | Table VI.Comparison of therapeutic effect
observed 6 months after discharge in the asthmatic groups. |
Table VI.
Comparison of therapeutic effect
observed 6 months after discharge in the asthmatic groups.
| Groups | N (cases) | Asthma control
rate | Recurrence rate | Re-hospitalization
rate |
|---|
| Control group | 48 | 44 (91.67) | 4 (8.33) | 3 (6.25) |
| Observation
group | 48 | 35 (72.92) | 14 (29.17) | 11 (22.92) |
| χ2 |
| 59.54 | 58.73 | 59.82 |
| P-value |
| 0.032 | 0.018 | 0.042 |
Discussion
Asthma is also known as bronchial asthma, basically
it is a chronic airway inflammation with a very high incidence in
children. Asthma symptoms in children are more significantly
noticed at night or early morning. The symptom can be relieved by
the appropriate treatment therapy (7). One of the main and common causes of
asthma is the chronic inflammatory reactions of the respiratory
tract. Airway inflammation occur in both the periods of acute
exacerbation of asthma and remission periods of asthma. The
stimulating and aggravating factors like activation of allergen,
hyperventilation, excessive exercise, cold air and strong emotional
changes can increase the symptoms of airway inflammation, thus,
inducing acute asthmatic attacks. Thus, the key to reduce the
asthmatic attacks is to control the airway inflammation (8,9).
Vitamin D (VitD), a second type of steroid
derivative. VitD can be converted into the 7-dehydrocholesterol
from cholesterol and be converted to vitamin D3 by ultraviolet
light. After its absorption into blood, VitD is finally converted
into a highly active form 25(OH)D3. At present,
25(OH)D3 is most commonly used in the evaluation of VitD
levels. The biological half-life of VitD is approximately 3 weeks
(10,11). VitD not only plays an important role
in regulating bone metabolism and calcium homeostasis, but also has
a key active role in the immune regulation system. The beneficial
effects of VitD on protective immunity are due in part to its
effects on the innate immune system. It is known that macrophages
recognize lipopolysacharide LPS, a surrogate for bacterial
infection, through toll-like receptors (TLR). Engagement of TLRs
leads to a cascade of events that produce peptides with potent
bacteriacidal activity such as cathelocidin and beta-defensin 4.
These peptides colocalize within phagosomes with injested bacteria
where they disrupt bacterial cell membranes and have potent
anti-microbacterial activity. VitD can also regulate the blood
calcium levels and tissue and cell differentiation (12). Studies have found that the VitD
levels and early transient wheezing are closely related to each
other, and higher infant cord serum VitD levels can usually lead to
lower incidence of wheezing (13).
The present study found that VitD levels in the children with
asthma were significantly lower than those in normal children and
serum IgE levels in children with asthma were significantly higher
than those in the normal children with significance at P<0.05.
The reason is that imbalance of Th1/Th2 cytokines also leads to
asthma. VitD is involved in the inhibition of autoimmune disorders
and low VitD level will reduce the inhibitory effect, which further
leads to the overexpression of Th2-type cytokines and eventually
increase the occurrence of asthma (14).
This study also found that there was no correlation
between VitD levels and FEV1, FVC, FEV1/FVC (P>0.05) and
positively correlated with MEF25 and MEF50 (P<0.05). The results
of the study showed that the VitD levels were negatively correlated
with IgE. Some studies have shown similar results and concluded
that the FEV1, FVC, FEV1/FVC parameters are not related to the
asthma symptoms, but small airway parameters MEF25 and MEF50 are
related to asthma symptoms and inflammatory response. VitD can also
reduce the division and proliferation of smooth muscle cells that
further leads to the decreased airflow and also reduces the small
airway obstruction (15,16). Thus, we hypothesized that low VitD
levels can decrease the resistant ability of children's airway to
infection, leading to the higher airway infection and induce
asthmatic attacks. Therefore, VitD supplementation can be
considered as adjuvant therapy for the prevention and treatment of
asthma in children.
As a kind of glucocorticoid, budesonide can inhibit
the synthesis and release of broncho-constrictor substances. These
substances reduce the contractile response of smooth muscle, and
further, significantly alleviate the acute onset of asthmatic
attacks (17). As the excitant of β2
receptor, salbutamol has strong effects on bronchial smooth
muscles. Salbutamol can relax the bronchial smooth muscle, relieve
bronchial spasm and reduce the permeability of the peripheral
capillaries (18). This study found
that the levels of IL-2 and IFN-γ in the observation group were
higher than those in the control group with significant values
(P<0.05), and the levels of IL-4 and IL-6 in the observation
group were significantly lower than those in the control group.
This is because the budesonide and salbutamol can bind to the
cysteine receptors, and VitD can be combined with the two drugs to
reduce the sensitivity of peripheral blood eosinophils. In
addition, VitD in combination with the two drugs can participate in
the regulation of Th1/Th2 cytokine. That will further regulate the
alveolar macrophages, pulmonary epithelial cells and dendritic
cells to inhibit the production of IL-4 and IL-6 cells, reducing
airway inflammation and promoting the secretion of IL-2 and IFN-γ
that prevents the reoccurrence of airway hyper-responsiveness
(19).
Animal model revealed that, the VitD can reduce the
secretion of chemokines from airway smooth muscle cells and reduce
the pathological changes of airway remodeling (20). The present study also found similar
results. The results revealed that the reoccurrence rate and
re-hospitalization rate of the observation group were significantly
lower than those of the control group (P<0.05), suggesting that
high VitD levels could reduce the recurrence of asthma. In
conclusion, VitD levels are closely related with the onset of
asthma in children. Atomization inhalation of budesonide combined
with albuterol and VitD supplementation can significantly improve
children's pulmonary function and reduce airway inflammation, which
will increase the asthma control rate. Future studies with larger
sample are still need to further investigate the mechanism.
References
|
1
|
Pasić A, Tahirović H and Hadzibeganović M:
Incidence of asthma in children in Tuzla Canton-Bosnia and
Herzegovina. Coll Antropol. 35:299–303. 2011.
|
|
2
|
Zhang YX, Liu Y, Xue Y, Yang LY, Song GD
and Zhao L: Correlational study on atmospheric concentrations of
fine particulate matter and children cough variant asthma. Eur Rev
Med Pharmacol Sci. 20:2650–2654. 2016.PubMed/NCBI
|
|
3
|
Yin GQ, Jiang WH, Wu PQ, He CH, Chen RS
and Deng L: Clinical evaluation of sublingual administration of
dust mite drops in the treatment of allergic asthma and allergic
rhinitis of children. Eur Rev Med Pharmacol Sci. 20:4348–4353.
2016.PubMed/NCBI
|
|
4
|
Turkeli A, Ayaz O, Uncu A, Ozhan B, Bas
VN, Tufan AK, Yilmaz O and Yuksel H: Effects of vitamin D levels on
asthma control and severity in pre-school children. Eur Rev Med
Pharmacol Sci. 20:26–36. 2016.PubMed/NCBI
|
|
5
|
Hoxha M, Zoto M, Deda L and Vyshka G:
Vitamin D and its role as a protective factor in allergy. Int Sch
Res Notices. 2014:9519462014.PubMed/NCBI
|
|
6
|
Baïz N, Dargent-Molina P, Wark JD,
Souberbielle JC and Annesi-Maesano I; EDEN Mother-Child Cohort
Study Group, : Cord serum 25-hydroxyvitamin D and risk of early
childhood transient wheezing and atopic dermatitis. J Allergy Clin
Immunol. 133:147–153. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gong L, Xu L, Diao M, Guo F, Bian FF, Min
J, Liu R and Zhang CL: Clinical effect of treating secondary asthma
attacks of children Mycoplasma pneumoniae with combined therapy of
montelukast and azithromycin. Eur Rev Med Pharmacol Sci.
20:5256–5260. 2016.PubMed/NCBI
|
|
8
|
Agarwal R, Dhooria S, Aggarwal AN, Maturu
VN, Sehgal IS, Muthu V, Prasad KT, Yenge LB, Singh N, Behera D, et
al: Guidelines for diagnosis and management of bronchial asthma:
Joint ICS/NCCP (I) recommendations. Lung India. 32 Suppl 1:S3–S42.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yadav M and Mittal K: Effect of vitamin D
supplementation on moderate to severe bronchial asthma. Indian J
Pediatr. 81:650–654. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Institute of Medicine (US) Committee to
Review Dietary Reference Intakes for Vitamin D and Calcium, .
Dietary reference intakes for calcium and vitamin D. Pediatrics.
130:14272011.
|
|
11
|
Dong CH, Gao QM, Wang ZM, Wang AM and Zhen
P: Vitamin D supplementation for osteoporosis in older adults: Can
we make it help better? Eur Rev Med Pharmacol Sci. 20:4612–4621.
2016.PubMed/NCBI
|
|
12
|
Mangge H, Zelzer S, Meinitzer A, Stelzer
I, Schnedl WJ, Weghuber D, Fuchs D, Postolache TT, Aigner E, Datz
C, et al: 25OH-Vitamin D3 levels in obesity and metabolic
syndrome-unaltered in young and not correlated to carotid IMT in
all ages. Curr Pharm Des. 21:2243–2249. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Einisman H, Reyes ML, Angulo J, Cerda J,
López-Lastra M and Castro-Rodriguez JA: Vitamin D levels and
vitamin D receptor gene polymorphisms in asthmatic children: A
case-control study. Pediatr Allergy Immunol. 26:545–550. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tamašauskienė L, Gasiūnienė E, Lavinskienė
S, Sakalauskas R and Šitkauskienė B: Evaluation of vitamin D levels
in allergic and non-allergic asthma. Medicina (Kaunas). 51:321–327.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ahmadabadi F, Mirzarahimi M, Barak Ahadi A
and Alipour R: The relationship between serum vitamin D level and
asthma severity in asthmatic children (aged 1–15 years) in Ardabil,
2012–13. Int J Res Med Sci. 3:239–243. 2015.
|
|
16
|
Bener A, Ehlayel MS, Bener HZ and Hamid Q:
The impact of Vitamin D deficiency on asthma, allergic rhinitis and
wheezing in children: An emerging public health problem. J Family
Community Med. 21:154–161. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lazarinis N, Jørgensen L, Ekström T,
Bjermer L, Dahlén B, Pullerits T, Hedlin G, Carlsen KH and Larsson
K: Combination of budesonide/formoterol on demand improves asthma
control by reducing exercise-induced bronchoconstriction. Thorax.
69:130–136. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Visser R, van der Palen J, de Jongh FH and
Thio BJ: Reversibility after inhaling salbutamol in different body
postures in asthmatic children: A pilot study. Respir Med.
109:459–462. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Das I, Saha K, Mukhopadhyay D, Roy S,
Raychaudhuri G, Chatterjee M and Mitra PK: Impact of iron
deficiency anemia on cell-mediated and humoral immunity in
children: A case control study. J Nat Sci Biol Med. 5:158–163.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Alyasin S, Momen T, Kashef S, Alipour A
and Amin R: The relationship between serum 25 hydroxy vitamin d
levels and asthma in children. Allergy Asthma Immunol Res.
3:251–255. 2011. View Article : Google Scholar : PubMed/NCBI
|