Introduction
A solid breast mass, with a wide variation in the
radiological appearance corresponding to different properties of
the pathological features, can be broadly classified as benign or
malignant (1). Thus, differential
diagnosis of solid breast masses is of great significance in
clinical therapy and prognostic evaluation. Breast cancer is one of
the most common malignant solid tumors in women, occurring in ~1.5
million women worldwide each year (2). The incidence of breast cancer is rising
each year and patients tend to be affected at a younger age
(3,4). Along with the improvement of imaging
diagnostic technology for breast diseases in recent years, early
diagnosis and treatment have been implemented, which significantly
improved the 5-year survival rate and life quality of patients with
breast cancer (5,6). Therefore, early and sensitive
diagnostic methods result in therapy at an earlier stage of the
disease and a better prognosis. Previous studies have demonstrated
that the 10-year survival rate was up to 80% in patients with
breast cancer when early and suitable treatment was administrated
(7,8).
Currently, there are various imaging methods for
non-invasive diagnosis of breast masses, including conventional
ultrasonography, X-ray mammography, multi-slice spiral computed
tomography, magnetic resonance imaging (MRI) and Doppler ultrasound
color flow imaging. However, each single method has various
advantages and disadvantages, and the results obtained from
different methods are often conflicting. Therefore, the combination
of two or three diagnostic methods is commonly adopted in
determining the properties of breast masses and for the clinical
diagnosis of breast cancer (9,10).
X-ray mammography is the most important tool in the
screening of breast cancer in clinical practice. However, MRI has
higher sensitivity than X-ray mammography in identifying occult
breast lesions, particularly dense lesions (11). MRI can provide a more reliable basis
for accurate staging and the development of a clinical treatment
strategy for breast cancer. Ultrasound elastography (UE) is another
examination technology for breast cancer with a rapid development
in recent years. UE is a method used to visualize the elasticity of
tumors and, thus, demonstrates more superior advantages in
differentiating benign and malignant breast tumors compared with
conventional ultrasonography (12).
The strain ratio (SR) and a five-point scoring system are the two
most useful and effective parameters to consider in UE. SR-based
elastographic analysis can provide a novel and more reliable
diagnostic tool in comparison to a five-point scoring system for UE
in the diagnosis of breast cancer (13).
The aim of the present study was to evaluate and
compare the performance of UE, MRI and the combination of these two
methods (UE+MRI) in the diagnosis of breast cancer and its
differentiation from benign lesions.
Materials and methods
Patient recruitment
Between October 2014 and October 2015, a total of 86
patients with solid lesions in the breast who were admitted to the
Department of Breast Surgery of the Nuclear Industry 215 Hospital
of Shanxi Province (Xianyang, China) were included in the study.
All patients underwent diagnostic examination with UE and MRI. The
patients were randomly divided into the UE+MRI (n=43), UE (n=26)
and MRI (n=17) groups. The inclusion criteria were as follows: i)
Patients had newly diagnosed breast nodules; ii) the breast lesions
were solid or mixed (cystic-solid) nodules, with or without
calcification; iii) patients voluntary underwent the UE or MRI
examination; and iv) patients signed informed consent prior to
surgery or biopsy. The exclusion criteria were as follows: i)
Patients with cystic nodules and ii) patients with malignant
nodules. The clinical characteristics of patients and histological
features of the breast lesions are shown in Table I. Prior written and informed consent
was obtained from every patient, and the study was approved by the
Ethics Review Board of the Nuclear Industry 215 Hospital of Shanxi
Province.
 | Table I.Clinical characteristics of patients
included in the present study. |
Table I.
Clinical characteristics of patients
included in the present study.
| Characteristics | UE+MRI group
(n=43) | UE group (n=26) | MRI group (n=17) | P-value |
|---|
| Age
(years)a | 34.4±8.7 | 39.6±10.6 | 41.3±9.7 | 0.083 |
| Mass location
(left/right) |
23/20 | 10/16 | 5/12 | 0.056 |
| Maximum diameter of
mass (0.3–4.0 cm)a |
2.6±1.2 |
2.0±0.65 |
2.3±318 | 0.094 |
| Axillary lymph nodes
and breast palpation (yes/no) | 35/8 | 19/7 | 12/5 | 0.042 |
| Calcification
(yes/no) |
24/21 |
11/15 | 6/11 | 0.037 |
| Mass appearance
(regular/irregular) |
28/15 | 17/9 | 10/7 | 0.058 |
| Echo intensity of UE
(strong/moderate) |
21/22 | 18/8 | 10/7 | 0.023 |
UE examination
UE was used to analyze the properties of breast
masses. UE examination was performed using Philips IU Elite color
Doppler ultrasound system (Philips Medical Systems, Bothell, WA,
USA) equipped with UE capacity and a L11-3 linear array transducer.
Firstly, two-dimensional ultrasound scanning was performed on the
patients' breasts to observe the number, location and size of the
masses. Real-time UE analysis was then conducted at the lesion
site. The blue, green and red images represented the strong tissue
stiffness, moderate tissue stiffness and soft tissue, respectively.
Next, the elastographic imaging was adjusted to an appropriate size
corresponding to the lesion size. The linear probe was maintained
at the lesion site and a slight vibration
(compression/decompression operation) was performed.
Two-dimensional and elasticity images were observed on a real-time
display. The region of interest (ROI) was set for the lesion tissue
and surrounding normal breast tissue in the same depth as the
breast lesion. Finally, the SR value was calculated to assess the
relative hardness of the breast lesion vs. the surrounding breast
tissue. Examination for each lesion was conducted in triplicate and
the average SR value was calculated.
MRI examination
All patients were placed in prone position and
examined on a 1.5-Tesla MRI scanner equipped with a dedicated
breast surface coil (Magnetom Avanto; Siemens Medical Solutions,
Erlangen, Germany). The scanning range included the bilateral
breasts and the corresponding level of prothoraxes and bilateral
axillae. The breast MRI protocol included axial T1-weighted FLASH,
T2-weighted TIRM and diffusion-weighted single-shot echo-planar MRI
sequences, as well as short inversion time inversion recovery as a
technique of fat suppression. The pathological features of benign
and malignant breast tumors in the MRI scans were as follows:
Benign tumors were generally round or oval in shape with a clear
boundary or lobulated appearance, whereas the edges of malignant
tumors were blurry and displayed irregular with unclear boundaries
from the surrounding tissues. Finally, the differential diagnosis
of benign and malignant breast masses was performed using the
Breast Imaging Reporting and Data System recommended by the
American College of Radiology (14).
The likelihood of malignancy of each lesion was classified
according to a five-point scale (15) as follows: 1, benign lesion; 2,
potentially benign; 3, possibly benign but in need of follow-up; 4,
potentially malignant; and 5, malignant tumor. Generally, tumors
classified on the scale as 1–3 were considered benign, while those
classified as 4 and 5 were considered malignant tumors. Classifying
scale 3 tumors as benign did not affect the study. Scale 3 refers
to tumors that have 98% chance of benign, but still in need of
follow-up. In the present study, the cases of scale 3 were all
benign cases, as confirmed by the follow-up data.
Hematoxylin and eosin (H&E)
staining
Pathological results from H&E staining were used
as the golden standard for definitive diagnosis of the breast
lesions. Breast tissues were collected from resected breast masses
subsequent to surgery, fixed in 10% formaldehyde and embedded in
paraffin. The tissues were cut into 5-µm sections and stained with
H&E. The diagnosis of benign or malignant breast tumor was
confirmed independently by two pathologists.
Observational parameters and image
analysis
Imaging findings in the two groups were evaluated
for breast masses including breast fibroadenoma, mastitis, invasive
ductal carcinoma, invasive lobular carcinoma, intraductal papillary
carcinoma, medullary carcinoma and mucinous carcinoma. The
diagnostic performances were compared among the UE, MRI and UE+MRI
methods according to their correlation with the pathological
diagnosis. In order to determine the optimal cut-off points for the
diagnosis of benign and malignant breast masses, a receiver
operating characteristic (ROC) curve was constructed. Subsequently,
the area under the ROC curve (AUC) was calculated to evaluate the
diagnostic performance of these methods, while the detection rate,
sensitivity and specificity of the three methods were also
determined.
Statistical analysis
All data were analyzed using the SPSS version 17.0
software (SPSS, Inc., Chicago, IL, USA). Comparison of continuous
data between two groups was performed by independent-samples
t-test, and comparison of categorical data was conducted by
χ2 test. Kappa coefficients were calculated. P<0.05
was considered to demonstrated differences that were statistically
significant.
Results
Clinical characteristics of patients
and imaging findings
A total of 86 patients with single solid lesions in
the breast were included in the present study. UE and MRI were used
to observe the breast masses, which were subsequently evaluated. In
the UE+MRI group, patients (mean age, 34.4±8.7 years; age range,
27–65 years) were examined by a combination of UE and MRI methods.
The mass was located in the left breast in 23 cases and in the
right breast in 20 cases. In addition, the mean maximum diameter of
the mass in the UE+MRI group was 2.6±1.2 cm, with a range of
0.3–4.0 cm. In the UE group (mean age, 39.6±10.6 years; age range,
22–67 years) and MRI group (mean age, 41.3±9.7 years; age range,
22–70 years), patients were examined by UE or MRI, respectively.
The left/right breast mass location ratio was 10/16 in the UE group
and 5/12 in the MRI group. The mean maximum diameters of the masses
were 2.0±0.5 and 2.3±0.8 cm in the UE and MRI groups, respectively
(Table I). The benign masses were
generally displayed as round or oval lesions with a clear boundary.
By contrast, the malignant tumors were blurry, and displayed
irregular lesion edges, non-uniform imaging signals and unclear
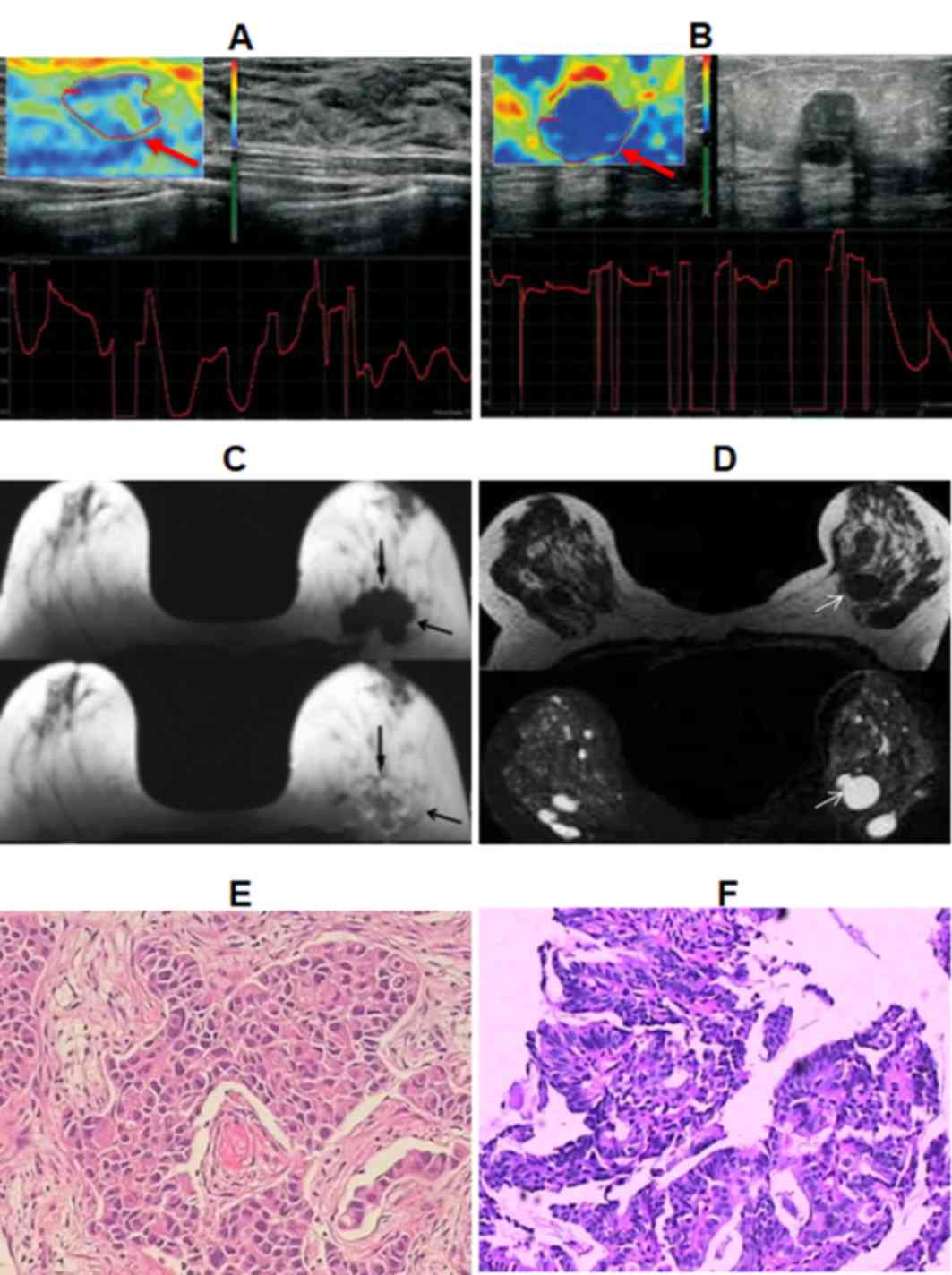
boundaries from the surrounding tissues. Representative UE scans of
patients with malignant and benign tumors are shown in Fig. 1A and B, respectively, while MRI scans
are shown in Fig. 1C and D. These
diagnoses were later confirmed by H&E staining of tissue
samples (Fig. 1E and F).
Comparison of detection rate of
different methods
The detection rates of the UE, MRI and UE+MRI
methods were evaluated based on the pathological analysis. As shown
in Table II, there were 28 cases of
malignant masses and 9 cases of benign masses in the UE group, 23
malignant masses and 5 benign masses in the MRI group, and 31
malignant masses and 9 benign masses in the UE+MRI group. The
detection rates were 85.8, 64.8 and 92.7% in the UE, MRI and UE+MRI
groups, respectively. The difference in the detection rates between
the UE and UE+MRI groups or between the MRI and UE+MRI groups were
statistically significant (all P<0.05), indicating that the
combination of UE and MRI method is superior to the application of
UE or MRI alone in the diagnosis of benign and malignant breast
masses.
 | Table II.Comparison of detection rates of UE,
MRI and UE+MRI methods. |
Table II.
Comparison of detection rates of UE,
MRI and UE+MRI methods.
| Parameter | UE | MRI | UE+MRI |
|---|
| Definitive
diagnosis |
|
|
|
| Breast
fibroma | 4 (9.3) | 3 (6.9) | 5
(11.6) |
| Breast
hyperplasia | 5
(11.6) | 2 (4.6) | 4 (9.3) |
| Invasive
ductal carcinoma | 10 (23.2) | 9
(20.9) | 11 (25.5) |
|
Intraductal papillary
carcinoma | 7
(16.2) | 5
(11.6) | 7
(16.2) |
| Invasive
lobular carcinoma | 8
(18.6) | 6
(13.9) | 9
(20.9) |
| Mucinous
carcinoma | 1 (2.3) | 2 (4.6) | 3 (6.9) |
| Medullary
carcinoma | 2 (4.6) | 1 (2.3) | 1 (2.3) |
| Detection rate
(%) | 85.8 | 64.8 | 92.7 |
Definition of optimal cut-off
points
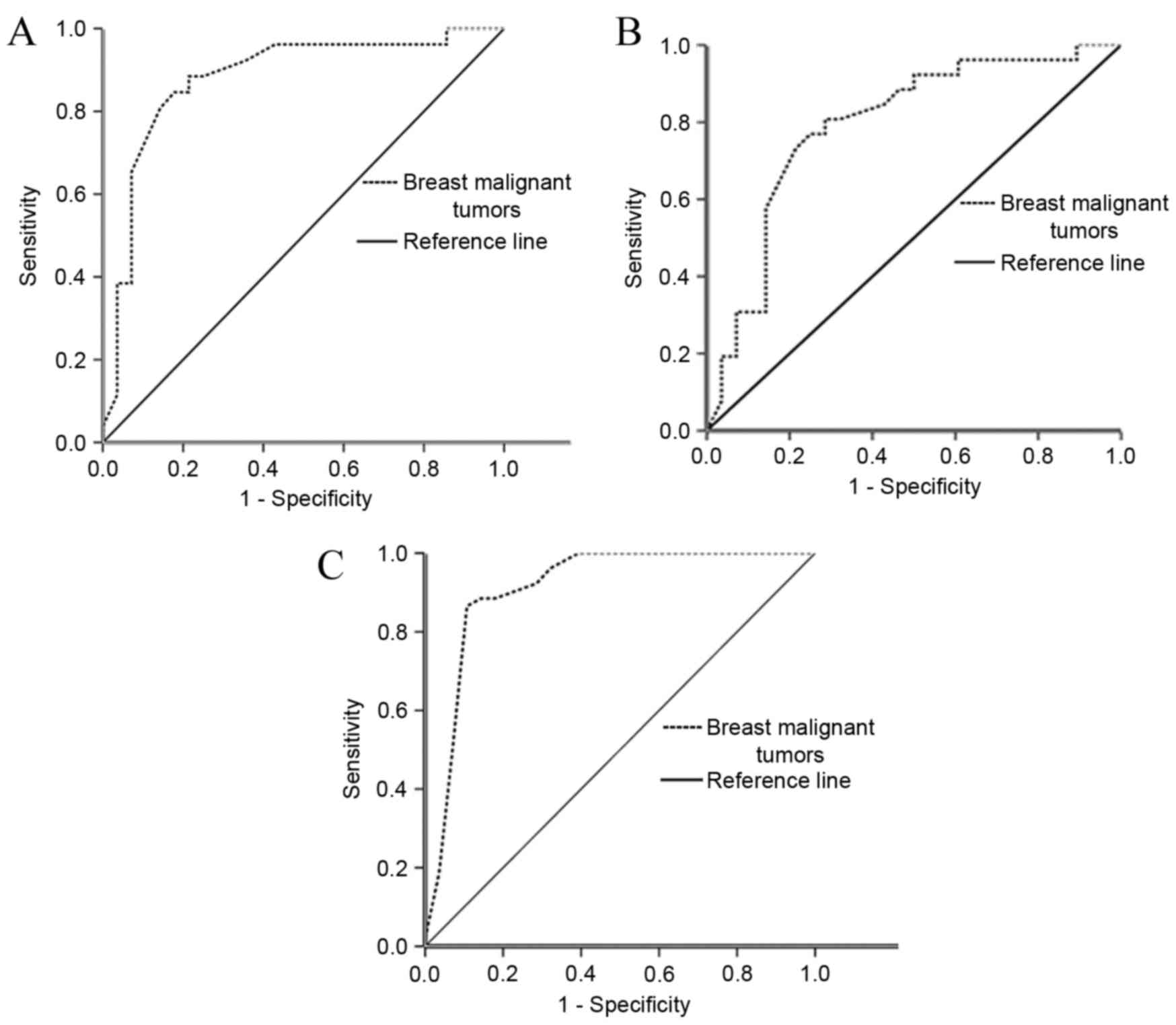
The ROC curve, with sensitivity as the y-axis and
1-specificity as the x-axis, was constructed to determine the
optimal cut-off points for the three methods. The results
demonstrated that the cut-off points of UE, MRI and UE+MRI methods
were 2.81, 3.76 and 3.42, respectively, in the diagnosis of benign
or malignant breast masses (Fig. 2),
while the AUC values were 86.7, 79.2 and 91.4%, respectively. The
differences in the AUC value between the UE and UE+MRI groups or
between the MRI and UE+MRI groups were statistically significant
(all P<0.05), which also revealed that combination of the UE and
MRI diagnostic methods yielded the best results for detection of
breast cancer.
Comparison of diagnostic accuracy
rates of different methods
A total of 72 cases of malignant breast cancer in
the 86 patients were pathologically diagnosed following surgery.
For the UE, MRI and UE+MRI diagnostic methods, the following values
were observed: The sensitivity values were 83.3, 77.7 and 95.8%;
the specificity values were 78.5, 64.2 and 92.8%; and the accuracy
rates of differential diagnosis were 82.5, 75.5 and 95.3%,
respectively (Table III). The
differences in accuracy rates between the UE and MRI methods or
between the UE and UE+MRI methods were found to be statistically
significant (all P<0.05); however, there was no significant
difference in the accuracy rate between the MRI and UE+MRI methods
(P>0.05). The Youden index in UE, MRI, and UE+MRI was 61.8,
41.9, and 88.6, respectively. There were significant differences in
Youden index among the three methods (all P<0.05; Table III). This suggests that the UE+MRI
method has higher test authenticity compared with UE or MRI
alone.
 | Table III.Comparison of diagnostic accuracy
rates of UE, MRI and UE+MRI methods. |
Table III.
Comparison of diagnostic accuracy
rates of UE, MRI and UE+MRI methods.
| Group | Sensitivity (%) | Specificity (%) | Youden index | Accuracy rate
(%) | P-value |
|---|
| UE | 83.3 | 78.5 | 61.8 | 82.5 | 0.023 |
| MRI | 77.7 | 64.2 | 41.9 | 75.5 | 0.057 |
| UE+MRI | 95.8 | 92.8 | 88.6 | 95.3 | 0.006 |
Diagnostic consistency of imaging
methods with pathological analysis
A total of 72 cases of malignant breast cancer were
selected from the 86 patients. These 72 patients were examined by
pathology and all three methods. The pathological results were used
as the golden standard. A curve-fitting analysis was performed to
evaluate the diagnostic consistency of the UE, MRI or UE+MRI
findings with the results of pathological analysis. The kappa
coefficients for UE, MRI and UE+MRI were 0.512, 0.527 and 0.630,
respectively (all P<0.001). These values indicate that the
diagnostic consistency of the combination of UE and MRI was higher
compared with the application of UE or MRI alone in the diagnosis
of benign and malignant breast masses (Table IV).
 | Table IV.Diagnostic consistency of the three
imaging methods with the pathological diagnosis. |
Table IV.
Diagnostic consistency of the three
imaging methods with the pathological diagnosis.
|
|
| Pathological
diagnosis |
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|---|
| Group | Imaging
diagnosis | + | − | Total | Pearson
χ2 | Kappa
coefficients | P-value |
|---|
| UE | + | 60 | 2 | 62 | 47.489 | 0.512 | 0.001 |
|
| − | 4 | 6 | 10 |
|
|
|
| MRI | + | 56 | 7 | 63 | 53.580 | 0.527 | 0.001 |
|
| − | 3 | 6 | 9 |
|
|
|
| UE+MRI | + | 69 | 1 | 70 | 47.314 | 0.630 | 0.001 |
|
| − | 0 | 2 | 2 |
|
|
|
Discussion
UE, as a novel ultrasound imaging technique based on
the measurement of the relative hardness of a lesion against the
adjacent normal tissues, has the ability to yield a more accurate
estimation compared with conventional ultrasound examination
technology in the differentiation of malignant from benign breast
lesions (16). A previous study has
demonstrated that UE was helpful in the differentiation of benign
and malignant breast lesions since the hardness of malignant breast
cancer was 2–3 times higher than that of benign cancer (17). MRI is another noninvasive diagnostic
tool that is useful in distinguishing soft tissue from other
tissues. Therefore, the combination of UE and MRI may be more
beneficial to identify the likelihood of benign or malignant breast
lesions based on the hardness of the lesions (18,19). As
a novel and effective imaging tool, the combination of UE and MRI
methods may significantly improve diagnostic accuracy and be more
objective.
A previous study showed that the accuracy rate of UE
was higher compared with color flow Doppler in the diagnosis of
breast cancer (20). In the present
study, when the diagnostic methods of UE and MRI were used to
distinguish between benign and malignant breast tumor properties,
the detection rates were found to be 85.8, 64.8 and 92.7% in the
UE, MRI and UE+MRI groups, respectively. These findings revealed
that UE and MRI were effective tools for identifying benign or
malignant breast cancer, while the combination of UE and MRI was
superior to the single application of UE or MRI.
The ROC curve is an effective method for evaluating
the performance of diagnostic tests. In addition, AUC is a common
index summarizing the information contained in the curve and
reflecting the reliability of diagnostic methods. In the current
study, the AUC values were 86.7, 79.2 and 91.4% in the UE, MRI and
UE+MRI methods, respectively, for the diagnosis of breast lesions.
The corresponding cut off points for these three methods were
defined as 2.81, 3.76 and 3.42, respectively. These cut off points
yielded the highest sensitivities of 83.3, 77.7 and 95.8% for UE,
MRI and UE+MRI, respectively. Previous studies reported similar
results, observing that the sensitivity of UE ranged between 87.1
and 95.0% in the diagnosis of breast cancer (19,21).
Furthermore, the present study revealed that the accuracy rates of
differential diagnosis were 82.5, 75.5 and 95.3% for UE, MRI and
UE+MRI, respectively. Therefore, the diagnostic accuracy rate of
the UE+MRI method was significantly higher compared with the single
application of UE or MRI. In addition, the three methods had high
diagnostic agreement with the pathological diagnosis; however, the
diagnostic consistency of UE+MRI was higher compared with the
application of UE or MRI alone for the diagnosis of benign and
malignant breast masses. Another study demonstrated the same trend,
but with higher AUC values of UE's diagnosis on breast mass
(22). This difference may be due to
a limited number of samples, selection bias and inconsistent
sampling of the present study.
In conclusion, UE and MRI are effective tools in the
diagnosis of breast cancer, while the combination of UE (SR-based)
and MRI is superior to the single use of UE or MRI and can greatly
improve the detection rate of malignant breast tumors. These
results may be beneficial for the optimized use of UE and MRI in
clinical practice, although further studies are warranted to
confirm these findings.
Acknowledgements
The authors wish to thank Professor Huawen Zhang
(Department of Radiology, Nuclear Industry 215 Hospital of Shanxi
Province, Xianyang, China) for the technical support concerning UE
and MRI.
References
|
1
|
Zheng Q, Wang JF, Dai ZQ, Hu J and Xu Y:
Diagnostic value of color doppler ultrasonography, ultrasonic
elastograqhy and mammography in the differentiation of breast
lesions. J Community Med. 11:14–16. 2013.(In Chinese).
|
|
2
|
Gong NM and Wu J: The Value analysis and
evaluation of randomized control of color doppler ultrasound
combined CT applying to analyze breast cancer. Chin J CT MRI.
131:51–53. 2015.(In Chinese).
|
|
3
|
Meng SP, Zhang ZP and Wang P: Research on
application value of CT, ultrasound and X-ray mammography in the
diagnosis of breast carcinoma. Chin J CT MRI. 16:33–35. 2014.(In
Chinese).
|
|
4
|
Jiang PL, Wang SH, Jiang DM, Tang LL and
YU LL: Study on cancer-related fatigue and disease characteristics
of breast cancer patients. China J Mod Med. 21:4443–4449. 2011.
|
|
5
|
Wind JJ and Ammerman JM: Pathologic
cervical burst fracture presenting with airway compromise. South
Med J. 103:551–553. 2010. View Article : Google Scholar
|
|
6
|
Warner E and Causer PA: MRI surveillance
for hereditary breast-cancer risk. Lancet. 365:1747–1749. 2005.
View Article : Google Scholar
|
|
7
|
Wu H and Ouyang QC: Protective effect of
dexrazoxane on anthracyclines cardio toxicity of the female breast
cancer patients with postoperative chemotherapy. China J Mod Med.
20:2188–2194. 2010.
|
|
8
|
Zheng Y, Wu CX and Wu F: Status and trends
of breast cancer mortality in Chinese females. Zhonghua Yu Fang Yi
Xue Za Zhi. 45:150–154. 2011.(In Chinese).
|
|
9
|
Xu JX: Application of ultrasound
elastography in qualitative diagnosis of solid breast masses. China
Health Ind. 8:147–148. 2014.(In Chinese).
|
|
10
|
Zhong XF: The investigation of the
diagnostic value of ultrasound elastography in breast masses.
Contemporary Med. 20:149–150. 2014.
|
|
11
|
Liberman L, Morris EA, Dershaw DD,
Abramson AF and Tan LK: MR imaging of the ipsilateral breast in
women with percutaneously proven breast cancer. AJR Am J
Roentgenol. 180:901–910. 2003. View Article : Google Scholar
|
|
12
|
Adamietz BR, Meier-Meitinger M, Fasching
P, Beckmann M, Hartmann A, Uder M, Häberle L, Schulz-Wendtland R
and Schwab SA: New diagnostic criteria in real-time elastography
for the assessment of breast lesions. Ultraschall Med. 32:67–73.
2011. View Article : Google Scholar
|
|
13
|
Zhao QL, Ruan LT, Zhang H, Yin YM and Duan
SX: Diagnosis of solid breast lesions by elastography 5-point score
and strain ratio method. Eur J Radiol. 81:3245–3249. 2012.
View Article : Google Scholar
|
|
14
|
Gu YJ, Wu B, Zhang S and Yang T: The
application experiences of breast imaging reporting and data system
in mammographic diagnoses of breast lesion with symptoms. Chin J
Radiol. 38:931–936. 2004.(In Chinese).
|
|
15
|
Gu Y, Wu B, Zhang S and Yang T: The
application experiences of breast imaging reporting and data system
in mammographic diagnoses of breast lesion with symptoms. Chin J
Radiol. 9:931–936. 2004.(In Chinese).
|
|
16
|
Hooley RJ, Scoutt LM and Philpotts LE:
Breast ultrasonography: State of the art. Radiology. 268:642–659.
2013. View Article : Google Scholar
|
|
17
|
Krouskop TA, Wheeler TM, Kallel F, Garra
BS and Hall T: Elastic moduli of breast and prostate tissues under
compression. Ultrason Imaging. 20:260–274. 1998. View Article : Google Scholar
|
|
18
|
Zhi H, Xiao XY and Yang HY: Primary
comparison of the diagnostic value of strain ratio measure method
and 5-scoring system in ultrasonic elestography for differentiation
breast benign and malignant solid lesions with ultrasonic
elastography. Chin J Ultrasonography 19: 142–144, 2010. Chin J
Ultrasonography 19: 142–144, 2010. 19: 142–144, 2010:142–144,
2010–144, 2010. 2010.(In Chinese).
|
|
19
|
Zhou J, Zhan W, Dong Y, Yang Z and Zhou C:
Stiffness of the surrounding tissue of breast lesions evaluated by
ultrasound elastography. Eur Radiol. 24:1659–1667. 2014. View Article : Google Scholar
|
|
20
|
Zhang ZM, Zhao L, Wang YL, Liu Y, Wang SL
and He Y: Diagnostic value of ultrasonic elastography, color
doppler flow imaging and mammography in breast diseases. Chongqing
Med. 12:3604–3606. 2013.
|
|
21
|
Wu YQ, Jin M, He LL and Huang AQ: Value of
ultrasonic elastography ratios for differentiating malignant and
benign breast lesions. Diagnostic Imaging Interventional Radiol.
24:134–137. 2015.
|
|
22
|
Zhi H, Xiao XY, Yang HY, Wen YL, Luo BM
and Liang BL: Diagnostic value of strain ratio for differentiation
breast benign and malignant solid lesions with ultrasonic
elastography. Chin J Ultrasonography. 18:589–591. 2009.
|