Introduction
In China, malignant anus neoplasm is a relatively
uncommon type of tumor (1), with
incidence rate of ~1.8–3.34% (2).
Perianal cancer and rectal cancer are main types of malignant anus
neoplasms occurring among males, while anal canal tumor is the main
type of malignant anus neoplasms among females. With the increased
incidence rate of tumors, the diagnosis of tumors becomes more and
more important. Ultrasound (3,4) is an
essential method to assist the diagnosis of malignant anus
neoplasm; therefore, ultrasound is frequently used for staging of
malignant anus neoplasm in clinical practices. Ultrasonic diagnosis
has many advantages, such as no trauma, high sensitivity of
diagnosis, no radioactivity and simple and convenient methods; as a
result, ultrasound has been widely applied in tumor diagnosis.
Ultrasonic elastography (UE) (5) is
an emerging tumor diagnosis technique, which expands the diagnostic
scope of conventional ultrasound in tumors, can indicate and locate
the positions of lesions and can differentiate the nature of
lesions, having obvious advantages in judging the malignancy of
tumors. In this study, some results were acquired from patients
with anal canal masses who were diagnosed with conventional
ultrasound combined with UE.
Patients and methods
Clinical data
One hundred and twenty patients, who were diagnosed
in Shanghai Pudong New Area People's Hospital from December 2014 to
December 2016, were selected; the anal canal masses were detected
by digital rectal examination, then the nature of the masses was
examined and determined using conventional ultrasound and UE, and
all the patients were admitted in our hospital to receive
operation. The study was approved by the Ethics Committee of
Shanghai Pudong New Area People's Hospital and informed consents
were signed by the patients or the guardians.
Apparatus and methods
Hi Vision Avius Color Doppler ultrasonic diagnostic
apparatus (Hitachi, Ltd., Tokyo, Japan), equipped with a 13-5
probe, was used to perform UE and conventional ultrasound
examinations. The positions of anal canal lesions, as well as the
diameters, shape, edge conditions, calcification or not,
thickness/length ratios of masses, in the patients were observed
through ultrasound (6). After that,
conventional ultrasound was switched to UE for examination. The
three-grade classification, including benign, undetermined and
malignant, was applied in conventional ultrasound. The UE scoring
criteria provided by Hitachi, Ltd. were used as references for UE
scoring (7,8), of which UE score ≥3 indicated malignant
lesions.
Statistical analysis
All the experimental results were analyzed using
SPSS 22.0 (IBM, Armonk, NY, USA), and analysis of variance was
performed for comparisons among multiple groups. The enumeration
data were expressed as percent (%), and χ2 test was
applied. The sensitivities and specificities of diagnoses via UE,
conventional ultrasound and UE combined with conventional
ultrasound in malignant anus neoplasm were calculated,
respectively; the receiver operating characteristic (ROC) curves
were used to investigate the diagnostic values of UE, conventional
ultrasound and UE combined with conventional ultrasound in
malignant anus neoplasm. P<0.05 suggested that the difference
was statistically significant.
Results
Basic data
There were 58 male patients and 62 female patients
aged 18–62 years, with an average age of 39.9±11.2 years. All the
postoperative masses of the 120 patients were diagnosed in the
Department of Pathology. Results of pathological diagnosis: There
were 43 cases of malignant anus neoplasm and 77 cases of benign
anus neoplasm. The diameter of the mass was 1.2–3.5 cm, with an
average diameter of 1.6±0.8 cm. Malignant melanoma was not included
in this study (Table I).
 | Table I.Clinical data of patients. |
Table I.
Clinical data of patients.
| Characteristics | Basic data | P-value |
|---|
| Sex |
|
|
| Male | 58 cases | 0.347 |
|
Female | 62 cases |
|
| Age (years) | 39.9±11.2 |
|
| Nature of mass |
|
|
|
Benign | 77 cases | 0.053 |
|
Malignant | 43 cases |
|
| Diameter of mass
(cm) | 1.6±0.8 |
|
| Component of
malignant anus neoplasm |
|
|
|
Cloacogenic carcinoma | 5 | 0.124 |
| Basal
cell carcinoma | 3 |
|
|
Epidermoid carcinoma or
mucoepidermoid carcinoma | 15 |
|
| Squamous
cell carcinoma (SCC) of anal canal | 20 |
|
Among the 120 patients, 77 were diagnosed with
benign lesions and 43 were diagnosed with malignant lesions via
pathological diagnosis for anal canal lesion surgery. Using
conventional ultrasound before operation, 53 patients were
diagnosed with benign anal canal masses and 26 with malignant anal
canal masses; the total accordance rate was 65.8%. Through UE
diagnosis, 66 patients had benign anal canal masses and 39 patients
had malignant anal canal masses, and the total accordance rate was
87.5%. The numbers of patients diagnosed with benign and malignant
masses via UE combined with conventional ultrasound were 77 and 43,
respectively, and the total accordance rate was 92.5%. Compared
with the pathological diagnosis results, 24 cases of benign lesions
were misdiagnosed as malignant ones, and 17 malignant lesions were
misdiagnosed as benign ones in conventional ultrasound before
operation. In preoperative UE, 11 cases of benign lesions were
misdiagnosed as malignant ones, and 4 malignant lesions were
misdiagnosed as benign ones. However, the diagnostic accuracy of UE
combined with conventional ultrasound was relatively high (Table II).
 | Table II.Diagnostic results and accordance
rates. |
Table II.
Diagnostic results and accordance
rates.
| Diagnostic
results |
| Conventional
ultrasound | UE | Conventional
ultrasound + EU | P-value |
|---|
| Benign lesion | Detected | 53 | 66 | 71 | 0.372 |
|
| Misdiagnosed | 24 | 11 | 6 |
|
| Malignant lesion | Detected | 26 | 39 | 40 | 0.859 |
|
| Misdiagnosed | 17 | 4 | 3 |
|
| Accordance rate of
pathological diagnosis (%) |
| 65.8 | 87.5 | 92.5 | 0.725 |
Results of preoperative ultrasound
examinations
Results of conventional ultrasound: Most of the
benign masses were round or oval shape, with well-defined edges;
typical micro-calcification was not observed in the lesions; 88.4%
(38/43) of the malignant lesions had irregular edges, 76.7% (33/43)
of the masses had a thickness/length ratio ≥1, and 62.8% (27/43) of
the masses had micro-calcification. UE results: The elasticity
score of the green region or the red-green region with green as the
main color was 1–2 points, suggesting benign lesions, with
surrounding tissues in green. The elasticity score of the red
region was 3–5 points, suggesting malignant lesions, with
surrounding tissues in red or green (Table III).
 | Table III.Results of preoperative ultrasound
examinations. |
Table III.
Results of preoperative ultrasound
examinations.
| Ultrasound
feature | Conventional
ultrasound |
| UE |
|---|
| Benign lesion | Round and oval
shape | Green: 1–2
points | 92.2% |
|
| Smooth edge |
|
|
|
| No typical
micro-calcification |
|
|
| Thickness/length
ratio ≥1 | 88.4% | Red: 3–5 points | 93.0% |
| Irregular edge | 76.7% |
|
|
|
Micro-calcification | 62.8% |
|
|
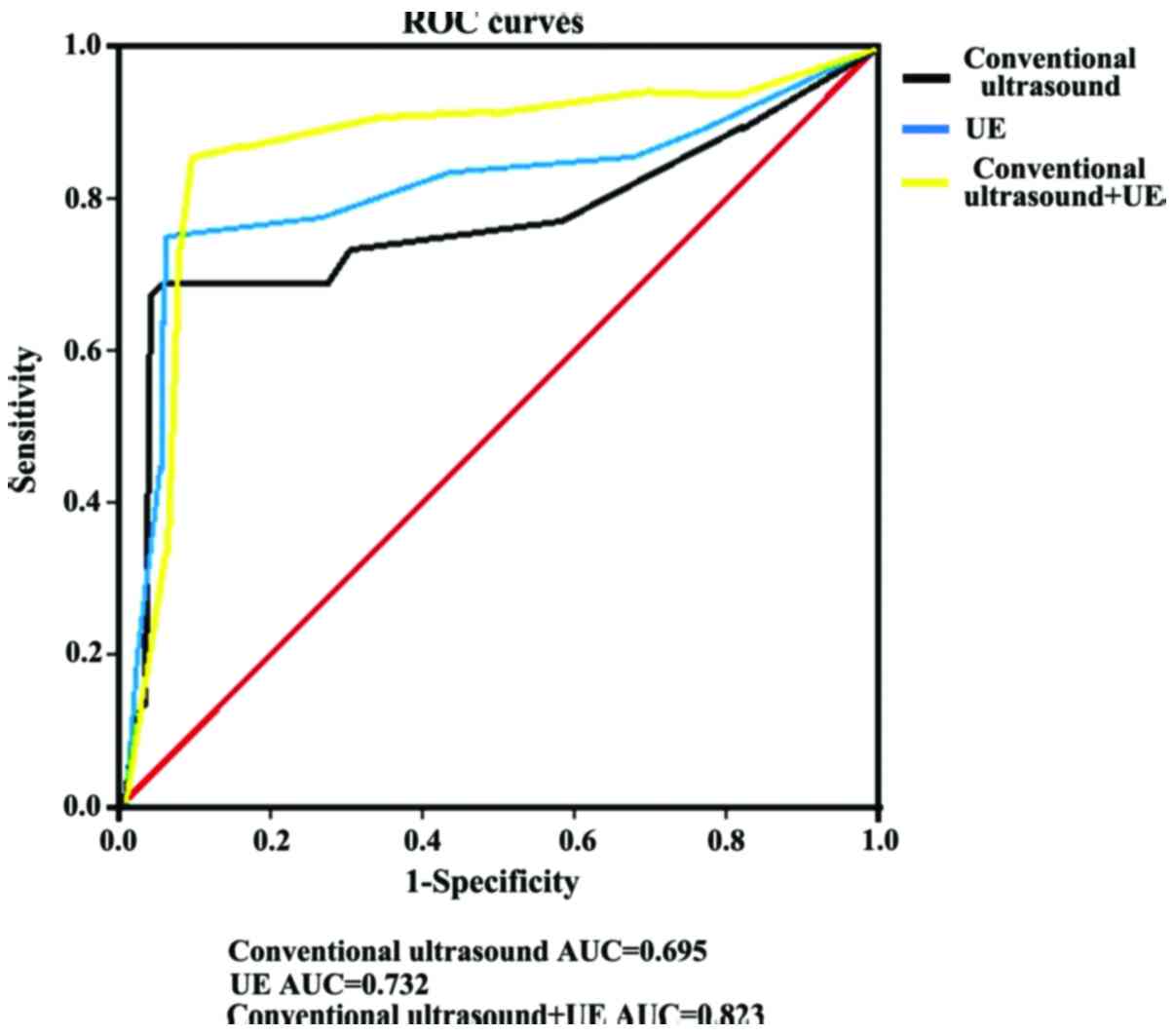
In terms of mass qualitative diagnosis, the
sensitivity and specificity of conventional ultrasound were 60.5
and 68.8%, respectively; those of UE were 90.7 and 85.7%,
respectively, and those of UE combined with conventional ultrasound
were 93.0 and 92.2%, respectively. According to the analysis
results of ROC curve, the area under curve (AUC) of malignant anus
neoplasm diagnosed via UE was 0.732 [95% confidence interval (95%
CI), 0.211–2.534], the AUC via conventional ultrasound was 0.695
(95% CI, 0.517–0.932), and that via UE combined with conventional
ultrasound was 0.823 (95% CI, 0.146–4.643) (Table IV and Fig. 1).
 | Table IV.Analyses of sensitivity and
specificity of three diagnostic methods. |
Table IV.
Analyses of sensitivity and
specificity of three diagnostic methods.
| Sensitivity and
specificity | Conventional
ultrasound | UE | Conventional
ultrasound + EU |
|---|
| Sensitivity (%) | 60.5 | 90.7 | 93.0 |
| Specificity (%) | 68.8 | 85.7 | 92.2 |
| AUC | 0.695 | 0.732 | 0.823 |
| 95% CI | 0.517–0.932 | 0.211–2.534 | 0.146–4.643 |
Discussion
Malignant anus neoplasm (9) is an uncommon type of cancer, but its
incidence rate shows an increasing trend, and the patients with the
disease become increasingly younger (10). Therefore, the screening of malignant
anus neoplasm is becoming more important. Based on ultrasonic
diagnosis, UE (11) conducts further
examinations on the lesions. The detection principles of UE
(12) are as follows: The mass to be
detected is compressed toward the probe, then the distributions of
elastic coefficient and strain of the detected mass are calculated
according to its displacement, and the figures for the results are
formulated. Conventional ultrasound combined with UE can increase
the diagnostic accuracy in malignant anus neoplasm.
In this study, the detection results of conventional
ultrasound in malignant anus neoplasm showed unclear edges,
irregular shapes and increased anterior-posterior diameter. On
determining whether the tumor is malignant or not, thickness/length
ratio >1 is a crucial index (13). The study results revealed that there
were 13 cases of lesions which were diagnosed as undetermined via
conventional ultrasound but were determined as benign via UE; 14
cases had a score >3 points in UE, which were judged as benign
lesions through conventional ultrasound. After the examinations by
UE combined with conventional ultrasound, the sensitivity and
accuracy of the diagnosis of malignant anus neoplasm were improved
significantly, thus avoiding missed diagnosis and misdiagnosis.
Currently, there are plenty of studies on the diagnosis of breast
cancer via UE (14–18); UE has good values in the diagnosis of
breast cancer, its sensitivity and accuracy are relatively high;
there is no great difference in diagnosis of the malignancy of
breast lesion between 5-point scoring evaluation and UE area ratio,
while the diagnosis combined with the two methods can increase the
diagnostic accuracy of tumors. UE has not been completely utilized
as a routine examination for tumors in clinic yet, and there are no
unified diagnostic criteria. Some studies revealed (19–21) that
the malignancy of breast lesion may cause adverse reactions to the
UE diagnostic results, and the accuracy of UE examination is
decreased along with the increased depth of the mass. It was
indicated in the ROC curve that UE had significant values in
diagnosis of malignant anus neoplasm, and that the diagnostic value
of UE combined with conventional ultrasound was greater. Some
studies have revealed that UE has great values in diagnosis of
liver fibrosis (22). In the
examination of masses, on the basis of lesion detection via
conventional ultrasound, lesions that cannot be confirmed by
conventional ultrasound are discovered and diagnosed using UE
examination, and the prognostic value in the lesions needs to be
further investigated.
In this study, the diagnostic effects of UE and
conventional ultrasound in malignant anus neoplasm were studied,
and the results showed that 4 cased were diagnosed as suspected
malignant masses via UE, with a score ≥3 points, which were
diagnosed as benign ones through pathological diagnosis. There was
a relatively high misdiagnosis rate of malignant lesions using UE
alone in this study. It was considered that misdiagnosis may be
associated with many reasons, such as depth of mass and too few
points of interest during the diagnosis. Since there are no reports
related to the diagnosis of UE and conventional ultrasound in
malignant anus neoplasm, a small sample size is adopted in this
study, which lacks representativeness; therefore, the results need
to be verified by large quantity of samples and data findings.
In conclusion, in the clinical diagnosis of
malignant anus neoplasm at present, examinations through
conventional ultrasound combined with UE has a high diagnostic
accuracy, and the devices used during popularization are relatively
simple; therefore, conventional ultrasound combined with UE can be
used as an effective method for preoperative diagnosis of malignant
anus neoplasm.
Acknowledgements
This study is supported by Pu Dong New Area Health
and Family Planning Commission Important Vulnerable Course Project
(no. PWzbr 2017-10) and Pu Dong New Area Health and Family Planning
Commission Subject leader Course Project (no. PWRd 2017-06).
References
|
1
|
Morris V, Rao X, Pickering C, Foo WC,
Rashid A, Eterovic K, Kim T, Chen K, Wang J, Shaw K, et al:
Comprehensive genomic profiling of metastatic squamous cell
carcinoma of the anal canal. Mol Cancer Res. 15:1542–1550. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zimmermann M, Beer J, Bodis S, von Moos R,
Vlachopoulou V, Zwahlen DR and Oehler C: PET-CT guided SIB-IMRT
combined with concurrent 5-FU/MMC for the treatment of anal cancer.
Acta Oncol. 30:1–7. 2017.
|
|
3
|
Zhang XL and Qian LX: Ultrasonic features
of papillary thyroid microcarcinoma and non-microcarcinoma. Exp
Ther Med. 8:1335–1339. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li B, Zhang Y, Yin P, Zhou J and Jiang T:
Ultrasonic features of papillary thyroid microcarcinoma coexisting
with a thyroid abnormality. Oncol Lett. 12:2451–2456. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lu R and Xiao Y: The diagnostic value of
ultrasonic elastography and ultrasonography comprehensive score in
cervical lesions. Zhonghua Yi Xue Za Zhi. 97:2111–2115.
2017.PubMed/NCBI
|
|
6
|
Tyloch JF and Wieczorek AP: The standards
of an ultrasound examination of the prostate gland. Part 2. J
Ultrason. 17:43–58. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hahn S, Lee YH, Lee SH and Suh JS: Value
of the strain ratio on ultrasonic elastography for differentiation
of benign and malignant soft tissue tumors. J Ultrasound Med.
36:121–127. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yağcı B, Erdem Toslak I, Çekiç B, Öz M,
Karakaş BR, Akdemir M, Yıldız S, Süren D and Bova D:
Differentiation between idiopathic granulomatous mastitis and
malignant breast lesions using strain ratio on ultrasonic
elastography. Diagn Interv Imaging. 98:685–691. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Torkzad MR, Kamel I, Halappa VG and
Beets-Tan RG: Magnetic resonance imaging of rectal and anal cancer.
Magn Reson Imaging Clin N Am. 22:85–112. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rödel F, Wieland U, Fraunholz I, Kitz J,
Rave-Fränk M, Wolff HA, Weiss C, Wirtz R, Balermpas P, Fokas E, et
al: Human papillomavirus DNA load and p16INK4a expression predict
for local control in patients with anal squamous cell carcinoma
treated with chemoradiotherapy. Int J Cancer. 136:278–288. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li LJ, Zeng H, Ou B, Luo BM, Xiao XY,
Zhong WJ, Zhao XB, Zhao ZZ, Yang HY and Zhi H: Ultrasonic
elastography features of phyllodes tumors of the breast: A clinical
research. PLoS One. 9:e852572014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mu WJ, Zhong WJ, Yao JY, Li LJ, Peng YL,
Wang Y, Liu LS, Xiao Y, Liu SJ, Wu CJ, et al: Ultrasonic
elastography research based on a multicenter study: Adding strain
ratio after 5-point scoring evaluation or not. PLoS One.
11:e01483302016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mainiero MB, Lourenco A, Mahoney MC,
Newell MS, Bailey L, Barke LD, D'Orsi C, Harvey JA, Hayes MK, Huynh
PT, et al: ACR appropriateness criteria breast cancer screening. J
Am Coll Radiol. 10:11–14. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ahmed M, Jozsa F, Baker R, Rubio IT,
Benson J and Douek M: Meta-analysis of tumour burden in
pre-operative axillary ultrasound positive and negative breast
cancer patients. Breast Cancer Res Treat. 10:1–8. 2017.
|
|
15
|
Diepstraten SC, Sever AR, Buckens CF,
Veldhuis WB, van Dalen T, van den Bosch MA, Mali WP and Verkooijen
HM: Value of preoperative ultrasound-guided axillary lymph node
biopsy for preventing completion axillary lymph node dissection in
breast cancer: A systematic review and meta-analysis. Ann Surg
Oncol. 21:51–59. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Berg WA, Bandos AI, Mendelson EB, Lehrer
D, Jong RA and Pisano ED: Ultrasound as the primary screening test
for breast cancer: Analysis from ACRIN 6666. J Natl Cancer Inst.
108:3672015. View Article : Google Scholar
|
|
17
|
Qi X, Chen A, Zhang P, Zhang W, Cao X and
Xiao C: Mammographic calcification can predict outcome in women
with breast cancer treated with breast-conserving surgery. Oncol
Lett. 14:79–88. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wu X, Lin Q, Lu J, Chen G, Zeng YI, Lin Y,
Chen Y, Wang Y and Yan J: Comparison of mammography and ultrasound
in detecting residual disease following bioptic lumpectomy in
breast cancer patients. Mol Clin Oncol. 4:419–424. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Evans A, Rauchhaus P, Whelehan P, Thomson
K, Purdie CA, Jordan LB, Michie CO, Thompson A and Vinnicombe S:
Does shear wave ultrasound independently predict axillary lymph
node metastasis in women with invasive breast cancer? Breast Cancer
Res Treat. 143:153–157. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mi XK, Liu QR, Zhu L, Sang MX, Guo LR and
Shan BE: Mechanism of the high coagulation state of breast cancer
tissue factor. Eur Rev Med Pharmacol Sci. 21:2167–2171.
2017.PubMed/NCBI
|
|
21
|
Ganott MA, Zuley ML, Abrams GS, Lu AH,
Kelly AE, Sumkin JH, Chivukula M, Carter G, Austin RM and Bandos
AI: Ultrasound guided core biopsy versus fine needle aspiration for
evaluation of axillary lymphadenopathy in patients with breast
cancer. ISRN Oncol. 2014:7031602014.PubMed/NCBI
|
|
22
|
Qi JS, Wang WH and Li FQ: Combination of
interventional adenovirus-p53 introduction and ultrasonic
irradiation in the treatment of liver cancer. Oncol Lett.
9:1297–1302. 2015. View Article : Google Scholar : PubMed/NCBI
|