Introduction
The rapid development of economy and the improvement
of people's living standards allow more patients to accept heart
surgery for the improvement of quality of life including the heart
valve repair or replacement, cardiac surgery and coronary artery
bypass grafting (1). The
preoperative cardiac reserve functions of patients before the heart
surgery are usually poor. Further, the surgical trauma,
intraoperative myocardial ischemia and CPB are also prone to
myocardial ischemia as well as ischemia reperfusion injury leading
to low cardiac output syndrome (2,3).
Therefore, it is very important to strengthen the protection of
cardiac functions and prevention of the myocardial damage in
patients undergoing cardiac surgery. This process would play an
important role in improving the success rates of surgery and
prognosis (4). Brain natriuretic
peptide is a member of natriuretic peptide family. Recombinant
human brain natriuretic peptide (rhBNP) is a kind of medicine for
the treatment of heart failure, and is a recommended drug for acute
as well as chronic heart failure (5). The related research showed that rhBNP
has the ability to maintain the normal cardiac output, dilation of
the pulmonary circulation/coronary circulation, reduction in
cardiac load, protection of ischemic myocardium (5). Moreover, it could also achieve good
clinical effects on heart functions after cardiac surgery (5). In the present study, patients were
treated with the combination of routine treatment with recombinant
human brain natriuretic peptide (rhBNP) after open-heart surgery
and the clinical potential of this combination was evaluated.
Patients and methods
General information
One hundred and fifty patients undergoing open heart
surgery in the Second Hospital of Shandong Universty from August
2015 to July 2016 were randomly divided into control group and
observation group by computer, with 75 cases in each group.
Patients in control group were treated by routine rehabilitation;
patients in the observation group were treated by routine
rehabilitation and rhBNP. Inclusion criteria: i) heart function
grade II–III of American New York Heart Association; ii)
cardiopulmonary bypass support for cardiac surgery includes: valve
repair or replacement, correction of congenital heart disease,
coronary artery and major blood vessel related surgery; and iii)
signed informed consent. Exclusion criteria: i) patients with
cardiac shock and hypotension (SBP <90 mmHg); ii) severe renal
insufficiency; and iii) allergy to the study drug and lactating
women. There was no significant difference between the two groups
of patients in general information (P>0.05), comparability is
shown in Table I. The study was
approved by the Ethics Committee of the Second Hospital of Shandong
Universty and informed consents were signed by the patients and/or
guardians.
 | Table I.Baseline data of two groups. |
Table I.
Baseline data of two groups.
| Item | Observation group
n=75 | Control group
n=75 | t/χ2 | P-value |
|---|
| Age (years) | 30–68 | 30–65 |
|
|
| Sex
(male/female) | 39/36 | 34/41 | 0.053 | 0.513 |
| Average age
(years) | 43.56±6.42 | 43.85±6.53 | 0.274 | 0.784 |
| BMI
(kg/m2) | 22.13±3.45 | 22.76±3.38 | 1.130 | 0.261 |
| Operation type (n,
%) |
|
| 0.042 | 0.874 |
| Valve
repair or replacement | 29 (38.67) | 31 (41.33) |
|
|
|
Correction of congenital heart
disease | 19 (25.33) | 20 (26.67) |
|
|
| Coronary
artery and major blood vessel related surgery | 27 (36.00) | 24 (32.00) |
|
|
| Preoperative cardiac
function (NYHA) |
|
| 0.027 | 0.739 |
| Grade II
(n, %) | 32 (42.67) | 29 (38.67) |
|
|
| Grade III
(n, %) | 43 (57.33) | 46 (61.33) |
|
|
Surgical methods
All patients underwent cardiac surgery with
cardiopulmonary bypass support including: valve repair or
replacement, repair of congenital heart disease, coronary artery
and major blood vessel related surgery. Postoperative patients with
tracheal intubation were sent to ICU to monitor the treatment along
with maintenance of circulation and smooth respiration. Further,
the late extubation extra corporeal circulation machine (German
Stockert-sc type) and membrane oxygen device were used in the two
groups of patients for the purpose of cardiopulmonary bypass.
Compounds sodium chloride (900 ml), dexamethasone (10 mg), mannitol
(250 ml) were used as the pre flushing fluids. Natriuretic peptide
(Chengdu Nuodikang Biological Pharmaceutical Co. Ltd.: license
number: NMPN S20050033) was added in observation group. Usage and
dosage: Patients began to use the above dose regime within 24 h
after surgery with continuous use of 24–48 h. The recommended
medication time was more than 48 h.
Evaluation criterion
Venous blood 4 ml of patients was collected before
operation, after operation and 7 days after the operation. The
N-terminal pro-brain natriuretic peptide (NT-proBNP) of patients
were detected by automatic chemiluminescence immunoassay. The left
ventricular ejection fraction (LVEF) was measured by color Doppler
echocardiography before operation, after operation and 7 days after
the operation. Cardiac function [cardiac output (CO), pulmonary
capillary wedge pressure (PAWP), central venous pressure (CVP)] of
patients were recorded and observed before the operation, after the
operation and 7 days after the operation. The ventilator support
time and ICU retention time of two groups of patients were
recorded. The incidence rate of postoperative complications was
observed. Blood pressure (BP), heart rate (HR) and blood oxygen
saturation (SaO2) were monitored and observed after 7 days of
treatment.
Statistical analysis
SPSS 19.0 (SPSS Inc., Chicago, IL, USA) software was
used for data processing. Measurement data are expressed by mean ±
SD, with t-test; count data were expressed by ratio with
χ2 test, and P<0.05 was considered to indicate a
statistically significant difference.
Results
T-proBNP levels of all patients
improved after operation
NT-proBNP levels of patients in both groups
decreased 7 days after operation, and the decrease of NT-proBNP
level in observation group was significantly higher than control
group (P<0.05) (Table II).
 | Table II.Comparison of NT-proBNP levels in two
groups. |
Table II.
Comparison of NT-proBNP levels in two
groups.
| Group | No. of cases | Before operation | Before medication
after operation | Seven days after
medication | F-value | P-value |
|---|
| Observation
group | 75 | 1315.35±221.14 | 1934.06±321.13 | 472.23±51.02 | 76.312 | <0.001 |
| Control group | 75 | 1326.06±231.23 | 1963.73±335.25 | 1062.76±311.17 | 75.431 | <0.001 |
| t-value | 0.290 | 0.129 | 16.219 |
|
|
|
| P-value | 0.772 | 0.897 | <0.001 |
|
|
|
The LVEF of patients in the groups
increased after operation
LVEF of patients in observation group was
significantly higher than that in control group after 7 days of
medication (P<0.05). (Table
III).
 | Table III.Comparison of changes of LVEF in two
groups. |
Table III.
Comparison of changes of LVEF in two
groups.
| Group | No. of cases | Before operation | Before medication
after operation | Seven days after
medication | F-value | P-value |
|---|
| Observation
group | 75 | 43.35±3.14 | 50.06±3.13 | 56.23±3.02 | 9.432 | <0.001 |
| Control group | 75 | 43.06±3.23 | 49.73±3.25 | 51.76±3.17 | 7.581 | <0.001 |
| t-value | 0.558 | 0.633 | 8.842 |
|
|
|
| P-value | 0.578 | 0.527 | <0.001 |
|
|
|
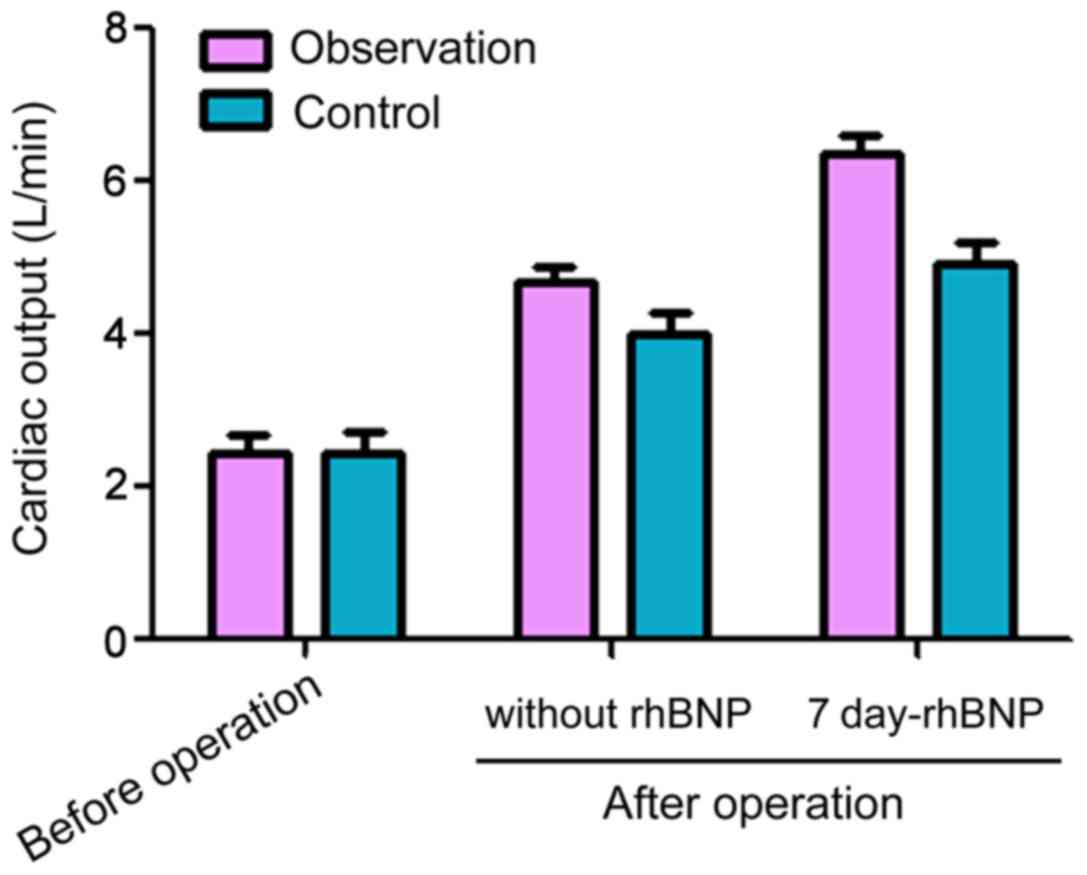
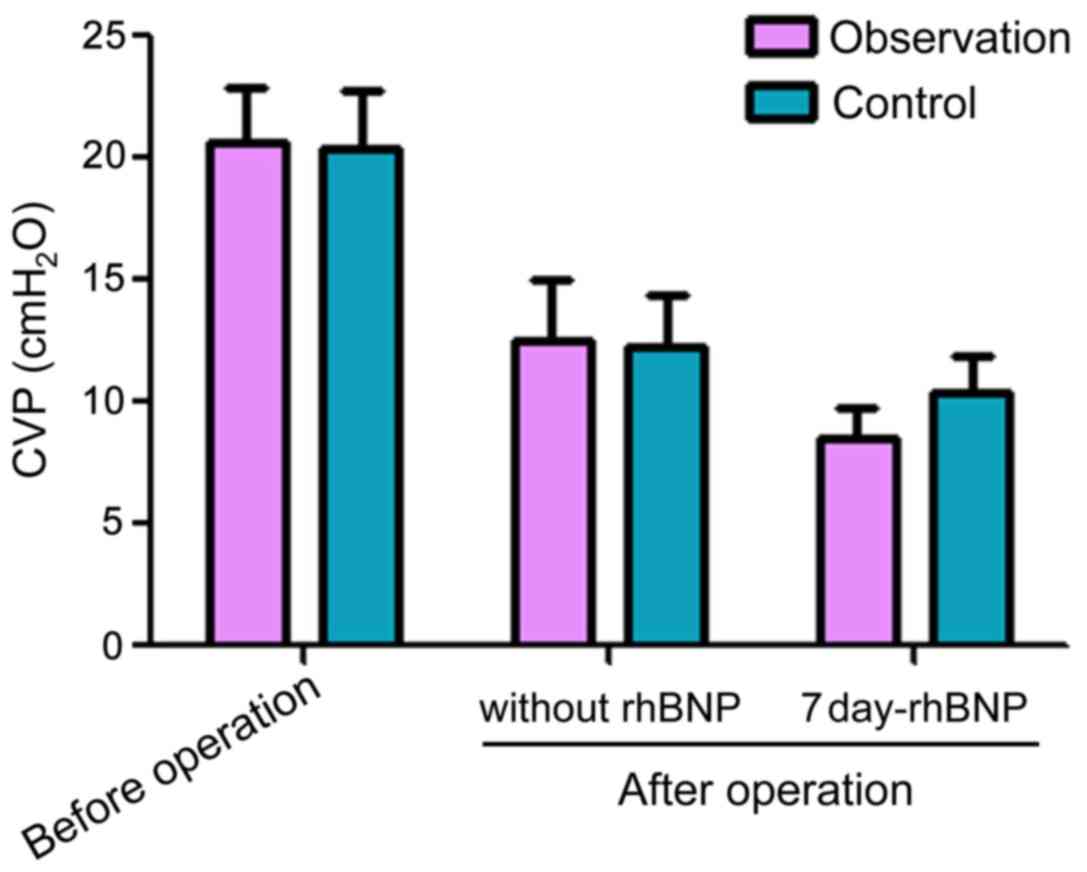
Comparison of the heart function
indexes of two groups
The indexes of CO, PAWP and CVP were significantly
improved in the two groups compared with before operation, and the
improvement degree of the observation group was better than that of
the control group 7 days after medication (P<0.05) (Figs. 1–3).
Mechanical ventilation time, ICU
indwelling time and postoperative complications of two groups of
patients
Compared with the control group, mechanical
ventilation time and ICU indwelling time in the observation group
were significantly shorter than those in the control group.
Further, the incidence of postoperative complications was
significantly lower than that of the control group, and the
differences were statistically significant (Table IV).
 | Table IV.Comparison of ventilator support and
ICU indwelling time and postoperative complications of two groups
of patients. |
Table IV.
Comparison of ventilator support and
ICU indwelling time and postoperative complications of two groups
of patients.
| Group | No. of cases | Ventilator support
time (h) | ICU indwelling time
(h) | Postoperative
complication (n,%) |
|---|
| Observation
group | 75 | 12.15±1.34 | 26.16±3.33 | 4 (5.33) |
| Control group | 75 | 16.76±1.53 | 36.83±3.45 | 13 (17.33) |
| t-value | 19.630 | 19.271 | 4.247 |
|
| P-value | <0.001 | <0.001 | 0.039 |
|
Comparison of vital signs in two
groups of patients during perioperative period
SBP, DBP, HR, and SaO2 indexes of the observation
group were significantly better than those of the control group
(P<0.05) (Table V).
 | Table V.Comparison of vital signs in two
groups of patients during perioperative period. |
Table V.
Comparison of vital signs in two
groups of patients during perioperative period.
| Group | No. of cases | SBP (mmHg) | DBP (mmHg) | HR (beats/min) | SaO2 (%) |
|---|
| Observation
group | 75 | 115.35±3.14 | 64.06±3.13 | 90.06±8.17 | 98.23±1.02 |
| Control group | 75 | 108.06±3.23 | 59.73±3.25 | 95.62±9.29 | 94.76±1.17 |
| t-value |
| 14.015 | 8.311 | 3.899 | 19.360 |
| P-value |
| <0.001 | <0.001 | 0.0001 | <0.001 |
Discussion
Cardiac reserve function is often affected after
heart surgery due to surgical trauma and myocardial ischemia.
Moreover, these patients are prone to myocardial ischemia and
ischemia reperfusion injury that in turn leads to a variety of
complications like heart failure, endotoxemia, the systemic
inflammatory response syndrome and low cardiac output syndromes
(6,7). The low cardiac output syndrome is the
most severe complication with high mortality, and there are many
factors of incidence, such as poor preoperative cardiac function in
patients, myocardial ischemia time, poor cardiac malformation
correction, intracardiac operation time, aortic clamping time,
postoperative blood volume insufficiency, arrhythmia, cardiac
tamponade and pulmonary artery hypertension (8). The reduction of the myocardial damage
post-cardiac surgery and the protection of heart function have
become the focus of clinical attention. Moreover, they have a
profound impact on the success rate of surgery and prognosis of
patients (9).
The secretion of NT-proBNP in patients with heart
disease is closely related to the ventricular pressure load and
volume load. When the ventricular wall tension load in patients
increases, the NT-proBNP level would rise sharply. Moreover, the
monitoring of it could prevent postoperative complications
(10,11). Moreover, the plasma NT-proBNP levels
of patients would continue to rise after open-heart surgery
(12). The results of the present
study showed that the NT-proBNP of patients of both groups
increased after operation, which might be affected by anesthesia,
surgical trauma, hemodynamic abnormalities, inflammatory
stimulation, CPB, myocardial damage and decreased contractile
ability. However, the levels of NT-proBNP in the two groups began
to decrease after 7 days of treatment. This was the result after
drug treatment that included inflammatory reaction of patients
(13).
The postoperative CO, PAWP and CVP indicators of the
two groups of patients were significantly improved and the
observation group was significantly better than the control group
after 7 days of treatment (P<0.05). The above observation could
be justified in the light of the fact that the natriuretic peptide
has balanced expansion arteriovenous/coronary artery diastolic
function (14). A related study also
showed improvements in the hemodynamic parameters after 15 min of
treatment (15). The natriuretic
peptide could improve the heart rate through the comprehensive
effect (16). The results of this
study showed that postoperative LVEF were higher than preoperative
in the two groups of patients, and the observation group was
significantly higher than the control group after 7 days of
treatment (P<0.05). Moreover, natriuretic peptide has ability to
directly affect myocardial cells, thereby reducing myocardial
oxygen consumption, with inhibition of excessive stress reaction of
the circulatory system, so as to have a protective effect on the
heart (17,18).
In the present study, SBP, DBP, HR, and SaO2 indexes
of the observation group were significantly better than those of
the control group (P<0.05). This is due to the natriuretic
peptide that has positive chronotropic effect, which not only
caused reflex tachycardia, but also inhibited cardiac sympathetic
nerve activity, thereby adjusted the blood pressure (19). Moreover, ICU indwelling time and
ventilator support were also reduced via natriuretic peptide
treatment. In summary, recombinant human brain natriuretic peptide
(rhBNP) could protect the cardiac functions of patients after
open-heart surgery, and it is safe and reliable. However, for the
concrete conclusions, the study needs further exploration in future
as the sample size and time were limited in the present study.
References
|
1
|
Pontoni G, Ferrari S, Gabbieri D, Pedulli
M, Gambetti D, Ghidoni I and Rigatelli M: FC28-04 - Quality of life
assessment after cardiac surgery in octogenarians: Is it really
feasible? Eur Psychiatry. 26:19742011.http://www.em-consulte.com/article/289736/fc28-04-quality-of-life-assessment-after-cardiac-s
View Article : Google Scholar
|
|
2
|
Massé L and Antonacci M: Low cardiac
output syndrome: Identification and management. Crit Care Nurs Clin
North Am. 17:375–383. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Algarni KD, Maganti M and Yau TM:
Predictors of low cardiac output syndrome after isolated coronary
artery bypass surgery: Trends over 20 years. Ann Thorac Surg.
92:1678–1684. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mangano DT, Hollenberg M, Fegert G, Meyer
ML, London MJ, Tubau JF and Krupski WC: The Study of Perioperative
Ischemia (SPI) Research Group: Perioperative myocardial ischemia in
patients undergoing noncardiac surgery - I: Incidence and severity
during the 4 day perioperative period. J Am Coll Cardiol.
17:843–850. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
He XM, Chen L, Luo JB, Feng XX, Zhang YB,
Chen QJ, Ji XL and Wang TS: Effects of rhBNP after PCI on
non-invasivehemodynamic in acute myocardial infarction patients
with left heart failure. Asian Pac J Trop Med. 9:791–795. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Targońska S, Kozioł MM, Czajkowski M,
Stążka J and Kozioł-Montewka M: Sternal wound complications after
cardiac surgery - a case report. Wiad Lek. 68:95–98. 2015.(In
Polish). PubMed/NCBI
|
|
7
|
Kerneis CK, Lafarge AL, Larnier LL,
Scalbert F, Brusset AB, Estagnasie PE and Squara PS: Bowel and
related complications after cardiac surgery. Crit Care. 19 Suppl
1:P3752015. View
Article : Google Scholar
|
|
8
|
Howell NJ, Ashrafian H, Drury NE,
Ranasinghe AM, Contractor H, Isackson H, Calvert M, Williams LK,
Freemantle N, Quinn DW, et al: Glucose-insulin-potassium reduces
the incidence of low cardiac output episodes after aortic valve
replacement for aortic stenosis in patients with left ventricular
hypertrophy: Results from the Hypertrophy, Insulin, Glucose, and
Electrolytes (HINGE) trial. Circulation. 123:170–177. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Howard BT, Iles TL, Coles JA, Sigg DC and
Iaizzo PA: Reversible and irreversible damage of the myocardium:
Ischemia/reperfusion injury and cardioprotectionHandbook of Cardiac
Anatomy, Physiology, and Devices. 3rd edition. Springer
International Publishing; New York: 2015, View Article : Google Scholar
|
|
10
|
Madamanchi C, Alhosaini H, Sumida A and
Runge MS: Obesity and natriuretic peptides, BNP and NT-proBNP:
Mechanisms and diagnostic implications for heart failure. Int J
Cardiol. 176:611–617. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oremus M, Don-Wauchope A, McKelvie R,
Santaguida PL, Hill S, Balion C, Booth R, Brown JA, Ali U, Bustamam
A, et al: BNP and NT-proBNP as prognostic markers in persons with
chronic stable heart failure. Heart Fail Rev. 19:471–505. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Boer BP, Vieira ML, Sampaio RO, Abensur H,
Oliveira AG, Fernandes JR and Grinberg M: Correlation to NT-ProBNP
and remodeling after cardiac surgery. Arq Bras Cardiol.
100:469–475. 2013.PubMed/NCBI
|
|
13
|
Recombinant Human Brain Natriuretic
Peptide Multicenter Clinical Study Group, . Hu DY: Efficacy and
safety of intravenous recombinant human brain natriuretic peptide
in patients with decompensated acute heart failure: A multicenter,
randomized, open label, controlled study. Zhonghua Xin Xue Guan
Bing Za Zhi. 39:305–308. 2011.(In Chinese). PubMed/NCBI
|
|
14
|
Xing K, Fu X, Wang Y, Li W, Gu X, Hao G,
Miao Q, Li S, Jiang Y, Fan W, et al: Effect of rhBNP on renal
function in STEMI-HF patients with mild renal insufficiency
undergoing primary PCI. Heart Vessels. 31:490–498. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang S and Wang Z: Effect of recombinant
human brain natriuretic peptide (rhBNP) versus nitroglycerin in
patients with heart failure: A systematic review and meta-analysis.
Medicine (Baltimore). 95:e47572016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhu XQ, Hong HS, Lin XH, Chen LL and Li
YH: Changes in cardiac aldosterone and its synthase in rats with
chronic heart failure: an intervention study of long-term treatment
with recombinant human brain natriuretic peptide. Braz J Med Biol
Res. 47:646–654. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang J, Zhang L, Wu Q, Liu H and Huang L:
Recombinant human brain natriuretic peptide therapy combined with
bone mesenchymal stem cell transplantation for treating heart
failure in rats. Mol Med Rep. 7:628–632. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bakkehaug JP, Kildal AB, Engstad ET,
Boardman N, Næsheim T, Rønning L, Aasum E, Larsen TS, Myrmel T and
How OJ: Response to letter regarding article, ‘Myosin activator
omecamtiv mecarbil increases myocardial oxygen consumption and
impairs cardiac efficiency mediated by resting myosin ATPase
activity’. Circ Heart Fail. 8:11422015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lyu T, Zhao Y, Zhang T, Zhou W, Yang F, Ge
H, Ding S, Pu J and He B: Natriuretic peptides as an adjunctive
treatment for acute myocardial infarction: Insights from the
meta-analysis of 1,389 patients from 20 trials. Int Heart J.
55:8–16. 2014. View Article : Google Scholar : PubMed/NCBI
|