Introduction
The mechanism of neonatal respiratory distress
syndrome (RDS) is still under study, but some studies have
suggested that oxidation/anti-oxidation disorders and inflammatory
responses may play essential roles in the pathogenesis (1). However, new developments have indicated
apoptosis as being another player. Cell apoptosis is a cellular
process of programmed cell death under the influence of several
gene products, and it is a recurring process necessary to maintain
a healthy internal environment. Events leading to apoptosis
disturbance may cause abnormal body development, deformation and
even death, and apoptosis has been associated with a variety of
diseases, such as endocrine disorders and tumors (2,3). It has
been confirmed that B-cell lymphoma gene-2 (Bcl-2) and cysteine
aspartic protease-3 (caspase-3) activate apoptosis cascades and are
associated with the development of neonatal RDS (4). In this study, the expression levels of
caspase-3 and Bcl-2 in alveolar lavage fluid of patients with
neonatal RDS and different thoracic X-ray grades were compared, so
as to investigate the correlation between the expression levels of
caspase-3 and Bcl-2 and the prognosis of neonatal RDS.
Materials and methods
General material
In total, 150 infants with neonatal RDS who
underwent alveolar lavage therapy in People's Hospital of Yucheng
City from December, 2015 to October, 2016 were enrolled in the
study. The diagnostic criteria of RDS in the fourth edition of
‘Practical Neonatology’ were adopted; progressive dyspnea occurred
within 4 h after birth and was accompanied by expiratory grunts,
results of thoracic X-ray examination included RDS3 or RDS4, and
blood gas analysis showed PaO2 <50 mmHg (6.6 kPa) or
PaCO2 >60 mmHg (7.8 kPa).
Inclusion criteria: i) The RDS occurred within 4 h
of birth; ii) the gestational age was not more than 37 weeks; iii)
the birth weight was less than 2.5 kg; iv) guardians of infants
agreed to cooperate with the study and signed the informed
consent.
Exclusion criteria: i) Patients diagnosed with
infection in prenatal diagnosis; ii) infants with shock or severe
asphyxia; iii) patients with lung or cardiac dysplasia; iv)
patients with severe genetic diseases; v) infants with suspected
chromosomal disease. The study was appoved by the Ethics Committee
of People's Hospital of Yucheng City.
Grouping of subjects
Hundred and fifty patients with neonatal RDS
receiving alveolar lavage therapy were divided into four groups:
RDS1 (group A, n=42), RDS2 (group B, n=38), RDS3 (group C, n=38)
and RDS4 (group D, n=32) according to thoracic X-ray film grading.
The RDS X-ray grading comprised four classifications: In RDS1, the
transparency of the whole lung was reduced or a diffuse net and
particle shadow appeared on both lungs, but the contours of the
heart shadow could be clearly observed. In RDS2, the transparency
of the whole lung was reduced, a diffuse particle shadow appeared,
patchy high density shadow spots could be observed in partial
pulmonary fields, the lung markings could not be identified, and
significant air bronchogram was present. In RDS3, the transparency
of the whole lung was reduced significantly, a large-particle
shadow covered the lungs, air bronchogram was present, all lung
markings disappeared, and the heart and diaphragmatic surfaces were
unclear. In RDS4, a compact shadow was uniform across the pulmonary
field, air bronchogram was partially clear or unclear, heart and
diaphragmatic surfaces could not be identified, and white lung
syndrome occurred.
Research methods
Bronchoalveolar lavage therapy
In this study, 150 cases of neonatal RDS underwent
bronchoalveolar lavage with a bronchofiberscope. Briefly, all
subjects received conventional sedation. A tracheal catheter was
used to drop 37°C sterile saline (0.5 ml/kg each time) into the
bronchial tubes. Oxygen was monitored and supplied three times
using a resuscitator. A suction tube was inserted into the tracheal
catheter or lifted up slightly when faced with resistance.
Aspiration was done under negative pressure of less than 6 kPa, the
catheter was gradually withdrawn within 0.5 min. The procedures
were performed three times on both sides of the bronchi. The
alveolar lavage fluid retrieved was centrifuged at 3,200 × g for 10
min and the supernatant was collected.
Monitoring and recording of clinical
variables
Conventional blood pressure, heart rate and
respiratory monitoring were performed for all infants. After the
procedures, the oxygen uptake score, oxygenation index and mean
airway pressure were analyzed.
The Apgar score 1 min after birth was used to
evaluate the neonate's condition. The hospital stays, complication
and death rates of all patients were recorded, and the expression
levels of caspase-3 and Bcl-2 in the alveolar lavage fluid were
determined.
Detection of the protein expression
level of caspase-3 in bronchoalveolar lavage fluid via
enzyme-linked immunosorbent assay (ELISA)
Standard ELISA experiments were conducted to
determine the bronchoalveolar lavage fluid levels of caspase-3. A
coating diluent of antibody was added to each sample at appropriate
concentrations and incubated at 37°C for 4 h. Sealing of
enzyme-labeled reaction wells was achieved using 5% calf serum at
37°C for 40 min. Next, the samples to be tested were added and
diluted to 1:100; enzyme-labeled antibodies were added and diluted
to 1:40. Finally, the substrate solution TMB-hydrogen peroxide urea
solution was added in the dark at 37°C for 5 min, followed by
termination of the reaction and color development; and the
wavelength at 450 nm was detected.
Detection of Bcl-2 gene expression
levels in bronchoalveolar lavage fluid via polymerase chain
reaction (PCR)
An RNA extraction kit was used to extract the total
RNA in the samples in strict accordance with the manufacturer's
instructions. After gel electrophoresis, the concentration of RNA
was determined using a photometer (Bio-Rad Laboratories, Hercules,
CA, USA). For annealing of primers, 2 µg RNA samples and 4 µl of
OligoPrimer were added into 18 µl non-enzyme water at 70°C for 10
min. Then 8 µl 5X buffer, 2 µl dNTP mixture, 1 µl RNase inhibitor
and RNaseM-MLV12Ul were added and supplemented with non-enzyme
water to 40 µl. The reactions were incubated at 42°C for 60 min and
then at 70°C for 15 min. After the reaction, the samples were
stored in a refrigerator. At a later time, PCR quantitative
detections were carried out under standard conditions using 40
cycles of 95°C for 30 sec, and 60°C for 30 sec, in a thermocycler.
See Table I for primer
sequences.
 | Table I.PCR primers. |
Table I.
PCR primers.
| Gene | Primer sequences | Primer length
(bp) |
|---|
| β-actin | F:
5-GCCAACACAGTGCTGTCTG-3 |
|
|
| R:
5-CACATCTGCTGGAAGGTGG-3 | 185 |
| Bcl-2 | F:
5-TTCTTTGAGTTCGGTGGGGTC-3 |
|
|
| R:
5-TGCATATTTGTTTGGGGCAGG-3 | 96 |
Statistical analysis
SPSS 20.0 software (SPSS Inc., Chicago, IL, USA) was
used for data analysis in this study. Analysis of variance was used
for measurement data. The results are presented as mean ± standard
deviation. The statistical methods used in the study included
t-test, Chi-square test and Pearsons correlation analysis. A
P<0.05 suggested that a given difference was statistically
significant.
Results
Neonatal Apgar scores of child
patients in the four groups
General survey results showed that there were no
significant differences in terms of gestational age, body weight
and time from birth to onset of symptoms among the infants in the
four groups (P>0.05). The Apgar scores at 1 min after birth in
groups A-D were low, and differed in a statistically significant
manner among the four groups, with scores decreasing with each
increase in severity evidenced by the X-ray classification group
(P<0.05) (Table II).
 | Table II.Neonatal Apgar scores of child
patients in the four groups. |
Table II.
Neonatal Apgar scores of child
patients in the four groups.
| Group | Gestational age
(weeks) | Body weight (kg) | Apgar score (1 min
after birth) | Time from birth to
onset (hours) |
|---|
| Group A (n=42) | 33.75±1.53 | 2.12±0.43 | 6.91±0.86 | 3.57±0.11 |
| Group B (n=38) | 32.78±2.31 | 2.05±0.39 | 6.50±0.92 | 3.09±0.51 |
| Group C (n=38) | 33.09±1.67 | 2.10±0.46 | 6.23±0.41 | 3.24±0.33 |
| Group D (n=32) | 33.41±1.61 | 2.01±0.47 | 5.78±0.30 | 3.15±0.40 |
| χ2 | 0.05 | 0.29 | 15.741 | 2.374 |
| P-value | 0.12 | 0.35 | 0.01 | 0.66 |
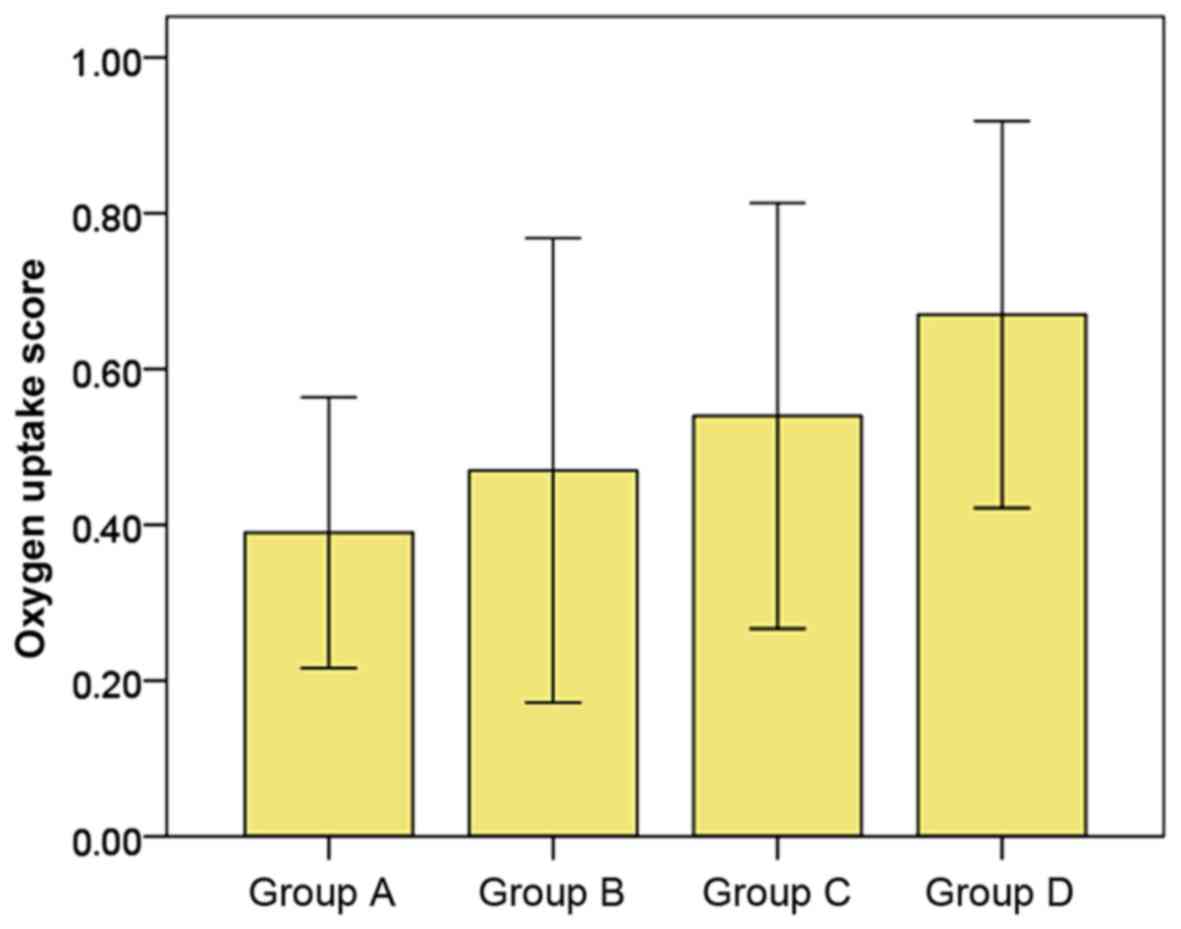
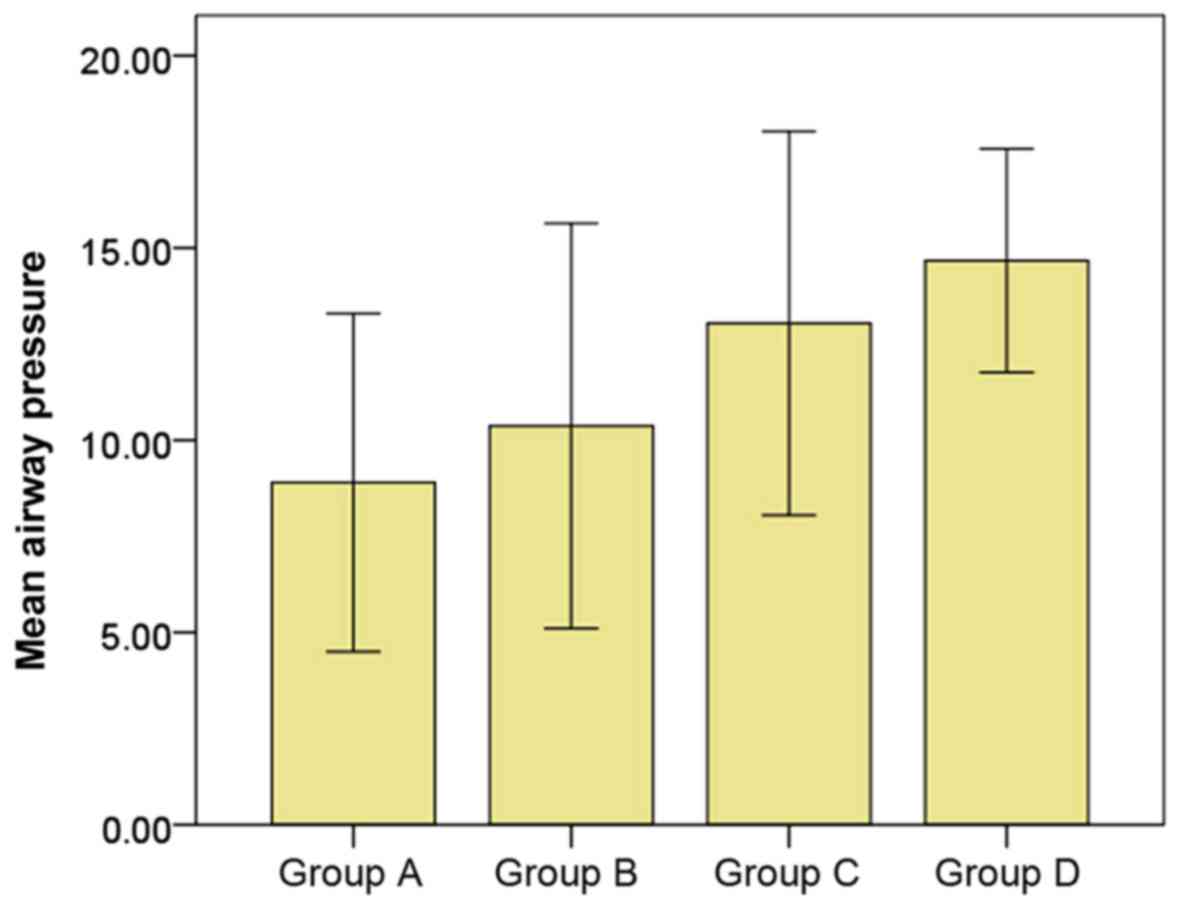
Comparisons of oxygen uptake score,
oxygenation index and mean airway pressure among the four
groups
The patients with higher thoracic X-ray grading
classification (from groups A to D) with RDS had the oxygen uptake
scores, oxygenation indexes and mean airway pressures higher with
each step in the severity classification ladder, and there were
statistically significant differences among the four groups
(P<0.05) (Table III and
Figs. 1–3).
 | Table III.Comparisons of oxygen uptake scores,
oxygenation indexes and mean airway pressures among the four
groups. |
Table III.
Comparisons of oxygen uptake scores,
oxygenation indexes and mean airway pressures among the four
groups.
| Group | Oxygen uptake
score | Oxygenation
index | Mean airway
pressure |
|---|
| Group A (n=42) | 0.39±0.07 | 11.52±2.90 | 8.90±1.77 |
| Group B (n=38) | 0.47±0.12 | 15.26±3.12 | 10.37±2.12 |
| Group C (n=38) | 0.54±0.11 | 22.50±4.08 | 13.04±2.01 |
| Group D (n=32) | 0.67±0.10 | 32.83±5.05 | 14.67±1.17 |
| χ2 | 7.845 | 11.303 | 7.920 |
| P-value | <0.001 | 0.002 | 0.002 |
Comparisons of caspase-3 and Bcl-2
expression levels in alveolar lavage fluid among the four
groups
The average caspase-3 expression levels in alveolar
lavage fluid increased from group A to D. On the contrary, the
average Bcl-2 expression levels decreased from group A to D; and
there were statistically significant differences among the four
groups (P<0.05) (Table IV).
 | Table IV.Comparisons of caspase-3 and Bcl-2
expression levels in alveolar lavage fluid among the four
groups. |
Table IV.
Comparisons of caspase-3 and Bcl-2
expression levels in alveolar lavage fluid among the four
groups.
| Group | Caspase-3 expression
level (ELISA, ng/l) | Bcl-2 expression
level (PCR) |
|---|
| Group A (n=42) | 38.20±5.06 | 4.85±0.45 |
| Group B (n=38) | 41.78±6.53 | 4.05±0.22 |
| Group C (n=38) | 46.39±6.21 | 3.27±0.08 |
| Group D (n=32) | 51.07±9.46 | 3.01±0.09 |
| χ2 | 8.873 | 9.762 |
| P-value | 0.001 | <0.001 |
Comparisons of hospital stay lengths,
complication and death rates among the four groups
The hospital stay lengths, and complication and
death rates got significantly worse in a sequential manner from
groups A to D (P<0.05) (Table
V).
 | Table V.Comparisons of hospital stay lengths,
and complications and death rates among the four groups. |
Table V.
Comparisons of hospital stay lengths,
and complications and death rates among the four groups.
| Group | Hospital stays
(day) | Complications
(n) | Death rate (n,
%) |
|---|
| Group A (n=42) | 13.37±3.35 | 3.14±0.94 | 2/42 (4.76) |
| Group B (n=38) | 18.32±4.31 | 4.17±0.61 | 4/38 (10.53) |
| Group C (n=38) | 20.14±3.09 | 6.34±1.21 | 5/38 (13.16) |
| Group D (n=32) | 24.65±6.37 | 9.55±1.64 | 8/32 (25.00) |
| χ2 | 8.546 | 7.322 | 7.397 |
| P-value | 0.002 | 0.012 | 0.003 |
Analysis of correlations of caspase-3
and Bcl-2 expression levels in alveolar lavage fluid with oxygen
uptake score, oxygenation index and mean airway pressure
The correlations of alveolar lavage fluid expression
levels of caspase-3 and Bcl-2 with oxygen uptake score, oxygenation
index and mean airway pressure, in infants with RDS, were analyzed
using Pearsons correlation analysis. The results showed a caspase-3
positive area positively correlated with oxygen uptake score,
oxygenation index and mean airway pressure (P<0.05); and a Bcl-2
expression level that was negatively correlated with oxygen uptake
score, oxygenation index and mean airway pressure (P<0.05). See
Table VI for values.
 | Table VI.Analysis of correlations of caspase-3
and Bcl-2 expression levels with oxygen uptake score, oxygenation
index and mean airway pressure. |
Table VI.
Analysis of correlations of caspase-3
and Bcl-2 expression levels with oxygen uptake score, oxygenation
index and mean airway pressure.
| Index | Oxygen uptake
score | Oxygenation
index | Mean airway
pressure |
|---|
| Caspase-3 positive
area | 0.039 | 0.022 | 0.015 |
| Bcl-2 expression
level | −0.003 | −0.021 | −0.012 |
Discussion
Neonatal RDS refers to a condition with respiratory
failure and progressive respiratory distress shortly after the
birth of an infant due to the lack of pulmonary surfactant and
end-expiratory alveolar collapse, and in which an initial symptom
is respiratory acidosis. In case of deterioration, the condition
develops into metabolic acidosis, greatly affecting the life
quality and survival rate of the newborn (5,6). The
main clinical manifestations include cyanosis, polypnea,
respiratory moaning inspiratory three depressions sign, and air
bronchogram and ground-glass changes on chest X-rays. It is
accepted that neonatal deaths due to neonatal RDS account for ~30%
of the total neonatal deaths, and neonatal RDS is one of the major
diseases leading to serious sequelae and death of the newborn. The
treatment of neonatal RDS aims at reducing mortality rates, improve
the prognosis and decrease the incidence of complications.
The development of multiple complications is closely
related to degree to which apoptosis is stimulated. The process of
apoptosis is very complex and usually influenced by the caspase and
the Bcl-2 family of factors (7,8).
Caspase-3 plays an important role in the protease cascade cleavage,
which can hydrolyze apoptotic proteins in cells, promoting
apoptosis of such cells. Other pathways like the mitochondrial
pathway are also important; when an apoptosis factor stimulates
cells, mitochondria can produce apoptosis factors, inducing cell
death (9–11). In the relationship between caspase-3
and neonatal RDS, caspase-3 is involved in the pathogenesis of
neonatal RDS in three ways. First, it affects the activity and
functions of major regulatory proteins effectively producing
phagocytosis. Second, it directly damages lung tissue cells.
Caspase-3 can cleave Lamin A, thus causing chromatin aggregation,
nuclear lamina collapse and changes in the nucleus. Third and
finally, caspase-3 can reduce the activity of DNase inhibitors and
alter the homeostatic level. It is known that the expression of
caspase-3 protease rises in the initial stages of acute necrotizing
pancreatitis-associated lung injury in rats, and reaches a peak
after 48 h (12). In this study, the
expression levels of caspase-3 in alveolar lavage fluid increased
with the severity of the condition in the patients (from patients
in groups A to D), and there were statistically significant
differences among the four groups (P<0.05). Furthermore,
Pearsons analysis showed a caspase-3 positive area that was
positively correlated with oxygen uptake score, oxygenation index
and mean airway pressure (P<0.05). These findings are consistent
with the degree of pathological damage of the lung tissues in
neonatal RDS patients, suggesting that the increased protein
expression of caspase-3 has a certain impact on lung injury.
The Bcl-2 family of proteins is prevalent in humans
and animals, where its main role is to inhibit apoptosis and
promote proliferation. The Bcl-2 gene inhibits apoptosis in three
ways (13–15): First, through its action as an
antioxidant; second, through its inhibition of the production of
endoplasmic reticulum calcium ions; and finally, through its
interaction with other apoptosis factors like Bax. Activated Bcl-2
can promote the migration and proliferation of endothelial cells
and inhibit apoptosis (16–18). It is generally believed that the
pathogenesis of neonatal RDS is due to the large-area of damage to
the alveolar-capillary membrane, which in turn causes atelectasis
and pulmonary edema. During the pathological process, pulmonary
vascular and alveolar epithelial endothelial cells are
progressively induced into apoptosis, and this apoptosis mode may
be related to the mediation by inflammatory factors. The Bcl-2 gene
inhibits apoptosis of cells, antagonizes caspase-3, makes the cells
resistant to apoptosis-stimulating factors, inhibits the
decomposition of proteins in cells and prolongs the cell survival
cycle. Even though the link between apoptosis and inflammation is
still being actively studied, both processes are closely related to
the expression of the Bcl-2 protein. In this study, the average
expression levels of Bcl-2 in alveolar lavage fluid decreased
sequentially from groups with less severe disease to those with
more severe conditions (from group A to D), and there were
statistically significant differences among the four groups
(P<0.05). Moreover, the expression level of Bcl-2 was negatively
correlated with oxygen uptake score, oxygenation index and mean
airway pressure (P<0.05). The above results suggest that
apoptosis is very common in neonatal RDS and the inhibition and low
expression levels of Bcl-2 may be the key in cases of worsening
disease (19,20).
In conclusion, the severity of neonatal RDS is
positively correlated with the caspase-3 expression level, but
negatively correlated with the Bcl-2 expression in alveolar lavage
fluid of child patients.
References
|
1
|
Frutos-Vivar F, Nin N and Esteban A:
Epidemiology of acute lung injury and acute respiratory distress
syndrome. Curr Opin Crit Care. 10:1–6. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Arakaki R, Yamada A, Kudo Y, Hayashi Y and
Ishimaru N: Mechanism of activation-induced cell death of T cells
and regulation of FasL expression. Crit Rev Immunol. 34:301–314.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tsang SM, Brown L, Lin K, Liu L, Piper K,
O'Toole EA, Grose R, Hart IR, Garrod DR, Fortune F, et al:
Non-junctional human desmoglein 3 acts as an upstream regulator of
Src in E-cadherin adhesion, a pathway possibly involved in the
pathogenesis of pemphigus vulgaris. J Pathol. 227:81–93. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu Q, Si T, Xu X, Liang F, Wang L and Pan
S: Electromagnetic radiation at 900 MHz induces sperm apoptosis
through bcl-2, bax and caspase-3 signaling pathways in rats. Reprod
Health. 12:652015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Crowther CA, Aghajafari F, Askie LM,
Asztalos EV, Brocklehurst P, Bubner TK, Doyle LW, Dutta S, Garite
TJ, Guinn DA, et al PRECISE Study Group, : Repeat prenatal
corticosteroid prior to preterm birth: a systematic review and
individual participant data meta-analysis for the PRECISE study
group (prenatal repeat corticosteroid international IPD study
group: Assessing the effects using the best level of evidence) -
study protocol. Syst Rev. 1:122012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sun H, Zhou Y, Xiong H, Kang W, Xu B, Liu
D, Zhang X, Li H, Zhou C, Zhang Y, et al: Prognosis of very preterm
infants with severe respiratory distress syndrome receiving
mechanical ventilation. Lung. 193:249–254. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Srivastava SK, Bhardwaj A, Arora S, Tyagi
N, Singh S, Andrews J, McClellan S, Wang B and Singh AP:
MicroRNA-345 induces apoptosis in pancreatic cancer cells through
potentiation of caspase-dependent and -independent pathways. Br J
Cancer. 113:660–668. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Takei Y, Okamoto S, Kawamura K, Jiang Y,
Morinaga T, Shingyoji M, Sekine I, Kubo S, Tada Y, Tatsumi K, et
al: Expression of p53 synergistically augments caspases-mediated
apoptosis induced by replication-competent adenoviruses in
pancreatic carcinoma cells. Cancer Gene Ther. 22:445–453. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pradeep AR: Expression of key executioner
of apoptosis caspase-3 in periodontal health and disease. J
Investig Clin Dent. 11:356–358. 2011.
|
|
10
|
Swamy M, Suhaili D, Sirajudeen KN,
Mustapha Z and Govindasamy C: Propolis ameliorates tumor nerosis
factor-α, nitric oxide levels, caspase-3 and nitric oxide synthase
activities in kainic acid mediated excitotoxicity in rat brain. Afr
J Tradit Complement Altern Med. 11:48–53. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tian F, Fu X, Gao J, Zhang C, Ning Q and
Luo X: Caspase-3 mediates apoptosis of striatal cells in GA I rat
model. J Huazhong Univ Sci Technolog Med Sci. 32:107–112. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Huang CS, Kawamura T, Peng X, Tochigi N,
Shigemura N, Billiar TR, Nakao A and Toyoda Y: Hydrogen inhalation
reduced epithelial apoptosis in ventilator-induced lung injury via
a mechanism involving nuclear factor-kappa B activation. Biochem
Biophys Res Commun. 408:253–258. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Merido D: Targeting BCL-2 to enhance
vulnerability to therapy in estrogen receptor-positive breast
cancer. Oncogene. 8:321–323. 2015.
|
|
14
|
Abdel Shakor AB, Atia M, Alshehri AS,
Sobota A and Kwiatkowska K: Ceramide generation during
curcumin-induced apoptosis is controlled by crosstalk among Bcl-2,
Bcl-xL, caspases and glutathione. Cell Signal. 27:2220–2230. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Adefolaju GA, Theron KE and Hosie MJ:
BAX/BCL-2 mRNA and protein expression in human breast MCF-7 cells
exposed to drug vehicles-methanol and dimethyl sulfoxide (DMSO) for
24 hours. Niger Med J. 56:169–174. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aliparasti MR, Alipour MR, Almasi S and
Feizi H: Ghrelin administration increases the Bax/Bcl-2 gene
expression ratio in the heart of chronic hypoxic rats. Adv Pharm
Bull. 5:195–199. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Dagistan Y, Cukur S, Dagistan E and Gezici
AR: Importance of IL-6, MMP-1, IGF-1 and BAX levels in lumbar
herniated discs and posterior longitudinal ligament in patients
with sciatic pain. World Neurosurg. 84:1739–1746. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wright C: S-Nitrosylation of Bcl-2
negatively affects autophagy in lung epithelial cells. J Cell
Biochem. 8:102–104. 2015.
|
|
19
|
Harazono Y, Kho DH, Balan V, Nakajima K,
Zhang T, Hogan V and Raz A: Galectin-3 leads to attenuation of
apoptosis through Bax heterodimerization in human thyroid carcinoma
cells. Oncotarget. 5:9992–10001. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Aboutaleb N, Shamsaei N, Khaksari M,
Erfani S, Rajabi H and Nikbakht F: Pre-ischemic exercise reduces
apoptosis in hippocampal CA3 cells after cerebral ischemia by
modulation of the Bax/Bcl-2 proteins ratio and prevention of
caspase-3 activation. J Physiol Sci. 65:435–443. 2015. View Article : Google Scholar : PubMed/NCBI
|