Introduction
The menisci are among the most commonly injured body
parts, with >1.7 million patients undergoing meniscal surgery
each year worldwide (1). In cases of
meniscal injury, the aim is to preserve the meniscus whenever
possible; however, many tears are either not repairable or the
repair ultimately fails (2). A
previous study reported a failure rate of 23.1% (3). In cases of untreatable or failed
meniscal surgery, meniscectomy is required; however, this method of
treatment is cautiously decided upon due to the certainty of
progressive pain, loss of function and development of
osteoarthritis (OA) caused by the altered biomechanical and
biochemical environment (2,4,5).
Although still relatively rare compared with other types of
orthopedic surgery, meniscal allograft transplant (MAT) is a
powerful tool for orthopedic surgeons that is gaining popularity
due to the known complications of meniscectomy (6).
Various MAT techniques have been developed since the
first MAT was performed in 1984, including arthroscopic-assisted
methods (5,7,8).
Controversies persist, however, regarding the optimal techniques
for what is still viewed by some as a ‘salvage procedure’ (5,9).
Furthermore, MAT has been associated with short-term failure (~4
years) at a rate of 10.6% and a high complication rate of 13.9%
(2). Consequently, additional
efforts to improve the MAT technique and technology are
warranted.
The purpose of the present study was to describe a
novel, all-arthroscopic MAT technique and demonstrate the effect of
associated instruments that were specifically designed for this
procedure. It is anticipated that an all-arthroscopic method may
assist in standardizing the procedure and ultimately shorten
surgical times by making a technically demanding procedure easier,
reduce intraoperative blood loss and improve short- and long-term
outcomes.
Materials and methods
Ethical statement
The present study was approved by the Ethics
Committee of the First Affiliated Hospital of PLA General Hospital
(Beijing, China). Informed, written consent was obtained from all
patients for the present study.
Instrumentation
Two sets of surgical implements were designed: One
to produce bone plugs of predefined sizes in the anterior and
posterior horns of the allograft meniscus (bone plug implements)
and a second to create bone tunnels in the receptor tibial plateau
to hold the bone plugs (bone tunnel implements).
The bone plug implements included a 1.8-mm guide pin
and hollow drill with a conical inner diameter varying 5–8.5 mm,
with the conical portion extending 15 mm in length. The drill had a
hollow inner diameter of 2 mm to permit passage of the 1.8-mm guide
pin. The bone tunnel implements included an eccentric bone drill
(with a 2.5-mm bone cutting head on the end), obturators and
attachment bolts.
Allograft preparation
Between March 2014 and March 2015, 24 patients (16
males and 8 females) with a mean age of 27.5 years (range, 17–48
years) participated in the present study. The inclusion criteria
were meniscal deficiency defined by the presence of <5 mm of
uninterrupted circumferential hoop fibers as determined by
preoperative MRI and confirmed by diagnostic arthroscopy. Exclusion
criteria were inflammatory joint disease, unresolved or recent
septic arthritis, metabolic or crystal disorders, body mass index
>35 kg/m2, and deficient soft tissue coverage or
tibiofemoral malalignment more than 2–3°. Residual synovial/soft
tissue and any bone connected to the anterior and posterior horns
of the allograft meniscus were removed. Disconnected bones on the
anterior and posterior horns of the allograft meniscus required two
precisely sized bone plugs with a diameter of 8.5 mm designed to
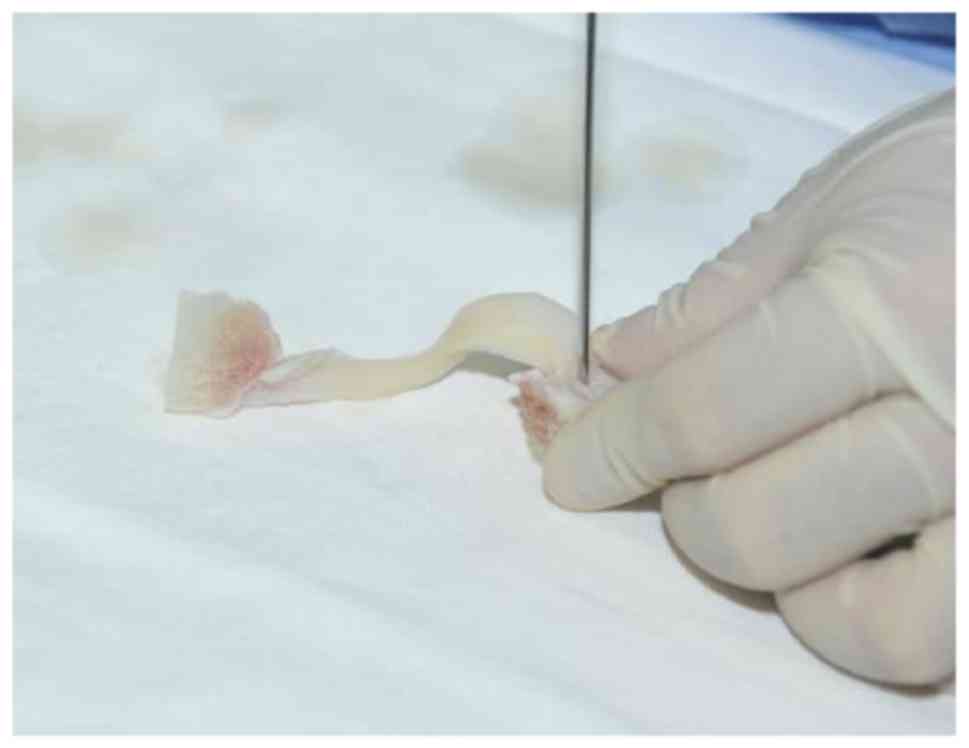
match corresponding bone tunnels in the tibial plateau. The 1.8-mm
guide pin was positioned in the center of the footprint of the
posterior horn of the meniscus, and the guide pin was maintained
either at an outward angle of 15° and a forward angle of 45°
(posterior horn), or backward angle of 30° (anterior horn) relative
to the plane of the tibial plateau (Fig.
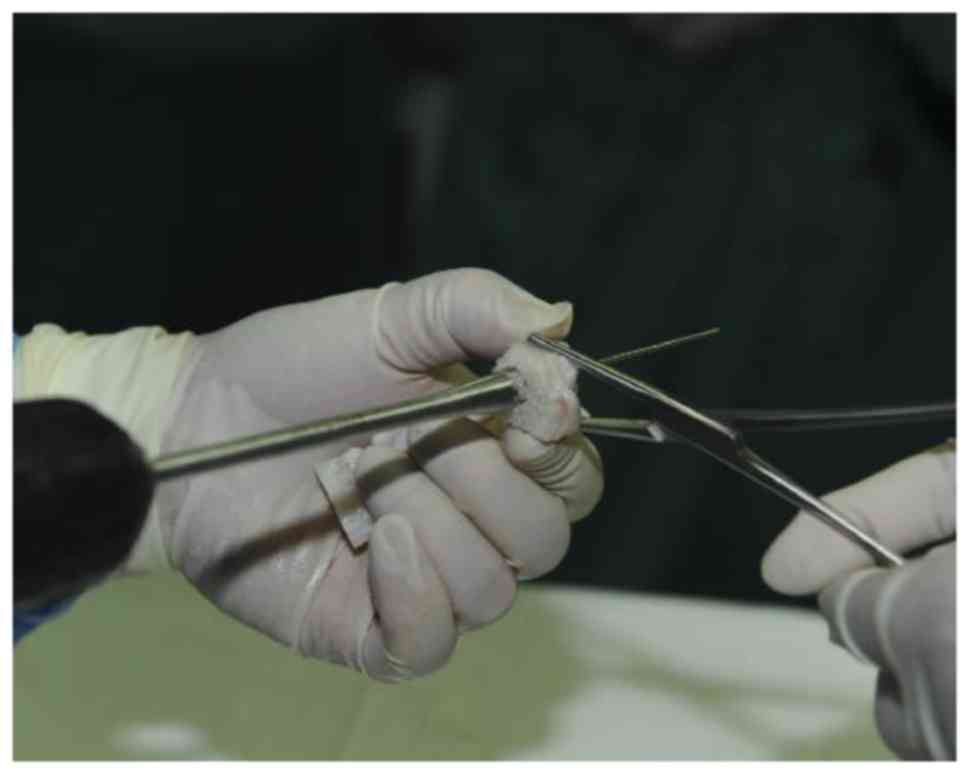
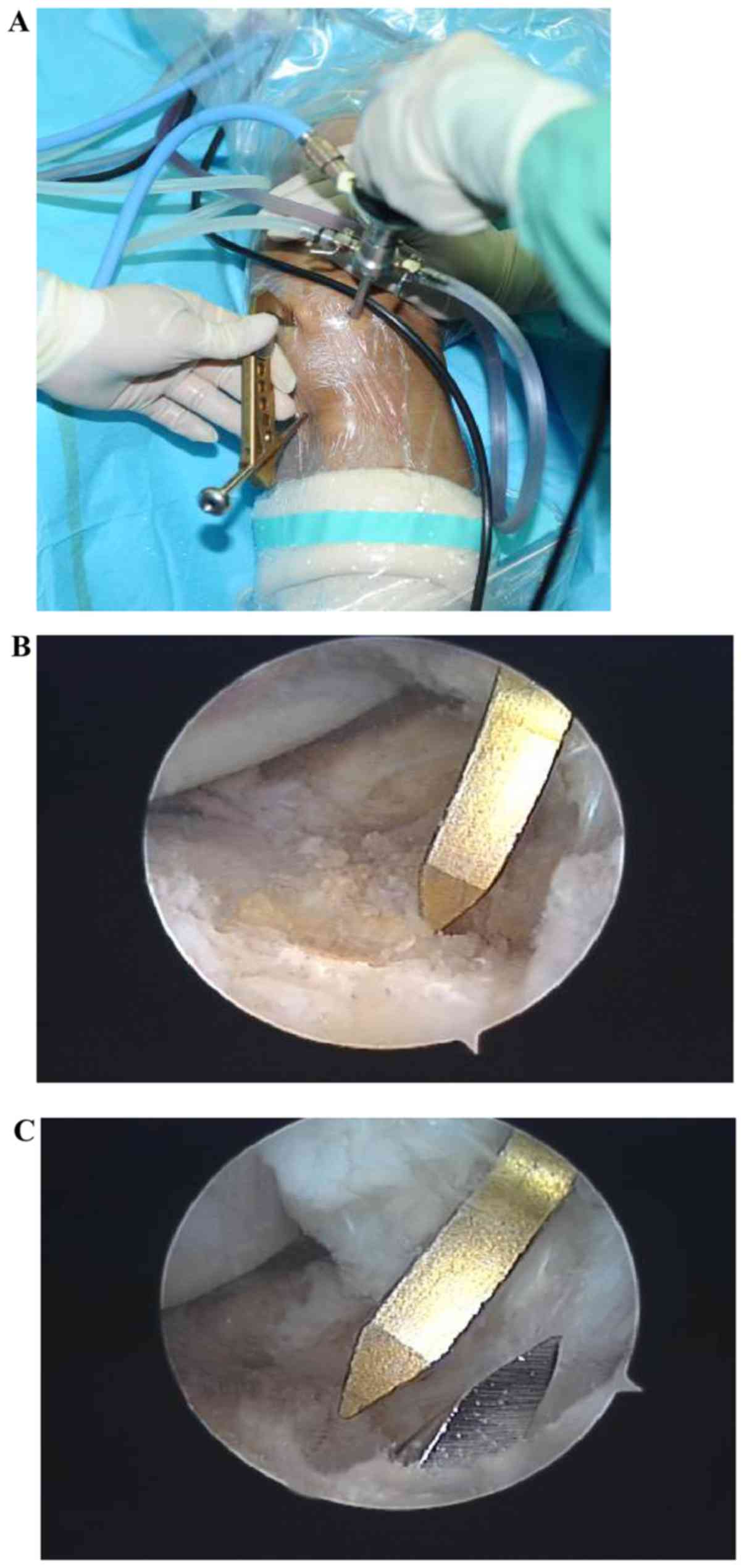
1). The conical hollow drill was used, following the guide pin
to drill from the side of the bone piece into the horn of the
meniscus until the hollow drill reached the posterior horn of the
meniscus, without damaging the horn of the meniscus (Fig. 2). Bone nibbling forceps were used to
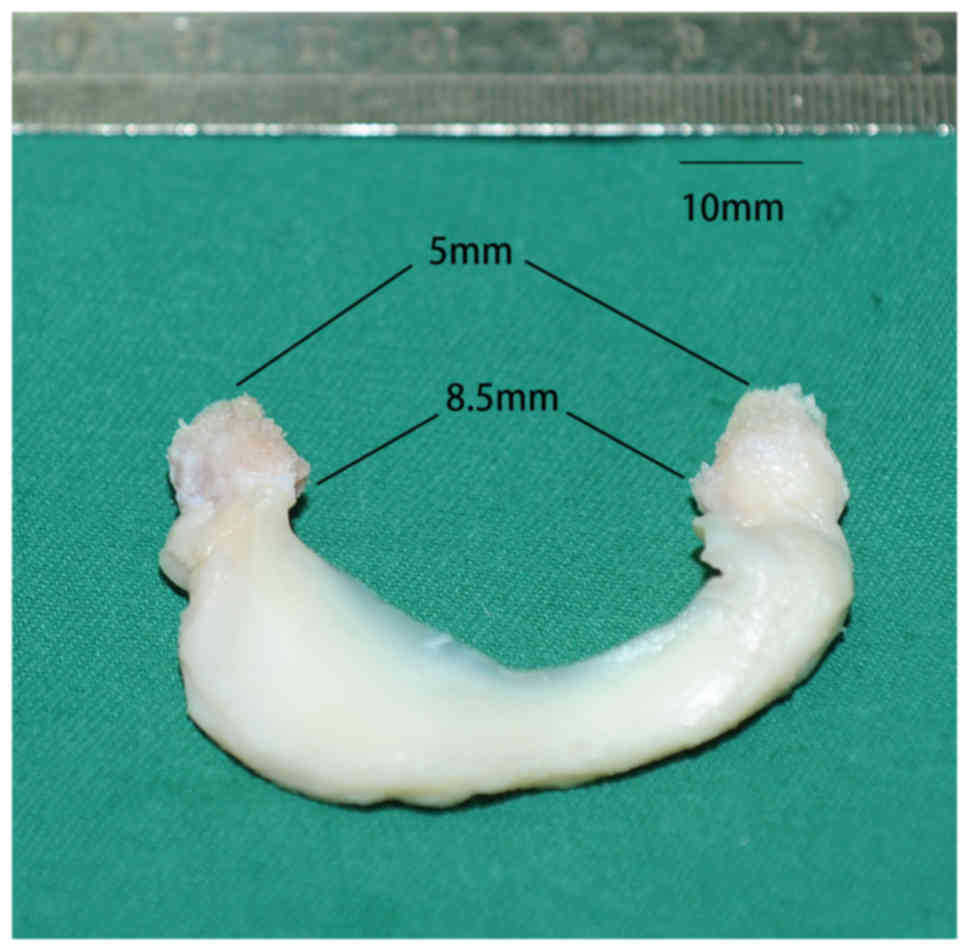
trim the residual bone from around the bone plug. The optimum bone
plug was 13 mm in length, which closely matched the length of the
bone groove in the tibial plateau (15 mm). Conical in shape, the
diameter of the bone plug closest to the meniscus was 8.5 mm and
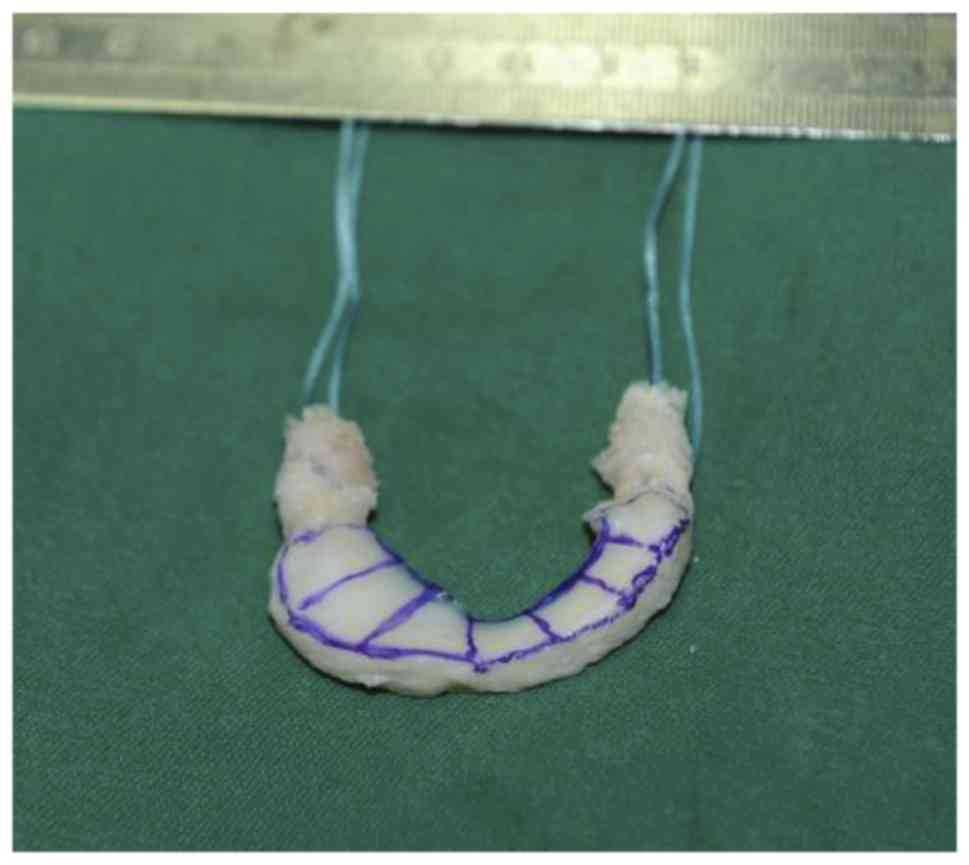
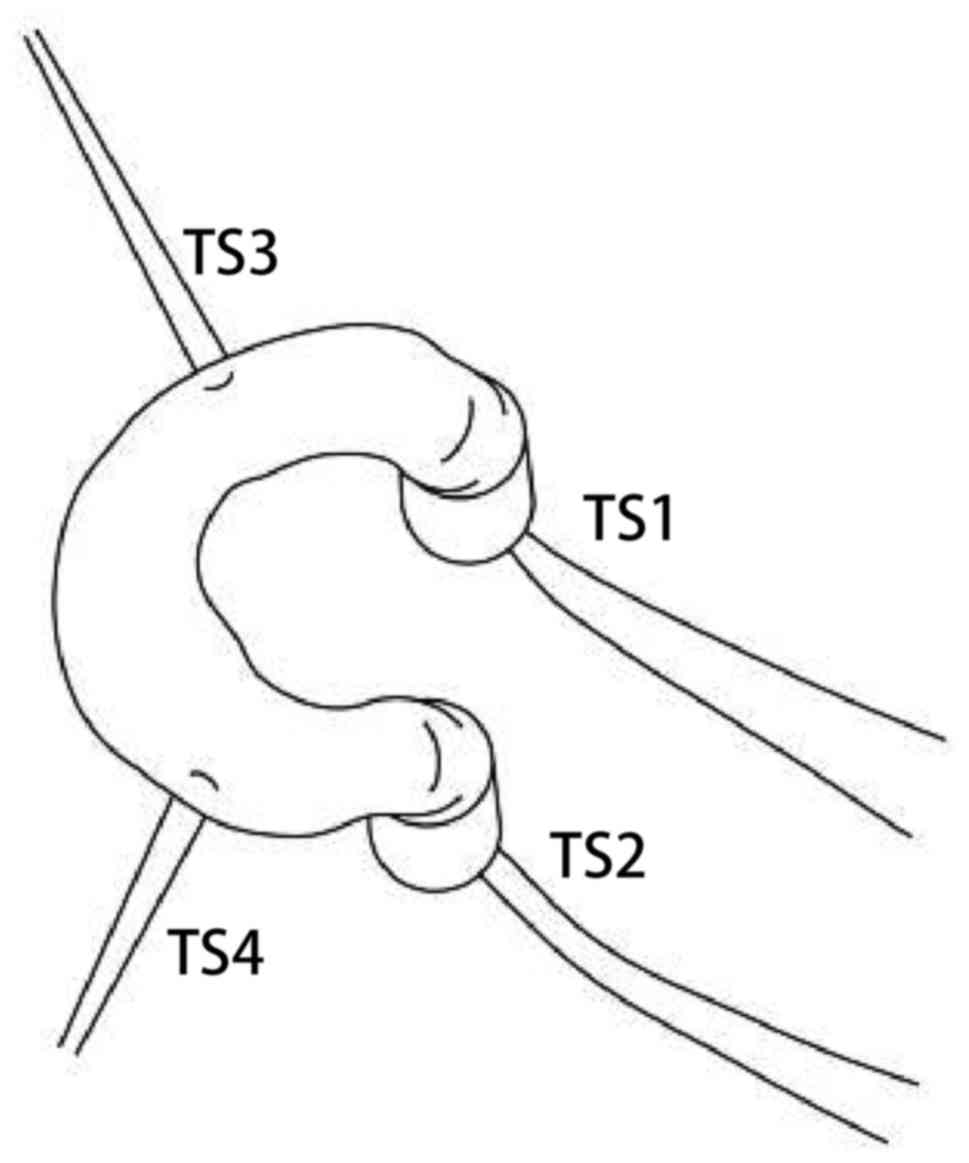
the free end of the bone plug was 5 mm in diameter (Fig. 3). Once the guide pin was removed to
produce the bone plug, a non-absorbable traction suture (TS1) was
used to suture the attachment area on the posterior horn of the
meniscus and the suture was passed through the hole made by the
guide pin. A 2–0 TiCron non-absorbable braided suture (Medtronic,
Fridley, MN, USA) or an Ethibond suture (Ethicon, LLC, Somerville,
NJ, USA) was used for TS3/TS4 and TS1/TS2, respectively. The
meniscal tissue near the meniscal allograft bone plug was also
securely sutured to fix the bone plug within the tibial tunnel
(Fig. 4). A traction suture (TS2)
was similarly passed through the bone plug, which was produced
using a similar method on the anterior horn of the meniscus. The
traction sutures aided the bone plug through the tunnel in the
tibial plateau and through the exit on the inner side of the tibial
tuberosity. Tension was maintained on TS1 and 2, which were tied
together to attach the anterior and posterior horns of the
meniscus. If the patient was young and energetic, screws were used
to suspend and attach the traction suture to the anterior and
posterior horns to increase stability.
A 2-0 nonabsorbable braided suture was used to
create two additional traction sutures at the junction of both the
anterior and posterior horns and the body of the meniscus (TS3 and
4). Once the meniscal allograft was implanted in the joint cavity,
the sutures were passed through the joint capsule to assist with
pulling the meniscal allograft into the joint cavity and preventing
the meniscus from springing back, ensuring the meniscus arrived at
the correct position (Fig. 5). The
sutures ultimately passed through the bone tunnels to the dorsal
surface of the tibia and exited on the inside of the tibial
tuberosity. TS3 and 4 had a certain amount of tension, as the
surgeon could feel resistance coming from the meniscus and were
tied to TS1 and 2.
Arthroscopic MAT
Once general anesthetic was induced in the patients
in dorsal recumbency, a tourniquet was applied to the affected
limb, and the knee was flexed at a 90° angle off the side of the
bed. Two incisions were made at the dorsomedial and dorsolateral
aspects of the knee. Depending on the side of the meniscal
transplant, either the medial or lateral incision was extended
slightly to 1–1.5 cm in length. An auxiliary incision to protect
the common peroneal nerve was created by the lateral meniscal
transplant. Additionally, an incision was made to loosen the
collateral ligament to expand the joint gap if it was too
narrow.
Routine arthroscopic examination of the joint was
performed and the pathology confirmed using standard techniques
(10–13). If the tibial intercondylar eminence
was prominent, 4–6 mm of the affected side of the tibial
intercondylar eminence and a small section (~4 mm) of the central
portion of the femoral condyle was removed prior to surgery to
clearly expose the posterior horn of the receptor meniscus and
facilitate surgical manipulation by performing intercondylar
notchplasty. Soft tissue debridement was performed until the center
of the posterior horn of the meniscus was clear, which in five
cases necessitated the severing of the proximal aspect of the
collateral ligament from the femoral condyle. Following surgery,
screws were used to reattach the ligament. The deeper layers of the
collateral ligament were not completely removed to avoid the
capsule from ‘ballooning out’ and complicating the suturing of the
meniscus.
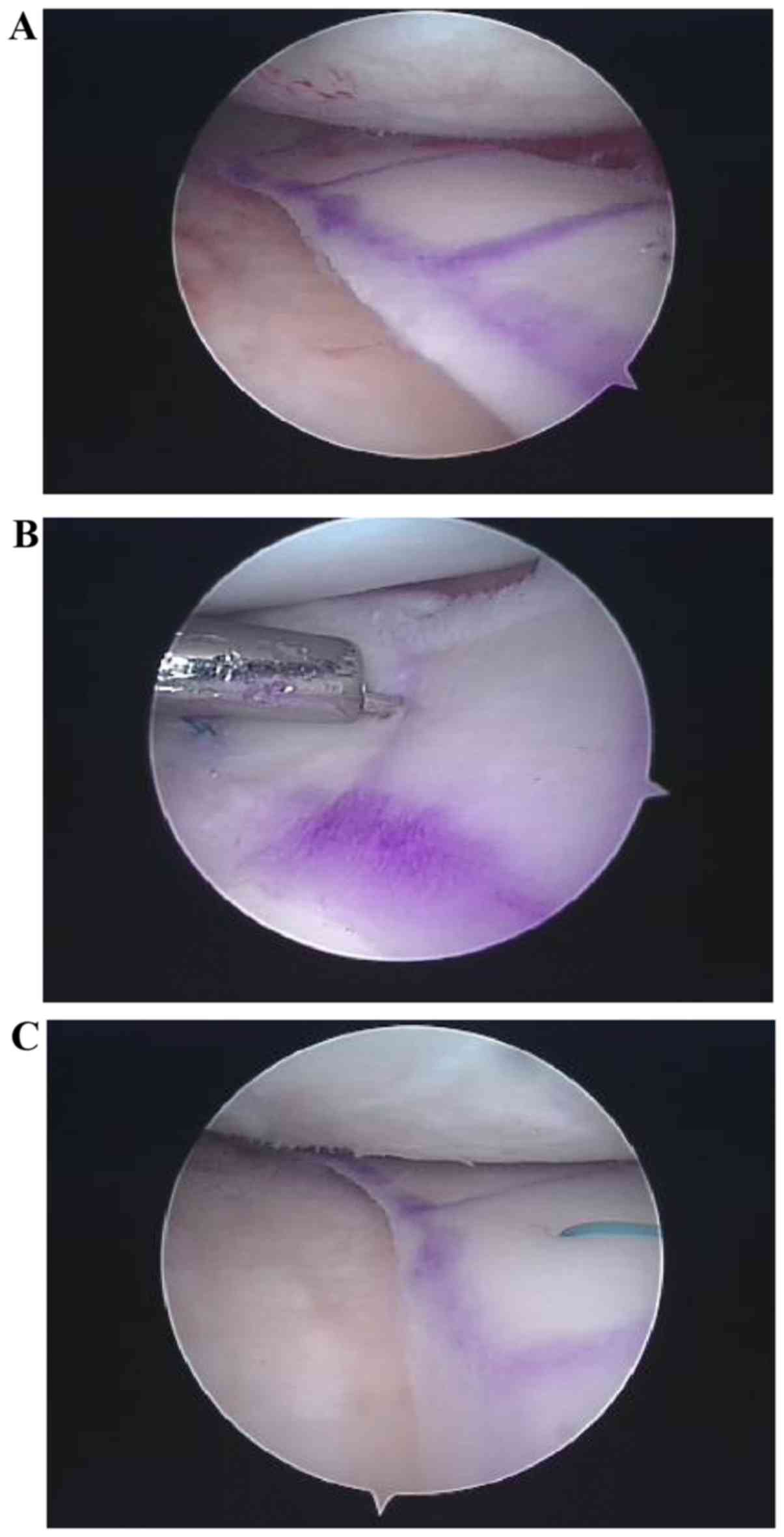
The residual receptor meniscus was filed and planed
until a rough, even margin was produced and bleeding occurred.
Retention of a 2 mm residual meniscus margin aided in confirming
that the anterior and posterior horns were transplanted to the
correct locations, and suturing the transplanted meniscus to the
margin of the stump aided in preventing outward herniation and
false crimping of the meniscus (Fig.
6) (14–16).
For junior surgeons, aluminum foil was used to
produce a template with dimensions similar to those of the
transplant. Placing this template on the tibial plateau within the
joint confirmed the location of the bone tunnel and determined
whether the transplant was appropriately situated on the tibial
plateau without any notable overhang.
Production of bone tunnels in the
tibial plateau
The anterior horn of the meniscus was attached to
the forward slope of the tibia and the location of the anterior
horn of the original meniscus indicated correct positioning. A
guide pin was used to drill into the center of the anterior horn. A
9-mm hollow drill followed the guide pin to create a bone tunnel
~15 mm deep. A triangular drill guide was placed in the bone tunnel
and a guide pin was used to drill into the bottom of the blind bone
tunnel from the cortical bone on the dorsomedial aspect of the
tibia. The bone tunnel was expanded by 3 mm and a guide wire was
passed through the cortical bone of the tibia and into the blind
bone tunnel. The wire was grasped for subsequent use where it
exited the knee joint.
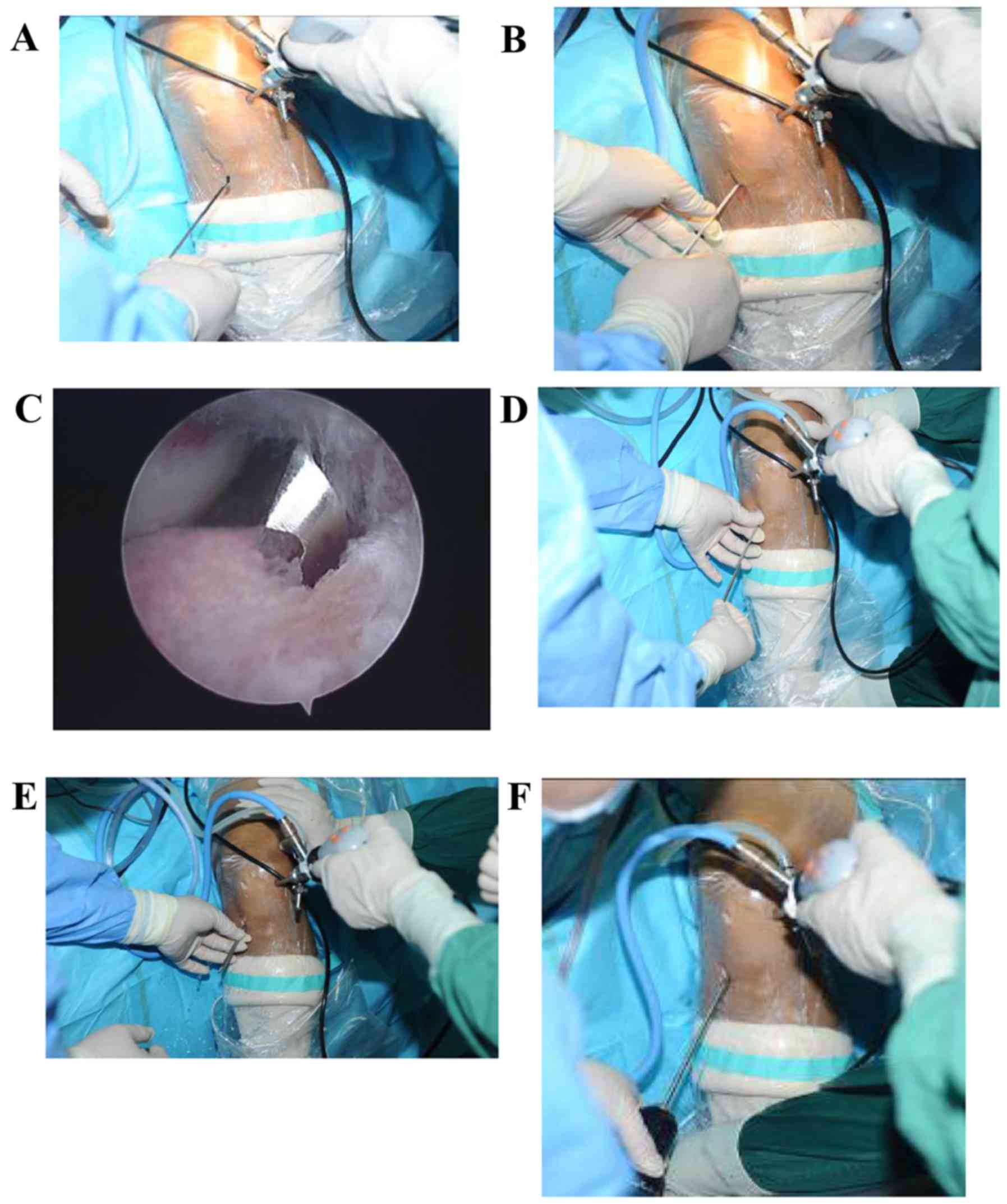
The bone tunnel for the posterior horn was created
by drilling a hole backwards from the tibial plateau. A 4-cm
incision in the skin lateral to the patella near the tibial
tuberosity was created and an anterior cruciate ligament (ACL)
guide was inserted into the joint cavity. The entrance to the
drilled hole was on the rear slope on the inside of the tibial
tuberosity and in the center of the inner aspect of the posterior
horn of the meniscus (Fig. 7A and
B). Using the guide, a guide pin was drilled into the center of
the footprint of the posterior horn of the receptor meniscus via
the inside of the tibial tuberosity for the medial meniscus
transplant or outside for the lateral meniscus transplant. A 4-mm
hollow drill was used to expand the bone tunnel (Fig. 7C). The eccentric bone drill was
inserted into the bone tunnel, and bone cutting head (2.5-mm in
size) was passed through the bone tunnel and into the joint cavity.
Subsequently, an obturator was inserted into the bone tunnel to
ensure that the bone cutting head at the end of the eccentric bone
drill was completely off-center relative to the bone tunnel and a
bolt was used to attach the eccentric bone drill and obturator,
which formed an eccentric bone drill head. The eccentric bone drill
head was turned using a power drill and removed while rotating in
reverse ~15 mm in the direction of the cortical bone at the front
of the tibia, which formed a cavity that allowed for the
accommodation of the bone plug (diameter, 9 mm; the diameter was
(4+2.5×2 mm); length, 15 mm) (Fig.
8A-F). Subsequently, the bolt was loosened, and the obturator
and eccentric bone drill were removed in sequence. A guide wire was
inserted into the bone tunnel and was pulled out from the anterior
incision where guide wire of the anterior horn of the meniscus had
been pulled out.
Inserting the meniscal allograft
TS1 and 2 were passed to the steel guide wire in the
anterior and posterior horns. The steel guide wire was removed so
that TS1 and 2 pulled the bone plugs of the anterior and posterior
horns into the joint cavity through the skin incision to the bone
tunnels in the tibial plateau to accommodate the anterior and
posterior horns. The bone plugs on the anterior and posterior horns
of the transplanted meniscus remained in the bone tunnels, and TS1
and 2 were pulled into the inner side of the tibial tuberosity on
the dorsal surface of the tibia. A suture grasper (Acufex; Smith
and Nephew plc, London, UK) pulled the suture at the junction of
the horns and the body of the meniscus (TS3 and 4) out through the
capsule and skin temporarily.
The knee joint was flexed at an angle of 20 and the
knee was turned to facilitate passage of the bone plug on the
posterior horn of the transplant. TS1 and 3 were pulled to guide
the meniscus into the joint cavity, causing the posterior horn to
enter the rear chamber of the joint cavity. In cases where it is
difficult to pull TS1 and 3 to guide the posterior horn of the
meniscus to enter the rear chamber of the joint cavity, a probe was
used to push aside the posterior cruciate ligament and a hook was
used to gently pull the posterior horn of the allograft meniscus to
allow the bone plug to pass through. The posterior horn of the
meniscus was prevented from entering the bone tunnel in the tibia
and only the bone plug on the posterior horn was allowed to enter
the bone tunnel to ensure the graft did not become too short. This
procedure was repeated with TS2 and 4 in order to maneuver the
entire graft into the joint, ensuring each horn entered the
appropriate bone tunnel. The meniscus was adjusted to its normal
location under arthroscopic observation.
To confirm the appropriate position and location of
the meniscus, the knee was straightened. Subsequently, the ends of
TS1 and 2 were tied together, pulling the anterior and posterior
horns of the meniscus outside of the cortical bone on the inside of
the tibial tuberosity. This method ensured that the horns could be
pulled tight and were able to enter the bone tunnels on the tibial
plateau. The locations of TS3 and 4 at the junction of the horns
and body of the meniscus were confirmed by locating the horn
junctions and the body of the residual former meniscus. Two bone
tunnels ~2 mm in diameter were drilled on the dorsal surface of the
tibia toward the two traction sutures at the edge of the joint
cartilage on the tibial plateau. A steel guide wire was inserted
and the traction sutures (TS3 and 4) were pulled through the bone
tunnels in the edge of the joint cartilage on the tibial plateau to
the outlet of the bone tunnel on the front surface of the tibia.
Tension was maintained on the traction sutures (TS3 and 4) and
these were tied to the traction sutures (TS1 and 2) holding the
anterior and posterior horns of the meniscal allograft at the front
surface of the tibia. This resulted in all four traction sutures
anchoring the four attachment points of the allograft. The present
approach allowed for TS3 and 4 to attach the synovial margin of the
meniscal allograft, re-established some of the function of the
coronary ligament between the meniscus and the edge of the tibial
plateau and reduced the risk of herniation of the meniscal
allograft.
Suturing the allograft
Standard meniscal suture repair methods were
employed to suture the margin of the meniscus to the capsule and
attach the meniscal allograft (5,16).
Vertical sutures are typically employed to attach the meniscus from
the rear 1/3 to the front in all cases and this was performed in
the present study. A 2–0 non-absorbable suture (Ethibond) was used
to attach the upper and lower surfaces of the meniscus with an
alternating pattern. The meniscus was sutured directly to the
meniscal bed (Fig. 9A and B) and it
was confirmed by observation that the meniscal allograft was
attached to the dissected portion of the tibia and the margin of
the residual meniscus, which created tension around the
circumference of the meniscus (Fig.
9C). A commonly used all-inside suturing method, including the
use of the FasT-Fix Suture System (Smith and Nephew plc), was used
to create two sutures on the posterior horn (with a low pulling
resistance) and the remaining 6–8 sutures employed an inside-out
vertical approach (17–20). Furthermore, a no. 18 spinal bone
marrow puncture needle was used to suture the anterior horn with an
outside-in pattern, using 0 braided nonabsorbable suture material,
or open sutures (21–23). When necessary, bone anchors were used
to attach the margin of the meniscus to the margin of the tibial
plateau, which ensured the meniscus was securely attached. Prior to
suturing the meniscus, incisions in the medio- or lateroplantar
aspect of the joint were created, which facilitated an
inside-to-outside pattern. Notably, when performing a lateral
meniscal transplant, a 3-cm long incision at the lateroplantar
aspect of the joint should be created to avoid injury to the common
peroneal nerve (located plantar to the inner collateral ligament
and the dorsal to the sartorius). In the present study, the
pesanserinus tendon was pulled in a plantar direction, blunt
dissection of the semimembranosus tendon and the knee capsule was
performed, and blunt separation of the gastrocnemius tendon and
capsule was established, avoiding the infrapatellar branch of the
saphenous nerve. Small curved forceps were used to separate the
subcutaneous tissue and deeper tissue until the capsule was
reached. When suturing the rear of the meniscus, the suture needle
was pulled through the 3 cm incision. A meniscal spoon retractor
was applied to prevent the inside-to-outside sutures from injuring
nerves or blood vessels and the suture cord was tied directly above
the capsule. Two or three small incisions were required to extract
all of the meniscal sutures. Subsequently, the joint was examined
while gently flexing and rotating prior to routine closure of the
incisions and bandaging the limb.
Results and discussion
A recent systematic review reported that the MAT
procedure has matured from an open approach with femoral condyle
osteotomy or distraction devices to the widely used
arthroscopically-assisted procedure with miniarthrotomy (4). Given the benefits of minimally invasive
surgery and desire to further develop MAT, the purpose of the
present study was to describe a novel all-arthroscopic technique
for performing meniscal MAT, either lateral or medial. In the
present study, the 1.8-mm guide pin was positioned in the center of
the footprint of the posterior horn of the meniscus and the
eccentric bone drill was inserted into the bone tunnel. The
eccentric bone drill head was turned using a power drill and
removed while rotating in reverse ~15 mm in the direction of the
cortical bone at the front of the tibia, which formed a cavity that
allowed for the accommodation of the bone plug (diameter, 9 mm; the
diameter was (4+2.5×2 mm); length, 15 mm). To the best of our
knowledge, this is the first study to use this method. Although
technically demanding, there are some benefits of minimally
invasive orthopedic procedures, as they have a finer bone tibial
tunnel compared with other methods (24). MAT is a procedure that has gained
interest since its inception in the early 1980s (25). However, despite being performed for
over three decades, controversy persists regarding several of the
finer aspects of MAT, including the following: Indications for
surgery and patient selection, including age, symptoms and timing
of surgery; graft preservation technique; fixation technique (bony
fixation vs. an all-suture technique); postsurgical rehabilitation
procedures; appropriate outcome measures, including Lysholm score,
International Knee Documentation Committee (IKDC) subjective knee
form, Tegner activity level score, Fulkerson questionnaire, WOMAC
index, and the Kellgren and Lawrence OA grade; the impact of
concomitant surgical procedures; impact on OA; and what is
considered a successful surgery. These controversies continue to be
salient in this field considering the growing number of MAT
procedures performed annually together with the lack of controlled
clinical studies and long-term follow-up data (2,4,6).
The all-arthroscopic MAT technique described in the
present study demonstrated a primary step to pioneer a standardized
procedure using specifically designed instruments for creating bone
plugs and tunnels. The present approach, rather than the bone
bridge approach, was selected as the literature has revealed that
the bone insertion technique offers a biodynamic advantage
(26–30). Previous studies have also indicated
that the reliable attachment of the anterior and posterior horns of
the meniscus to precisely dissected locations on the receptor is a
key surgical determinant of postoperative meniscal function
(28,31,32). If
the anterior and posterior horns are not securely attached, poor
meniscal function may cause widespread deterioration of the
cartilage in load-bearing areas of the joint (27,33).
Overall, it is currently accepted that bone attachment of the
anterior and posterior horns of the meniscus is the gold standard
for MAT (34,35).
The bone plug attachment technique, either the
arthroscopic-assisted or all-arthroscopic approach, attaches one
bone plug to the anterior and posterior horns, respectively.
Several advantages are associated with this method, including
little trauma to the tibial plateau, little requirement to remove
bone, the preservation of the tibial intercondylar eminence and
adjustment of the meniscus location depending on allograft size and
maintenance of optimal meniscal allograft tension (8,36).
However, the technique is difficult and time consuming and the
distances and locations of the anterior and posterior horns may be
inaccurate (37). Meniscus
transplant abnormalities may occur due to error in the location of
tibial tunnels (38). For example, a
large bone tunnel diameter may increase the risk of injury to the
receptor tibial plateau and increase the risk of tibial plateau
fracture. This is particularly prominent for patients requiring
concomitant surgical procedures to the ACL (39).
Presently, one of the largest concerns with MAT is
the lack of standard surgical implements, which has forced surgeons
to depend on their hands and eyes alone to produce the bone plugs
and bone tunnels. As a result, bone plugs and tunnels are
frequently inconsistent in size and/or shape, requiring repeated
corrections that prolong surgery time and reduce surgical accuracy,
potentially achieving suboptimal attachment of the anterior and
posterior horns of the meniscus.
The development of the surgical implements described
in the present study was anticipated to facilitate bone plug
creation, implantation and attachment, minimize trauma to the
tibial plateau caused by the bone plug attachment technique and
reduce the risk of postsurgical complications, including tibial
fracture. In addition, such instrumentation may promote surgical
standardization, minimize trauma, simplify bone tunnel production,
enhance bone plug attachment quality, shorten surgical times and
decrease intraoperative bleeding among other potential benefits
(37,40).
The success of the bone plug attachment technique
depends on correct dissection and maintenance of annular tension.
Previous studies have indicated that crimping due to protrusion of
the margin of the meniscus, or even subluxation, may occur
following meniscal transplantation (15). The meniscus is typically attached to
the tibial plateau via the tibia ligaments, not by the capsule.
Consequently, it is crucial for the meniscus to be attached to the
dissected portion of the tibia and to the margin of the residual
meniscus. In the procedure described in the present study, a steel
guide wire was used to pull the traction sutures to the junction
between the posterior horn and the body of the meniscus, and the
junction between the anterior horn and the body of the meniscus to
the inside of the tibial tuberosity, while maintaining appropriate
tension when tying the sutures outside the cortical bone (inside
the tibial tuberosity). The sutures attached to the anterior and
posterior horns formed four attachment points, simplifying meniscal
implantation and preventing the meniscus from protruding.
Furthermore, it is hypothesized that the attachment of a meniscal
allograft to the synovial margin may allow a certain degree of
reconstruction of the function of the coronary ligament joining the
meniscus and margin of the tibial plateau because the sutures (TS3
and 4) were applied to fix the meniscus to the margin of the tibial
plateau, which may stabilize the margin of the meniscal allograft,
increase the stability of the meniscus and largely avoid risk of
meniscal herniation and/or dislocation (24). This approach is also supported by
Stone and Walgenbach (24), who
noted that out of three attachment methods, a four-point attachment
method that involved the anterior and posterior horns and the
junctions employed between the posterior horn and the body meniscus
achieved the greatest meniscal stability, which prevented bulging
and improved the accuracy of meniscal positioning. Thus, the
surgery was successfully performed without any complications of
meniscal herniation and/or dislocation in all cases.
The present study comprehensively described a novel
bone all-arthroscopic technique and instrumentation for MAT. The
present findings provided preliminary results for future clinical
studies, which are required to identify the outcomes associated
with the present technique. Those outcomes may then be compared
with other studies to assist in improving MAT. Furthermore,
although the present indicates the use of the surgical implements
in an inner meniscal transplantation, the described technique may
also be adapted for use in outer meniscal transplantations
(8,37).
References
|
1
|
Samitier G, Alentorn-Geli E, Taylor DC,
Rill B, Lock T, Moutzouros V and Kolowich P: Meniscal allograft
transplantation. Part. 1:Systematic review of graft biology, graft
shrinkage, graft extrusion, graft sizing, and graft fixation. Knee
Surg Sports Traumatol Arthrosc 23: 310–322. 2015.
|
|
2
|
Smith NA, MacKay N, Costa M and Spalding
T: Meniscal allograft transplantation in a symptomatic meniscal
deficient knee: A systematic review. Knee Surg Sports Traumatol
Arthrosc. 23:270–279. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nepple JJ, Dunn WR and Wright RW: Meniscal
repair outcomes at greater than five years: A systematic literature
review and meta-analysis. J Bone Joint Surg Am. 94:2222–2227. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Myers P and Tudor F: Meniscal allograft
transplantation: How should we be doing it? A systematic review.
Arthroscopy. 31:911–925. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Smith NA, Costa ML and Spalding T:
Meniscal allograft transplantation: Rationale for treatment. Bone
Joint J. 97-B:1–594. 2015. View Article : Google Scholar
|
|
6
|
Samitier G, Alentorn-Geli E, Taylor DC,
Rill B, Lock T, Moutzouros V and Kolowich P: Meniscal allograft
transplantation. Part. 2:Systematic review of transplant timing,
outcomes, return to competition, associated procedures, and
prevention of osteoarthritis. Knee Surg Sports Traumatol Arthrosc
23: 323–333. 2015.
|
|
7
|
Jang KM and Wang JH: Lateral meniscus
allograft transplantation using a single-incision technique. Knee
Surg Sports Traumatol Arthrosc. 23:258–263. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lubowitz JH, Verdonk PC, Reid JB and
Verdonk R: Meniscus allograft transplantation: A current concepts
review. Knee Surg Sports Traumatol Arthrosc. 15:476–492. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lubowitz JH: Editorial commentary:
Meniscal allograft yields acceptable outcomes (for a salvage
procedure). Arthroscopy. 31:9262015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Javidan P, Ahmed M and Kaar S:
Arthroscopic release of the deep medial collateral ligament to
assist in exposure of the medial tibiofemoral compartment. Arthrosc
Tech. 3:e699–e701. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Harato K, Niki Y, Nagashima M, Masumoto K,
Otani T, Toyama Y and Suda Y: Arthroscopic visualization of
abnormal movement of discoid lateral meniscus with snapping
phenomenon. Arthrosc Tech. 4:e235–e238. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gauffiny H, Tagesson S, Meunier A,
Magnusson H and Kvist J: Knee arthroscopic surgery is beneficial to
middle-aged patients with meniscal symptoms: A prospective,
randomised, single-blinded study. Osteoarthritis Cartilage.
22:1808–1816. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sihvonen R, Englund M, Turkiewicz A and
Järvinen TL: Mechanical symptoms as an indication for knee
arthroscopy in patients with degenerative meniscus tear: A
prospective cohort study. Osteoarthritis Cartilage. 24:1367–1375.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Iñigo-Pavlovich R: Radiofrequency and
meniscus. From excision to repair. Sports Med Arthrosc Rev.
13:193–197. 2005. View Article : Google Scholar
|
|
15
|
Khetia EA and McKeon BP: Meniscal
allografts: Biomechanics and techniques. Sports Med Arthrosc.
15:114–120. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yoldas EA, Sekiya JK, Irrgang JJ, Fu FH
and Harner CD: Arthroscopically assisted meniscal allograft
transplantation with and without combined anterior cruciate
ligament reconstruction. Knee Surg Sports Traumatol Arthrosc.
11:173–182. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Grant JA, Wilde J, Miller BS and Bedi A:
Comparison of inside-out and all-inside techniques for the repair
of isolated meniscal tears: A systematic review. Am J Sports Med.
40:459–468. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Turman KA, Diduch DR and Miller MD:
All-inside meniscal repair. Sports Health. 1:438–444. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nelson CG and Bonner KF: Inside-out
meniscus repair. Arthrosc Tech. 2:e453–e460. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Choi NH, Kim TH and Victoroff BN:
Comparison of arthroscopic medial meniscal suture repair
techniques: Inside-out versus all-inside repair. Am J Sports Med.
37:2144–2150. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rodeo SA: Arthroscopic meniscal repair
with use of the outside-in technique. Instr Course Lect.
49:195–206. 2000.PubMed/NCBI
|
|
22
|
Kelly JD IV and Ebrahimpour P: Chondral
injury and synovitis after arthroscopic meniscal repair using an
outside-in mulberry knot suture technique. Arthroscopy. 20:e49–e52.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Abdelkafy A, Aigner N, Zada M, Elghoul Y,
Abdelsadek H and Landsiedl F: Two to nineteen years follow-up of
arthroscopic meniscal repair using the outside-in technique: A
retrospective study. Arch Orthop Trauma Surg. 127:245–252. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Stone KR and Walgenbach AW: Meniscal
allografting: The three-tunnel technique. Arthroscopy. 19:426–430.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Milachowski KA, Weismeier K and Wirth CJ:
Homologous meniscus transplantation. Experimental and clinical
results. Int Orthop. 13:1–11. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Abat F, Gelber PE, Erquicia JI, Pelfort X,
Gonzalez-Lucena G and Monllau JC: Suture-only fixation technique
leads to a higher degree of extrusion than bony fixation in
meniscal allograft transplantation. Am J Sports Med. 40:1591–1596.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Alhalki MM, Howell SM and Hull ML: How
three methods for fixing a medial meniscal autograft affect tibial
contact mechanics. Am J Sports Med. 27:320–328. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen MI, Branch TP and Hutton WC: Is it
important to secure the horns during lateral meniscal
transplantation? A cadaveric study. Arthroscopy. 12:174–181. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Paletta GA Jr, Manning T, Snell E, Parker
R and Bergfeld J: The effect of allograft meniscal replacement on
intraarticular contact area and pressures in the human knee. A
biomechanical study. Am J Sports Med. 25:692–698. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang H, Gee AO, Hutchinson ID, Stoner K,
Warren RF, Chen TO and Maher SA: Bone plug versus suture-only
fixation of meniscal grafts: Effect on joint contact mechanics
during simulated gait. Am J Sports Med. 42:1682–1689. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bryan TK, Robert HB and Scott AR: Meniscal
allograft transplantation: Surgical technique. Techniques in Knee
Surgery. 3:8–18. 2004. View Article : Google Scholar
|
|
32
|
Paletta GA Jr, Manning T, Snell E, Parker
R and Bergfeld J: The effect of allograft meniscal replacement on
intraarticular contact area and pressures in the human knee. A
biomechanical study. Am J Sports Med. 25:692–698. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lazovic D, Wirth CJ, Knösel T, Gossé F and
Maschek HG: Meniscus replacement using incongruent transplants-an
experimental study. Z Orthop Ihre Grenzgeb. 135:131–137. 1997.(In
German). PubMed/NCBI
|
|
34
|
Shelton WR and Dukes AD: Meniscus
replacement with bone anchors: A surgical technique. Arthroscopy.
10:324–327. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Vaquero J and Forriol F: Meniscus tear
surgery and meniscus replacement. Muscles Ligaments Tendons J.
6:71–89. 2016.PubMed/NCBI
|
|
36
|
Farr J and Gersoff W: Current meniscal
allograft transplantation. Sports Med Arthrosc Rev. 12:69–82. 2004.
View Article : Google Scholar
|
|
37
|
Farr J, Rawal A and Marberry KM:
Concomitant meniscal allograft transplantation and autologous
chondrocyte implantation: Minimum 2-year follow-up. Am J Sports
Med. 35:1459–1466. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sekaran SV, Hull ML and Howell SM:
Nonanatomic location of the posterior horn of a medial meniscal
autograft implanted in a cadaveric knee adversely affects the
pressure distribution on the tibial plateau. Am J Sports Med.
30:74–82. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhang YD, Hou SX, Zhang YC, Luo DZ, Zhong
HB and Zhang H: Arthroscopic combined medial and lateral meniscus
transplantation after double-tunnel, double-bundle anterior
cruciate ligament reconstruction in the same knee. Knee.
19:953–958. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Faivre B, Boisrenoult P, Lonjon G, Pujol N
and Beaufils P: Lateral meniscus allograft transplantation:
Clinical and anatomic outcomes after arthroscopic implantation with
tibial tunnels versus open implantation without tunnels. Orthop
Traumatol Surg Res. 100:297–302. 2014. View Article : Google Scholar : PubMed/NCBI
|