Introduction
Gastric cancer is one of the most common malignant
tumors of the digestive system, and the incidence of this disease
ranks second among all types of cancer worldwide. Approximately
600,000 new cases are affected by gastric cancer every year
worldwide, and 66% of these patients lose their lives due to this
disease. The incidence of gastric cancer is two-fold higher in men
than in women (1). Epidemiological
studies have confirmed that gastric cancer occurs mainly in
developing countries, such as China. Gastric cancer is a serious
threat to human health. Therefore, in-depth studies on the
mechanism of the occurrence and development of gastric cancer, as
well as early detection and prevention, are extremely important for
the treatment of patients with this disease (2). Related studies have shown that etiology
of gastric cancer may be associated with environmental and dietary
factors, and is also closely associated with Helicobacter
pylori infection (3).
With the increased incidence of gastric cancer,
effects of the disease-associated metabolic syndrome (MS) on the
prognosis of patients with gastric cancer have been increasing. MS
is a kind of syndrome with the main manifestations of central
obesity, insulin resistance (IR), hypertension, high levels of
triglycerides (TGs) and LDL-C, impaired glucose tolerance (IGT) and
type 2 diabetes mellitus (T2DM) (4).
Bloomgarden et al (5) showed
that 70–80 million individuals in the United States are suffering
from MS, accounting for 1/3 of the total population of that
country. In China, the incidence of MS is 12.25% in the southern
area (6) and 11.6% in the northern
area (7,8), which were both lower than that in the
United States, possibly due to the healthy Chinese diet and low
incidence of obesity. With the changes in lifestyle, the incidence
of gastric cancer has shown an increasing tendency, and gastric
cancer is one of the major current health issues.
Radical gastrectomy is currently recognized as the
only way to cure gastric cancer. However, clinical application of
radical gastrectomy is still challenged by the two classes of
complications. The first class includes surgery-related
complications, including postoperative bleeding, incision
infection, incision split, lymphatic leakage, pancreatic fistula,
anastomotic fistula, duodenal stump fistula, abdominal abscess,
gastroparesis and intestinal obstruction. The other class includes
postoperative complications, such as pneumonia, pleural effusion,
cardiovascular accidents, pulmonary infarction and urinary tract
infections, among which anastomotic fistula, pancreatic fistula,
abdominal abscess and pneumonia are often referred to as the four
major complications associated with radical gastrectomy (9).
The purpose of this study was to investigate the
effects of blood glucose, blood lipid and blood pressure control on
the occurrence of complications and postoperative recovery after
radical gastrectomy in patients with gastric cancer complicated
with MS.
Materials and methods
General information
A total of 150 patients with gastric cancer who were
treated at the Daqing Longnan Hospital (Daqing, China) from
November, 2015 to May, 2017 were enrolled in this study. Patients
were divided into the MS and non-MS groups according to the
presence of MS. The non-MS group included 70 patients, of whom 33
were females and 37 were males, and the mean age was 61.3±12.1
years. The MS group included 80 patients, of whom 39 were females
and 41 were males, and the mean age was 62.4±10.4 years (Table I). There was no significant
difference between the two groups regarding parameters such as age,
sex, course of disease, BMI and other factors (Table I, p>0.05). Patients in the MS
group were divided into the normal and abnormal groups according to
the levels of blood glucose, blood lipids and blood pressure. All
normal groups were referred to as group A, and abnormal groups were
referred to as group B. Different types of radical gastrectomy were
performed for different patients according to their conditions.
Inclusion criteria were: All enrolled patients were diagnosed with
gastric cancer by gastroscopy and biopsy before surgery, and MS was
diagnosed according to the diagnostic criteria of MS proposed by
the Chinese Medical Association Diabetes Branch (10).
 | Table I.General information of the MS and
non-MS groups. |
Table I.
General information of the MS and
non-MS groups.
| Groups | Cases | Age (years) | Sex ratio
(male/female) | Course of disease
(months) | BMI
(kg/m2) |
|---|
| MS group | 80 | 62.4±10.4 | 1.12 | 11.9±2.4 | 24.2±4.3 |
| Non-MS group | 70 | 61.3±12.1 | 1.05 | 11.4±2.1 | 24.7±5.1 |
| P-value |
| 0.521 | 0.143 | 0.243 | 0.211 |
Patients who met three or all of the criteria of the
following four items were diagnosed as MS: i) Overweight and (or)
obesity BMI≥25.0; ⅱ) hyperglycemia: FDG≥6.1 mmol/l and (or) 2
hPG≥7.8 mmol/l and (or) patients diagnosed with diabetes and
received treatment; ⅲ) hypertension: SBP/DBP≥140 and (or) has been
diagnosed with hypertension and received treatment; and ⅳ)
dyslipidemia: Fasting blood TG≥1.7 mmol/l. Exclusion criteria were:
Severe cardiovascular and cerebrovascular diseases, renal failure,
digestive system inflammation and mental disorders. This study was
approved by the Ethics Committee of Daqing Longnan Hospital and all
patients signed informed consent.
Research methods
Patients in the MS group were given corresponding
drugs to control blood pressure, blood lipids and blood glucose,
while patients in non-MS group were not treated with those drugs.
Blood glucose, blood lipids, blood pressure, BMI, postoperative
complications and recovery conditions of the two groups were
recorded at 1 day before operation, and 1 and 3 months after
operation.
Control standards
Patients in the MS group were treated with
medication to control blood sugar, blood lipids and blood pressure
after surgery. Specific requirements were as follows:
Postoperative blood glucose was controlled according
to the recommended standards of the American Diabetes Association
(2009) (11): i) FBG≤7.0 mmol/l, 2
hPG≤10 mmol/l, HbAlc ≤6.5%; and ⅱ) FBG or 2hPG decrease >1.39
mmol/l or HbAlc decrease >1%.
Postoperative blood glucose control: Outcomes met at
least one of the three criteria referred to as effective blood
glucose control: i) TGs, total cholesterol and LDL decreased by
>30%; ⅱ) high-density lipoprotein (HDL) increased by >30%;
and ⅲ) blood lipids reached below-normal levels.
Postoperative blood pressure control: Outcomes met
at least one of the three criteria referred to as effective blood
pressure control: SBP or DBP dropped by >10 mmHg (1 mmHg=0.133
kPa) or reached below normal (140/90 mmHg) levels.
Statistical analysis
SPSS 17.0 statistical software (SPSS Inc., Chicago,
IL, USA) was used for statistical analysis. Measurement data were
expressed as mean ± SD, and paired t-test was used for comparisons
within the two groups. In addition, count data were expressed as
percentage and comparisons were performed by the χ2
test. Finally, logistic regression analysis was performed to
analyze the correlations between postoperative complications and
blood glucose, blood lipids and blood pressure. P<0.05 was
considered to be statistically significant.
Results
Comparison of blood glucose, blood
lipids and blood pressure between the MS and non-MS groups before
and at 1 month after surgery
Blood glucose, blood lipids and blood pressure
levels were significantly higher in the MS group than in the non-MS
group before and at 1 month after surgery (p<0.05). Compared to
pre-treatment levels, blood glucose, blood lipids and blood
pressure in the MS group dropped significantly at 1 month after
surgery (p<0.05) (Table II).
 | Table II.Comparison of blood glucose, blood
lipids and blood pressure between the MS and non-MS groups before
and at 1 month after surgery mean ± SD. |
Table II.
Comparison of blood glucose, blood
lipids and blood pressure between the MS and non-MS groups before
and at 1 month after surgery mean ± SD.
|
| MS group | Non-MS group |
|---|
|
|
|
|
|---|
| Items | Before treatment | 1 month after
treatment | Before treatment | 1 month after
treatment |
|---|
| Blood glucose
(mmol/l) | 11.32±3.21 | 8.1±3.5a | 7.2±2.5b | 7.8±3.1 |
| SBP | 151.3±9.7 |
132.5±8.9a |
128.9±10.4b | 130.4±9.4 |
| DBP | 98.5±8.7 |
89.32±9.5a | 85.5±8.6b | 89.43±7.4 |
| BMI
(kg/m2) | 24.2±4.3 |
20.16±1.22a | 24.7±5.1 | 23.15±1.06 |
| Total TGs
(mmol/l) | 2.85±1.05 |
1.92±0.65a |
1.70±1.25b | 1.81±0.55 |
| Total cholesterol
(mmol/l) | 5.51±1.65 |
3.82±1.42a |
3.01±1.45b | 3.32±1.23 |
Effects of blood glucose, blood lipids
and blood pressure control on the occurrence of postoperative
complications at 3 months after surgery
Incidence of postoperative complications in patients
with normal blood glucose, blood lipids and blood pressure in the
MS group was significantly lower than that in patients with
abnormal blood glucose, blood lipids and blood pressure (Table III).
 | Table III.Effects of blood glucose, blood lipids
and blood pressure control on the occurrence of postoperative
complications at 3 months after surgery (n, %). |
Table III.
Effects of blood glucose, blood lipids
and blood pressure control on the occurrence of postoperative
complications at 3 months after surgery (n, %).
|
| Blood pressure | Blood glucose | Blood lipids |
|---|
|
|
|
|
|
|---|
| Variables | Normal (n=51) | Abnormal (n=29) | Normal (n=48) | Abnormal (n=32) | Normal (n=53) | Abnormal (n=27) |
| Incision
infection | 1 | 0 | 2 | 2 | 1 | 1 |
| Incision rupture | 0 | 2 | 1 | 2 | 0 | 3 |
| Abdominal
infection | 0 | 2 | 0 | 2 | 0 | 1 |
| Lung infection | 0 | 1 | 1 | 2 | 0 | 1 |
| Anastomotic
fistula | 1 | 3 | 0 | 2 | 1 | 2 |
| Pancreatic
fistula | 1 | 3 | 0 | 0 | 1 | 1 |
| Delayed emptying | 1 | 1 | 0 | 1 | 0 | 0 |
| Deep vein
thrombosis | 1 | 2 | 1 | 2 | 1 | 1 |
| Total
incidence | 5 (9.8) | 14 (48.3) | 5 (10.4) | 13 (40.6) | 4 (7.5) | 10 (37) |
| χ2 | 35.958 | 24.004 | 25.153 |
| P-value | <0.001 | <0.001 | <0.001 |
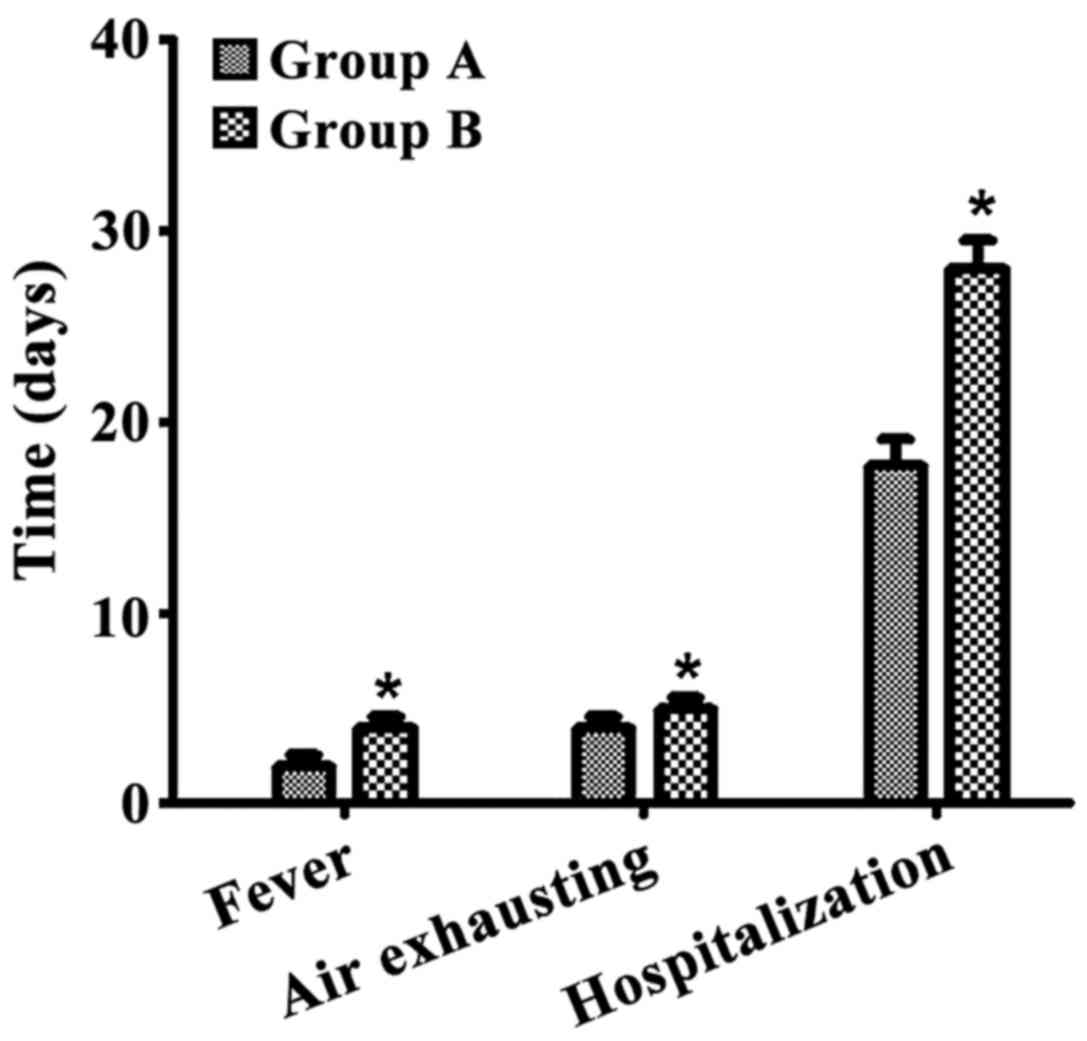
Comparison of postoperative recovery
between the normal groups (group A) and corresponding abnormal
groups (group B)
The incidence of postoperative complications was
significantly lower in group A than in group B (p<0.05; Table IV). Furthermore, postoperative
recovery was significantly better in group A than in the
corresponding group B (p<0.05, Fig.
1).
 | Table IV.Comparison of postoperative
complications between groups A and B at 1 and 3 months after
surgery (n, %). |
Table IV.
Comparison of postoperative
complications between groups A and B at 1 and 3 months after
surgery (n, %).
|
| 1 month after
surgery | 3 months after
surgery |
|---|
|
|
|
|
|---|
| Complications | Group A (n=22) | Group B (n=58) | Group A (n=22) | Group B (n=58) |
|---|
| Intestinal
obstruction | 1 (4.5) | 3 (5.2) | 2 (9) | 5 (8.6) |
| Ascites | 1 (4.5) | 3 (5.2) | 2 (9) | 4 (6.8) |
| Pleural
effusion | 0 (0) | 2 (3.4) | 1 (4.5) | 2 (3.4) |
| Anastomotic
fistula | 1 (4.5) | 4 (6.8) | 1 (4.5) | 4 (6.8) |
| Incision
infection | 0 (0) | 3 (5.2) | 0 (0) | 5 (8.6) |
| Incision
rupture | 0 (0) | 3 (5.2) | 0 (0) | 5 (8.6) |
| Total
incidence | 3 (13.6) | 18 (31) | 6 (27.3) | 25 (43.1) |
| χ2 | 8.737 | 5.472 |
| P-value | 0.003 | 0.019 |
Correlations between postoperative
complications and blood glucose, blood lipids and blood pressure by
logistic regression analysis
Logistic regression analysis showed that the
incidence of postoperative complications was associated with
fasting blood glucose, 2 h postprandial blood glucose, glycosylated
hemoglobin, LDL, mean blood pressure and BMI (p<0.05) (Tables V and VI).
 | Table V.Value assignment of blood glucose,
blood lipids, blood pressure and other related factors. |
Table V.
Value assignment of blood glucose,
blood lipids, blood pressure and other related factors.
| Serial no. | Items | Value
assignment |
|---|
| 1 | FBG | ≥0; male, 1 |
| 2 | 2 h postprandial
blood glucose | <7.8 mmol/l, 0;
≥7.8 mmol/l, 1 |
| 3 | Glycated
hemoglobin | <6.1, 0; ≥6.1,
1 |
| 4 | Total TGs | <1.7 mmol/l, 0;
≥1.7 mmol/l, 1 |
| 5 | LDL | >0.9 mmol/l, 0;
≤0.9 mmol/l, 1 |
| 6 | Average blood
pressure | SBP/DBP<140/90
mmHg, 0; SBP/DBP≥140/90 mmHg, 1 |
| 7 | BMI | <25, 0; ≥25,
1 |
 | Table VI.Correlations between the
postoperative complications and blood glucose, blood lipids and
blood pressure by logistic regression analysis. |
Table VI.
Correlations between the
postoperative complications and blood glucose, blood lipids and
blood pressure by logistic regression analysis.
| Observation
indexes | Partial regression
coefficient | Partial regression
coefficient standard error | Wald χ2
value | P-value | OR (95% CI) |
|---|
| Fasting blood sugar
2 h postprandial blood | 1.344 | 0.336 | 15.977 | <0.001 | 3.834
(1.984–7.411) |
| glucose | 0.783 | 0.443 | 8.126 | 0.037 | 2.189
(6.918–10.215) |
| Glycated
hemoglobin | 0.644 | 0.336 | 3.906 | 0.048 | 1.942
(1.006–3.752) |
| Total TGs | 0.468 | 0.274 | 2.916 | 0.088 | 1.596
(0.93–2.730) |
| HDL | 0.436 | 0.327 | 7.223 | 0.040 | 1.515
(6.814–8.941) |
| Average blood
pressure | 0.345 | 0.127 | 9.306 | 0.035 | 1.485
(7.912–12.540) |
| BMI | 0.012 | 0.007 | 3.943 | 0.045 | 1.358
(1.065–1.650) |
Discussion
The incidence and mortality rate of gastric cancer
are relatively high in China. The mortality rate of gastric cancer
is affected by regional factors and sex, and is higher in males
than in females (12). The cure rate
of gastric cancer at an early stage is relatively high, but most
patients with gastric cancer are diagnosed at advanced stages due
to lack of manifestations at early stages (13). MS is a group of metabolic disorders
characterized by IR, including obesity, hyperglycemia, hypertension
and dyslipidemia (14). Reynolds and
He (15) reported that the incidence
of MS was 19.5% in adults and 18% in women. MS is closely
associated with the occurrence and development of various malignant
tumors, especially gastrointestinal tumors, most commonly
colorectal, liver and gastric cancer. In addition, Corley et
al (16) have shown that
diabetes is a risk factor for gastric cancer. Metabolic
abnormalities can promote the occurrence and development of cancer,
and dyslipidemia is closely associated with the occurrence of
gastric cancer (17). The 5-year
survival rate of cancer patients complicated with MS who underwent
blood pressure and blood glucose control was significantly higher
than that of those without proper blood pressure and blood glucose
control (18). This study showed
that the proper use of drugs for 1 month led to a decrease of blood
pressure, blood lipids and blood glucose control to normal levels
in the MS group, and there was no statistical difference between
the MS and non-MS groups. In addition, the incidence of
postoperative complications was significantly lower, while recovery
conditions were significantly better in patients with normal blood
pressure, blood lipids and blood glucose than that of patients with
abnormal blood pressure, blood lipids and blood glucose at 1 and 3
months after surgery.
Wang et al (19) have shown that preoperative correction
and improvement of certain medical factors in patients can reduce
the incidence of complications to some extent. A body's stress
response caused by surgical stimulation can cause IR in patients,
which in turn affects the level of insulin and cause fluctuations
of blood glucose, resulting in the occurrence of related
complications. For MS patients, blood glucose, blood lipids and
blood pressure should be controlled by using corresponding drugs
after surgery to improve dyslipidemia. Compared with other risk
factors, MS and its related factors have less controllability and
are prone to fluctuate during the perioperative period, making them
more prominent in occurrence of postoperative complications of
gastric cancer patients. In this study, logistic regression
analysis showed that incidence of postoperative complications was
related to fasting blood glucose, 2 h postprandial blood glucose,
glycosylated hemoglobin, total TGs, LDL, mean blood pressure and
BMI (p<0.05). These findings are consistent with those reported
by Kim et al (20) that
patients with hyperglycemia, hypertension, and hyperlipidemia had a
significantly higher probability of developing adverse reactions
than non-MS patients, and BMI was in direct proportion to the
incidence of hyperlipidemia.
In conclusion, effective control of blood glucose,
blood lipid and blood pressure in patients with gastric cancer
complicated with MS after radical gastrectomy can reduce the
incidence of postoperative complications and promote postoperative
recovery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LS was a major contributor in writing this
manuscript and patient treatment. PZ collected the data. QH
analysed the data. CJ provided ideas on methods and interpreted the
results. CG designed this study and performed the research. BS
revised and finalized this report. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Daqing Longnan Hospital (Daqing, China). The patients who
participated in this study, signed informed consent and had
complete clinical data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hartgrink HH, Jansen EPM, van Grieken NCT
and van de Velde CJH: Gastric cancer. Lancet. 374:477–490. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Catalano V, Labianca R, Beretta GD, Gatta
G, de Braud F and Van Cutsem E: Gastric cancer. Crit Rev Oncol
Hematol. 71:127–164. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Baghestani AR, Daneshva T, Pourhoseingholi
MA and Asadzadeh H: Survival of colorectal cancer in the presence
of competing-risks-modeling by Weibull distribution. Asian Pac J
Cancer Prev. 17:1193–1196. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hu D, Peng F, Lin X, Chen G, Zhang H,
Liang B, Ji K, Lin J, Chen LF, Zheng X, et al: Preoperative
metabolic syndrome is predictive of significant gastric cancer
mortality after gastrectomy: The Fujian Prospective Investigation
of Cancer (FIESTA) Study. EBioMedicine. 15:73–80. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bloomgarden ZT: Obesity and diabetes.
Diabetes Care. 23:1584–1590. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Katzmarzyk PT, Janssen I, Ross R, Church
TS and Blair SN: The importance of waist circumference in the
definition of metabolic syndrome: Prospective analyses of mortality
in men. Diabetes Care. 29:404–409. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lin Y, Ness-Jensen E, Hveem K, Lagergren J
and Lu Y: Metabolic syndrome and esophageal and gastric cancer.
Cancer Causes Control. 26:1825–1834. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Peng F, Hu D, Lin X, Chen G, Liang B,
Zhang H, Ji K, Huang J, Lin J, Zheng X, et al: Preoperative
metabolic syndrome and prognosis after radical resection for
colorectal cancer: The Fujian prospective investigation of cancer
(FIESTA) study. Int J Cancer. 139:2705–2713. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sasako M, Sano T, Yamamoto S, Kurokawa Y,
Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai
K, et al: Japan Clinical Oncology Group: D2 lymphadenectomy alone
or with para-aortic nodal dissection for gastric cancer. N Engl J
Med. 359:453–462. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Biesen R, Burmester GR and Hiepe F:
Rheumatoid factor or antinuclear antibodies as incidental finding.
Internist (Berl). 55:1157–1164. 2014.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pourhoseingholi MA, Moghimi-Dehkordi B,
Safaee A, Hajizadeh E, Solhpour A and Zali MR: Prognostic factors
in gastric cancer using log-normal censored regression model.
Indian J Med Res. 129:262–267. 2009.PubMed/NCBI
|
|
12
|
Won KB, Chang HJ, Han D, Sung J and Choi
SY: Metabolic syndrome predicts long-term mortality in subjects
without established diabetes mellitus in asymptomatic Korean
population: A propensity score matching analysis from the Korea
Initiatives on Coronary Artery Calcification (KOICA) registry.
Medicine (Baltimore). 95:e54212016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Esposito K, Chiodini P, Colao A, Lenzi A
and Giugliano D: Metabolic syndrome and risk of cancer: A
systematic review and meta-analysis. Diabetes Care. 35:2402–2411.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhou HC, Lai YX, Shan ZY, Jia WP, Yang WY,
Lu JM, Weng JP, Ji LN, Liu J, Tian HM, et al: Effectiveness of
different waist circumference cut-off values in predicting
metabolic syndrome prevalence and risk factors in adults in China.
Biomed Environ Sci. 27:325–334. 2014.PubMed/NCBI
|
|
15
|
Reynolds K and He J: Epidemiology of the
metabolic syndrome. Am J Med Sci. 330:273–279. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Corley DA, Kubo A and Zhao W: Abdominal
obesity and the risk of esophageal and gastric cardia carcinomas.
Cancer Epidemiol Biomarkers Prev. 17:352–358. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
MacInnis RJ, English DR, Hopper JL and
Giles GG: Body size and composition and the risk of gastric and
oesophageal adenocarcinoma. Int J Cancer. 118:2628–2631. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee S, Bacha F and Arslanian SA: Waist
circumference, blood pressure, and lipid components of the
metabolic syndrome. J Pediatr. 149:809–816. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang H, Zhou XB, Zhou YB, Niu ZJ, Chen D,
Wang DS, Lü L and Li Y: Multivariate logistic regression analysis
of postoperative severe complications and discriminant model
establishment in gastric cancer post gastrectomy. Zhonghua Wai Ke
Za Zhi. 46:1902–1905. 2008.(In Chinese). PubMed/NCBI
|
|
20
|
Kim HA, Jeon JY, An JM, Koh BR and Suh CH:
C-reactive protein is a more sensitive and specific marker for
diagnosing bacterial infections in systemic lupus erythematosus
compared to S100A8/A9 and procalcitonin. J Rheumatol. 39:728–734.
2012. View Article : Google Scholar : PubMed/NCBI
|