Introduction
Solitary pulmonary nodule (SPN) represents solitary
round lesions with diameter of less than 3.0 cm, which are
generally not accompanied by nodular lesions (such as atelectasis,
lymphadenopathy, and pleural effusion) (1). Common causes for SPN mainly include
tumor-like lesions (benign and malignant lesions), infectious
lesions, and non-infectious lesions. There are significant
differences in the treatment and prognosis between benign and
malignant lesions. Therefore, the diagnosis of benign and malignant
lesions is of great importance for the disease clinical diagnosis
and treatment (2,3). However, differential diagnosis of SPN
(benign or malignant) is still an important and difficult task for
imaging technology (4).
In recent years, the rapid development of multislice
spiral computed tomography (MSCT) technology represents a promising
approach for the diagnosis of SPN. MSCT can display the lesions
more clearly and intuitively, which is great helpful for the
qualitative diagnosis of SPN (5).
Moreover, MSCT dynamic enhancement scanning could provide more
detailed evidence for the blood supply of lesions and their
relationship with surrounding blood vessels, which is a reliable
basis for the clinical feasibility of surgery (6). In this study, SPN was systematically
characterized with the combination of dynamic enhancement
parameters and morphological features of nodules, in order to
improve the correct diagnosis rate of the disease.
Materials and methods
Study subjects
Totally 93 patients with SPN, who were confirmed by
CT detection in our hospital from July 2014 to June 2016, were
included in this study. There were 55 males and 38 females, with an
average age of 40.71±3.64 years (ranging from 27 to 61 years).
According to the pathological detection, 52 cases were ultimately
diagnosed as malignant nodules and 41 cases were finally determined
as benign nodules (including 26 cases of inflammatory nodules).
Inclusion criteria were as follows: i) Patients of
SPN as confirmed by CT detection, with diameter of <30 mm,
without atelectasis, satellite lesions, or lymphadenopathy
(mediastinal lymph node, or in the hilus pulmonis region); ii)
patients with detailed, complete clinical data, as well as
corresponding examination results; iii) patients without serious
organic diseases of heart, brain, and other vital organs; and iv)
patients not receiving radiotherapy or chemotherapy. Prior written
and informed consent were obtained from every patient and the study
was approved by the ethics review board of our hospital. Exclusion
criteria included: i) Patients with multiple pulmonary nodules, or
with lung mass with diameter of >30 mm; ii) patients with
contrast agent allergies; iii) patients who could not tolerate
imaging due to failures of heart, liver, kidney, and/or other
organs; and iv) patients who refused to participate in this
study.
CT scanning
CT scanning was performed with the 64-slice
multidetector CT scanner (Aquilion 64; Toshiba, Otawara, Japan).
All patients were subjected to routine and enhanced CT scanning.
During scanning, the patients were asked to hold their breath after
breathing in. Scanning range covered from the apex pulmonis to the
basis pulmonis. CT scanning parameters were as follows: Voltage,
120 kV; current, 200 mAs; slice thickness, 3.0 mm; pitch, 1.5 mm;
and reconstruction interval, 3.0 mm. Based on the routine scanning,
dynamic enhancement scanning was conducted over the reduced range
covering the nodules (±2 cm), with the same scanning parameters
mentioned. Enhanced scanning contrast agent was iohexol (100 ml),
which was injected (as a bolus) with the high-pressure syringe, at
the injecting rate of 2 ml/s. Scanning images were obtained at 0,
30, 60, 90, 120, 300 and 540 sec, respectively, after the injection
of contrast agent.
Image processing and analyzing
For the original images from CT routine and dynamic
enhancement scanning, 0.625-mm thin-slice reconstruction was
conducted. Obtained data were transferred to the GE ADW 4.3
post-processing work station (General Electric Healthcare,
Milwaukee, WI, USA), and multi-planar reformation (MPR), curved
planar reformation (CPR), and volume reproduction (VR) were
performed. The lesions were clearly displayed, particularly for the
SPN size, distribution, morphology, and boundary, as well as the
relationship between SPN and bronchus. The mean CT values for each
time point from the routine and dynamic enhancement scanning were
obtained. MSCT original scanning images, reconstruction images, and
dynamic enhancement images were analyzed by two senior
radiologists. Each case was diagnosed, and the lesion location,
range, and bronchial involvement were determined. Diagnosis was
confirmed only when consensus was achieve.
Statistical analysis
Data were expressed as mean ± SD. SPSS 14.0 software
(SPSS, Inc., Chicago, IL, USA) was used for statistical analysis.
Measurement data were analyzed by ANOVA, with the LSD test, while
counting data were compared with the χ2 test. P<0.05
was considered to indicate a statistically significant
difference.
Results
Imaging characteristics of benign and
malignant SPN cases
All these 93 patients were diagnosed by biopsy or
surgical pathology. Detailed results from the pathological
diagnosis were shown in Table I. For
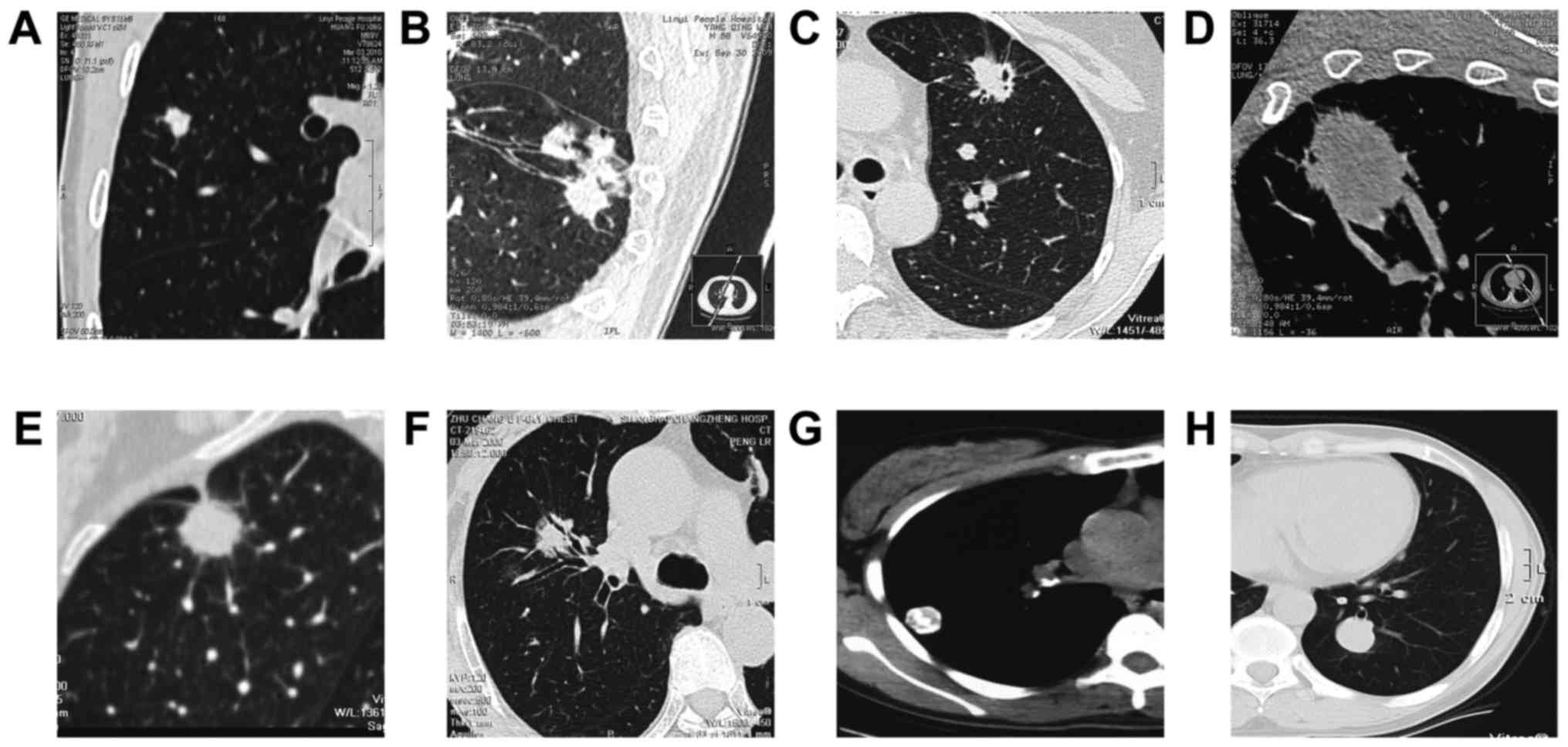
the CT scanning, the main signs for these 93 SPN cases included the
lobulation, spicular sign, pleural indentation, vessel convergence,
vacuole sign, aerial bronchogram, satellite lesions, and
calcification (Fig. 1). As shown in
Table II, compared with the benign
SPN group, the incidences of lobulation, spicular sign, pleural
indentation, and vacuole sign were significantly elevated in the
malignant SPN group (P<0.05). On the other hand, the incidence
of calcification in the benign SPN group was significantly higher
than the malignant SPN group (P<0.05). However, no significant
differences were observed in the incidences of vessel convergence,
aerial bronchogram, or satellite lesions between the benign and
malignant SPN groups (P>0.05). Taken together, these results
suggest that significant differences in the CT image morphology
could be observed between benign and malignant SPN cases.
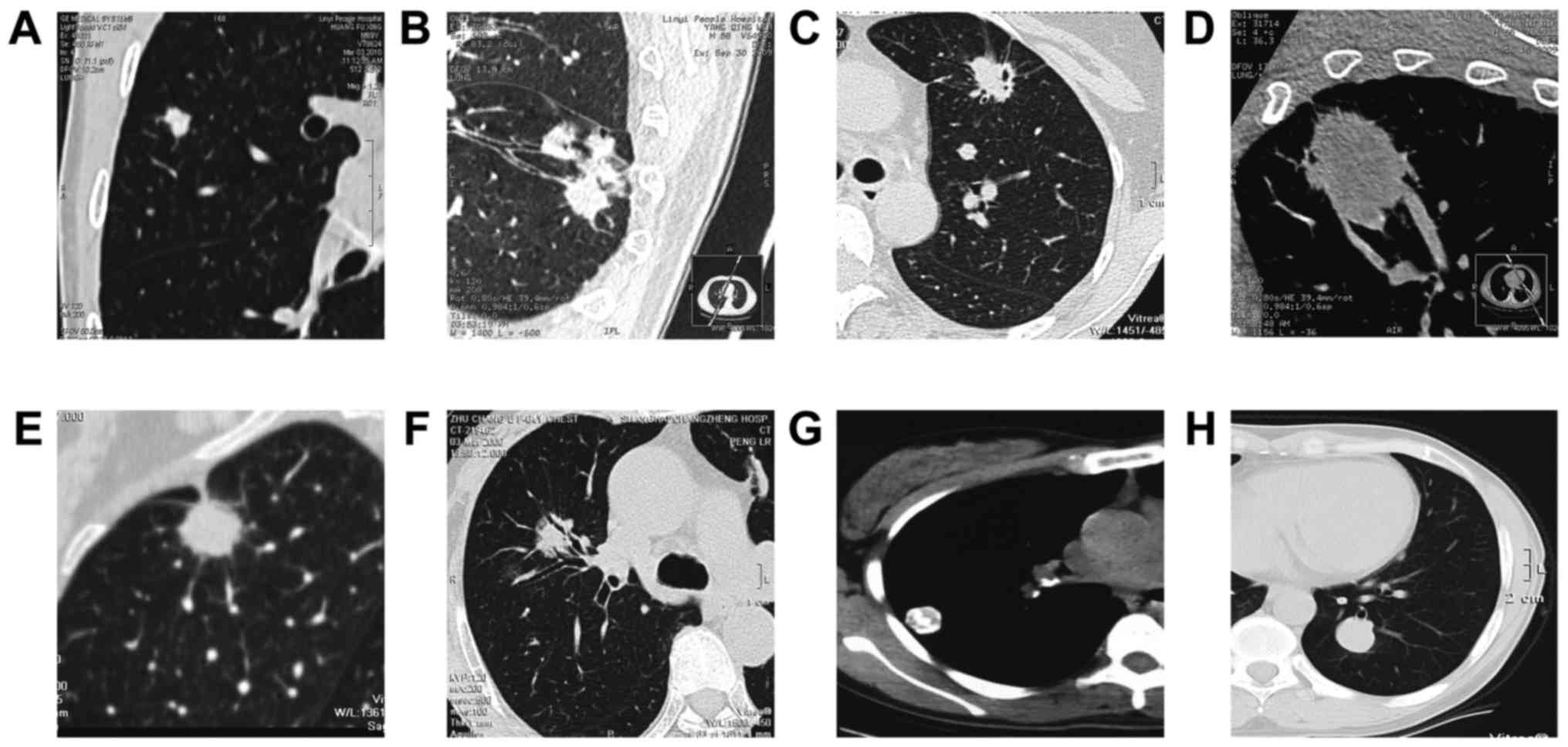 | Figure 1.Imaging characteristics of benign and
malignant SPN cases. (A) MPR reconstruction showing right upper
lobe nodule with shallow lobulation (adenocarcinoma as confirmed by
postoperative pathology). (B) MPR reconstruction showing right
lower lobe nodule with deep lobulation. Pleural indentation and
vacuole sign were also observed, and the bronchus was truncated at
the nodule boundary (squamous carcinoma as confirmed by
postoperative pathology). (C) Left upper lobe with lobulation,
spicular sign at the boundary. Vacuole sign was also observed
(adenocarcinoma as confirmed by postoperative pathology). (D) MPR
reconstruction showing that the left upper lobe nodules, surrounded
by a number of blood vessels accumulating towards the nodule, i.e.,
vessel convergence (squamous carcinoma as confirmed by
postoperative pathology). (E) MPR reconstruction showing right
upper lobe nodule, with spicular sign and pleural indentation
(adenocarcinoma as confirmed by postoperative pathology). (F) MPR
reconstruction showing right upper lobe nodule, with vacuole sign
inside (squamous carcinoma as confirmed by postoperative
pathology). (G) Right lower lobe nodule, with smooth boundary and
calcification sign inside (hamartoma as confirmed by puncture
biopsy). (H) Left lower lobe nodule, with smooth boundary and
uniform density, closely related to peripheral blood vessels
(sclerosing hemangioma as confirmed by postoperative
pathology). |
 | Table I.Pathological diagnosis of 93 included
patients. |
Table I.
Pathological diagnosis of 93 included
patients.
| Diagnosis | No. | Incidence (%) |
|---|
| Malignant SPN | 52 | 55.91 |
| Squamous
carcinoma | 25 | 48.08 |
|
Adenocarcinoma | 17 | 32.69 |
| Bronchial
alveolar carcinoma | 7 | 13.46 |
| Small
cell carcinoma | 3 | 5.77 |
| Benign SPN | 41 | 44.09 |
|
Sclerosing hemangioma | 6 | 14.63 |
|
Hamartoma | 5 | 12.20 |
|
Tuberculosis ball | 11 | 26.83 |
| Inflammatory
nodules | 19 | 46.34 |
 | Table II.Comparison of the morphological signs
between benign and malignant SPN cases. |
Table II.
Comparison of the morphological signs
between benign and malignant SPN cases.
|
| Malignant SPN (n=52),
n (%) | Benign SPN (n=41), n
(%) | χ2 | P-value |
|---|
| Spicular sign | 31 (59.62) | 7 (17.07) | 22.115 | <0.01 |
| Lobulation | 33 (63.46) | 8 (19.51) | 23.804 | <0.01 |
| Pleural
indentation | 28 (53.85) | 6 (21.43) | 18.988 | <0.01 |
| Vacuole sign | 13 (25.00) | 2 (4.88) | 7.752 | <0.01 |
| Aerial
bronchogram | 6 (11.54) | 4 (9.76) | 0.098 | <0.01 |
| Vessel
convergence | 9 (17.31) | 7 (17.07) | 0.413 | <0.01 |
| Satellite
lesions | 2 (3.84) | 2 (4.88) | 0.375 | <0.01 |
| Calcification | 3 (5.77) | 9 (21.95) | 4.137 | <0.01 |
Dynamic enhancement of different SPN
types
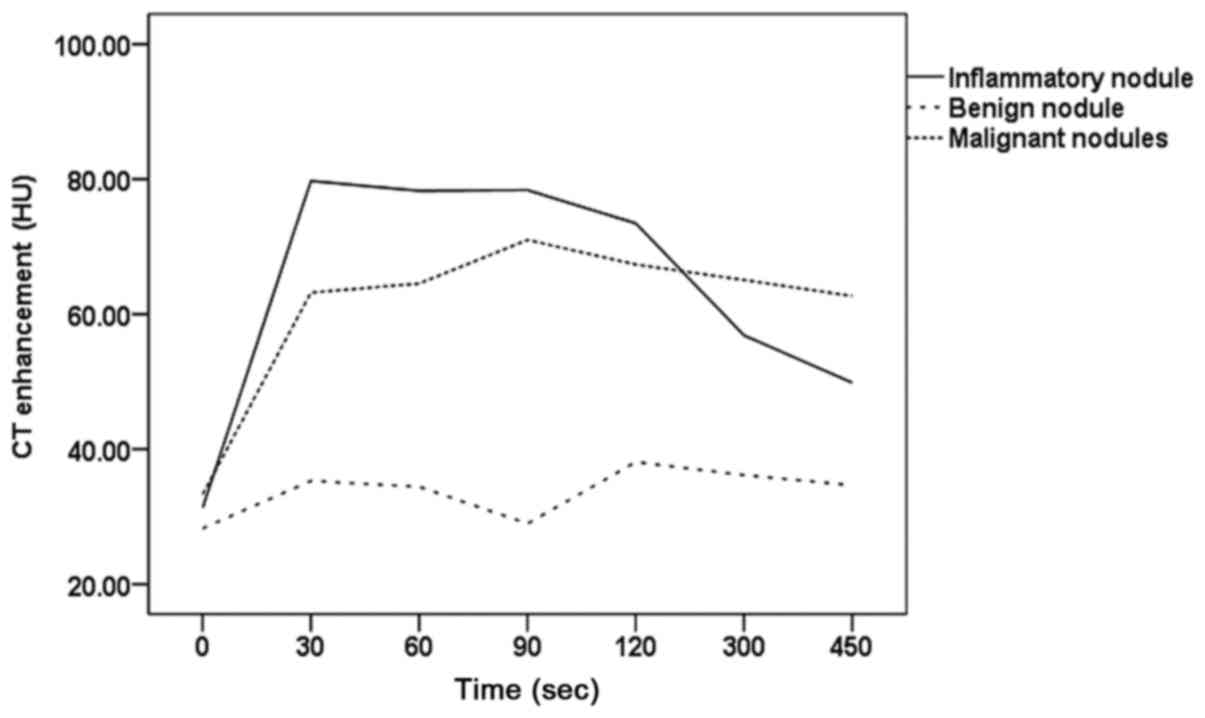
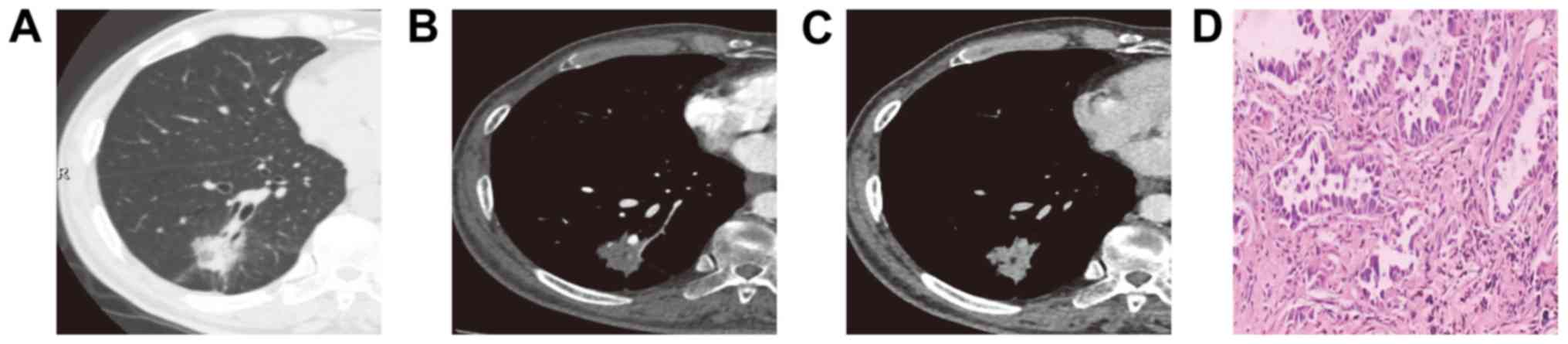
Different time density curve (TDC) types were
observed for malignant and benign SPN, and inflammatory nodules
(Fig. 2). Our results showed that,
for the malignant SPN, obvious enhancement was observed at 30 sec
after contrast injection, which peaked at 90 sec after injection
and then maintained at high levels for a period (Fig. 3). For the benign SPN, only mild or
less evident enhancement was noted during the enhancement process.
For the inflammatory nodules, obvious enhancement was observed
immediately after the contrast injection, which begun to decline at
120 sec after injection (Fig. 4).
For the malignant SPN and inflammatory nodules, during the dynamic
enhancement scanning, the CT values at all the time points were
significantly higher than the benign SPN group (t=8.10, 8.55, 8.32,
8.97, 9.44, 10.52, 7.62, 7.85, 6.02, 5.41, 5.22, and 3.69,
respectively; P<0.05). Dynamic enhancement CT values at
different time points between benign and malignant groups were next
compared. Our results showed that, dynamic enhancement CT values
were elevated for both groups, at 30, 60, 90, and 120 sec after
contrast injection, without significant difference (t=3.27 and
3.69, respectively; P<0.05). However, at 300 and 540 sec after
contrast injection, the dynamic enhancement CT values for the
inflammatory nodule group was obviously declined, which were
significantly lower than the dynamic enhancement CT values at
corresponding time points in the malignant SPN group (t=3.27 and
3.69; P<0.05). In fact, no obvious decline was observed in the
dynamic enhancement CT value in the malignant SPN group, at 300 and
540 sec after contrast injection (Table III). Taken together, these results
suggest that, during the dynamic enhancement, significant
differences could be observed in the CT values between different
TDCs and different time points.
 | Table III.Comparison of dynamic enhancement CT
values for benign an malignant SPN. |
Table III.
Comparison of dynamic enhancement CT
values for benign an malignant SPN.
| Dynamic enhancement
time (s) | Benign SPN (n=22),
HU | Malignant SPN (n=52),
HU | Inflammatory nodules
(n=19), HU |
|---|
| 0 (routine) |
27.38±10.87 |
33.69±7.21 |
31.25±10.10 |
| 30 |
35.41±14.97 |
63.95±11.32a |
79.13±23.62a |
| 60 |
34.87±18.75 |
64.57±10.21a |
78.37±21.57a |
| 90 |
28.06±11.52 |
71.33±11.08a |
78.95±26.21a |
| 120 |
38.32±15.64 |
67.89±10.14a |
73.95±20.35a |
| 300 |
36.02±13.27 |
65.13±9.22a |
57.22±28.63a,b |
| 540 |
34.81±13.95 |
62.57±7.61a |
49.36±23.04a,b |
Diagnostic accordance rate of
morphological signs combined with dynamic enhancement
diagnosis
Diagnostic accordance rates of morphological signs
alone, as well as morphological signs combined with dynamic
enhancement diagnosis, were then investigated. Our results showed
that, the diagnostic accordance rate for the morphological signs
combined with dynamic enhancement diagnosis was 83.87%, which was
significantly higher than that for the morphological signs alone
(70.97%) (Table IV; P<0.05).
These results suggest that, CT image morphology combined with
dynamic enhancement diagnosis might lead to relatively high
diagnostic accordance rate.
 | Table IV.Comparison of diagnostic accordance
rates. |
Table IV.
Comparison of diagnostic accordance
rates.
|
| In accordance with
surgical and puncture findings |
|
|
|---|
|
|
|
|
|
|---|
| Variables | Yes, n (%) | No, n (%) | χ2 | P-value |
|---|
| Morphological
signs | 66 (70.97) | 27 (29.03) | 6.257 | <0.05 |
| Morphological signs +
dynamic enhancement | 78 (83.87) | 15 (16.13) |
|
|
Discussion
SPN have been observed for different lesions.
Malignant SPN cases are mostly peripheral lung cancers, with less
cases of metastasis. Benign SPN cases mainly include tuberculoma,
inflammatory lesions, and hamartoma (7). Qualitative diagnosis of SPN is
important for the clinical treatment and disease prognosis.
However, there are many difficulties for the CT-based qualitative
diagnosis of SPN in clinic due to it simply depends on the
morphological changes (1,8). With the rapid development and wide
application of CT technology, more and more SPN cases have been
diagnosed. Therefore, the early detection and accurate diagnosis of
SPN are critical and important for the clinical treatment and
disease.
Thoracic CT 3-D reconstruction is superior to
ordinary thoracic CT scanning in the diagnostic sensitivity and the
morphological observation of SPN. For the 3-D reconstruction, due
to its high resolution and satisfactory continuity, small lesions
would not be missed, and it is easier to determine the lesion size
and accurate location. Moreover, the surface characteristics of SPN
(lobulation, sub-thorns, thorn-like processes, and halo sign) could
be intuitively displayed, which might contribute to distinguish the
benign and malignant cases, and help to develop the therapeutic
regimen. Compared with the 16-slice MSCT, the 64-slice MSCT has
more powerful post-processing ability, including MPR, CPR, MIP, and
VRT, which could clearly show the nodule morphology and various
signs. Meanwhile, scanning speed has been greatly increased, which
reduces the respiratory motion-induced artifacts, making it
possible for the nodular volume dynamic enhanced scanning.
Benign and malignant SPN cases exhibited
differential characteristics on CT imaging. In the present study,
our results showed that, the main CT signs for malignant SPN cases
included the lobulation, spicular sign, pleural indentation, and
vacuole sign, with the incidences of 63.46, 59.62, 53.85, and
25.00%, respectively, which reflected the pathological changes for
the lung tumors. Boundaries of malignant SPN lesions are mostly
irregular or lobulated, which are associated with the different
growth rate of each tumor part, as well as the surrounding
structure restriction. In particular, deep lobulation in the
malignant SPN lesions has great diagnostic value (1). In the present study, the incidence of
lobulation was 63.46% for the malignant SPN group. In line with
this, a previous study has shown that the incidence of lobulation
for the malignant SPN cases (64.40%) is significantly higher than
the benign SPN cases (9).
Moreover, spicular sign is a result of the extension
and infiltration of tumor tissues into the adjacent lung
parenchyma, which has been commonly seen in malignant nodules. A
previous study has shown that the incidence of spicular sign for
malignant SPN is 67.7%, which represents a risk factor for
malignant SPN (10). In the present
study, the incidence of spicular sign for the malignant SPN group
was 59.62%. Vacuolar sign is induced by the tumor-damaged alveolar
structures within the nodules. It has been shown that the incidence
of vacuolar sign in the lung tumors is approximately 24–48%, which
has been mainly seen in the adenocarcinomas, squamous carcinomas,
and bronchiolo-alveolar carcinomas (11). Our results for the incidence of
vacuolar sign (25.00%) were basically consistent with these
findings. In addition, pleural indentation is another potent sign
for the identification of benign and malignant SPN cases (12).
A previous study has shown that, in 29 cases of
malignant nodules, there are 18 cases with pleural indentation, and
the majority of remaining cases without pleural indentation have
malignant nodules far away from pleura (13). Li et al (13) have shown that, the incidence of
pleural indentation is 13.1% for the benign nodules, which is 25.4%
for the malignant nodules. Moreover, Cui et al (14) have shown that, it is not specific to
diagnose lung cancer with only pleural indentation, while the
specificity for pleural indentation combined with associated notch
(i.e., the notch connected to nodules) in diagnosing lung cancer is
as high as 96%, with the positive prediction rate of 97%.
Air bronchogram refers to the presence of air bronch
within SPN lesions. It has been shown that, the incidences of air
bronchogram for benign and malignant nodules are 5.9 and 33%,
respectively. Ma et al (15)
have shown that, the incidence of air bronchogram for the
adenocarcinoma is as high as up to 48. 8%, while the incidences for
squamous carcinoma, alveolar carcinoma, and undifferentiated
carcinoma were 20, 9.1, and 28.6%, respectively.
Vessel convergence refers to the sign in which one
or more vessels surrounding SPN were dragged by the lesions to
accumulate around or pass through the lesions, or truncated by the
boundaries. It has been shown that, malignant lesions are
associated with truncation, uneven wall thickening, lumen
expansion, and tail-like changes of adjacent bronchi. On the other
hand, benign lesions usually compress and flatten the adjacent
bronchi, without wall thickening (16). It has been previously shown that the
incidences of vessel convergence for benign and malignant SPN are
12 and 31%, respectively. However, in this study, no significant
differences have been observed in the air bronchogram and vessel
convergence between benign and malignant groups. This might be due
to the limited sample size herein, which needed further in-depth
studies.
Our results showed that, the case number of
calcification within benign SPN lesions is significantly higher
than the malignant lesions. In the past, calcification has once
been recognized as benign lesion (17). However, later studies have shown
that, even SPN cases with calcification could not be excluded from
malignant tumors (18). Fat in the
SPN represents a strong evidence for benign lesions, which is
commonly seen in hamartoma. Calcification and fat density could be
present within SPN, which always imply benign lesions. At present,
studies concerning SPN have been mainly focusing on single sign and
the prediction model for benign and malignant lesions (19). However, in fact, there might be one
or more signs in a case. Therefore, it is difficult to distinguish
between benign and malignant lesions based on one single sign, and
analysis of combined multiple signs is needed.
Due to the lack of typical signs such as lobulation
and burr in some SPN cases, the imaging performance crossover with
some benign nodules, making it difficult for the early diagnosis
and treatment of cancers. Some patients with benign nodules receive
surgical treatment before the clear diagnosis, which increases the
patients' suffering, reduce their quality of life, and causes the
waste of medical resources. MSCT dynamic enhancement is an
important method to evaluate SPN (assessing hemodynamics and
perfusion status), which measures densities at different time
points after injection of contrast agent and provides evaluable
evidence for differential diagnosis. A previous study performed
enhancement detection on small nodules in lung, and they have found
out that the enhancement peak values are different between benign
and malignant nodules (20,21). Appropriate peak enhancement threshold
can help identifying the characteristics of SPN. They have shown
that, CT values increase after enhancement of <15 HU indicate
benign nodules, while CT values increase after enhancement of
>15 HU suggest malignant nodules, with the sensitivity,
specificity, and accuracy of 98, 58, and 77%, respectively.
Moreover, it has been also shown that, enhancement of ≤20 HU or ≥60
HU indicates benign nodules, while the enhancement of 20–60 HU
suggests malignant nodules, and enhancement of ≥60 HU is probably
associated with active inflammatory nodules (22).
Jeong et al, and Zhang and Kono (23,24) have
studied the time-density curve (TDC) of SPN. They have found that,
for inflammatory SPN, the TDC increases rapidly, with the highest
peak, after which the TDC shortly decreases and then increases,
then followed by obvious decline. However, for benign SPN, the TDC
is at a low level, or almost without elevation. Furthermore, for
malignant SPN, the TDC increases rapidly, stays on plateau after
peaking, and then slightly declines. In line with our results,
different TDC morphologies for benign and malignant lesions reflect
the differences in fluid volume outside nodular cells and
dispersion rate of contrast agent. In this study, for the
inflammatory nodules and malignant SPN, during the dynamic
enhancement scanning, the CT values at each time points were all
significantly higher than the benign SPN group. Comparing the
dynamic enhancement CT values at different time points, our results
showed that, the dynamic enhancement CT values at 30, 60, 90, and
120 sec were significantly elevated for both the inflammatory
nodules and malignant SPN cases. However, no significant
differences were observed between these two groups. On the other
hand, at 300 and 540 sec, the dynamic enhancement CT values were
significantly declined in the inflammatory nodules, while no
obvious decline was observed for the malignant SPN group. The
dynamic enhancement CT values at 300 and 480 sec for the
inflammatory nodules were significantly lower than the malignant
SPN group. Based on these results, CT dynamic enhancement detection
has great value for the identification of benign and malignant
nodules. However, the differential findings from different studies
might be due to different nodule natures, different parameters
(such as the total amount of contrast agent, injection rate, and
delayed scanning time), and some complex physiological factors
(such as cardiac output, pulmonary blood flow, and body weight),
which should be considered for the differential diagnosis. Clear
and accurate exhibition and identification of morphological signs,
combined with the dynamic enhancement detection, are of great
clinical value for the differential diagnosis of benign and
malignant nodules. Our results showed that, the diagnostic
accordance rate for the morphological signs combined with dynamic
enhancement diagnosis was significantly higher than the
morphological signs alone.
In summary, the morphological features of SPN are of
great significance and importance for the differential diagnosis in
clinic. Dynamic enhancement CT scanning could provide a variety of
dynamic enhancement parameters for nodules, which might be valuable
for the identification of benign and malignant lesions.
Comprehensive application of morphological features and dynamic
enhancement detection can improve the diagnostic accuracy of
malignant nodules, contributing to the disease early diagnosis, in
time treatment, and prognosis, and avoiding the waste of medical
resources due to unnecessary surgeries.
Acknowledgements
We are grateful to Jian Yang, Deputy Chief Physician
from the Department of Radiology, Chongqing General Hospital for
the assistance in the manuscript preparation.
References
|
1
|
Wahidi MM, Govert JA, Goudar RK, Gould MK
and McCrory DC: American College of Chest Physicians: Evidence for
the treatment of patients with pulmonary nodules: When is it lung
cancer? ACCP evidence-based clinical practice guidelines (2nd
edition). Chest. 132 3 Suppl:94S–107S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Prakashini K, Babu S, Rajgopal KV and
Kokila KR: Role of computer Aided diagnosis (CAD) in the detection
of pulmonary nodules on 64 row multi detector computed tomography.
Lung India. 33:391–397. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lin JZ, Zhang L, Zhang CY, Yang L, Lou HN
and Wang ZG: Application of gemstone spectral computed tomography
imaging in the characterization of solitary pulmonary nodules:
Preliminary result. J Comput Assist Tomogr. 40:907–911. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Truong MT, Sabloff BS and Ko JP:
Multidetector CT of solitary pulmonary nodules. Radiol Clin North
Am. 48:141–155. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wu B: Comparison and analysis of diagnosis
spiral CT and high-resolution CT for peripheral lung cancer with
diameter of <3 cm. Chin Med Herald. 8:78–79. 2011.(In
Chinese).
|
|
6
|
Wang B and Li H: Significance of dynamic
contrast-enhanced CT in the differential diagnosis of solitary
pulmonary nodules. Chin J Lab Diagn. 16:1495–1496. 2012.(In
Chinese).
|
|
7
|
LN E and Ma D: Imaging diagnosis and
management of small pulmonary nodules. Chin J Radio. 43:332–334.
2009.(In Chinese).
|
|
8
|
Shi Z, Wang Y and He X: Differential
diagnosis of solitary pulmonary nodules with dual-source spiral
computed tomography. Exp Ther Med. 12:1750–1754. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
He Q, Yu F, Dai P, Liu Z, Guo R and Yang
B: Comparative study of MSCT and pathological findings of solitary
pulmonary nodules. Chongqing Med. 43:3912–3915. 2014.
|
|
10
|
Yang D, Li Y, Liu J, Jiang G, Li J, Zhao
H, Yang F, Liu Y, Zhou Z, Bu L and Wang J: Study on solitary
pulmonary nodules: Correlation between diameter and clinical
manifestation and pathological features. Zhongguo Fei Ai Za Zhi.
13:607–611. 2010.(In Chinese). PubMed/NCBI
|
|
11
|
Macdonald K, Searle J and Lyburn I: The
role of dual time point FDG PET imaging in the evaluation of
solitary pulmonary nodules with an initial standard uptake value
less than 2.5. Clin Radiol. 66:244–250. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Harders SW, Madsen HH, Rasmussen TR, Hager
H and Rasmussen F: High resolution spiral CT for determining the
malignant potential of solitary pulmonary nodules: Refining and
testing the test. Acta Radiol. 52:401–409. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li Y, Sui X and Yang D: Solitary pulmonary
nodules: A risk factor analysis. Chin J Thoracic Cardiovasc Surg.
26:161–164. 2010.(In Chinese).
|
|
14
|
Cui Y, Ma D and Yang J: The value of
pleural indentation in the diagnosis of pulmonary nodule: A
meta-analysis. J Cap Med Univ. 28:709–712. 2007.
|
|
15
|
Ma YH, Li YX and Fang Y: A comparative
study on pathology and CT signs of small peripheral lung cancer.
Chin J Mod Med. 100–103. 2013.(In Chinese).
|
|
16
|
Zhao BY, Geng C and Beng BZ: The value of
CT-vessel convergence sign in differential diagnosis of SPN. Chin
Imaging Integr Trad West Med. 4:339–341. 2006.(In Chinese).
|
|
17
|
Khan A: ACR Appropriateness criteria on
solitary pulmonary nodule. J Am Coll Radiol. 4:152–155. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lin HL: Development in the diagnosis of
solitary pulmonary nodule by CT. Med Recapitulate (Issue 11).
1725–1727. 2010.(In Chinese).
|
|
19
|
Li Y, Chen KZ, Sui XZ, Bu L, Zhou ZL, Yang
F, Liu YG, Zhao H, Li JF, Liu J, et al: Establishment of a
mathematical prediction model to evaluate the probability of
malignancy or benign in patients with solitary pulmonary nodules.
Beijing Da Xue Xue Bao Yi Xue Ban. 43:450–454. 2011.(In Chinese).
PubMed/NCBI
|
|
20
|
Kim JH, Kim HJ, Lee KH, Kim KH and Lee HL:
Solitary pulmonary nodules: A comparative study evaluated with
contrast-enhanced dynamic MR imaging and CT. J Comput Assist
Tomogr. 28:766–775. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Swensen SJ, Viggiano RW, Midthun DE,
Müller NL, Sherrick A, Yamashita K, Naidich DP, Patz EF, Hartman
TE, Muhm JR and Weaver AL: Lung nodule enhancement at CT:
Multicenter study. Radiology. 214:73–80. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang M, Hua Z and Yu Z: Quantitative
investigation of solitary pulmonary nodules with dynamic
contrast-enhanced functional CT. Clin Oncol Cancer Res. 1:229–235.
2004.
|
|
23
|
Jeong YJ, Lee KS, Jeong SY, Chung MJ, Shim
SS, Kim H, Kwon OJ and Kim S: Solitary pulmonary nodule:
Characterization with combined wash-in and washout features at
dynamic multi-detector row CT. Radiology. 237:675–683. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang M and Kono M: Solitary pulmonary
nodules: Evaluation of blood flow patterns with dynamic CT.
Radiology. 205:471–478. 1997. View Article : Google Scholar : PubMed/NCBI
|