Introduction
The research on ischemic preconditioning (IPC) has
demonstrated that IPC-induced brain tolerance may be early or late,
with the early phase ranging between min and h after the onset of
IPC, and the late phase ranging between h and days after the onset
of IPC (1). Furthermore, IPC
activates several protective molecular pathways, including protein
kinase C, mitogen-activated protein kinase and phosphatidylinositol
3-kinase at different time points (1). A previous study has indicated that,
between 12 and 24 h after IPC, the expression of heat shock protein
heme oxygenase (HO)-1 was activated in newborn rat brains, and
upregulation of HO-1 expression remained for 7 days (2). A previous study also indicated that
HO-1 was able to partially mediate the neuroprotective roles on IPC
(3).
It is known that the rate-limiting enzyme HO is able
to degrade heme in vivo and subsequently antagonize stress
reactions, resulting in a protective effect against cell damage
(4). The pro-oxidant heme may be
subjected to oxidative degradation into the potent antioxidants
carbon monoxide, biliverdin, and free iron by HO (5). Subsequently, biliverdin reductase is
converted rapidly from biliverdin to bilirubin (4–6). There
are two isoenzymes of HO, namely HO-1 and HO-2 (6). HO-2 gene knockout reduces oxidative
stress in nerve cell damage (6).
Conversely, HO-1 knockout mice are more sensitive to
ischemia-reperfusion injury; however induced HO-1 overexpression
may promote a protective effect (7).
Furthermore, HO-1 upregulation may provide protection against
damage induced by cold ischemia (7).
These findings suggest that promoting the activity of HO-1, may
have a potential cytoprotective effect against cell damage. In HO-1
transgenic rats, overexpression of HO-1 has been demonstrated to
attenuate ischemic stroke damage induced by middle cerebral artery
occlusion (MCAO) (8). It has been
indicated that the activity of HO-1 with pharmacological
stimulation may be a novel therapeutic target for the treatment of
ischemic injury (8–10).
Gene transfer was used in the present study to
investigate stroke by transducing genes into neurons (11). There are alternative approaches for
expressing transgenes of interest in adult animals, and then
investigating their effects on cerebral ischemia-reperfusion injury
(11). One viral gene transfer
method involves the use of recombinant adeno-associated viral
vectors, which may deliver transgenes into neurons through a number
of delivery pathways, including intramuscular (12), subcutaneous, intraneural (13), intrathecal (14,15) and
intraspinal applications (16,17),
direct injections into dorsal root ganglia (18), and application of virus accompanied
with herpes simplex virus locality (19).
The objectives of the present study included the
following: i) Identification of the role of HO-1 gene in cerebral
ischemia-reperfusion injury based on the transfection method; ii)
confirmation of the high expression of the HO-1 gene and its
anti-apoptotic effects; and iii) to illuminate the cellular or
physiological effect of recombinant adenovirus bearing HO-1
(Ad-HO-1) against ischemia-reperfusion injury of the brain, which
may have a protective role against stroke or neurological disorders
associated with stroke.
Materials and methods
Adenovirus vector production
The adenovirus-bacterial recombination system
(AdEasy) was supplied by Dr Chen Jing from Thomas Jefferson
University (Philadelphia, PA, USA), including the expression
vectors pGEM-3ZF (+) and pAdEasy-1, which were labeled with green
fluorescent protein (GFP). The rat HO-1 gene was constructed into
adenoviral vectors in the AdEasy Vector System as described
previously (20). The spleens were
taken from 6 3-month-old female Wistar rats (weight, 250±25 g) and
stored at −80°C. The rats were maintained within a specific
pathogen free facility with a constant humidity (55±5%) and
temperature (22±2°C) in a 12 h light/dark cycle with free access to
food and water. Total RNA was extracted from the rats spleen cells
using an RNeasy Total RNA Isolation kit (Qiagen, Inc., Valencia,
CA, USA). Reverse transcription-quantitative polymerase chain
reaction (RT-qPCR) was performed and the products were used for the
gene amplification of HO-1, and subsequently cloned into pAdEasy-1
vectors. The RNA (2 µg per reaction) was reverse transcribed using
avian myeloblastosis virus reverse transcriptase (Promega
Corporation, Madison, WI, USA) at 42°C for 70 min in the presence
of 250 µM dNTPs, avian myeloblastosis reverse transcription 5X
reaction buffer (250 mM Tris-HCl, 250 mM KCl, 50 mM
MgCl2, 50 mM DTT and 2.5 mM spermidine; all Promega
Corporation) and 1 µM oligo-p (dT)15 primer (Roche Molecular
Diagnostics, Pleasanton, CA, USA). PCR amplification reactions were
performed in a total volume of 20 µl containing 1.5 U Taq DNA
polymerase, 2 µl 10X PCR buffer (100 mM Tris-HCl, 500 mM KCl, 15 mM
MgCl2), 0.4 µl 10 mM dNTP (all Promega Corporation) and
~100 ng DNA template on a GeneAmp® PCR System 9700
(Roche Molecular Diagnostics). The thermocycling conditions were as
follows: Predenaturing at 94°C for 5 min, followed by 32 cycles of
denaturing at 94°C for 45 sec, annealing at the temperature
appropriate for each pair of primers for 45 sec and extending at
72°C for 45 sec with a final extension at 72°C for 10 min.
According to the published GeneBank sequence of rat HO-1
(NM_010442) (ncbi.nlm.nih.gov/nuccore/NM_010442.2?report=genbank),
the upstream primer sequence was 5′-ATGGAGCGTCCACAGCTCGAC-3′ and
the downstream primer sequence was 5′-GGGCCAACACTGCATTTACAT-3′. The
HO-1 gene was synthesized by Shanghai Sangon Biological Engineering
Technology & Services Co., Ltd. (Shanghai, China). Prior to
use, assessments for viral concentration and titer of the pAdEasy-1
viral vectors were conducted. The concentration of virus
[plaque-forming unit (pfu)/ml] was measured (21). The 50% tissue culture infection
dosage (TCID50) method was used to measure virus titers. The cells
were seeded into clear, flat-bottomed 96-well plates at
105 cells in 100 µl of DMEM containing 10% fetal calf
serum (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA,
USA), 1% 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid, 1%
L-glutamine, and 1% penicillin/streptomycin. The cells were added
to all wells except column 10, which was left blank to separate the
infected wells and the uninfected control wells. Prior to the assay
an additional 80 µl of maintenance media with DMEM containing 2%
FCS was added to all wells. A total of 20 µl neat or diluted virus
was added to each well in the first column of the plate. The virus
was then serially diluted (1:10, 20 µl into 180 µl) across the
plate from columns 1 to 9 with pipette tips changed between each
column. Column 10 was left empty, and columns 11 and 12 contained
media only and served as controls for uninfected cells. The plates
were then incubated at 37°C with 5% CO2 for 6 days. On
the 6th day, 3 µl (1.5%) Neutral Red solution (Sigma-Aldrich; Merck
KGaA, Darmstadt, Germany) was added to every well containing cells
to aid visualization and the plates were returned to the incubator
for an additional 24 h. On the 7th day postinoculation, the cells
were fixed with 100 µl 10% formal-saline (prepared by diluting 37%
formaldehyde with PBS, pH 7.4). Following fixation for a minimum of
30 min at room temperature, all liquid was removed from the plate
and each well was examined for cytopathic effect. For each
dilution, the number of wells that were positive for CPE was
scored. A Reed and Muench calculation was then performed to
determine the 50% infectious dose, which was then scaled up to give
a count of the TCID50 per ml (21).
The viral titers of Ad-GFP and Ad-HO-1 were 2.0×1011
pfu/ml and 2.5×1011 pfu/ml, respectively. Briefly, the
vector plasmids and ViraPower Package mixture (containing the pLP1,
pLP2 and pLP/VSVG plasmids) were cotransfected into 293T cells and
cultured at 37°C. At 48 h post transfection the viruses were
harvested and concentrated in PBS by ultracentrifugation (for 16 h
at 9,000 × g at 4°C) to 1.25×109 transducing units/ml.
The virus titer kit was purchased from MellGen Laboratories, Inc.
(Surrey, BC, Canada) and used according to the manufacturer's
protocol (21).
Animals and adenovirus infection
Based on the National Institutes of Health
Guidelines on Use of Laboratory Animals, all experiments were
conducted and approved by the Second Hospital of Shanxi Medical
University Committee on Animal Care (Shanxi, China).
Male Sprague-Dawley (SD) rats (n=48; weight, 240–280
g; age, 3–6 months) were purchased from the Experimental Animal
Center of the Fourth Military Medical University (Xi'an, China).
The rats were maintained in a specific pathogen free facility with
a constant humidity (55±5%) and temperature (22±2°C) and a 12 h
light/dark cycle with free access to food and water. Rats were
randomly divided into 4 groups (n=6/group): Sham group, vehicle
group, empty adenovirus vector (Ad) group and Ad-HO-1 transfection
group. Rats in the vehicle, Ad and Ad-HO-1 groups were respectively
injected with 20 µl saline, saline containing 1.25 µl empty vector
adenovirus or saline containing 1 µl recombinant HO-1 adenovirus
via the right lateral ventricle once daily for 3 days prior to
cerebral ischemia-reperfusion injury induction. The injection site
was referred to as the Paxinos and Watson rat brain stereotactic
atlas (10).
Transient focal cerebral
ischemia-reperfusion injury models
Rats in the vehicle group, Ad group and Ad-HO-1
group were anesthetized (3% isoflurane for induction and 1% for
maintenance) and the transient focal cerebral ischemia-reperfusion
injury models were induced via the MCAO method and intraluminal
suture technique (22,23). The rats in the sham group did not
receive MACO or intraluminal suture, however a sham operation was
performed. Blood flow was reduced to 87–90% in the ipsilateral
parietal cortex, which was considered as confirmation of successful
occlusion. During the experiment, a laser-Doppler flowmeter (Probe
407-1; Perimed AB, Järfälla, Sweden) was used for all groups to
monitor the blood flow at a maintained body temperature
(37.0±0.5°C). Following occlusion for 90 min, blood flow was
restored for 90 min to the ischemic region of brain and the
filament was removed from lumen. All rats recovered from anesthesia
prior to being returned to their cages.
Detection of GFP
Following a 24-h recovery period from MCAO, rat MCAO
models were anesthetized terminally with sodium pentobarbital (60
mg/kg; intraperitoneal; Sigma-Aldrich; Merck KGaA) and saline was
used for transcardial perfusion. Rat brains were harvested, and
sliced into 5 coronal sections (2-mm thick) from the frontal pole,
fixed in 4% formalin overnight at 30°C and stained with 0.5% w/v
triphenyltetrazolium chloride (TTC) dissolved in PBS for 15 min at
room temperature. Infarct areas of each slice were analyzed using
the SigmaScan Pro 5 Image Analysis software (Systat Software, Inc.,
Point Richmond, CA, USA). Direct GFP signals were digitally
photographed using an Olympus BX51 fluorescence microscope
(magnification, ×200; Olympus Corporation, Tokyo, Japan). A total
of 5 fields of view were randomly selected in each slice, 100 cells
were randomly selected in each, and the number of fluorescent cells
were counted. Subsequently, the efficiency of transfection was
calculated as follows: Efficiency of transfection=number of
positively stained cells/total number of cells ×100%, which was
automatically calculated and exported to Image-ProPlus 6.0 (Media
Cybernetics, Inc., Rockville, MD, USA) and GraphPad Prism 5.0
(GraphPad Software, Inc., La Jolla, CA, USA) for further
analysis.
Western blot analysis
Total protein was extracted from cortices of SD rats
in all groups using a radioimmunoprecipitation lysis buffer (Thermo
Fisher Scientific, Inc.). Protein concentration was determined
using the BCA Protein Assay kit (Pierce; Thermo Fisher Scientific,
Inc.) according to the manufacturer's protocol. Equal amounts of
protein (50 µg/lane) were resolved by 10% SDS-PAGE and transferred
to a polyvinylidene difluoride membrane (EMD Millipore, Billerica,
MA, USA). The western blot assays were performed with a
Mini-PROTEAN®TGX™ system (Bio-Rad
Laboratories, Inc., Hercules, CA, US). A 5% skimmed milk powder in
Tris-buffered saline with Tween-20 blocking solution was used for 1
h at room temperature. The membranes were incubated with β-actin
(cat. no. RB-9010-R7; 1:4,000; Invitrogen; Thermo Fisher
Scientific, Inc.) and anti-HO-1 (cat. no. sc-120745; 1:3,000; Santa
Cruz Biotechnology, Inc., Dallas, TX, USA) primary antibodies
overnight at 4°C. The membranes were incubated with horseradish
peroxidase-conjugated anti-mouse immunoglobulin G secondary
antibodies (cat. no. 7076; 1:5,000; Cell Signaling Technology,
Inc., Danvers, MA, USA) at room temperature for 1 h. The protein
bands were detected using the enhanced chemiluminescent method with
ECL™ Western Blotting Detection reagents (GE Healthcare, Chicago,
IL, USA) and subsequent autoradiography. The protein levels of the
bands were normalized against β-actin.
Assessment of neurological deficit
score (NDS)
Following a 24-h recovery period from MCAO, the NDSs
of rats were examined as described previously (18) with a modified scoring system. The
modified scoring system was adopted to determine the neurological
functional deficit at 4 h after the MCAO. Neurological deficit
score (NDS; 0–10% normal, 100% maximum deficit). The modified
neurological severity score (mNSS), a composite of motor, sensory,
reflex and balance tests was used to test the sensorimotor deficit.
The mNSS was graded on a scale of 0–18. A normal score was 0 and
the maximal deficit score was 18, 1 point was awarded for the
inability to perform the task or the lack of a tested reflex. (0,
no neurological deficits; 1, failure to extend right forepaw fully;
2, circling to right; 3, falling to right; 4, did not walk
spontaneously and has depressed levels of consciousness).
Volume of infarct regions
At 24 h following MCAO establishment, the tissues of
rat brains were sectioned as described above. Six samples from each
group were used in each experiment. The volume of infarct regions
was assessed using TTC staining in the dark overnight at 30°C, and
images of each section were captured using an Olympus BX51
fluorescence microscope (magnification, ×200). The infarct areas of
each slice were analyzed using the SigmaScan™ Pro V5.0
Image Analysis software (Systat Software, Inc., San Jose, CA, USA).
The injured tissues remained unstained by TTC, as staining did not
occur in areas where neuronal loss was observed. Therefore, the
unstained areas (infarct tissues) were examined and analyzed with
Photoshop software 7.0 (Adobe Systems, Inc., San Jose, CA, USA).
The sections were used to determine the volumes of infarct region.
For the ipsilateral hemisphere, the infarct regions of each brain
were calculated in mm3, which was corrected for swelling
in the same brain with translation on the percentage of
contralateral hemisphere as described previously (24).
Terminal
deoxynucleotidyl-transferase-mediated dUTP nick end (TUNEL)
staining
At 24 h following MCAO, brain tissue sections were
fixed in 4% formalin overnight at 30°C then stained with TUNEL
(Roche Diagnostics GmbH; Mannheim, Germany) at 37°C for 1 h. The
incorporated digoxigenin-conjugated nucleotides were detected using
a horseradish peroxidase-conjugated anti-digoxigenin antibodies and
3,3′-diaminobenzidine. The dehydrated sections were cleared in
xylene, mounted with Canada balsam and enclosed with coverslips.
The sections of brain tissues (n=6 per group) in contralateral
hemisphere and five fields of view were randomly selected for
counting and NDSs were determined. Subsequently, brain tissue
sections were dewaxed and rehydrated at 60°C for 2 h. These slides
were incubated for 30 min at room temperature in a 20 µg/ml
DNase-free proteinase K and rat terminal
deoxynucleotidyl-transferase (both Sigma-Aldrich; Merck KGaA)
reaction mix. Following rinsing with PBS 3 times for 15 min each
time, these sections were treated with streptavidin horseradish
peroxidase (1:200; Roche Diagnostics GmbH) at 37°C for 30 min and
positive signals were enhanced with diaminobenzidine (1:200; Roche
Diagnostics GmbH) at room temperature for 30 min. The tissue slide
was digitally photographed using an Olympus BX51 fluorescence
microscope (magnification, ×400). The apoptotic index (positively
stained cells count/total number of cells ×100%) was automatically
calculated and exported to GraphPad Prism 5.0 for further
analysis.
Activation of caspase-3
The neuronal activity of caspase-3 was examined
using a Caspase-3 Activity Assay kit (cat. no. CST 5723S; Cell
Signaling Technology Inc.) according to the manufacturer's
protocol. Brain tissues of the total suspension weighing 3 g were
homogenized for 2 min in Mcllwain's buffer, then the homogenates
were centrifuged at 3,000 g for 5 min at room temperature and the
supernatants were collected.
Statistical analysis
The normally distributed continuous variables were
indicated as the mean ± standard deviation. Statistical analysis
was performed using GraphPad Prism 5.0. Between groups, the
Student's t-test (for two group comparisons) or one-way analysis of
variance with Kruskal-Wallis post hoc tests (for multiple group
comparisons) were used to analyze and compare quantitative data.
The data that were abnormally distributed were analyzed between
groups with Kruskal-Wallis analysis of variance method. SPSS
software (version 18.0; SPSS, Inc., Chicago, IL, USA) was used to
analyze these statistical data. P<0.05 was considered to
indicate a statistically significant difference.
Results
Overexpression of HO-1 protects
against transient cerebral ischemia-reperfusion injury
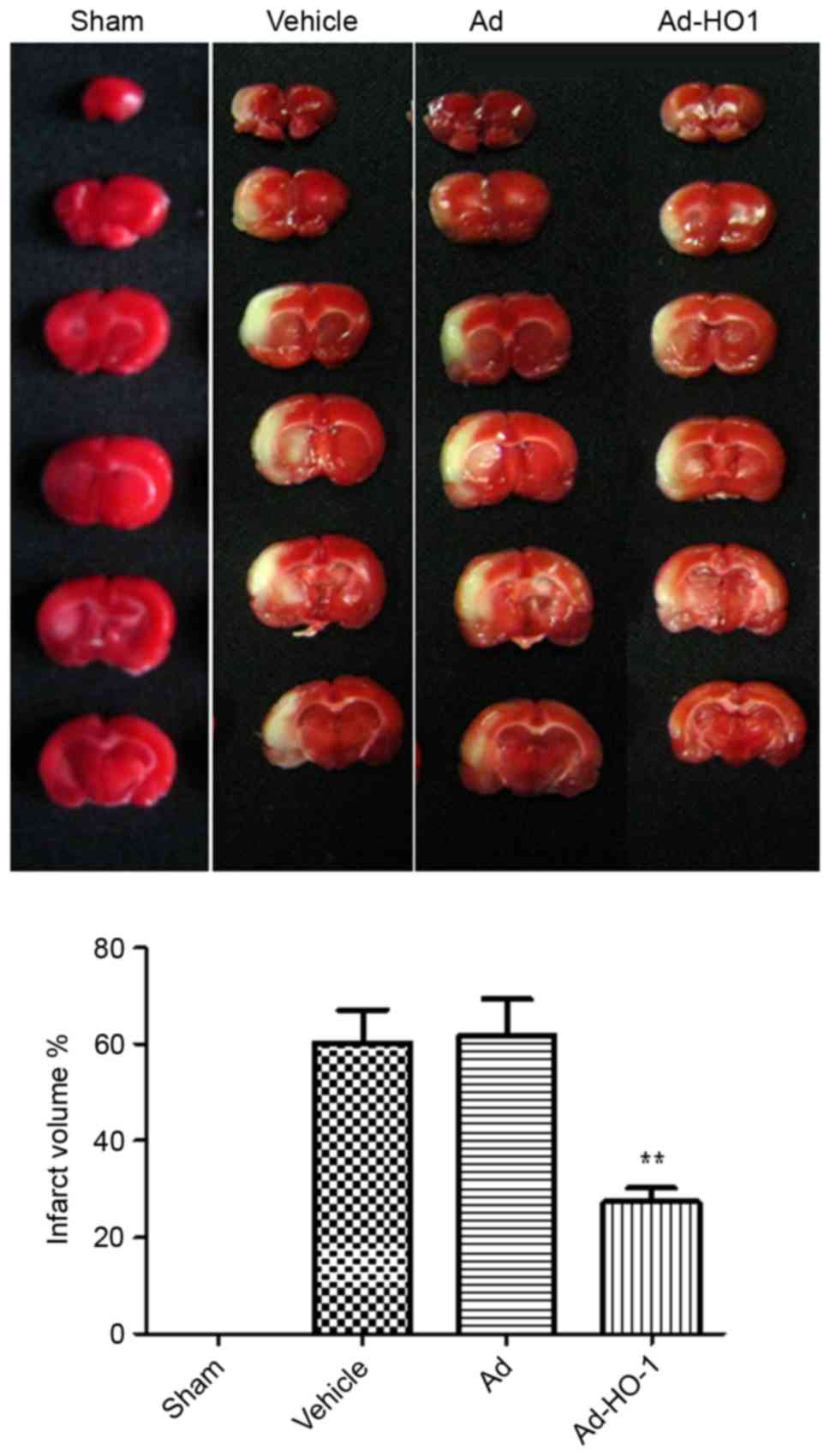
MCAO establishment was considered successful when
the blood flow of the rat models was decreased to 80–90% of the
baseline level in the core area. Following MCAO establishment, the
cerebral blood flow was not significantly different in the model
groups treated with vehicle or Ad (data not shown). The total
volume of infarction and infarction area of the representative
brain sections at 24 h following ischemia-reperfusion injury
establishment in each group are indicated in Fig. 1. The total volume of infarction in
the Ad-HO-1 group was 27.31±2.913%, which was significantly
decreased compared with those in the vehicle (60.36±6.750%;
P<0.01) and Ad groups (61.80±7.544%; P<0.01).
Overexpression of HO-1 with
recombinant adenovirus reverses post-ischemic neuronal apoptosis
induced by secondary brain damage in transient cerebral
ischemia-reperfusion injury
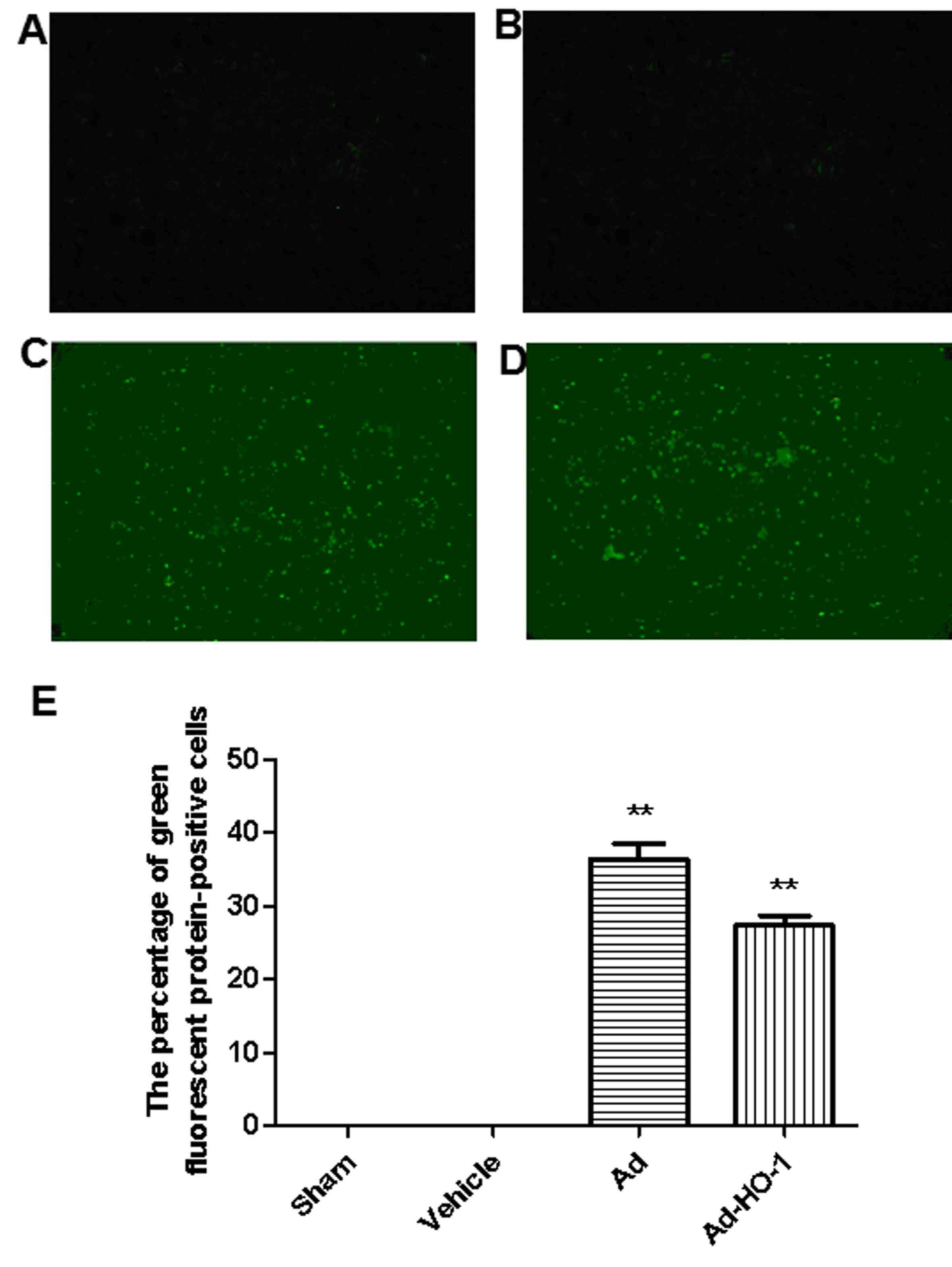
In sham and vehicle groups, limited GFP was detected
(Fig. 2A and B, respectively).
Conversely, expression of GFP was prevalent in the brain tissue
(hippocampus, striatum, cortex penumbra) when transfected with Ad
and Ad-HO-1 (Fig. 2C-E). The
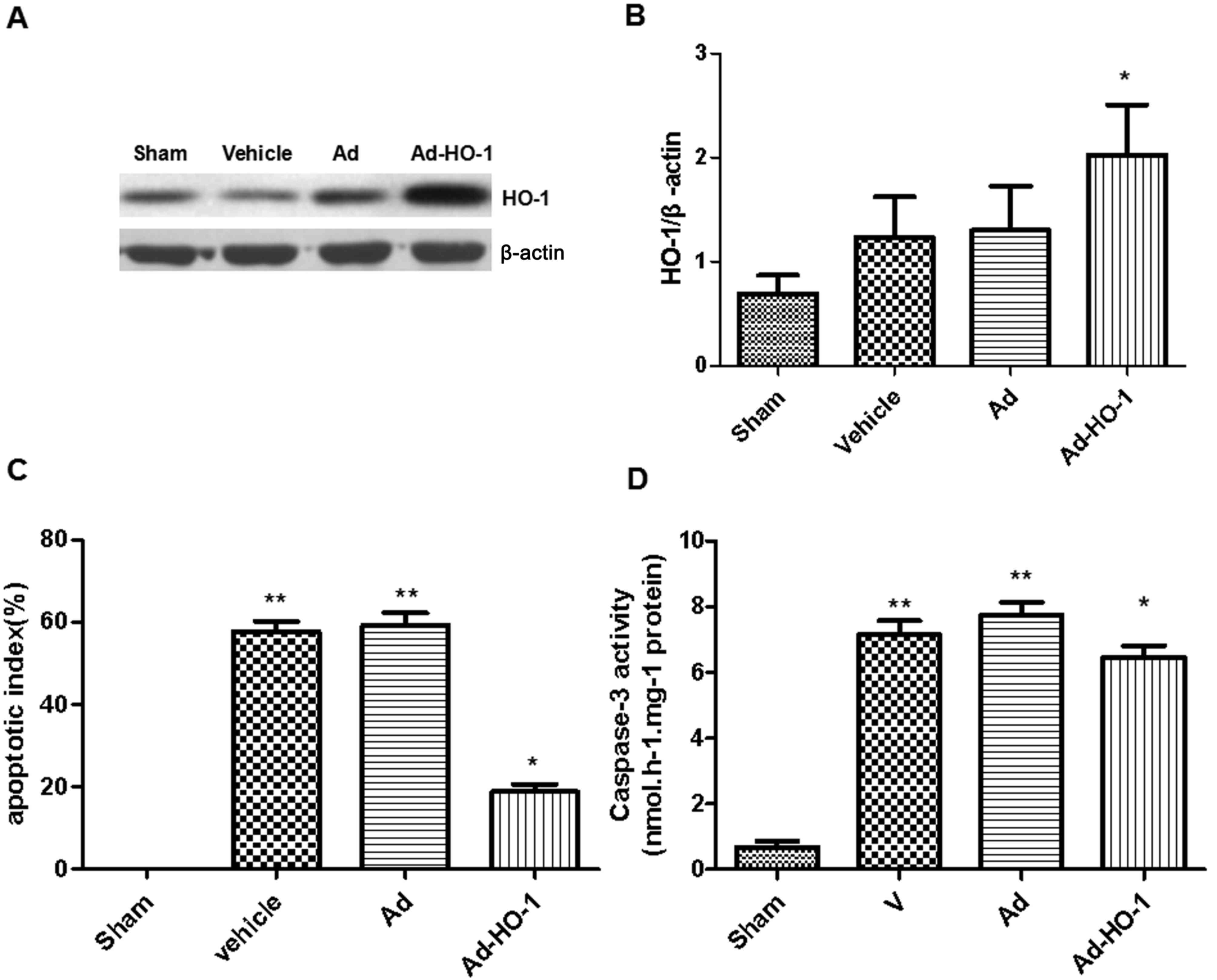
expression levels of HO-1 were assessed in each group using western
blot analysis (Fig. 3A). In HO
gene-treated rats, HO-1 expression levels were increased
significantly compared with the vehicle and Ad groups (P<0.05;
Fig. 3B). Furthermore, compared with
the sham group, transient cerebral ischemia-reperfusion injury
induced in the vehicle and Ad groups exhibited a significant
increase in apoptotic index score at 24 h following MCAO
(P<0.01; Fig. 3C). However,
overexpression of HO-1 significantly reversed this score
(18.28±0.18%) compared with the vehicle (57.68±2.11%) and Ad
(58.22±1.96%) groups with transient cerebral ischemia-reperfusion
injury (P<0.05).
The role of the caspase-dependent apoptosis pathway
in neuronal cell apoptosis was assessed based on caspase-3
activity. Neuronal apoptosis induced by ischemia was further
examined following transfection with the HO-1 gene to identify its
specific role. The vehicle and Ad groups were significantly
increased compared with the sham group (P<0.01). Caspase-3
activation in rat brains induced by cerebral ischemia-reperfusion
injury was significantly reduced following treatment with HO-1 gene
compared with the vehicle and Ad group (P<0.05; Fig. 3D). In the sham group, the percentage
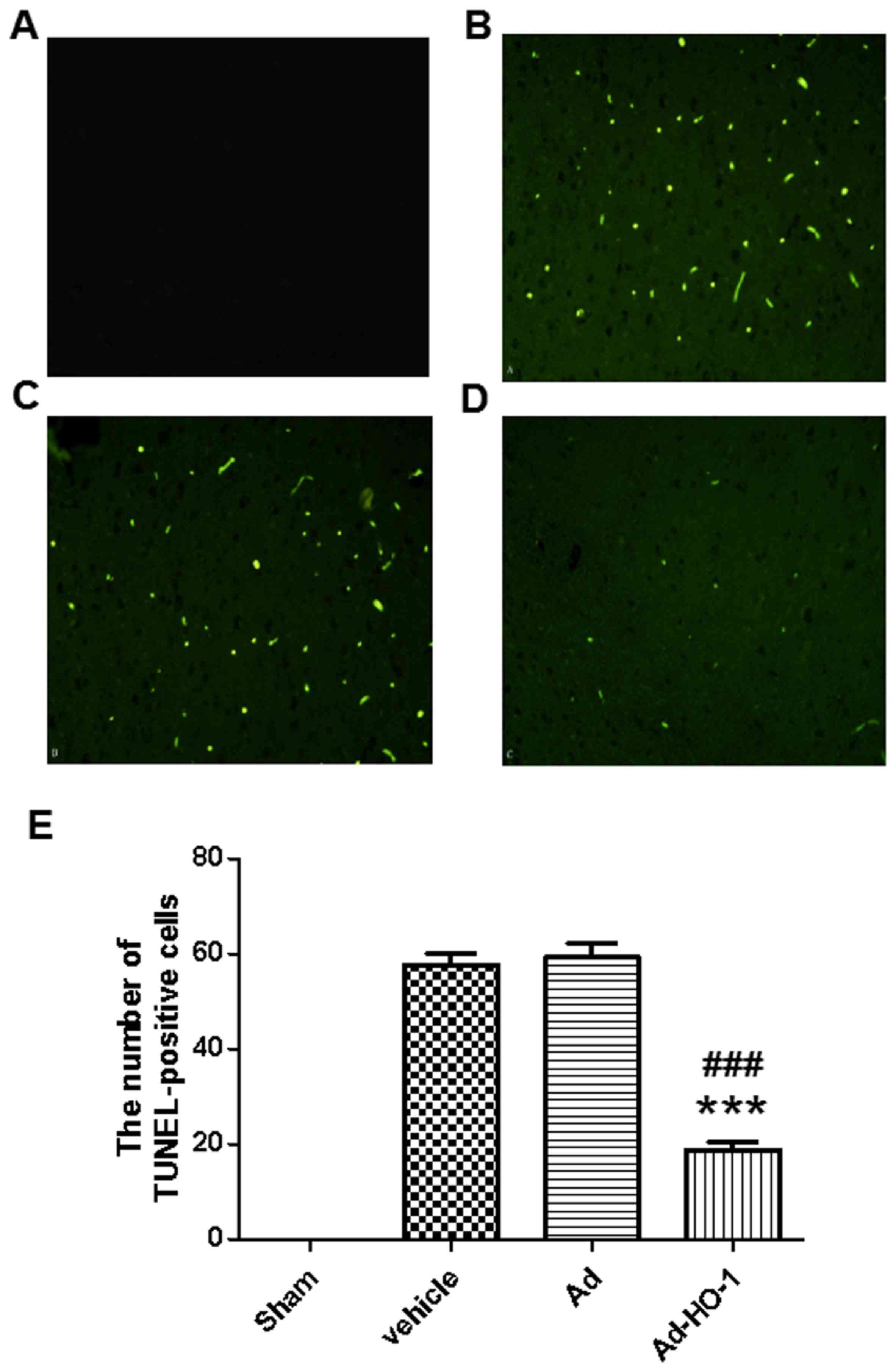
of detected TUNEL-positive cells was 0.1% (Fig. 4). Results demonstrated that
detectable neuronal apoptosis was not induced by surgical procedure
in the sham group. Conversely, in the tissues from brains of
ischemic-reperfused rats, the nuclei with TUNEL-positive stain were
prevalent. However, the number of TUNEL-positive cells was
significantly reduced following treatment with HO-1 gene
(18.83±1.82) compared with the Ad group (59.33±2.95; P<0.001)
(Fig. 4). These findings suggest
that HO-1 gene overexpression may have an inhibitive role in
post-ischemic neuronal apoptosis.
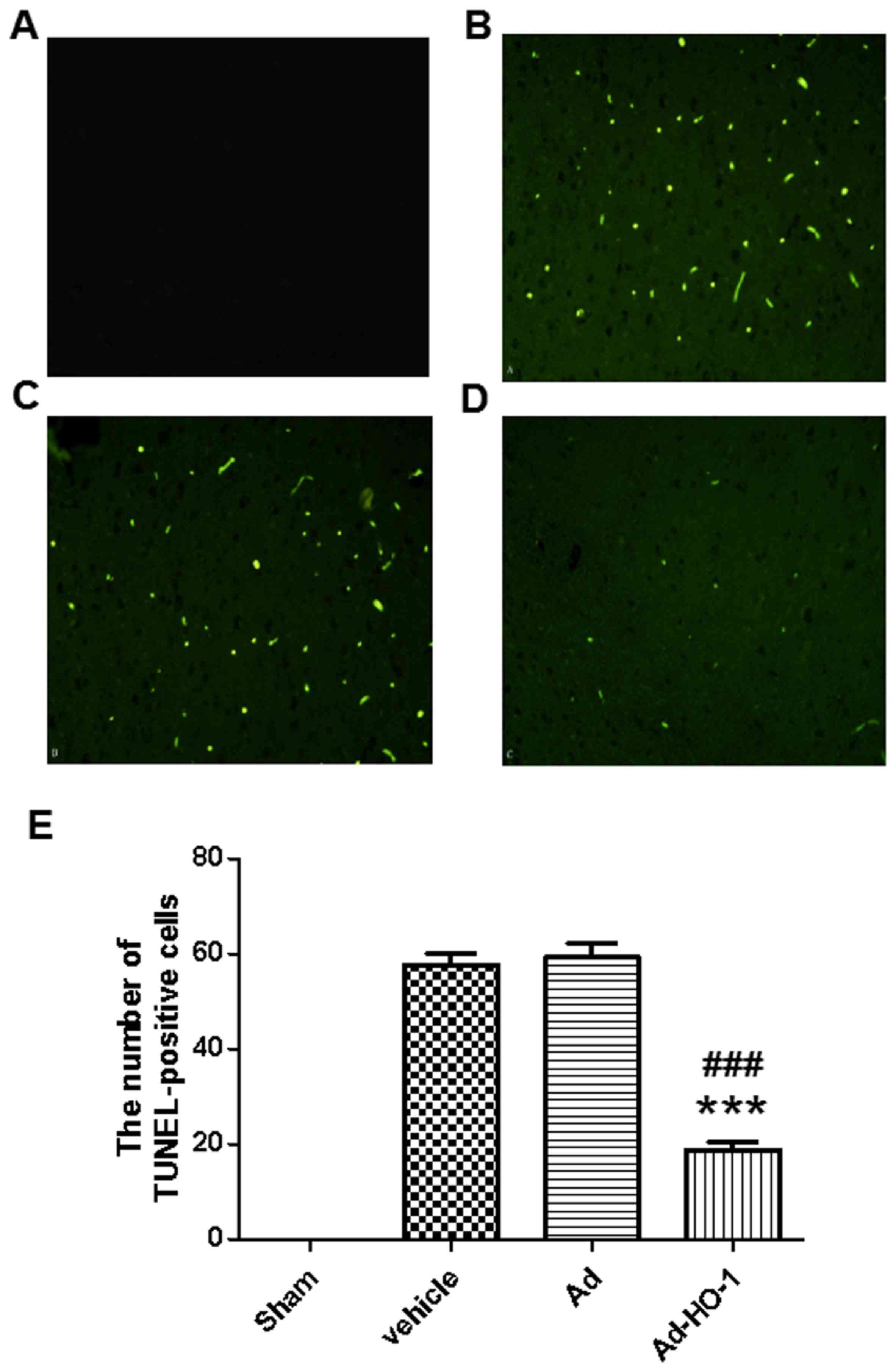 | Figure 4.TUNEL stain. In the brain tissues of
the sham group, the percentage of positive cells stained with TUNEL
was 0.1% (magnification, ×400). Conversely, in the tissues from
brains of ischemic-reperfused rats, TUNEL-positive nuclei were
prevalent. However, the number of TUNEL-positive cells was markedly
reduced following treatment with Ad-HO-1. (A) Sham group, (B)
Vehicle group, (C) Ad group and (D) Ad-HO-1 transfection group. (E)
The results were quantified. ***P<0.001 vs. the vehicle group
and ###P<0.001 vs. the Ad group. TUNEL, terminal
deoxynucleotidyl-transferase-mediated dUTP nick end staining, Ad,
empty adenovirus vector; HO-1, heme oxygenase-1; Ad-HO-1,
recombinant HO-1 adenovirus. |
Overexpression of HO-1 with
recombinant adenovirus reverses behavioral impairments induced by
secondary brain damage in transient cerebral ischemia-reperfusion
injury
Transient cerebral ischemia-reperfusion damage
markedly reduced the NDS (Fig. 5) at
24 h following MCAO. The neurological deficit scores were
significantly reduced in the MCAO groups (Vehicle and Ad group)
compared with the sham group (P<0.01). Overexpression of HO-1
significantly ameliorated the NDS (12.45±0.18%) compared with the
vehicle (9.82±0.17%) and Ad (9.96±0.09%) groups (P<0.001;
Fig. 5). These findings suggest that
overexpression of the HO-1 gene has a potential protective role
against secondary brain damage of the cerebral cortex induced by
transient cerebral ischemia-reperfusion injury, and may restore
neurological/behavioral impairment.
Discussion
Globally, stroke is one of the major causes of
long-term disability and death (25). Stroke is associated with notable
socioeconomic and clinical implications; furthermore, there is an
urgent requirement for effective therapies to treat stroke. In
practice, stroke is a pathological process involving multiple
factors that are typically associated with oxidative stress,
inflammation, calcium overload, brain edema and cell apoptosis
(26).
TIAs (transient ischemic attacks) are known as brief
ischemic episodes and have been studied for over two decades
(27,28). Tolerance to stroke may be induced by
TIAs through elevating the safety threshold of human brain tissue
(29). The potential molecular
mechanisms of neuroprotection induced by TIAs were unclear
(29). No clinically effective
therapies are currently available for treating stroke, despite a
number of studies based on experimental neuroprotective compounds
and animal models that have demonstrated promising results
(30,31). Investigation into the potential
molecular mechanisms associated with TIAs may aid the
identification of the novel targets for the prevention and
treatment for stroke (32).
HO-1 has a crucial role in the normal function of
neurons (33). In normal rats, the
expression of HO-1 is located at the neuronal nuclei of Purkinje or
hindbrain cells in the cerebellum (34). Furthermore, heat shock proteins,
trauma, bleeding and hypoxia may induce the expression of HO-1
(35). HO broadly participates in
the functional regulation of the heart, brain, lungs, liver,
kidneys and other tissue cells associated with anti-oxidative
stress injury (36). Previous
results have demonstrated that the increase in HO expression was
able to protect neuronal cells against ischemia through
anti-oxidative stress (37),
anti-apoptosis (38) and inhibition
of the inflammatory response (39),
thereby improving the cerebral microcirculation blood flow,
stabilizing the cell membrane and mitochondrial membrane, and
reducing brain edema (40). IPC
induces the expression of HO-1, which has an important role in
mediating the protection against transient and permanent brain
ischemia (41). Additionally,
following permanent ischemia, HO-1 may be the critical factor in
improving the NDS and reducing infarct volume of the brain
(42). In summary, HO-1 is the key
element in the protection against stroke, particularly in the
tolerance to stroke induced by IPC (3).
Conventional therapeutic strategies, which are
administered via a range of methods, including orally,
subcutaneously, intramuscularly and intravenously, are subject to
different degrees of blood-brain barrier obstacles, which makes the
outcome of an effective therapeutic response a challenge. As a
novel therapeutic strategy, brain stereotactic injection of
exogenous gene therapy for brain disease has received a lot of
interest in recent years (43).
In the present study, the recombinant adenovirus
vector of HO-1 was transfected into rats on the right lateral
ventricle and the HO-1 gene was injected directly into the brain.
The protein expression levels of HO-1 were continuously detected
for 3 days following transfection, and were significantly increased
in the cortex compared with the Ad group. However, protein
expression levels of HO-1 were decreased in the Ad group
transfected with adenovirus vector compared with the Ad-HO-1 group,
which demonstrated that the injection method of
intracerebroventricular administration was feasible and
effective.
The present results indicated that intraventricular
injection with Ad-HO-1 is an effective method to enhance the
expression of HO-1 and reverse brain injury induced by transient
focal cerebral ischemia-reperfusion injury in rats. Furthermore,
the present findings suggested that this approach may significantly
inhibit neuronal apoptosis and attenuate neurological behavioral
deficits. The results also demonstrated that rats that received
MCAO and pretreatment with HO-1 gene exhibited a significant
decrease in infarct volume compared with rats that were subjected
to MCAO and treated with vehicle or Ad. Furthermore, the present
findings indicated that intraventricular injection with the HO-1
gene significantly induced the expression of HO-1, which improved
neurological behavioral. This intervention method may lead notable
clinical benefits through decreasing the volume of infarct at a
later time point (at 24 h after reperfusion).
Similar to reports in previous studies (44,45), the
present study demonstrated that the expression of HO-1 increased
significantly in focal ischemic brains, which indicated that HO-1
may be a potential sensor for therapy in vitro. In the
present study, a common adenovirus vector was used for the control,
which did not affect the expression level of HO-1. However, in the
Ad-HO-1 group, expression was significantly increased. These
results demonstrated that the protective effects originated from
the successful expression of HO-1 introduced by transfection
compared with endogenous HO-1.
In conclusion, the HO-1 gene carried by adenovirus
may be effectively transfected into the brain tissue and expressed
stably in vivo. The programmed cell death in neuronal cells
following cerebral ischemia-reperfusion injury may be significantly
reversed by overexpression of HO-1. The results of the present
study suggested that HO-1 was able to mediate the effective
reduction of infarct volume, and provide neuroprotection against
transient cerebral ischemia-reperfusion induced brain damage.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 30600524).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XL performed all experiments analyzed and
interpreted the data. RG, WH and ZS performed some of the
experiments. GW, LW and YX were major contributors in writing the
manuscript and contributed to the conception and design of the
study. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by The Second Hospital of
Shanxi Medical University Committee on Animal Care (Shanxi,
China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Steiger HJ and Hanggi D: Ischaemic
preconditioning of the brain, mechanisms and applications. Acta
Neurochir (Wien). 149:1–10. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bergeron M, Ferriero DM, Vreman HJ,
Stevenson DK and Sharp FR: Hypoxia-ischemia, but not hypoxia alone,
induces the expression of heme oxygenase-1 (HSP32) in newborn rat
brain. J Cereb Blood Flow Metab. 17:647–658. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zeynalov E, Shah ZA, Li RC and Doré S:
Heme oxygenase 1 is associated with ischemic
preconditioning-induced protection against brain ischemia.
Neurobiol Dis. 35:264–269. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Poss KD and Tonegawa S: Heme oxygenase 1
is required for mammalian iron reutilization. Proc Natl Acad Sci
USA. 94:10919–10924. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ryter SW, Alam J and Choi AM: Heme
oxygenase-1/carbon monoxide: From basic science to therapeutic
applications. Physiol Rev. 86:583–650. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tenhunen R, Marver HS and Schmid R: The
enzymatic catabolism of hemoglobin: Stimulation of microsomal heme
oxygenase by hemin. J Lab Clin Med. 75:410–421. 1970.PubMed/NCBI
|
|
7
|
Kato H, Amersi F, Buelow R, Melinek J,
Coito AJ, Ke B, Busuttil RW and Kupiec-Weglinski JW: Heme
oxygenase-1 overexpression protects rat livers from
ischemia/reperfusion injury with extended cold preservation. Am J
Transplant. 1:121–128. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Panahian N, Yoshiura M and Maines MD:
Overexpression of heme oxygenase-1 is neuroprotective in a model of
permanent middle cerebral artery occlusion in transgenic rats. J
Neurochem. 72:1187–1203. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shen C, Cheng W, Yu P, Wang L, Zhou L,
Zeng L and Yang Q: Resveratrol pretreatment attenuates injury and
promotes proliferation of neural stem cells following
oxygen-glucose deprivation/reoxygenation by upregulating the
expression of Nrf2, HO-1 and NQO1 in vitro. Mol Med Rep.
14:3646–3654. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ryu MJ and Chung HS: Fucoidan reduces
oxidative stress by regulating the gene expression of HO-1 and
SOD-1 through the Nrf2/ERK signaling pathway in HaCaT cells. Mol
Med Rep. 14:3255–3260. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tulsulkar J, Glueck B, Hinds TD Jr and
Shah ZA: Ginkgo biloba extract prevents female mice from ischemic
brain damage and the mechanism is independent of the HO1/Wnt
pathway. Transl Stroke Res. 7:120–131. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sugiura S, Kitagawa K, Tanaka S, Todo K,
Omura-Matsuoka E, Sasaki T, Mabuchi T, Matsushita K, Yagita Y and
Hori M: Adenovirus-mediated gene transfer of heparin-binding
epidermal growth factor-like growth factor enhances neurogenesis
and angiogenesis after focal cerebral ischemia in rats. Stroke.
36:859–864. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shen F, Fan Y and Su H: Adeno-associated
viral vector-mediated hypoxia-regulated VEGF gene transfer promotes
angiogenesis following focal cerebral ischemia in rats. Gene Ther.
15:30–39. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Paxinos G, Watson CR and Emson PC:
AChE-stained horizontal sections of the rat brain in stereotaxic
coordinates. J Neurosci Methods. 3:129–149. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Longa EZ, Weinstein PR, Carlson S and
Cummins R: Reversible middle cerebral artery occlusion without
craniectomy in rats. Stroke. 20:84–91. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pantoni L, Bartolini L, Pracucci G and
Inzitari D: Interrater agreement on a simple neurological score in
rats. Stroke. 29:871–872. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Amantea D, Nappi G, Bernardi G, Bagetta G
and Corasaniti MT: Post-ischemic brain damage: Pathophysiology and
role of inflammatory mediators. FEBS J. 276:13–26. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Maines MD: Heme oxygenase: Function,
multiplicity, regulatory mechanisms and clinical applications.
FASEB J. 2:2557–2568. 1998. View Article : Google Scholar
|
|
19
|
Regan RF, Guo Y and Kumar N: Heme
oxygenase-1 induction protects murine cortical astrocytes from
hemoglobin toxicity. Neurosci Lett. 282:1–4. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
He TC, Zhou S, Costa LT, Yu J, Kinzler KW
and Vogelstein B: A simplified system for generating recombinant
adenoviruses. Proc Natl Acad Sci USA. 95:2509–2514. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sodt AJ, Venable RM, Lyman E and Pastor
RW: Nonadditive compositional curvature energetics of lipid
bilayers. Phys Rev Lett. 117:1381042016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shah ZA, Namiranian K, Klaus J, Kibler K
and Doré S: Use of an optimized transient occlusion of the middle
cerebral artery protocol for the mouse stroke model. J Stroke
Cerebrovasc Dis. 15:133–138. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zeynalov E, Nemoto M, Hurn PD, Koehler RC
and Bhardwaj A: Neuroprotective effect of selective kappa opioid
receptor agonist is gender specific and linked to reduced neuronal
nitric oxide. J Cereb Blood Flow Metab. 26:414–420. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dziennis S, Qin J, Shi L and Wang RK:
Macro-to-micro cortical vascular imaging underlies regional
differences in ischemic brain. Sci Rep. 5:100512015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chang L, Yin CY, Wu HY, Tian BB, Zhu Y,
Luo CX and Zhu DY: (+)-Borneol is neuroprotective against permanent
cerebral ischemia in rats by suppressing production of
proinflammatory cytokines. J Biomed Res. 31:306–314.
2017.PubMed/NCBI
|
|
26
|
Voelker R: Reducing stroke disability.
JAMA. 316:15382016. View Article : Google Scholar
|
|
27
|
Phan TG, Srikanth V, Cadilhac DA, Grimley
R, Donnan GA and Anderson CS: Better outcomes for hospitalized
patients with TIA when in stroke units: An observational study.
Neurology. 87:1745–1746. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Murry CE, Jennings RB and Reimer KA:
Preconditioning with ischemia: A delay of lethal cell injury in
ischemic myocardium. Circulation. 74:1124–1136. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wegener S, Gottschalk B, Jovanovic V, Knab
R, Fiebach JB, Schellinger PD, Kucinski T, Jungehülsing GJ,
Brunecker P, Müller B, et al: Transient ischemic attacks before
ischemic stroke: Preconditioning the human brain? A multicenter
magnetic resonance imaging study. Stroke. 35:616–621. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lip GY, Kongnakorn T, Phatak H, Kuznik A,
Lanitis T, Liu LZ, Iloeje U, Hernandez L and Dorian P:
Cost-effectiveness of apixaban versus other new oral anticoagulants
for stroke prevention in atrial fibrillation. Clin Ther.
36:192–210. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Cherry MG, Greenhalgh J, Osipenko L,
Venkatachalam M, Boland A, Dundar Y, Marsh K, Dickson R and Rees
DC: The clinical effectiveness and cost-effectiveness of primary
stroke prevention in children with sickle cell disease: A
systematic review and economic evaluation. Health Technol Assess.
16:1–129. 2012. View
Article : Google Scholar
|
|
32
|
Wilson D, Charidimou A, Ambler G, Fox ZV,
Gregoire S, Rayson P, Imaizumi T, Fluri F, Naka H, Horstmann S, et
al: Recurrent stroke risk and cerebral microbleed burden in
ischemic stroke and TIA: A meta-analysis. Neurology. 87:1501–1510.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Doan KV, Kinyua AW, Yang DJ, Ko CM, Moh
SH, Shong KE, Kim H, Park SK, Kim DH, Kim I, et al: FoxO1 in
dopaminergic neurons regulates energy homeostasis and targets
tyrosine hydroxylase. Nat Commun. 7:127332016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Li W, Jiang D, Li Q, Yao S, Sun X, Yang Y,
Meng Z and Liu W: Lipopolysaccharide-induced preconditioning
protects against traumatic spinal cord injury by upregulating Nrf2
expression in rats. Life Sci. 162:14–20. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lin R, Cai J, Kostuk EW, Rosenwasser R and
Iacovitti L: Fumarate modulates the immune/inflammatory response
and rescues nerve cells and neurological function after stroke in
rats. J Neuroinflammation. 13:2692016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hawrylycz M, Anastassiou C, Arkhipov A,
Berg J, Buice M, Cain N, Gouwens NW, Gratiy S, Iy Leszl-Ishiguro M,
Horvath B, Johnson RA, Johnson FK, Lenzsér G, Hermán P, Horváth EM
and Benyó Z: Influence of the heme-oxygenase pathway on
cerebrocortical blood flow. Neuroreport. 18:1193–1197. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen K, Gunter K and Maines MD: Neurons
overexpressing heme oxygenase-1 resist oxidative stress-mediated
cell death. J Neurochem. 75:304–313. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Leszl-Ishiguro M, Horvath B, Johnson RA,
Johnson FK, Lenzsér G, Hermán P, et al: Influence of the
heme-oxygenase pathway on cerebrocortical blood flow. Neuroreport.
18:1193–1197. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhen-Wei X, Jian-Le S, Qi Q, Wen-Wei Z,
Xue-Hong Z and Zi-Li Z: Heme oxygenase-1 improves the survival of
discordant cardiac xenograft through its anti-inflammatory and
anti-apoptotic effects. Pediatr Transplant. 11:850–859. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jumnongprakhon P, Govitrapong P, Tocharus
C and Tocharus J: Melatonin promotes blood-brain barrier integrity
in methamphetamine-induced inflammation in primary rat brain
microvascular endothelial cells. Brain Res. 1646:182–192. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhang X, Xiao Z, Yao J, Zhao G, Fa X and
Niu J: Participation of protein kinase C in the activation of Nrf2
signaling by ischemic preconditioning in the isolated rabbit heart.
Mol Cell Biochem. 372:169–179. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Mohammadi E and Bigdeli MR: Effects of
preconditioning with normobaric heperoxia on
Na+/Ca2+ exchanger in the rat brain.
Neuroscience. 237:277–284. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Gowing G, Svendsen S and Svendsen CN: Ex
vivo gene therapy for the treatment of neurological disorders. Prog
Brain Res. 230:99–132. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Yen TL, Chen RJ, Jayakumar T, Lu WJ, Hsieh
CY, Hsu MJ, Yang CH, Chang CC, Lin YK, Lin KH and Sheu JR:
Andrographolide stimulates p38 mitogen-activated protein
kinase-nuclear factor erythroid-2-related factor 2-heme oxygenase 1
signaling in primary cerebral endothelial cells for definite
protection against ischemic stroke in rats. Transl Res. 170:57–72.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Xue F, Huang JW, Ding PY, Zang HG, Kou ZJ,
Li T, Fan J, Peng ZW and Yan WJ: Nrf2/antioxidant defense pathway
is involved in the neuroprotective effects of Sirt1 against focal
cerebral ischemia in rats after hyperbaric oxygen preconditioning.
Behav Brain Res. 309:1–8. 2016. View Article : Google Scholar : PubMed/NCBI
|