Introduction
Recurrent patellar dislocation is most common in
adolescents, with a male:female ratio of ~1:5 (1–3).
Dislocation is triggered principally by trauma, which subsequently
induces medial patellar instability, which, when accompanied by
abnormal knee joint anatomy, may trigger repeated patellar
dislocation or subluxation during knee torsion, flexion, or
extension (4). The treatment of
recurrent patellar dislocation include conservative treatment and
operative treatment (5). Some
patients may receive satisfactory therapeutic effects through
conservative treatment including manual reduction, plaster
immobilization and functional rehabilitation (6). Muscle recovery instruments may also
strengthen the vastus medialis muscle and thus treat recurrent
patellar dislocation. However, surgery is still utilized for
patients with complex conditions (7). A number of surgical treatments are
available, but it is difficult for a single surgical method to
completely correct the complex pathology due to every case being
unique to each patient (8). Combined
surgical approaches are typically employed to restore the soft
tissue balance of the patella, to correct abnormal anatomical
structures and to restore stable patellar biomechanics (9). However, it is difficult to completely
restore a normal anatomical relationship and stable mechanical
balance via surgery alone. The principal aim of surgery is to
restore the patellar trajectory, affording robust medial support
and preventing further dislocation via reconstruction of the medial
patellofemoral ligament (MPFL) (10). Thereby, It's more beneficial to later
rehabilitation exercise. Sallay et al (11) reported that ~94% patients with
patellar dislocation have a torn medial patellofemoral ligament. So
MPFL reconstruction is important when treating recurrent patellar
dislocation (12). The present study
details the use of intraoperative arthroscopy to explore and repair
patellofemoral joint cartilage injuries. In this procedure, the
lateral collateral ligament is released and MPFL is positioned at
the femoral isometric point by C-arm fluoroscopy (Siremobil Compact
L; Siemens, Germany) (13). The MPFL
was then reconstructed using the autologous semitendinosus muscle
tendon.
Materials and methods
Materials
The picture archiving and communication system
(PACS) was obtained from (Tianjian Technology Group, Beijing,
China) and was utilized to collect the image data of patients and
calculate parameters including congruence angle, lateral
patellofemoral angle and the Insall-Salvati index (14). The Smith and Nephew model 3.5 line
anchors (Smith & Nephew, Watford, UK) were used to
double-anchor the medial patellofemoral margin. C-arm fluoroscopy
(SIREMOBIL Compact L; Siemens AG, Munich, Germany) was employed to
position the MPFL at the femoral isometric point during
surgery.
Data and methods
Data was reviewed from 52 patients who underwent
arthroscopic surgery on one knee, during which C-arm fluoroscopy
was employed to position the MPFL at the femoral isometric point
and the MPFL was reconstructed using the autologous semitendinosus
muscle tendon. Between October 2013 and March 2017, a total of 27
males and 25 females aged 16–47 years (21.90±6.78 years) were
treated in the third department of Orthopedics, Hospital of
Traditional Chinese Medicine of Xinjiang Medical University
(Urumqi, China). Patients had experienced dislocations on 2–60
occasions (7.75±10.27). Re-dislocations had developed in ≤6 weeks
in 16 cases, between 6 weeks and 6 months in 7 cases, between 6
months and 3 years in 15 cases and after 3 years in 14 cases. The
initial dislocation was typically associated with knee movement,
with examples including skipping, falling, playing basketball,
crouching and rising to full height. The principal clinical
manifestations of 9 patients with primary dislocations were knee
pain or instability, or leg weakness. Patients wore plasters or
knee braces from 1 week-2 months. All patients were positive on the
patella apprehension test (14), 30
exhibited different extents of femoral head four-muscle atrophy and
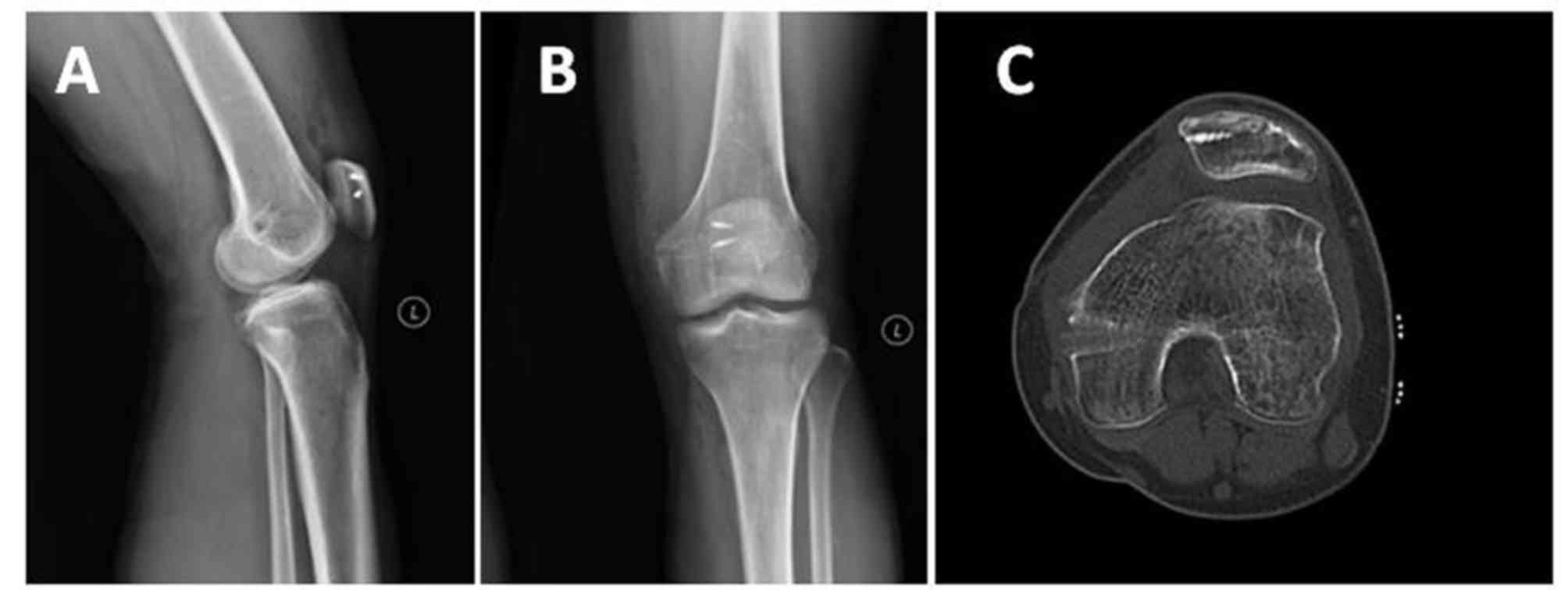
27 were positive on the knee patellar tilt test (15). X-ray results of a representative case
of dislocation are presented in Fig.
1.
As recommended by Beaconsfield et al
(16), X-ray measurements of the
patellar axis were performed at 30° of knee joint flexion. PACS was
utilized to collect images and calculate the following parameters:
i) The congruence angle (CA; between the pulley angle bisector and
center of the patellar central ridge at the lowest point of the
pulley; normal, −8±6°); ii) the lateral patellofemoral angle (AC;
between the vertex of the femoral condyle and the extension of the
lateral surface of the patella, typically increasing toward the
exterior); iii) the patellar removal rate (LPE) (17), measured vertically to the outer
condylar apex (the ratio of the transverse diameter of the lateral
patella to that of the patella; normal, <0.5); and iv) the
Insall-Salvati index [the ratio of the length of the patellar
tendon (LT) to the length of the patella (LP); normal, <1.0].
Computed tomography (CT) was used to measure the length of the
tibial tuberosity trochlear groove (TT-TG; normal, <15 mm) and
the Q angle (that between the tension line of the four biceps
muscles and the lengthening line of the patellar tendon at the
patellar center; normal values, 8–10° in males and 15±5° in
females). All normal ranges are obtained from (16).
Inclusion criteria were as follows: i) Recurrent
patellar dislocation; and ii) epiphyseal plate closure or expiry of
the peak growth period.
Exclusion criteria were as follows: i) Serious
femoral condylar dysplasia (tilt angle ≤9°) with accompanying knee
valgus deformity; ii) a significantly elevated patella
(Insall-Salvati index ≥1.2); and/or iii) significant knee
osteoarthritic changes [Kellgren-Lawrance X-ray grade ≥III
(18)].
The present study was approved by the Ethics
Committee of the Hospital of Traditional Chinese Medicine of
Xinjiang Medical University (Urumqi, China) and all patients
provided written, informed consent prior to their inclusion.
Surgical methods
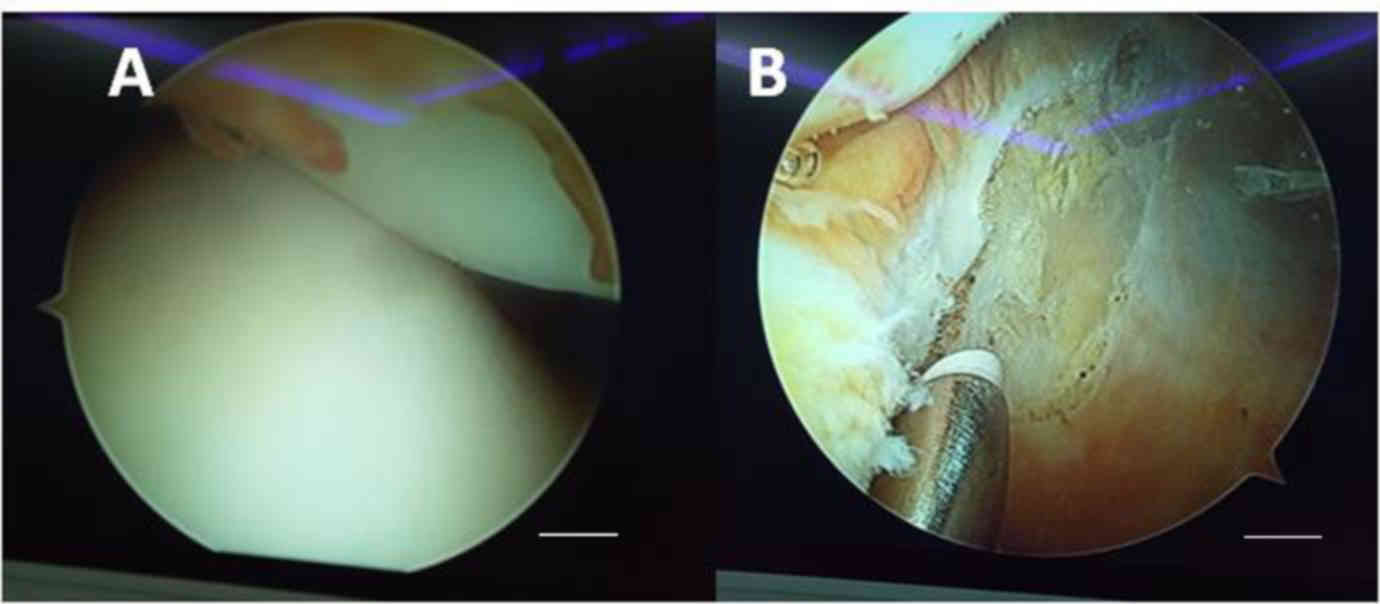
Arthroscopic exploration and loosening
of the lateral retinaculum
All patients underwent arthroscopic exploration
prior to ligament reconstruction. Synovial congestion and synovitis
performance was exhibited in 2 patients and osteochondral loose
bodies and synovitis performance in 12 patients. Patients with
Patellofemoral joint cartilage injuries were scored according to
Outerbridge (17) and were as
follows: 14 of grade II, 5 of grade III, and 3 of grade IV. A total
of 3 instances of patellar cartilage fracture were encountered, of
which 1 (a large fracture) was treated via open reduction and
suturing. Other patients' joint cartilage was normal and did not
exhibit synovitis performance. Arthroscopy, performed 6 weeks
later, revealed that the fracture had healed well. Fracture of the
external condylar cartilage was exhibited by 1 case. The synovial
cavity and free body of the joint cavity were arthroscopically
cleared with simultaneous dressing and reconstruction of the
damaged cartilage. In patients with grade II or grade III, local
plasma knife gasification was used to repair the cartilage surface.
Patients with grade IV injuries were treated via microfracture.
Intra-operative reconstruction of the MPFL was performed to treat 3
patients who exhibited patellar lateral avulsion fractures. A total
of 46 patients required arthroscopic release of the lateral
retinaculum. Patient histories, physical examination data and
intraoperative measurements of the patellar trajectory and impact
were evaluated. If the pre-operative history was short (<6
weeks), the patellar range of motion normal, the patellar tilt
negative, no obvious contracture of the lateral patellar
retinaculum was apparent, the lateral patellar retinaculum was not
loosened. Conversely, if the lateral patellar retinaculum was
loosened by ~1 cm when the knee was stretched (over regions on
either side of the upper and lower patellar poles), the retinaculum
was loosened to the level of the deep fascia. Patellar dislocation
had a marked improvement, which was assessed using arthoscopy
(Fig. 2).
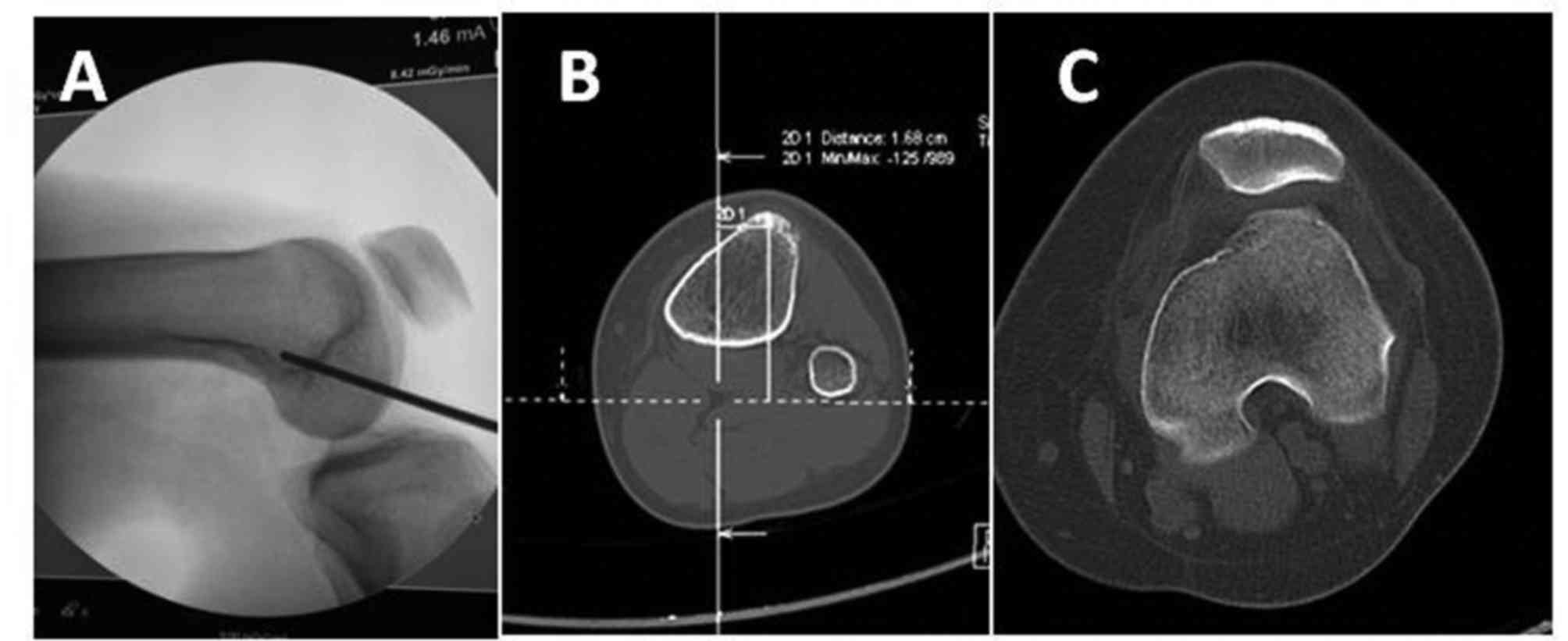
Reconstruction of the MPFL
To reconstruct the MPFL, the procedure of Schöttle
et al (19) was followed.
Initially, the MPFL was located at the medial femoral condyle and
an isometric view was established using C-arm fluoroscopy during
the surgery (Siremobil Compact L; Siemens AG, Munich, Germany;
Fig. 3A). The medial and lateral
femoral condyles were then overlapped and fixed with Kirschner
wire, commencing in the interior of this region, and progressing
toward the exterior. At the pes anserinus attachment point, an
outwardly extending 2.5-cm-long oblique incision was created in the
skin and subcutaneous tissue of the medial tibial tubercle to
reveal the semitendinosus muscle tendon, which was removed in a
standard manner, with both ends then sutured to allow measurement
of the diameter of the braided end of the graft. This allowed
evaluation of the graft whip structure and to measure the
pre-reserve. Creation of a 2-cm longitudinal incision in the inner
edge of the patella. The osteophyte in the inner edge of patella
was removed using a rongeur and a bony groove was formed. The
groove was positioned between the articular surfaces and the cortex
of bone, the size of which ranged from the patellar midpoint to the
superior border of patellar. Two 3.5-grade studs (Smith &
Nephew) were horizontally placed at either end of the fresh bone
surface and the semitendinosus tendon was folded around the bone,
pulled through the bone groove, and sutured. The skin and
subcutaneous tissue were cut (incision lengths, ~1 cm) in the
regions of the medial femur using a Kirschner wire. Blunt
dissection to the bone surface followed and a femoral tunnel was
drilled by reference to the diameter of the braided end of the
graft, creating a shallow soft tissue channel. The woven ends of
the two tendons were pulled along the soft tissue of the femoral
tunnel. The tendon was flexed and contracted under tension to
observe patellar motility and the anatomy of the patellofemoral
joint. On application of external stress to the patella, it was
ensured that the passive sliding distance was 25–50% of the
patellar width. When the tendon attained physiological tension, it
was fixed in the medial femoral tunnel using a 7-mm-diameter
interface squeeze screw (Smith & Nephew).
Transposition of the tibial
tubercle
In accordance with the Weber et al (20), 2 patients with pre-operative TT-TGs
>20 mm and Q angles >20° underwent proximal tibial tubercular
transposition using the Fulkerson method (21,22)
(Fig. 3B and C). The distal and
lateral oblique incisions were extended by ~3 cm, exposing the
tibial nodule and distal 6 cm of the long tibial crest, and oblique
(30°) osteotomy was performed, commencing at the medial margin of
the tibial tubercle and progressing to the lateral nodule, creating
a wedge-shaped osteotomic block 6 cm in length and 7 mm in
thickness. The block was moved 8–10 mm up along the osteotomy face,
and the movable tibial tubercle temporarily fixed with two
4.5-grade hollow nail guide pins. The patellar trajectory was
assessed via knee flexion and, if the surgeon judged it
satisfactory, two 4.5-grade cannulated screws were used to fasten
the nodules.
Post-operative treatment
Drainage tubes were not placed, but all operative
sites were pressure-bandaged for 3 days and the sutures removed
during the next 14 days depending on healing status. The knee joint
was fixed for 3 months. At 2 days following surgery, ankle pumping
and four-head muscle and straight leg elevation exercises were
commenced. Knee stretch exercises while wearing knee braces were
gradually introduced following another week, as were weight-bearing
walking and flexion and extension exercises while in bed. Within 2
weeks of surgery, ≥90° of movement was attained. After 6 weeks,
full weight-bearing-supported walking and progressive resistance
training were introduced, and, after 12 weeks, the knee joint
restraints were removed, and knee joint activity and muscle
strength training were commenced. Simple uniform motion was
permitted after 6 months and full resumption of sporting activities
after 1 year.
Follow-up and statistical
analysis
All patients were followed up in the orthopaedic
clinic of the Hospital of Traditional Chinese Medicine of Xinjiang
Medical University at 1, 3, 6 and 12 months after surgery, and then
via telephone or in the clinic every 6 months thereafter. Each
follow-up evaluation explored symptom improvement, included
physical and radiological examinations, and evaluated the
International Knee Documentation Committee (IKDC), Lysholm Knee
Function and Tegner Knee Movement scores (23). Data were analyzed using SPSS 19.0
(IBM Corp., Armonk, NY, USA). Pre- and post-operative data were
compared using the paired t-test. P<0.05 was considered to
indicate a statistically significant difference.
Results
All patients were followed up for 1–40 months
(21±6.24 months). No patellar dislocation or fracture occurred
during follow-up. The fear test was negative and the patellar tilt
was essentially symmetrical. CA, AC and LPE at the last follow-up
differed significantly from the pre-operative values. The IKDC and
Lysholm scores also improved significantly following surgery
(Table I). As presented in
post-operative X-rays of the knee joint (Fig. 4A and B) and CT of the lateral knee
joint (Fig. 4C), the anchor position
was good, the tunnel was located at the isometric point and the
patellar position was appropriate.
 | Table I.Radiographic and function assessment
prior to and following surgical protocols. |
Table I.
Radiographic and function assessment
prior to and following surgical protocols.
| Index | Pre-operative | Post-operative | T-value | P-value |
|---|
| CA | 9.67°±6.93° | 0.22°±4.23° | 10.15 | <0.001 |
| AC | −0.40°±6.65° | 3.44°±1.30° | −4.09 | <0.001 |
| LPE | 0.70±0.28 | 0.36±0.14 | 7.49 | <0.001 |
| IKDC score | 56.98±5.72 | 87.84±3.74 | −33.24 | <0.001 |
| Lysholm score | 47.88±7.78 | 87.48±3.35 | −33.69 | <0.001 |
Discussion
The typical patellar dislocation case is a
diminutive young female exhibiting poor patellar alignment and
ligament relaxation (1). Acute
dislocation is triggered principally by direct trauma; dislocation
develops during the application of knee torsion stress over the
line of abnormality. The majority of patellar dislocations are
lateral (24,25). The MPFL is the most important
ligament in terms of medial patellar strength (50–60% of all the
strength that is imparted) (26–28). The
MPFL maintains the patellar trajectory and minimizes dislocation.
Therefore, MPLF reconstruction is essential to restore
patellofemoral joint stability.
The treatment success rate when recurrent patellar
dislocations are supported by only simple lateral support bands is
68% and most scholars do not advocate that recurrent dislocations
should be treated by simply loosening the lateral supports
(2). Lind et al (29) previously demonstrated that
reconstruction of the medial patellar ligament afforded
significantly improved results than simple repair. Schöttle et
al (30) recommended the use of
double anchors to fix the patellar tendon, double-beam MPFL
reconstruction and placement of interfacial extruded screws on the
femoral side. Typically, the femoral condyle is located visually,
and the adductor node and internal condyle serve as anatomical
landmarks during MPFL reconstruction. In 2 of the present patients,
the use of this approach was associated with larger internal
condylar incisions in the femoral shaft and increased trauma. The
optimal location may be affected by the position of the internal
adductor node and extent of development of the internal femoral
condyle. Schöttle et al (19)
suggested that the knee be viewed laterally and that the medial and
lateral femoral condyles should be overlapped by reference to the
inflection points of the femoral condyle, the posterior cortex, and
the final extension of the Blumensaat line. A perpendicular should
be drawn to the tangential extension of the posterior femoral
cortex, 1.3 mm in front of the cortex, distal to the end of the
femoral condyle and 2.5 mm toward the back of the cortex. The
proximal 3-mm position of the Blumensaat line at the end of the
vertical point thus created defines the length of the MPFL. Prior
to 2013, patients with recurrent patellar dislocations at our
hospital were treated via open, descending, medial patellar
ligament overlap suturing, lateral patellar thigh support, and MPFL
loosening or reconstruction. The ‘saddle zone’ between the proximal
femur and the femoral condyle was used to reconstruct the femoral
MPFL. After surgery, X-rays revealed the MPFL at the femoral side
of the tunnel. During follow-up, no instances of patellar
re-dislocation were observed, but in many cases the MPFL was
observed to relax, which is associated with patellar instability.
Medial patellar support was required to treat tenderness and other
manifestations. More recently, developments in sports medicine have
encouraged the treatment of recurrent dislocations via arthroscopic
exploration and cleaning, loosening of the lateral support bands,
C-arm fluoroscopy to locate the femoral condyle and other long
points, autogenous half-tendon muscle double-beam reconstruction of
the MPFL, pre-operative positioning of the knee joint in the
lateral position, axial patellar positioning at 30° and 45° during
fully erect standing, and the use of knee CT and magnetic resonance
imaging to determine whether anatomical abnormalities are evident
(with or without injury to the articular cartilage or formation of
free bodies, and with or without merger of other ligaments and
meniscal injury). After surgery, data obtained in the lateral
position and the patellar axis, and knee CT data were reviewed.
Arthroscopy was useful to define the trajectory of patellar
activity, to clear inflamed synovial tissue, to detect injuries to
the anterior and posterior cruciate ligaments and the menisci, to
clear the articular cavity of free bodies, and to assess damage to
the articular surface. Radiofrequency catheter ablation and/or
microfracture treatments were performed depending on the extent of
contracture of the lateral support band both before and during the
operation; the support was relieved via appropriate arthroscopy.
The choice between an open operation and arthroscopic loosening
remains controversial. Either treatment should permit maximal
loosening, avoiding residual contracture stress that may trigger
symptoms of patellofemoral arthritis. The use of hamstring muscle
to restore tensile strength to the MPFL ligament afforded a
strength ~10-fold that of the normal MPFL, significantly affecting
the patellofemoral joint. In addition, in patients with basic
anatomical abnormalities, simple lateral support combined with
loosening and medial MPFL reconstruction may not completely
eliminate degenerative patellar joint degeneration. Furthermore,
distal rearrangement may be required. At present, Elmslie-Trillat
surgery (31) and Fulkerson
osteotomy (21,22) are used widely. TT-TG >20 mm and Q
angle >20° indicates that distal rearrangement is required.
Fulkerson osteotomy is typically used to treat non-professional
athletes exhibiting severe patellofemoral degeneration (22). The recent cadaveric study by Tanaka
et al (32) demonstrated that
the MPFL was structurally large and narrow-sided on the patellar
side, and that the MPFL patellar side-stop was typically located
proximal to the end of the patellar four-headed muscle. The patella
occupied ~66% of the relevant area and the four-headed muscle
segment occupied ~33%. Double anchoring and the placement of
patellar stops restricting transplanted tendon movement to ~2.0 cm
ensure effective femoral tendon bone healing, approximating
anatomical reconstruction of the MPFL. The C-arm perspective of the
femoral side ensures good patellar trajectory and avoids the
‘rubber band’ MPFL effect after reconstruction, mitigating the risk
of patellofemoral arthritis. The medial femoral incision length was
~1 cm in length, the lateral support band was relieved by
arthroscopy and the incisional length was only ~0.5 cm in the
bilateral genus eye. Therefore, the procedure was less invasive
than open surgery. Two-beam anatomical reconstruction of the MPFL
via autogenous half-tendon anastomosis is facilitated when the
patellar tunnel method (accompanied by double-anchor nail fixation)
is employed, associated with (at least) enhanced short-term
curative effects (30). The
long-term effects require further study.
In conclusion, in the short term, recurrent patellar
dislocation treatment via knee arthroscopy combined with C-arm
fluoroscopy and reconstruction of the medial patellofemoral
ligament was effective. The procedure benefits the patients by
reducing pain and recovery time. This surgery may provide a new
direction for future clinical treatment of recurrent patellar
dislocation.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author
Authors' contributions
LL and HW operated on patients. YH, YS and HZ
completed the patient follow-up. XW analyzed the relevant data. LL,
HW and YH were major contributors in writing the manuscript and all
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Hospital of Traditional Chinese Medicine of
Xinjiang Medical University (Urumqi, China) and all patients
provided written, informed consent prior to their inclusion.
Consent for publication
All patients provided written, informed consent
prior to their inclusion.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fithian DC, Paxton EW, Stone ML, Silva P,
Davis DK, Elias DA and White LM: Epidemiology and natural history
of acute patellar dislocation. Am J Sports Med. 32:1114–1121. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Du H, Tian XX, Guo FQ, Li XM, Ji TT, Li B
and Li TS: Evaluation of different surgical methods in treating
recurrent patella dislocation after three-dimensional
reconstruction. Int Orthop. 41:2517–2524. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gao B, Shi Y and Zhang F: Pediatric
patellar dislocation: a review. Minerva Pediatr. Mar 27–2017.(Epub
ahead of print).
|
|
4
|
Chang CB, Shetty GM, Lee JS, Kim YC, Kwon
JH and Nha KW: A combined closing wedge distal femoral osteotomy
and medial reefing procedure for recurrent patellar dislocation
with Genu Valgum. Yonsei Med J. 58:878–883. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Saccomanno MF, Sircana G, Fodale M, Donati
F and Milano G: Surgical versus conservative treatment of primary
patellar dislocation. A systematic review and meta-analysis. Int
Orthop. 40:2277–2287. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cao WQ, Yang ZQ, Wang G, Men YX and Cheng
XY: Current therapy progress on the recurrent patellar dislocation.
Zhongguo Gu Shang. 30:282–286. 2017.(In Chinese). PubMed/NCBI
|
|
7
|
Zhao ZD, Li PC and Wei XC: Current status
and expectations in the surgical treatment of recurrent lateral
patellar dislocation. Zhongguo Gu Shang. 30:982–985. 2017.(In
Chinese). PubMed/NCBI
|
|
8
|
Chen S, Zhou Y, Qian Q, Wu Y, Fu P and Wu
H: Arthroscopic lateral retinacular release, medial retinacular
plication and partial medial tibial tubercle transfer for recurrent
patellar dislocation. Int J Surg. 44:43–48. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gaweda K, Walawski J, Wegłowski R, Drelich
M and Mazurkiewicz T: Early results of one-stage knee extensor
realignment and autologous osteochondral grafting. Int Orthop.
30:39–42. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chouteau J: Surgical reconstruction of the
medial patellofemoral ligament. Orthop Traumatol Surg Res. 102 1
Suppl:S189–S194. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sallay PI, Poggi J, Speer KP and Garrett
WE: Acute dislocation of the patella. A correlative pathoanatomic
study. Am J Sports Med. 24:52–60. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hinckel BB, Gobbi RG, Kaleka CC, Camanho
GL and Arendt EA: Medial patellotibial ligament and medial
patellomeniscal ligament: Anatomy, imaging, biomechanics, and
clinical review. Knee Surg Sports Traumatol Arthrosc. 26:685–696.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ziegler CG, Fulkerson JP and Edgar C:
Radiographic reference points are inaccurate with and without a
true lateral radiograph: The importance of anatomy in medial
patellofemoral ligament reconstruction. Am J Sports Med.
44:133–142. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dimon JH III: Apprehension test for
subluxation of the patella. Clin Orthop Relat Res. 39:1974.
|
|
15
|
Grawe B, Schroeder AJ, Kakazu R and Messer
MS: Lateral collateral ligament injury about the knee: Anatomy,
evaluation, and management. J Am Acad Orthop Surg 2018. Feb
13–2018.(Epub ahead of print). View Article : Google Scholar
|
|
16
|
Beaconsfield T, Pintore E, Maffulli N and
Petri GJ: Radiological measurements in patellofemoral disorders. A
review. Clin Orthop Relat Res. 18–28. 1994.PubMed/NCBI
|
|
17
|
Duchman K, Mellecker C, El-Hattab AY and
Albright JP: Case report: Quantitative MRI of tibial tubercle
transfer during active quadriceps contraction. Clin Orthop Relat
Res. 469:294–299. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kellgren JH and Lawrence JS: Radiological
assessment of osteo-arthrosis. Ann Rheum Dis. 16:494–502. 1957.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schöttle PB, Schmeling A, Rosenstiel N and
Weiler A: Radiographic landmarks for femoral tunnel placement in
medial patellofemoral ligament reconstruction. Am J Sports Med.
35:801–804. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Weber AE, Nathani A, Dines JS, Allen AA,
Shubin-Stein BE, Arendt EA and Bedi A: An Algorithmic approach to
the management of recurrent lateral patellar dislocation. J Bone
Joint Surg Am. 98:417–427. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fulkerson JP: Anteromedialization of the
tibial tuberosity for patellofemoral malalignment. Clin Orthop
Relat Res. 176–181. 1983.PubMed/NCBI
|
|
22
|
Fulkerson JP, Becker GJ, Meaney JA,
Miranda M and Folcik MA: Anteromedial tibial tubercle transfer
without bone graft. Am J Sports Med. 18:490–497. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tegner Y and Lysholm J: Rating systems in
the evaluation of knee ligament injuries. Clin Orthop Relat Res.
43–49. 1985.PubMed/NCBI
|
|
24
|
Schorn D, Yang-Strathoff S, Gosheger G,
Vogler T, Klingebiel S, Rickert C, Andreou D and Liem D: Long-term
outcomes after combined arthroscopic medial reefing and lateral
release in patients with recurrent patellar instability-a
retrospective analysis. BMC Musculoskelet Disord. 18:2772017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gravesen KS, Kallemose T, Blønd L,
Troelsen A and Barfod KW: High incidence of acute and recurrent
patellar dislocations: A retrospective nationwide epidemiological
study involving 24.154 primary dislocations. Knee Surg Sports
Traumatol Arthrosc. Jun 23–2017.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Clark D, Walmsley K, Schranz P and
Mandalia V: Tibial tuberosity transfer in combination with medial
patellofemoral ligament reconstruction: Surgical technique.
Arthrosc Tech. 6:e591–e597. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Joyner PW, Bruce J, Roth TS, Mills FB IV,
Winnier S, Hess R, Wilcox L, Mates A, Frerichs T, Andrews JR and
Roth CA: Biomechanical tensile strength analysis for medial
patellofemoral ligament reconstruction. Knee. 24:965–976. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hinckel BB, Gobbi RG, Demange MK, Pereira
CAM, Pécora JR, Natalino RJM, Miyahira L, Kubota BS and Camanho GL:
Medial patellofemoral ligament, medial patellotibial ligament, and
medial patellomeniscal ligament: Anatomic, histologic,
radiographic, and biomechanical study. Arthroscopy. 33:1862–1873.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lind M, Jakobsen BW, Lund B and
Christiansen SE: Reconstruction of the medial patellofemoral
ligament for treatment of patellar instability. Acta Orthop.
79:354–360. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Schöttle PB, Fucentese SF and Romero J:
Clinical and radiological outcome of medial patellofemoral ligament
reconstruction with a semitendinosus autograft for patella
instability. Knee Surg Sports Traumatol Arthrosc. 13:516–521. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Trillat A, Dejour H and Couette A:
Diagnosis and treatment of recurrent dislocations of the Patella.
Rev Chir Orthop Reparatrice Appar Mot. 50:813–824. 1964.(In
French). PubMed/NCBI
|
|
32
|
Tanaka MJ, Voss A and Fulkerson JP: The
anatomic midpoint of the attachment of the medial patellofemoral
complex. J Bone Joint Surg Am. 98:1199–1205. 2016. View Article : Google Scholar : PubMed/NCBI
|