Introduction
Sleep apnea syndrome (SAS) is a sleep respiratory
disturbance disease, which is characterized by a high incidence
rate, many complications and potential risks (1). Obstructive sleep apnea syndrome (OSAS)
accounts for the majority of cases clinically. Epidemiological
survey showed that the incidence rate of OSAS is 2–4% in adults,
4.63% in individuals aged >30 years and up to 30–50% in
individuals complicated with hypertension and coronary artery
disease (CAD) (2,3). OSAS is defined as follows: Repeated
attack of apnea and hypopnea for more than 30 times during the 7 h
sleep at night, or AHI ≥5. Polysomnography (PSG) detection is the
gold standard of OSAS (4). OSAS can
manifest in multiple organ system damage, leading to functional and
organic changes in vital organs (5,6). Sleep
structural disorder and hypoxemia in sleep stage are important
features of OSAS. The repeated hypoxemia and hypercapnia during
sleep result in a series of pathophysiological changes in the body,
which can promote the development of CAD, and increase the
morbidity and mortality rates of CAD and other vascular
diseases.
Many studies have shown that OSAS is closely related
to the risk factors of vascular diseases, such as hypertension,
arrhythmia, CAD, stroke and pulmonary arterial hypertension
(5–8). The morbidity and mortality rates of CAD
in OSAS patients are significantly increased, but the exact
relationship between OSAS and CAD remains unclear. In the present
study, 84 patients with suspected CAD were enrolled for sleep
detection and coronary angiography, in order to investigate the
correlation between OSAS and CAD and analyze the risk factors.
Materials and methods
Subjects
A total of 84 patients with suspected CAD due to
chest tightness, chest pain and nocturnal angina, admitted in the
Department of Cardiology of The Affiliated Hospital of Medical
College Qingdao University (Qingdao, China) from March, 2016 to
June, 2017 were selected, including 56 males and 28 females.
According to the results of coronary angiography, the patients were
divided into two groups; the control group with a negative coronary
angiography and the CAD group with a positive coronary angiography
(Table I). Inclusion criteria were:
i) Patients with repeated snoring for >5 years; ii) with chest
tightness, chest pain or nocturnal angina, or with ST-segment
depression or pathological Q wave in electrocardiogram; and iii)
age between 18–75 years. Exclusion criteria were: i) Cardiac
dysfunction or heart failure (ejection fraction <40%); ii)
chronic obstructive pulmonary disease and daytime hypoxemia; iii)
recent oxygen therapy or mechanical ventilation treatment; iv)
valvular disease or cardiomyopathy; v) variant angina pectoris or X
syndrome; vi) recent cerebral stroke; vii) central sleep apnea; and
viii) intolerance to PSG monitoring. The present study was approved
by the Ethics Committee of the Affiliated Hospital of The
Affiliated Hospital of Medical College Qingdao University. Written
informed consent was obtained from all the participants before the
study.
 | Table I.General conditions in different
groups. |
Table I.
General conditions in different
groups.
|
| Groups |
|
|---|
|
|
|
|
|---|
| Items | Control (n=34) | CAD (n=50) | P-value |
|---|
| Age (years) | 60.37±8.45 | 69.96±7.48 | 0.064 |
| Sex
(male/female) | 16/18 | 40/10 | 0.071 |
| BMI
(kg/m2) | 27.08±4.72 | 25.34±4.03 | 0.052 |
| LVEF (%)b | 70.26±6.98 | 62.95±9.14 | 0.004 |
| AHI
(n/min)a | 14.03±11.21 | 21.22±13.66 | 0.019 |
| Lowest oxygen
saturationa | 88.45±5.19 | 84.32±7.59 | 0.023 |
| TC (mmol/l) | 4.50±0.92 | 4.12±0.89 | 0.075 |
| TG
(mmol/l)a | 1.97±1.14 | 2.33±1.78 | 0.044 |
| Gensini
scoreb | 7.25±12.62 | 42.37±38.81 | 0.008 |
| Diabetes
mellitusa | 3 (8.82%) | 7 (14.00%) | 0.039 |
| Hypertension | 13 (38.24%) | 39 (78.00%) | 0.087 |
| Smokingb | 3 (8.82%) | 29 (58.00%) | 0.003 |
| Obesity | 21 (61.76%) | 26 (52.00%) | 0.068 |
| OSAS | 21 (61.76%) | 40 (80.00%) | 0.056 |
Methods
General data collection
At admission, the patients were asked about their
medical history in detail and received a questionnaire (habitual
snoring in the questionnaire was defined as the snoring affecting
the bedfellows for at least 3 nights a week). The vital signs were
measured and the body mass index (BMI) was calculated. After
fasting for 8 h, blood was drawn for blood biochemistry, blood
routine examination, myocardium and enzymogram. Before coronary
angiography, echocardiography and electrocardiographic examination
were performed.
Sleep monitoring
Before and after coronary angiography, the sleep
respiratory monitoring was performed using the Stardust II portable
sleep monitor (Wellkang, Melbourne, FL, USA). Sleeping pills and
drinking alcohol were prohibited at 48 h before sleep monitoring.
The nose and mouth airflow, chest and abdomen movement, blood
oxygen saturation in finger tips, heart rate, snoring, body
position and other parameters of patients were monitored (4). Diagnostic criteria of OSAS: Recurrent
episodes of apnea (nose and mouth breathing stops for >10 sec)
and hypopnea (respiratory airflow is reduced to 50% of normal
airflow intensity, accompanied by decreased blood oxygen saturation
of >4%) >30 times, or apnea hypopnea index (AHI) ≥5 recorded
by the sleep monitor.
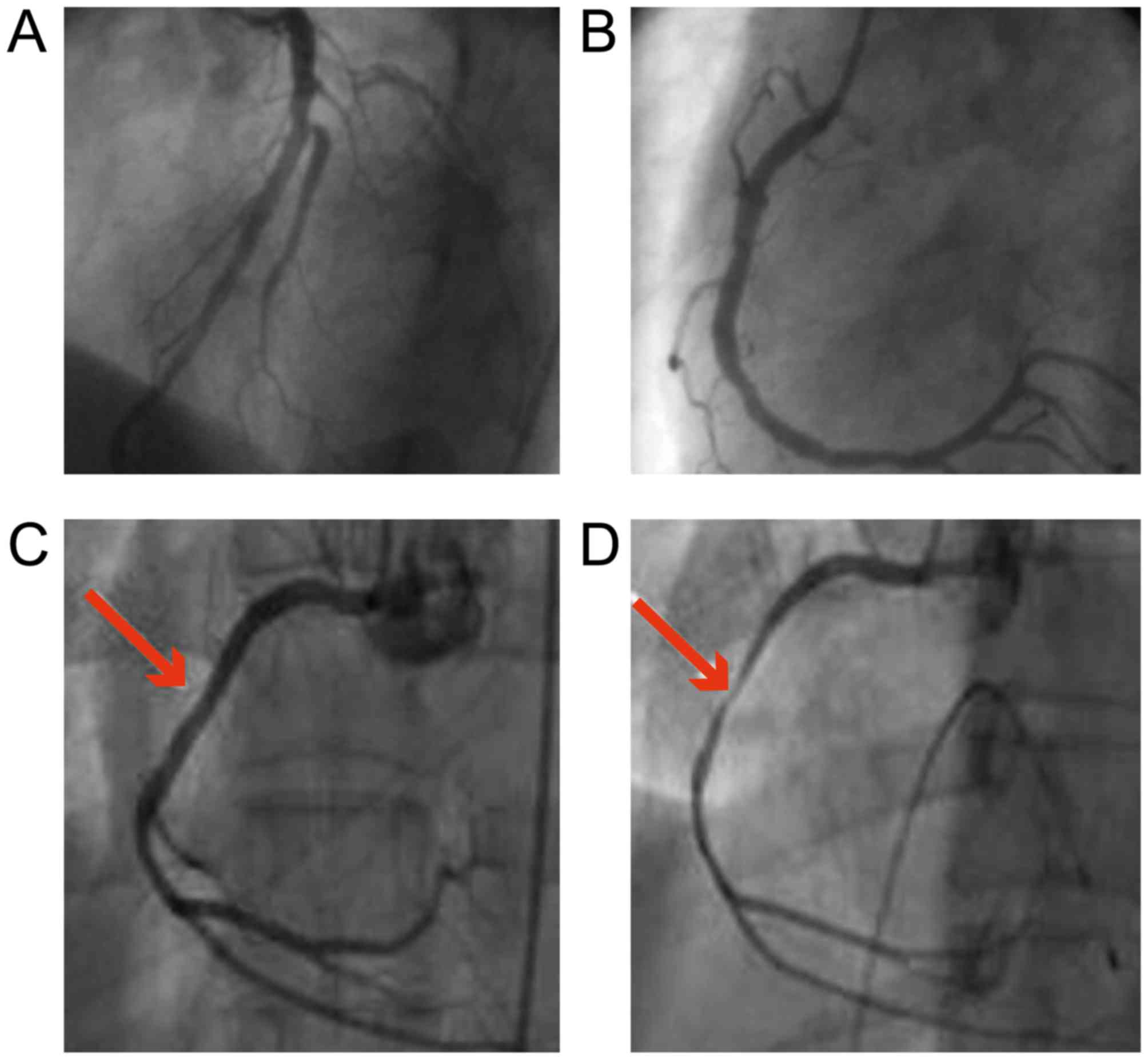
Coronary angiography
According to the guidelines of coronary angiography
of American College of Cardiology (ACC)/American Heart Association
(AHA), three experienced chief physicians performed the coronary
angiography. The multi-location angiography was conducted using
Judkin's method. The image processing system of angiography machine
was used for the quantitative analysis of stenosis. Diagnostic
criteria of coronary angiography: Stenosis of at least one coronary
artery or its major lumen >50% indicated the positive results
(Fig. 1).
Gensini score
According to the results of coronary angiography,
the degree of vascular lesion was quantitatively scored using the
Gensini scoring system. The scoring criteria were composed of two
parts: i) The basic score was given according to the degree of
coronary artery stenosis; and ii) the scoring coefficient was
determined according to the location of coronary artery lesions.
The accumulated total in each lesion site was the total score of
severity of coronary artery lesions in patients.
Statistical analysis
All statistics were performed using SPSS 20.0
software, (IBM, Armonk, NY USA). Comparison between groups was done
using One-way ANOVA test followed by post hoc test (least
significant difference). Percentage (%) was used to express the
enumeration data and Chi-square test was used for data analysis.
One-way analysis of variance was used to evaluate the relationship
between relative risk factors and CAD. The statistically
significant factors were screened for multivariate logistic
regression analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
General conditions
There were statistically significant differences in
AHI, lowest oxygen saturation, left ventricular ejection fraction,
triglyceride level, Gensini score, smoking and diabetes mellitus
between the CAD and control groups (P<0.05). BMI, total
cholesterol level, OSAS, hypertension, hyperlipidemia, obesity and
age were not statistically significant between the two groups
(P>0.05). The more severe OSAS was identified in the CAD group
compared to that in the control group, but the statistical analysis
showed that there was no statistically significant difference
between the two groups (80.00 vs. 61.76%, P=0.056) (Table I).
Correlation analysis of CAD and
OSAS
The cumulative number of vessels in CAD group was
high, and the coronary artery stenosis of moderate-severe patients
generally involved multiple vessels. The CAD patients were divided
into mild, moderate and severe group according to the severity of
OSAS. The difference in Gensini score was significant among the
three groups, and the analysis of variance showed the statistically
significant difference (P=0.025). The more severe the OSAS was, the
higher the Gensini score would be, suggesting that OSAS is closely
related to CAD (Table II).
 | Table II.Relationship between coronary artery
involvement and Gensini score and severity of OSAS in CAD
group. |
Table II.
Relationship between coronary artery
involvement and Gensini score and severity of OSAS in CAD
group.
|
| Coronary artery
involvement |
|
|
|---|
|
|
|
|
|
|---|
| CAD group | 0 | 1 | 2 | 3 | Gensini | P-value |
|---|
| Complicated with mild
OSAS | 0 | 7 | 0 | 6 |
19.38±20.15a | 0.045 |
| Complicated with
moderate OSAS | 0 | 4 | 2 | 6 |
25.42±19.61a | 0.037 |
| Complicated with
severe OSAS | 2 | 9 | 3 | 11 |
60.16±43.39a | 0.028 |
Univariate analysis of CAD-related
risk factors
Univariate analysis was performed for screening with
CAD as the dependent variable and the risk factors as the
independent variables. The results showed that the hypertension
(P=0.006), hyperlipidemia (P=0.034), smoking (P<0.001) and AHI
>20 (P=0.027) had significant correlations with CAD, but AHI
>5 had no correlation with CAD (P>0.05) (Table III).
 | Table III.Univariate analysis of CAD-related
risk factors. |
Table III.
Univariate analysis of CAD-related
risk factors.
| Risk factor | No. | CAD n (%) | χ2 | P-value |
|---|
| Smokingb | 32 | 29 (90.63%) | 10.375 | <0.001 |
|
Hyperlipidemiaa | 40 | 30 (75.00%) | 6.934 | 0.034 |
| Obesity | 47 | 26 (55.32%) | 1.358 | 0.528 |
|
Hypertensionb | 52 | 39 (75.00%) | 7.116 | 0.006 |
| Diabetes
mellitus | 10 | 6 (60.00%) | 2.217 | 0.615 |
| AHI
>20a | 34 | 27 (79.41%) | 5.623 | 0.027 |
Multivariate logistic analysis of
CAD-related risk factors
The risk factors obtained via univariate analysis
were included into the multivariate logistic regression, and the
results showed that smoking (P=0.029) and AHI >20 (P=0.038) were
the risk factors of CAD, and they had significantly positive
correlations with CAD, odds ratio (OR) = 7.036 and 5.377 Table IV).
 | Table IV.Multivariate logistic analysis of
CAD-related risk factors. |
Table IV.
Multivariate logistic analysis of
CAD-related risk factors.
| Risk factor | OR | Wald | P-value |
|---|
| Hypertension | 3.489 | 2.126 | 0.087 |
|
Smokinga | 7.036 | 5.204 | 0.029 |
| Hyperlipidemia | 3.125 | 1.469 | 0.146 |
| AHI
>20a | 5.377 | 2.478 | 0.038 |
Discussion
SAS is a common disease, clinically dominated by
OSAS, which can exist in a variety of cardiovascular system
diseases, such as congestive heart failure, hypertension and CAD
(1–3). Sleep structural disorder and hypoxemia
in sleep stage are important features of OSAS. The most common
cardiovascular symptoms of OSAS are stable angina and myocardial
infarction. The incidence of angina pectoris and myocardial
infarction in patients with OSAS and CAD is higher and more
pronounced.
The results of this study showed that the lowest
oxygen saturation was significantly different in CAD and control
group (P=0.023). AHI was higher but the lowest oxygen saturation
was lower in CAD group (P<0.05). Furthermore, CAD group was
divided into mild, moderate and severe group according to the
severity of OSAS. The Gensini score had statistically significant
difference among the three groups, and it was increased with the
increasing severity of OSAS (P<0.05). Univariate analysis
suggested that the hypertension (P=0.006), hyperlipidemia
(P=0.034), smoking (P<0.001) and AHI >20 (P=0.027) had
significant correlations with CAD, but AHI >5 had no correlation
with CAD (P>0.05). Logistic regression analysis was performed
for the CAD-related risk factors. The results showed that AHI
>20 was one of the risk factors of CAD (P=0.038), which was
consistent with the literature in China and world-wide (9,10). It
has been reported that OSAS, like obesity, smoking and
hypertension, is an independent risk factor of myocardial
infarction (2,3,8,11). The findings of American Sleep Health
Research Center also showed that AHI >5 is a risk factor of
cardiovascular disease and can significantly increase the incidence
and mortality rates of cardiovascular events. Studies have also
pointed out that OSAS is also an important factor affecting the
prognosis of CAD (12). This study
showed that the moderate-severe OSAS is one of the risk factors of
CAD, and the probability of CAD in moderate-severe OSAS patients is
5,377 times that in non-OSAS patients.
The main influencing mechanisms of OSAS (10,13–16), as
a risk factor of CAD, are as follows: i) Hypoxemia in OSAS patients
caused by repeated apnea can activate the chemical receptors and
sympathetic nerve, resulting in vascular smooth muscle remodeling
and hypertrophy, increasing oxygen consumption of heart and
aggravating myocardial ischemia and hypoxia; ii) the platelet
activity and aggregation capacity in OSAS patients are increased,
leading to the occurrence of cardiovascular events; iii) the
activity and content of tissue plasminogen activator inhibitor in
OSAS patients are increased, inhibiting the fibrinolytic system in
the body and leading to the hypercoagulable state, thrombosis and
atherosclerosis development; iv) repeated apnea hypoxia activates
the oxidative stress, which further leads to the lipid
peroxidation, vascular endothelial cell injury and increased
aggregation of inflammatory factors; v) nocturnal hypoxia may
affect the activity of lipoprotein receptor, leading to the
increased blood lipids and aggravating the development of
atherosclerosis; and vi) accompanying factors: OSAS patients are
mostly complicated by obesity, lipid metabolism disorders,
hypertension, arrhythmia and other susceptibility factors of CAD.
In order to reduce the incidence rate and improve the prognosis of
CAD in OSAS patients, therefore, it is recommended to provide
appropriate prevention and treatment for OSAS, as a risk
factor.
The multivariate logistic regression analysis showed
that smoking was also positively correlated with CAD, and was one
of the risk factors of CAD (correlation coefficient =7.036,
P<0.001). Epidemiological investigation and clinical studies
worldwide have also confirmed that smoking is an independent risk
factor of CAD (11,17,18). The
risk of CAD for smokers is 1.5- to 4-fold that of non-smokers.
Smoking can cause cardiovascular events including possible
mechanism leading to changes in hematology, neurohumor, metabolism,
hemodynamics, molecular genetics and biochemistry, causing coronary
artery spasm or atherosclerosis, eventually resulting in CAD.
Therefore, smoking cessation is an important measure to reduce the
risk of CAD.
Logistic regression analysis revealed that
hypertension and hyperlipidemia were not significant risk factors
for coronary heart disease (P=0.087), which may be associated with
the limited experimental cases.
CAD is one of the important causes of human death,
which has been confirmed to be related to age, sex, blood lipids,
blood pressure, diabetes mellitus, obesity and smoking.
Nevertheless, there is little research on the correlation between
OSAS and CAD. The results of the present study have shown that AHI
>20 was a risk factor of CAD (P=0.038), and the Gensini score of
CAD is related to the severity of OSAS. It is recommended that CAD
patients receive PSG monitoring for diagnosis and treatment in
time. In order to improve the prognosis of CAD patients, OSAS, as a
risk factor, should be actively prevented and treated. The timely
diagnosis and treatment of OSAS in CAD patients are secondary
preventive measures of CAD. However, the small sample size is a
limitation of the present study, and we would like to increase the
sample size in future studies.
In conclusion, the results of the present study have
shown that CAD is closely correlated with OSAS. In addition,
smoking and AHI >20 are the risk factors of CAD, which should be
paid close attention. To reduce the incidence rate and improve the
prognosis of CAD, patients should quit smoking and OSAS, as a risk
factor, should be prevented and treated appropriately.
Acknowledgements
Not applicable.
Funding
Not funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
JZ and WZ designed the study, YS performed the
collection and the entry of the data, YJ analysed the data, JZ
prepared the manuscript, YY carried out the search and the
literature analysis. All the authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The Affiliated Hospital of Medical College Qingdao University
(Qingdao, China). Signed written informed consents were obtained
from the patients and/or guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Imataka G, Nakajima I, Goto K, Konno W,
Hirabayashi H and Arisaka O: Drop episodes improved after
tracheotomy: A case of Coffin-Lowry syndrome associated with
obstructive sleep apnea syndrome. Eur Rev Med Pharmacol Sci.
20:498–501. 2016.PubMed/NCBI
|
|
2
|
Lombardi C, Tobaldini E, Montano N,
Losurdo A and Parati G: Obstructive sleep apnea syndrome (OSAS) and
cardiovascular system. Med Lav. 108:276–282. 2017.PubMed/NCBI
|
|
3
|
Barbosa FR, Silva CM, Lima GA, Warszawski
L, Domingues RC, Dominic M, Fontes R, Neto Vieira L and Gadelha MR:
Prevalence of obstructive sleep apnea in patients with prolactinoma
before and after treatment with dopamine agonists. Pituitary.
17:441–449. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Buccheri A, Chinè F, Fratto G and Manzon
L: Rapid maxillary expansion in obstructive sleep apnea in young
patients: Cardio-Respiratory monitoring. J Clin Pediatr Dent.
41:312–316. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Karimzadeh F, Nami M and Boostani R: Sleep
microstructure dynamics and neurocognitive performance in
obstructive sleep apnea syndrome patients. J Integr Neurosci.
16:127–142. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Alvarez-Sabín J, Romero O, Delgado P,
Quintana M, Santamarina E, Ferré A, Maisterra O, Riba-Llena I,
Montaner J and Sampol G: Obstructive sleep apnea and silent
cerebral infarction in hypertensive individuals. J Sleep Res.
20:962–1105. 2017.
|
|
7
|
Li L, Lu J, Xue W, Wang L, Zhai Y, Fan Z,
Wu G, Fan F, Li J, Zhang C, et al: Target of obstructive sleep
apnea syndrome merge lung cancer: Based on big data platform.
Oncotarget. 8:21567–21578. 2017.PubMed/NCBI
|
|
8
|
Micarelli A, Liguori C, Viziano A, Izzi F,
Placidi F and Alessandrini M: Integrating postural and vestibular
dimensions to depict impairment in moderate-to-severe obstructive
sleep apnea syndrome patients. J Sleep Res. 26:487–494. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Arik B, Inci MF, Gumus C, Varol K, Ege MR,
Dogan OT and Zorlu A: Advanced age and apnea-hypopnea index predict
subclinical atherosclerosis in patients with obstructive sleep
apnea syndrome. Multidiscip Respir Med. 8:92013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Meng S, Fang L, Wang CQ, Wang LS, Chen MT
and Huang XH: Impact of obstructive sleep apnoea on clinical
characteristics and outcomes in patients with acute coronary
syndrome following percutaneous coronary intervention. J Int Med
Res. 37:1343–1353. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhu H, Xu H, Chen R, Liu S, Xia Y, Fu Y,
Li X, Qian Y, Zou J, Yi H, et al: Smoking, obstructive sleep apnea
syndrome and their combined effects on metabolic parameters:
Evidence from a large cross-sectional study. Sci Rep. 7:88512017.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Capodanno D, Milazzo G, Cumbo M, Marchese
A, Salemi A, Quartarone L, Benvenuto E, Galseran C, Distefano SM
and Tamburino C: Positive airway pressure in patients with coronary
artery disease and obstructive sleep apnea syndrome. J Cardiovasc
Med (Hagerstown). 15:402–406. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Singh A, Prasad R, Garg R, Kant S, Hosmane
GB, Dubey A, Agarwal A and Verma RK: A study to estimate prevalence
and risk factors of obstructive sleep apnoea syndrome in a
semi-urban Indian population. Monaldi Arch Chest Dis. 87:7732017.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mihaicuta S, Udrescu M, Topirceanu A and
Udrescu L: Network science meets respiratory medicine for OSAS
phenotyping and severity prediction. PeerJ. 5:e32892017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang ZH, Zhu D, Xie S, Deng Y, Pan Y, Ren
J and Liu HG: Inhibition of rho-kinase attenuates left ventricular
remodeling caused by chronic intermittent hypoxia in rats via
suppressing myocardial inflammation and apoptosis. J Cardiovasc
Pharmacol. 70:102–109. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vitulano N, Di Marco Berardino A, Re A,
Riccioni G, Perna F, Mormile F, Valente S and Bellocci F:
Obstructive sleep apnea and heart disease: The biomarkers point of
view. Front Biosci (Schol Ed). 5:588–599. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Foody J, Huo Y, Ji L, Zhao D, Boyd D, Meng
HJ, Shiff S and Hu D: Unique and varied contributions of
traditional CVD risk factors: A systematic literature review of CAD
risk factors in China. Clin Med Insights Cardiol. 7:59–86. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schmermund A, Lehmann N, Bielak LF, Yu P,
Sheedy PF II, Cassidy-Bushrow AE, Turner ST, Moebus S, Möhlenkamp
S, Stang A, et al: Comparison of subclinical coronary
atherosclerosis and risk factors in unselected populations in
Germany and USA. Atherosclerosis. 195:e207–e216. 2007. View Article : Google Scholar : PubMed/NCBI
|