Introduction
Haglund's syndrome is recognized to cause heel pain
(1,2). Repeated pressure caused by calcaneus in
dorsiflexion on the retrocalcaneal bursa and Achilles tendon
occasionally leads to aching bursitis and insertional Achilles
tendinopathy (3).
A typical patient with symptomatic Haglund's
syndrome may have an aching, red, inflamed heel with an obvious
osseous prominence on the lateral radiographs of the
posterosuperior heel. This is always associated with insertional
Achilles tendinopathy, retrocalcaneal bursitis, and superficial
adventitious Achilles tendon bursitis (4). The patient complains of enlargement of
the posterior heel and encounters problems with footwear and sport.
The posterolateral surface becomes extremely enlarged and reddened
(5).
Painful bone prominence in the retrocalcaneal region
of the posterior calcaneus with no relief after 6 months of
conservative therapy is considered to require surgery (6). Surgical treatment mainly includes the
elimination of retrocalcaneal bursitis and visible osseous
prominence, debridement and reattachment of Achilles insertion
point.
Open surgical management and minimal invasive
surgery are both used in the treatment of Haglund's syndrome. The
advantage of the former technique is that it is a more rapid
procedure, although it requires extensive exposure and it is
difficult to determine the exact amount of bone resected on the
medial side unless a double approach with an additional medial
incision is used (5). With open
surgery, a large wound in a poor blood supply area takes time to
heal and various other complications have been reported, such as
weak calcaneus following removal of the posterosuperior osseous
prominence (7), persistent ache
(8), and hypoesthesia in the area of
the scar (9). The advantage of
minimally invasive surgery is that it can be performed through a
small incision, which heals very well. However, this technique does
increase the operating time because radiology is used to position K
wires in occasionally, and then, osteotomy occurs using a
mechanical shaver or other intrument (5).
In most of the severe cases, after calcified lesion
on Achilles tendon is removed, Achilles insertion point
reconstruction is necessary. Anderson et al (10) suggest that if the point of dissected
Achilles insertion was less than 50% of the total surface area,
then the reconstruction cannot be implemented. If the point of
dissected Achilles insertion was more than 50% of the total surface
area, then the reconstruction can be implemented and fixed with two
parenchyma anchors. In most of the studies, the anchors were
implanted under direct vision, creating a larger wound. In 2013,
Chiu et al suggested that acute Achilles tendon laceration
can be repaired with modified percutaneous Bunnell suture treatment
under endoscopy-assisted percutaneous repair (11).
We used this method in endoscopic Achilles tendon
repair during the treatment of Haglund's syndrome. The suture
anchors were implanted arthroscopically. The advantage of this
method is that it avoids the occurrence of complications after
traditional conservative treatment and open surgery. This method
cannot only improve the suture effect and accuracy, but also retain
the advantages of the operation of percutaneous tendon repair.
Materials and methods
Between September 2014 and July 2015, our technique
was performed on 7 patients (3 female with 3 heels, 4 male with 4
heels), with an average age of 35.2 years. The average symptom time
of all the patients was approximately 17.1 months (range, 12–24
months) before operation. Haglunds syndrome is mainly diagnosed by
clinical symptoms, physical examination and lateral X-ray results
as well as magnetic resonance imaging (MRI). The typical clinical
symptoms of Haglunds syndrome include ankle Achilles tendon pain,
redness, and swelling. In addition, all the patients with Haglunds
syndrome exhibit an osseous prominence that directly affects their
heel. All 7 patients were treated with lateral ankle X-ray and MRI
examinations before operation. Standardized lateral ankle X-ray
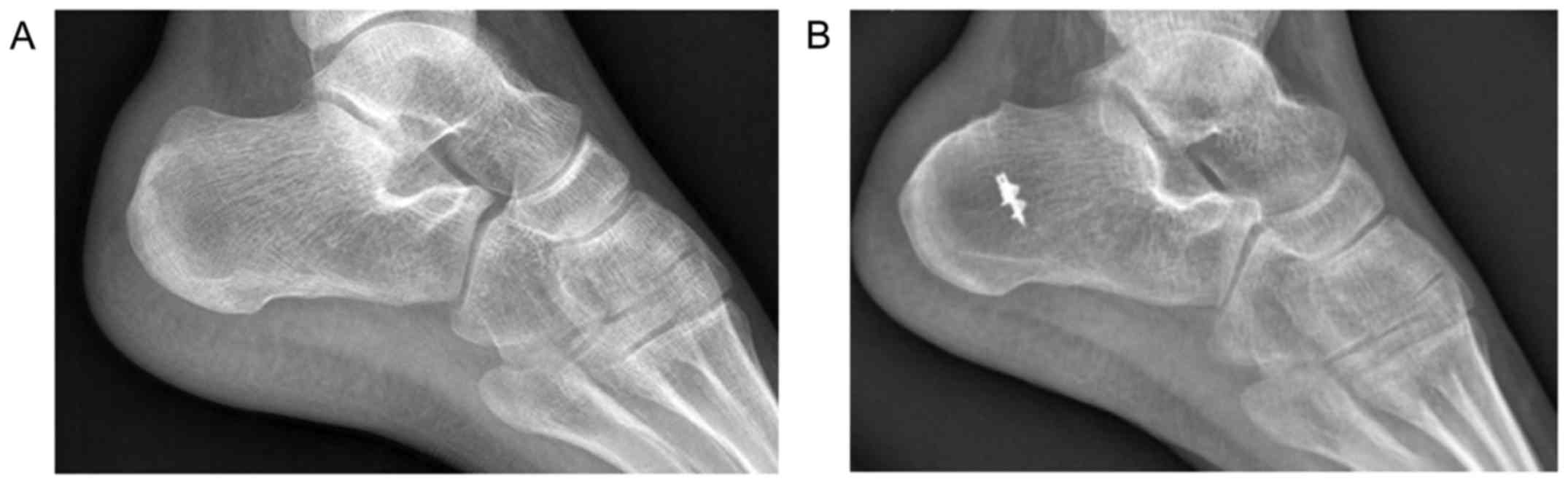
(Fig. 1A) of the weightbearing foot
shows the prominence of posterosuperior calcaneus in the heel. The
parallel pitch lines and Fowler and Philip angle (FPA) of each
preoperative radiograph were measured. Posterosuperior calcaneal
prominence of the patients had positive heel parallel pitch lines
and FPA. The MRI results showed inflammation and swelling at the
retrocalcaneal bursa and the soft tissue around the Achilles tendon
insertion. Marrow edema was also observed in the posterosuperior
calcaneal prominence of all 7 patients. MRI showed intratendinous
calcifications in the 7 heels (Fig.
2).
None of the patients benefitted from conservative
treatment, including avoidance of tight shoes, non-steroidal
anti-inflammatory drugs, activity modification and physical
therapy.
Surgical technique
Arthroscopic surgery occurred under lumbar or
general anesthesia with the surgical patients in the prone
position. A surgical tourniquet was applied to the thigh of the
patient. The limb of the patient that was affected was elevated and
set beyond the operating table. The first two portals were
established as medial and lateral of the Achilles tendon and
posterosuperior calcaneal prominence were at the same level. A 4 mm
endoscopic arthroscope with 30° field of view was placed as close
as possible to the superior edge of the calcaneus, and also as far
posterior as possible. If this portal was placed high, it would be
difficult later during the procedure to reach the posteroinferior
part of the calcaneus. A 4 mm shaver was inserted from the opposite
portal. The posterior calcaneal fat pad was identified and removed.
The bursectomy and posterior calcaneoplasty was performed as
described by Jerosch (12).
Partial tearing of the Achilles tendon insertion
after the debridement was repaired with 5.0 mm suture anchors and
modified Bunnell sutures immediately. A 4 mm incision was made at
the posteromedial calcaneus. According to the dissection scope, 1
or 2 suture anchors were implanted in the Achilles tendon insertion
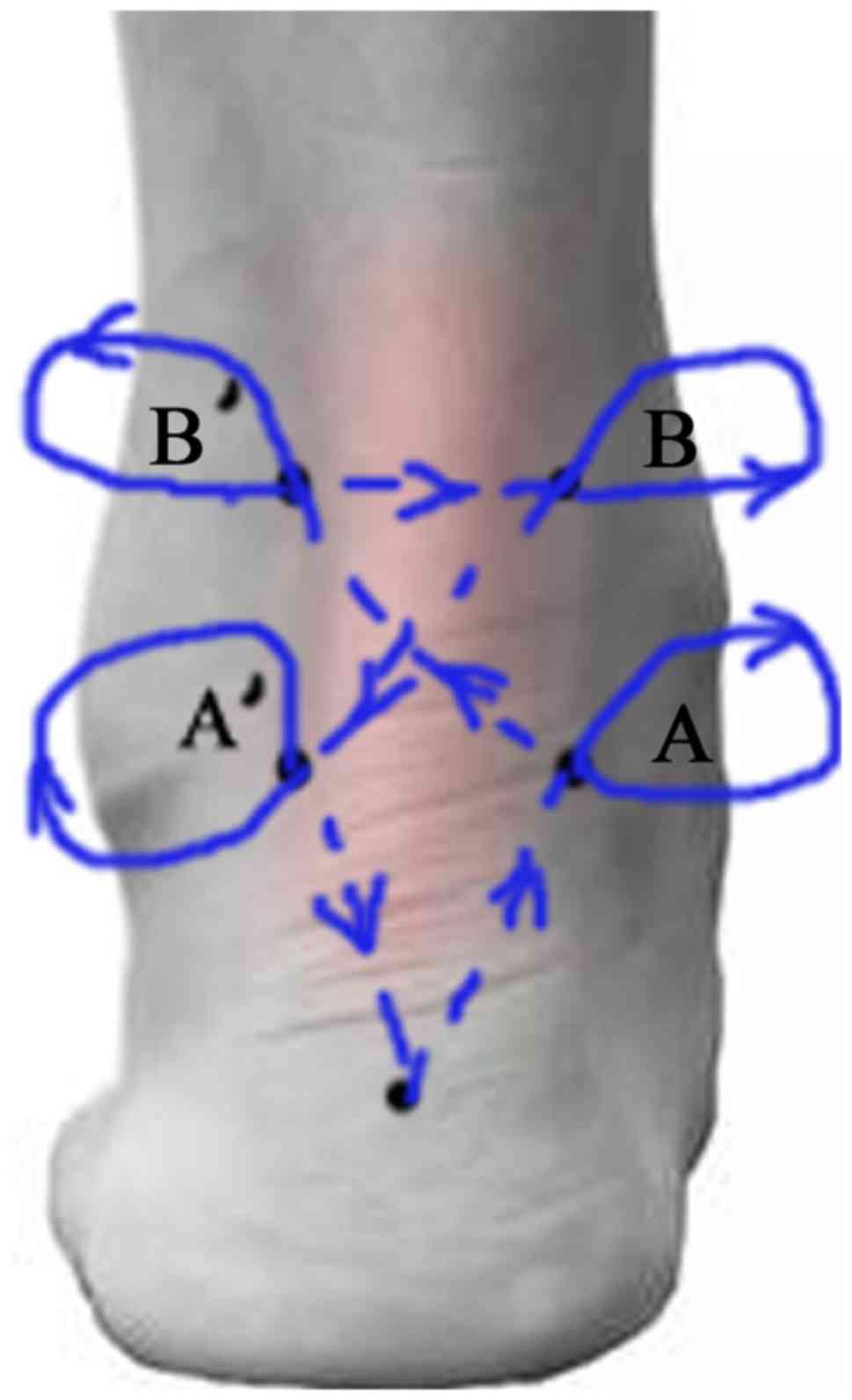
site (Fig. 3). Four stab wounds were
made above the insertion site, 2 at each side (Fig. 4). The suture was passed using a
straight needle from the surgical incision wound to the lateral
surgical wound (incision to A), through the heel tendon and drawn
out. The operative needle was passed through the heel tendon and
removed from the portal vein B (from portal vein A to B).
Subsequently, the operative needle was passed from portal B' to B,
portal B to A', portal A' back to the incision wound and then
knotted with another suture. Of note, the whole needle had to be
taken out and then pierced back at the 4 stab wounds.
Repetitious irrigation was used in the operation
region. The incisions and stab wounds were sewn up and dressed with
appropriate pressure.
Postoperative care
The leg was lifted on a pillow to reduce swelling at
the first week after operation. Sutures were taken out 14 days
later. Partial weightbearing activities wearing the Achilles
walking boots were started 28 days postoperatively and full weight
bearing activities 42 to 56 days postoperatively. The patient
returned to normal activities and performed exercises 90 days
postoperatively.
Statistical analysis
Parallel pitch lines of the patients and the
American Orthopaedic Foot and Ankle Society (AOFAS) score were used
to evaluate the clinical effect of patients at the last
postoperative follow-up period. According to the patients' AOFAS
score, the clinical curative effect was judged as: Poor curative
(0–70 points), fair curative (70–79 points), good curative (80–89
points) and excellent curative effect (90–100 points) (13). The Wilcoxon two-sample test was used
to detect the difference between the AOFAS score before and after
operation. The results showed there was a significant difference
between the AOFAS score before and after operation. P<0.05 was
considered to indicate a statistically significant difference.
Statistical analysis was carried out using SPSS 20.0 software (IBM
Inc., Armonk, NY, USA).
Results
All 7 patients underwent only one procedure and were
followed up from 18 to 31 months (mean, 22 months). In all heels,
the osseous prominence, retrocalcaneal bursitis and chondroid
metaplasia of Achilles tendon insertion were observed under
arthroscope (10). No Achilles
tendon tear was reported. Negative parallel pitch lines and
sufficient bony planning was shown in postoperative lateral
position film (Fig. 1B). The average
AOFAS score of the patients increased from 58.7±13.0 points (before
operation) to 87.8±12.7 points (last follow-up period), and the
difference was statistically significant.
Five of the 7 patients had excellent curative effect
(90–100 points), 2 patients had good (80–89 points) and 0 patients
had poor (0–70 points) or fair curative effect (70–79 points). None
of the patients had postoperative nerve damage or postoperative
permanent vascular injuries. In addition, there were no
postoperative wound infections or postoperative Achilles tendon
avulsions.
Discussion
Preoperative diagnosis of Haglund's syndrome holds
significant value to the operation plan. The diagnosis of Haglund's
syndrome was mainly based on the patients' clinical symptoms,
physical examination, X-Ray, and MRI results. FPA has been observed
to yield 86–100% false-negative results in previous studies
(1,14–16). Lu
et al (17) also suggested
that the FPA and parallel pitch lines were not accurate indicators
in reflecting the severity of symptomatic Haglunds syndrome. The
surgeon should assess the surgery according to the patient's
clinical symptoms. Radiographic measurements should be for
reference only. MRI is commonly performed to assess the adjacent
tendon for the need of intraoperative debridement concomitantly
with the calcaneal osteoplasty. Insertional tendinosis is
frequently associated with adjacent calcaneal marrow edema. This
marrow edema was the most predictable sign of a symptomatic
Achilles tendon in Haims et al MRI comparison of symptomatic
and asymptomatic patients and has been shown to be a common
associated finding in insertional tendinosis (18). Intraoperative endoscopic examination
is useful when the ankle is passively dorsiflexed to observe the
status of the patients' Achilles tendon along the calcaneus. If
there is any pressure on the heel tendon with osseous prominence,
posterior calcaneoplasty is considered feasible.
At present, large intratendinous calcifications
correlated with heel chronic insertional Achilles tendinopathy
limits the use of arthroscopic tenodesis (19). Arthroscopic planning of large
prominences may lead to tendon insertional tearing if there is
insufficient exposure (20). Jerosch
(12) suggested that arthroscopic
calcaneoplasty should be avoided in those types of ossific Achilles
tendon insertions. Arthroscopic treatment may also be avoided in
the intrinsic lesions of Achilles tendon.
Posterior midline approach and split of the Achilles
tendon is preferred in those patients. Once posterosuperior
calcaneal prominence is removed, the tendon is reattached with
either transosseous sutures or bone anchors. Related research
showed that bioabsorbable knotless screws with a spiked washer may
be used in the operation of Achilles tendon reduction (20). Syed and Perera (5) suggested that a small amount of tendon
elevation does not require reattachment. However, if this is
significant, then suture anchors can be passed percutaneously
through the tendon and the skin opened superficially to allow these
to be tied off. Alternatively, these can be tied off internally by
pulling the sutures through into the retrocalcaneal space, out of
the instrument portal and tied off under direct vision with a knot
pusher. Ma and Griffith suggested (21) the development of acute closed
ruptured Achilles tendon percutaneous repair firstly, followed by
some treatment modifications, including heel repair of Achilles
tendon with plantaris tendon augmentation (22–26).
Previous findings have shown that acute Achilles tendon rupture
repair with endoscopy can repair the rears of Achilles tendon and
finish the strengthening through the modification of Bunnell
sutures (11). This method can
effectively avoid the incidence of complications, ensure the good
repairing effect of the patient's skin and tendon and improve the
accuracy of suture after surgery. Wiegerinck et al (27) report that no minimal invasive
surgical studies offer a clear method to reinsert the Achilles
tendon with bone anchors or perform augmentation (plantaris tendon
or FHL). In our practice, when the sutures were tied with a knot
guide under endoscopy, the ankle was held to perform plantar
flexion within a certain range of motion under the doctor's
guidance. The gap between tendon and calcaneus was checked through
the endoscope in real time. Less ankle plantar flexion was
performed and tied relatively when the clearance distance was small
after detection. If the clearance distance was large enough, it was
tied with stronger ankle dorsiflexion. Thus, surgeons can reach a
solid and suitable fixation of the torn tendon end.
Our study is a supplement of endoscopic repair and
strengthening of the Achilles tendon. It expands the indication of
arthroscopic therapy of Haglund's syndrome and is a reliable
technique.
Study limitations include lack of a control group
(only 3 cases were compared with self control). As the number of
subjects included was less, the postoperative follow-up time was
relatively short. Therefore, more subjects are required in
prospective research to verify our results. Theoretically, our
technique is also suitable for Achilles tendon augmentation or the
repair of full rupture of Achilles tendon after intratendinous
debridement.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chang C-D and Wu JS: MR Imaging findings
in heel pain. Magn Reson Imaging Clin N Am. 25:79–93. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wiegerinck JI, Kok AC and van Dijk CN:
Surgical treatment of chronic retrocalcaneal bursitis. Arthroscopy.
28:283–293. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu Z, Hua Y, Li Y and Chen S: Endoscopic
treatment of Haglund's syndrome with a three portal technique. Int
Orthop. 36:1623–1627. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jerosch J and Nasef NM: Endoscopic
calcaneoplasty-rationale, surgical technique, and early results: A
preliminary report. Knee Surg Sports Traumatol Arthrosc.
11:190–195. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Syed TA and Perera A: A proposed staging
classification for minimally invasive management of Haglund's
syndrome with percutaneous and endoscopic surgery. Foot Ankle Clin.
21:641–664. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Frey C: Surgical advancements:
Arthroscopic alternatives to open procedures: Great toe, subtalar
joint, Haglund's deformity, and tendoscopy. Foot Ankle Clin.
14:313–339. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Perlman MD: Enlargement of the entire
posterior aspect of the calcaneus: Treatment with the Keck and
Kelly calcaneal osteotomy. J Foot Surg. 31:424–433. 1992.PubMed/NCBI
|
|
8
|
Nesse E and Finsen V: Poor results after
resection for Haglund's heel. Analysis of 35 heels in 23 patients
after 3 years. Acta Orthop Scand. 65:107–109. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pauker M, Katz K and Yosipovitch Z:
Calcaneal ostectomy for Haglund disease. J Foot Surg. 31:588–589.
1992.PubMed/NCBI
|
|
10
|
Anderson JA, Suero E, O'Loughlin PF and
Kennedy JG: Surgery for retrocalcaneal bursitis: A tendon-splitting
versus a lateral approach. Clin Orthop Relat Res. 466:1678–1682.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chiu CH, Yeh WL, Tsai MC, Chang SS, Hsu KY
and Chan YS: Endoscopy-assisted percutaneous repair of acute
Achilles tendon tears. Foot Ankle Int. 34:1168–1176. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jerosch J: Endoscopic calcaneoplasty. Foot
Ankle Clin. 20:149–165. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jardé O, Quenot P, Trinquier-Lautard JL,
Tran-Van F and Vives P: Haglund disease treated by simple resection
of calcaneus tuberosity. An angular and therapeutic study. A propos
of 74 cases with 2 years follow-up. Rev Chir Orthop Repar Appar
Mot. 83:566–573. 1997.(In France).
|
|
14
|
Heneghan MA and Pavlov H: The Haglund
painful heel syndrome. Experimental investigation of cause and
therapeutic implications. Clin Orthop Relat Res. 187:228–234.
1984.
|
|
15
|
Ruch JA: Haglund's disease. J Am Podiatry
Assoc. 64:1000–1003. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fuglsang F and Torup D: Bursitis
retrocalcanearis. Acta Orthop Scand. 30:315–323. 1961. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lu CC, Cheng YM, Fu YC, Tien YC, Chen SK
and Huang PJ: Angle analysis of Haglund syndrome and its
relationship with osseous variations and Achilles tendon
calcification. Foot Ankle Int. 28:181–185. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Haims AH, Schweitzer ME, Patel RS, Hecht P
and Wapner KL: MR imaging of the Achilles tendon: Overlap of
findings in symptomatic and asymptomatic individuals. Skeletal
Radiol. 29:640–645. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Leitze Z, Sella EJ and Aversa JM:
Endoscopic decompression of the retrocalcaneal space. J Bone Joint
Surg Am. 85-A:1488–1496. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Maquirriain J: Endoscopic Achilles
tenodesis: A surgical alternative for chronic insertional
tendinopathy. Knee Surg Sports Traumatol Arthrosc. 15:940–943.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ma GW and Griffith TG: Percutaneous repair
of closed ruptured achilles tendon: A new technique. Clin Orthop
Relat Res. 128:247–255. 1977.
|
|
22
|
Assal M, Jung M, Stern R, Rippstein P,
Delmi M and Hoffmeyer P: Limited open repair of Achilles tendon
ruptures: A technique with a new instrument and findings of a
prospective multicenter study. J Bone Joint Surg Am. 84-A:161–170.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cretnik A, Kosanović M and Smrkolj V:
Percutaneous suturing of the ruptured Achilles tendon under local
anesthesia. J Foot Ankle Surg. 43:72–81. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kakiuchi M: A combined open and
percutaneous technique for repair of tendo Achillis. Comparison
with open repair. J Bone Joint Surg Br. 77:60–63. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lui TH: Endoscopic-assisted Achilles
tendon repair with plantaris tendon augmentation. Arthroscopy.
23:556.e1–556.e5. 2007. View Article : Google Scholar
|
|
26
|
Majewski M, Rohrbach M, Czaja S and
Ochsner P: Avoiding sural nerve injuries during percutaneous
Achilles tendon repair. Am J Sports Med. 34:793–798. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wiegerinck JI, Zwiers R, van Sterkenburg
MN, Maas MM and van Dijk CN: The appearance of the pre-Achilles fat
pad after endoscopic calcaneoplasty. Knee Surg Sports Traumatol
Arthrosc. 23:2400–2405. 2015. View Article : Google Scholar : PubMed/NCBI
|