Introduction
Hematomas are masses of usually clotted blood that
form in tissues, organs or body spaces as a result of a broken
blood vessel (1–3). Among hematomas, chronic expanding
hematomas (CEHs) are rare (1–21).
Chronic inflammation, invoked by hematoma, is thought to lead to
the formation of a capsule around the hematoma, and new vessel
growth in and around the capsule (22). Furthermore, the gradual formation of
a hematoma accompanies leakage of blood from the new vessels, which
increases permeability through a plasminogen activator that is
precipitated in the clot (1). The
majority of patients with CEH in the chest typically have a history
of medical or surgical therapy for tuberculosis (2–14),
although some develop CEH after thoracic surgery for
non-tuberculous diseases (15–19) or
blunt thoracic trauma (19–21). CEH was initially reported as a
clinical entity in the 1980s, but the exact prevalence of CEH
within populations and mortality rates are unknown because of its
rarity. The symptoms of CEH differ depending on the site where CEH
occurs, but similar symptoms accompanying the increase of CEH have
been identified. When CEH occurs in the chest, dyspnea and chest
wall masses occur due to an increase in the volume of the hematoma
(22). In a recent review of the
Japanese and English literature, only 91 patients with this disease
have been described (22). According
to the review, they had a broad age distribution; 70.3% of them
were male, and lesions were predominantly on the trunk and lower
extremities. The range of clinical latent periods was wide, ranging
from one month to 57 years (1,23–26). A
commonly used treatment method for CEH is complete excision, which
yields the best clinical outcomes (26). The current report presents the
natural history of a CEH that presented as a slow-growing mass,
which was determined by calculating its doubling time and volume
changes.
Case report
A 76-year-old man was referred to the University of
Tsukuba-Mito Kyodo General Hospital (Mito, Japan) in March 2013
because of dyspnea upon exertion, which had first become apparent 4
years before. A large mass with a maximum diameter of 17×12 cm had
been found on a chest X-ray nine years ago in a mass screening by
the prefecture where the patient lived. This finding was followed
up for seven years at a local clinic near the patient's address by
chest X-ray, and the mass was slowly growing. However, the patient
did not want further examination and treatment during this period.
Thereafter, the patient visited the thoracic surgery department in
University of Tsukuba Hospital (Tsukuba, Japan) in August 2013, but
decided not to undergo surgical removal of the lesion. In addition,
the patient had a 10 pack-years smoking history up to the age of
45, and reported that he had suffered a blunt chest trauma in a
traffic accident 29 years before, but no medical record or imaging
study of this was available.
On admission to the University of Tsukuba-Mito Kyodo
General Hospital, respiratory sounds in the left lung were absent
and heart sounds were audible in the right thorax. A chest
radiograph and computed tomography (CT) revealed a mass of
inhomogeneous density, with focal calcification within the mass
(Fig. 1A). A percutaneous biopsy was
performed but the pathological diagnosis was not established
because only necrotic tissue was present within the specimen. The
patient was discharged, and he received oxygen therapy at home
because he did not want any further invasive treatment, then his
respiratory condition gradually deteriorated. Furthermore, the
patient succumbed to respiratory failure two years after the
initiation of home oxygen therapy and died in March 2015. Over the
course of the patient's illness, he received seven chest CT scans.
Fig. 1B reports the chest CT scan
taken 9 years prior to patient mortality. Finally, an autopsy was
performed and the final diagnosis of the mass was CEH.
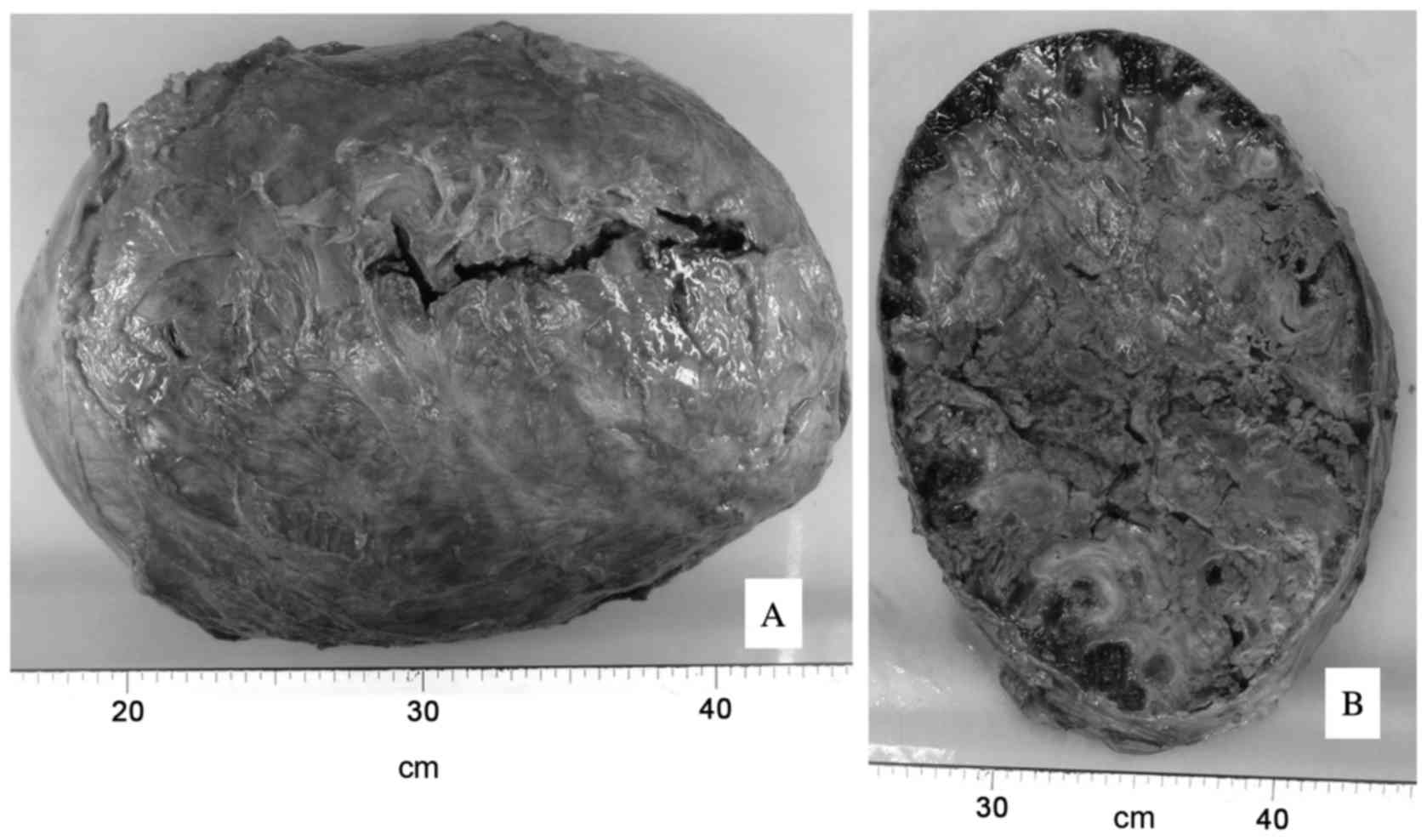
With regard to the autopsy observations, grossly, a
29 cm, 5.9 kg mass containing coagulative necrotic tissue occupied
the entire left thoracic cavity (Fig.
2A). The wall of the lesion was well demarcated, strongly
adherent and was expanding to the surrounding structures. In
addition, the lesion was encased in a thick capsule (Fig. 2B), and there was no evidence of
neoplasia. Fig. 3 shows the
relationship between ‘volume of mass’ and ‘days prior to mortality’
using the results from CT scans taken over the course of the
patient's disease.
The graph line, which was constructed by taking
plots of the estimated volume of the lesion and analyzed with
VINCENT v. 4.0 (Fujifilm Workstation, Tokyo, Japan), the time when
the CEH began to develop was evaluated using the least-squares
method (27). The estimation
indicated that the onset time of CEH was 8.2–11.0 years before the
patient mortality.
The doubling time of the disease (DTD) was
calculated using the chest CT scans that were recorded 7 times
during the clinical course. The DTD was calculated using a
modification of the following Schwartz formula of exponential
growth (28): DTD=(txlog2)/(3×log
(V2/V1)); where V1 and V2 were the largest diameters on the CT scan
measured at 2 different times, and t was the time interval between
2 measurements. The DTD of the CEH in this patient is shown in
Table I.
 | Table I.Doubling time of the chronic expanding
hematoma. |
Table I.
Doubling time of the chronic expanding
hematoma.
| Days prior to
mortality | Interval, days | Doubling time,
days |
|---|
| −5 to −373 | 368 | 2,072 |
| −373 to −665 | 292 | 3,626 |
| −665 to −1,089 | 424 | 1,896 |
| −1,089 to −1,474 | 385 | 7,296 |
| −1,474 to −1,839 | 365 | 1,818 |
| −1,839 to −3,246 | 1,407 | 3,549 |
Discussion
CEH in the chest is a rare clinicopathological
entity. The majority of patients with this disease have a history
of medical or surgical therapy for tuberculosis (2–14),
although some develop CEH after thoracic surgery for
non-tuberculous diseases (15–18) or
blunt thoracic trauma (19–21). The most common symptoms of CEH in the
chest are dyspnea related to compression of the lung, and slowly
growing chest wall mass (22).
Although the possibility of being treated as another disease in
countries outside Northeast Asia cannot be denied, almost of the
patients previously reported to have CEH in the chest were Japanese
(3–6,8,9,11–14) with
some from other Northeast Asian countries (2,7,10). Radiologically, CEH in the chest
appears as an intrathoracic mass in chest X-ray. Findings in chest
CT scan consist of a heterogeneous mass with a wall of variable
thickness that often contains peripheral areas of calcification
(4). The pathogenesis of CEH is
still unknown. According to a theory by Labadie and Glover,
however, the self-perpetuating expanding process in CEH is due to
the irritant effects of blood and its breakdown products, which
cause repeated episodes of bleeding from capillaries in the
granulation tissue (1). The range of
clinical latent period in previous reports is wide, ranging from 1
month to 57 years (1,23–26).
In the present case, a surgical resection of the
lesion could not be performed due to the patient's refusal to
undergo surgery. As a result, the clinical course of the disease
could be observed from the time of the first CT scan taken 9 years
before his referral to the hospital. CEH may grow very slowly,
however, the natural course of the disease has not been elucidated,
either for those with a prior history of tuberculosis or for those
without it.
Currently, the natural history, pathogenesis and
mechanism of CEH are unknown. It is important to provide and
accumulate knowledge on the increase in the size of the lesion and
on its doubling time. The present study therefore showed the DTD
(Table I) and the volume change of
CEH. The estimation indicated that the onset time of CEH was
8.2–11.0 years before the patient mortality. However, this onset
time was not the same as that at which he said he had suffered a
blunt chest trauma in a traffic accident (about 26 years before
succumbing to the present disease). As no medical records or
imaging were available, the difference cannot be explained but it
is believed that this chest trauma had no direct association with
the development of CEH. The patient of the present study had no
prior history of tuberculosis and a relatively short interval
between the prior medical event and the development of CEH, which
was consistent with the results of previous cases with no prior
history of tuberculosis (2–14).
Therefore, the present study has reported a case of
CEH. The patient did not undergo any surgical resection due to his
refusal of surgery, but this case illustrated a natural course of
CEH, which may provide clues towards clarifying the mechanism and
etiology of CEH. Furthermore, accumulation of knowledge about this
rare disease will help to elucidate it further.
Acknowledgements
The authors thank Dr Yoko Deguchi for her skillful
clinical management of the patient. We are especially grateful to
Ms. Flaminia Miyamasu for her review of the manuscript and Ms.
Kikue Sato for her secretarial assistance.
References
|
1
|
Labadie EL and Glover D:
Physiopathogenesis of subdural hematomas. Part 1. Histological and
biochemical comparisons of subcutaneous hematoma in rats with
subdural hematoma in man. J Neurosurg. 45:1382–1392. 1976.
View Article : Google Scholar
|
|
2
|
Dezube R, Terry P, Akulian J, Mathai SC,
Boyle M, Khasab T and Yarmus L: Chronic expanding hematoma of the
lung. Am J Respir Crit Care Med. 188:e712013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nomori H, Horio H, Kobayashi R and
Morinaga S: Expanding intrathoracic hemorrhagic lesion penetrating
the thoracic wall: A rare complication of chronic tuberculous
pleurisy. Thorac Cardiovasc Surg. 43:358–360. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hanagiri T, Muranaka H, Hashimoto M,
Nishio T, Sakai S, Ono M, Toyoshima S and Nagashima A: Chronic
expanding hematoma in the chest. Ann Thorac Surg. 64:559–561. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Akata S, Ohkubo Y, Jinho P, Saito K,
Yamagishi T, Yoshimura M, Kotake F, Kakizaki D and Abe K: MR
features of a case of chronic expanding hematoma. Clin Imaging.
24:44–46. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Uramoto H, Nakanishi R, Eifuku R, Muranaka
H, Takenoyama M, Yoshino I, Osaki T and Yasumoto K: Chronic
expanding hematoma in the chest. J Cardiovasc Surg (Torino).
41:143–146. 2000.PubMed/NCBI
|
|
7
|
Roper CL and Cooper JD: Chronic expanding
hematoma of the thorax. J Thorac Cardiovasc Surg. 122:1046–1048.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sato M, Kosaka S and Takahashi T: Life
threatening chronic expanding hematoma of the thorax. J Cardiovasc
Surg (Torino). 45:511–514. 2004.PubMed/NCBI
|
|
9
|
Okubo K, Okamoto T, Isobe J and Ueno Y:
Rupture of a chronic expanding hematoma of the thorax into lung
parenchyma. J Thorac Cardiovasc Surg. 127:1838–1840. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kwon YS, Koh WJ, Kim TS, Lee KS, Kim BT
and Shim YM: Chronic expanding hematoma of the thorax. Yonsei Med
J. 48:337–340. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tsubochi H, Sato N and Imai T: Chronic
expanding hematoma with bronchopleural fistula and empyema space.
Ann Thorac Cardiovasc Surg. 15:171–173. 2009.PubMed/NCBI
|
|
12
|
Takahama M, Yamamoto R, Nakajima R, Izumi
N and Tada H: Extrathoracic protrusion of a chronic expanding
hematoma in the chest mimicking a soft tissue tumor. Gen Thorac
Cardiovasc Surg. 58:202–204. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Muramatsu T, Shimamura M, Furuichi M,
Ishimoto S, Ohmori K and Shiono M: Treatment strategies for chronic
expanding hematomas of the thorax. Surg Today. 41:1207–1210. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ueda H, Baba H and Ondo K: Treatment of
chronic expanding hematoma of the thorax with median sternotomy.
Gen Thorac Cardiovasc Surg. 61:466–468. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shimokawa T, Hattori R, Hayashida R and
Hayashi A: Chronic expanding hematoma following pneumonectomy
managed with a thoracic balloon: A case report. Kyobu Geka.
50:417–420. 1997.(In Japanese). PubMed/NCBI
|
|
16
|
Kunisawa S, Kosaka S, Matsukura T,
Nakashima T, Okabayashi T, Miyagawa H and Miyake Y: Chronic
expanding hematoma in sternum resected 5 years after median
sternotomy. Ann Thorac Surg. 85:1447–1448. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Maniwa Y, Okada M, Ishii N, Yoshida M,
Sakamoto T and Harada N: A surgical case for the huge chronic
expanding hematoma developed in the thoracic cavity. Kyobu Geka.
50:1069–1073. 1997.(In Japanese). PubMed/NCBI
|
|
18
|
Kainuma S, Masai T, Yamauchi T, Takeda K,
Iwakura K, Ito H, Abe K and Sawa Y: Chronic expanding
intrapericardial hematoma after coronary artery bypass surgery
presenting with congestive heart failure. Ann Thorac Cardiovasc
Surg. 14:52–54. 2008.PubMed/NCBI
|
|
19
|
Kawachi H, Shirakata S, Niu S, Takahashi
A, Oga K and Oka T: A case of ‘chronic expanding hematoma’, with an
intrapulmonary fresh hemorrhage resected 25 years after thoracic
injury. Nihon Kyobu Geka Gakkai Zasshi. 38:1068–1072. 1990.(In
Japanese). PubMed/NCBI
|
|
20
|
Kouritas VK, Roussakis AG, Soultanis K and
Bellenis I: Extrathoracic chronic heamatoma presenting as a chest
wall tumor 2 years after a blunt thoracic injury. J Cardiothorac
Surg. 6:1562011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kuronuma K, Ootake S, Ikeda K, Taniguchi
M, Takezawa C and Takahashi H: Chronic expanding hematoma in the
chest. Intern Med. 47:1411–1414. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ito T, Nakahara T, Takeuchi S, Uchi H,
Takahara M, Moroi Y and Furue M: Four cases of successfully treated
chronic expanding soft tissue hematoma. Ann Dermatol. 26:107–110.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Friedlander HL and Bump RG: Chronic
expanding hematoma of the calf. A case report. J Bone Joint Surg
Am. 50:1237–1241. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Reid JD, Kommareddi S, Lankerani M and
Park MC: Chronic expanding hematomas. A clinicopathologic entity.
JAMA. 244:2441–2442. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Miyazaki H, Goto A, Hino R, Ota S,
Okudaira R, Murakawa T, Nakajima J and Fukayama M: Pleural cavity
angiosarcoma arising in chronic expanding hematoma after
pneumonectomy. Hum Pathol. 42:1576–1579. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Saotome K, Koguchi Y, Tamai K, Sakai H,
Ohno W and Yamato M: Enlarging intramuscular hematoma and
fibrinolytic parameters. J Orthop Sci. 8:132–136. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pollack A, Zagars GK and Kavadi VS:
Prostate specific antigen doubling time and disease relapse after
radiotherapy for prostate cancer. Cancer. 74:670–678. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Nakamura R, Inage Y, Tobita R, Mori K,
Numata T, Yanai H, Endo T, Ohtani H, Satoh H, Yuzawa K, et al:
Epidermal growth factor receptor mutations: Effect on volume
doubling time of non-small-cell lung cancer patients. J Thorac
Oncol. 9:1340–1344. 2014. View Article : Google Scholar : PubMed/NCBI
|