Introduction
Knee osteoarthritis (OA) is a common disease
associated with tissue inflammation, physical disability and
imbalanced homeostasis in the cartilage. Approximately 25% of
people aged >50 years experience knee pain, articular stiffness
and decreased function due to knee OA (1). At present, various types of surgery are
available for the treatment of knee OA. Arthroscopic surgery is a
minimally invasive surgical procedure and is advocated as one
treatment option for symptomatic relief. The procedure includes
lavage, partial meniscectomy, limited synovectomy, excision of
osteophytes, removal of loose bodies and adhesiolysis (2,3). The
curative effect is satisfactory; however, the long-term efficacy of
arthroscopic surgery in the treatment of knee OA has remained a
topic of controversy amongst clinicians (4,5), since
the surgery may remove cartilage fragments, mechanical irritations,
inflammatory cells and other factors from the joint, but cannot
reverse or repair the knee OA. Therefore, numerous investigators
have sought solutions combining arthroscopic surgery and
viscosupplementation, including steroids and hyaluronan (HA), to
improve outcomes of knee OA (6–10).
However, studies have suggested that the use of
viscosupplementation to repair damaged articular cartilage has
limited efficacy after arthroscopic surgery.
In the past decade, there has been an increasing
interest in the use of ozone injection for the treatment of knee
OA. Ozone is a soluble gas with high oxidative activity, and exerts
an anti-nociceptive effect through several mechanisms (11). Several studies and clinical
experiments have demonstrated that ozone therapy has positive
effects in terms of reducing pain and inflammation, improving
function and benefiting the trophism of bone and cartilage,
increasing vascularization, and increasing repair of the articular
and subchondral bone (12–14). Intra-articular ozone injections are
an effective and low-cost procedure to control pain in knee OA.
Based on this previous work, the aim of the present study was to
investigate whether OA injections exert a beneficial effect on OA
of the knee after arthroscopic surgery.
Materials and methods
Participants
This study was approved by the Ethics Committee of
the Sixth Affiliated Hospital of Guangzhou Medical University and
was performed in accordance with the provisions of the World
Medical Association's Declaration of Helsinki 1995 (revised in
Tokyo, 2004). Due to the retrospective nature of the study, the
Ethics Committee of the Sixth Affiliated Hospital of Guangzhou
Medical University waived the requirement for study participants to
provide informed consent (15).
The inclusion criteria were as follows: i) Patients
with knee OA (Kellgren-Lawrence Grade II or III) (16) with pain ≥4 on the visual analogue
scale (VAS) (17); ii) patients aged
60–80 years; iii) patients for whom any other conservative
treatments had failed (non-anti-inflammatory steroidal drugs,
rehabilitation or physical therapy); and iv) patients with stable
knees without malalignment.
The exclusion criteria were as follows: i) Patients
with severe OA or aged <60 or >80 years; ii) patients with
any systemic, mental or neurological deficiency; iii) patients in
whom any invasive procedure had been applied to the knee or any
intra-articular injection had been administered prior to the
treatment; and iv) patients with any formal contraindication to
ozone therapy (thrombocytopenia, angiotensin-converting enzyme
inhibitor treatment, favism, hyperthyroidism, serious
cardiovascular instability or ozone) or a history of previous ozone
therapy.
The participants of the present study were selected
from a total of 110 patients who had undergone arthroscopic surgery
at the Sixth Affiliated Hospital of Guangzhou Medical University
(Qingyuan, China) between March 2011 and May 2014 and who were
retrospectively evaluated. Among them, 90 patients had been
diagnosed with mild-to-moderate or moderate knee OA
(Kellgren-Lawrence Grade II or III) and met the enrolment criteria
of the study. Following arthroscopic surgery, the patients were
divided into two groups according to the type of treatment
administered. In the ozone group, patients received 20 ml of 20
µg/ml ozone as intra-articular injections after arthroscopic
surgery, while another group who did not receive any
intra-articular ozone injection served as a control group. The
intra-articular ozone injections were performed once per week for 4
consecutive weeks, starting 2 weeks after surgery. The mean
duration of follow-up was 13.7 months and the minimum follow-up
duration was 12 months. In the ozone group, 6 patients were lost to
follow-up and 4 cases were lost to follow-up in the control group.
At the final follow-up, there were 42 patients in the ozone group
and 38 in the control group. All arthroscopic surgeries and
injections were performed by the same experienced physicians. Data
on endpoints were collected prior to arthroscopic surgery and at 6
weeks and 3, 6 and 12 months after arthroscopic surgery.
Demographic data and all post-operative outcome data were obtained
from patient records (Fig. 1).
Arthroscopic surgical procedure
The standard arthroscopic debridement was performed
under spinal or general anesthesia. The procedure in these patients
included lavage of the joint with varying amounts of serum saline
solution, and debridement of roughened surfaces with removal of
loose debris. Meniscal tears were often resected and only loose
unstable fragments were repaired, while carefully preserving as
much meniscal tissue as possible. Loose bodies were removed as
required. According to the protocol specifications, all patients
received the same analgesic and exercise program after surgery.
Celecoxib (200 mg) was administered orally as an analgesic
supplement from postoperative 3 h and was repeated every 8 h until
2 days post-operation if the recorded VAS score was ≥4. The total
celecoxib consumption after the operation was also recorded.
Intra-articular injection
procedure
The patient was placed in a supine position with the
knee in an extended position. The knee to be punctured was
subjected to an anti-sepsis procedure with iodine. After the
patella had been located, its medial margin was pressed to
subluxation in the lateral margin to increase the articular rim as
much as possible. A 22-gauge needle was inserted along the
superlateral margin of the patella into the suprapatellar pouch
without ultrasound or other imaging guidance. Physicians ensured
that the needle was not inside a blood vessel by aspirating the
syringe. The ozone generator (Herrmann, Germany) was set to produce
ozone (O3) from O2 at a concentration of 20
µg/ml. A 20-ml syringe was connected to the exit of the generator
and 20 ml of the produced gas was drawn into the syringe. Before
the injection of gas (18), 2 ml 1%
lidocaine was injected into the knee. Lidocaine was administered to
reduce the burning pain felt in the knee during gas injection,
which lasted several minutes.
Outcome measures
The efficacy of the treatment was evaluated using
the VAS (17), Lequesne index
(19), and Western Ontario and
McMaster University Osteoarthritis Index (WOMAC) questionnaires
(20). In the VAS, the proband
selects a whole number on a scale of 0–10, with 10 representing
severe pain and 0 representing the absence of pain. The Lequesne
index consists of 10 specific questions, including 5 items
associated with pain or discomfort, 1 item associated with the
maximum distance walked and 4 items associated with daily life
activities. The score ranges from 0 to 24 points. The WOMAC scale
consists of 24 questions that evaluate pain, stiffness and physical
function during daily life activities, and each question has five
response choices (none, mild, moderate, severe and extreme); the
subtotal scores for pain (5 items), stiffness (2 items) and
physical function (17 items) range from 0–20, 0–8 and 0–68,
respectively, and the sum of all the points generates a value
between 0 and 96 inclusive. Higher values indicate a worse patient
condition. At the 12-month follow-up, the patient's overall
impression of the treatment outcome was measured by a clinical
global impression (CGI), including a 5-point ordinal scale (1,
excellent; 2, good; 3, satisfactory; 4, unchanged; 5, worse).
Statistical analysis
Statistical analyses were performed using the SPSS
version 19.0 software package (IBM Corp., Armonk, NY, USA). Values
are expressed as the mean ± standard deviation or sample
proportions unless specified otherwise. To assess the normality of
the data distributions, the data were compared using a
Kolmogorov-Smirnov test. Quantitative data were compared between
the two groups using an independent-samples t-test. The Chi-square
test was used to assess the differences between the two groups in
terms of qualitative data. To compare quantitative variables within
each group prior to and after treatment, one-way analysis of
variance with the LSD post hoc test was used. P<0.05 was
considered to indicate a statistically significant difference.
Results
Demographic characteristics of the
patients
A total of 80 patients (mean age, 71.5 years; age
range, 60–80 years) with symptomatic knee OA (Kellgren-Lawrence
grade II or III), comprising 42 patients in the ozone group and 38
in the control group, were enrolled in the present study. The two
groups were comparable in terms of baseline demographics and
disease profile, and there were no statistically significant
differences between the groups (Table
I). After ozone injection, 5 patients in the ozone group
experienced a mild pain accompanied by erythema; the pain
disappeared within a few minutes.
 | Table I.Comparison of demographic data as well
as VAS, Lequesne and WOMAC scores at baseline between the Ozone and
Control groups. |
Table I.
Comparison of demographic data as well
as VAS, Lequesne and WOMAC scores at baseline between the Ozone and
Control groups.
| Parameter | Ozone group
(n=42) | Control group
(n=38) | P-value |
|---|
| Agea (± SD) | 68.83±5.56 | 69.63±4.96 | 0.502 |
| Median
(range) | 69 (60–79) | 71 (60–77) |
|
| Sexb |
|
| 0.408 |
| Male | 17 (40.5) | 12 (31.6) |
|
|
Female | 25 (59.5) | 26 (68.4) |
|
| Kneeb |
|
| 0.888 |
|
Right | 27 (64.3) | 25 (65.8) |
|
| Left | 15 (35.7) | 13 (34.2) |
|
| Knee OA
gradeb |
|
| 0.866 |
| Grade
II | 24 (57.1) | 21 (55.3) |
|
| Grade
III | 18 (42.9) | 17 (44.7) |
|
| VAS
(initial)a | 7.52±1.57 | 7.66±1.32 | 0.682 |
| Lequesne
(initial)a | 15.07±3.82 | 14.26±2.64 | 0.280 |
| WOMAC
(initial)a |
|
|
|
| Pain | 12.36±2.79 | 13.55±3.45 | 0.091 |
|
Stiffness | 2.95±1.75 | 3.32±2.04 | 0.394 |
| Physical
function | 55.12±6.99 | 57.45±6.16 | 0.120 |
|
Total | 70.43±8.37 | 73.68±10.07 | 0.119 |
VAS, Lequesne index and WOMAC
scores
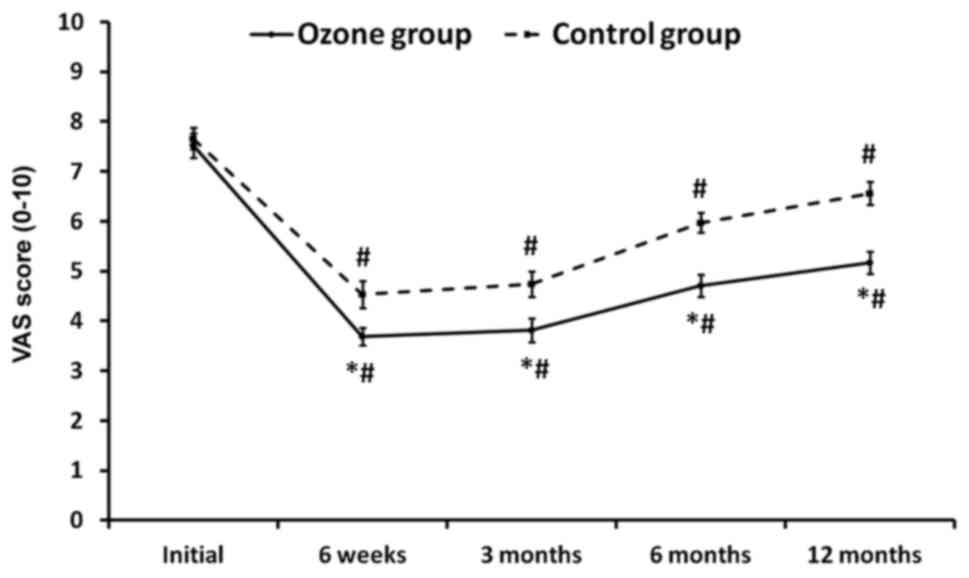
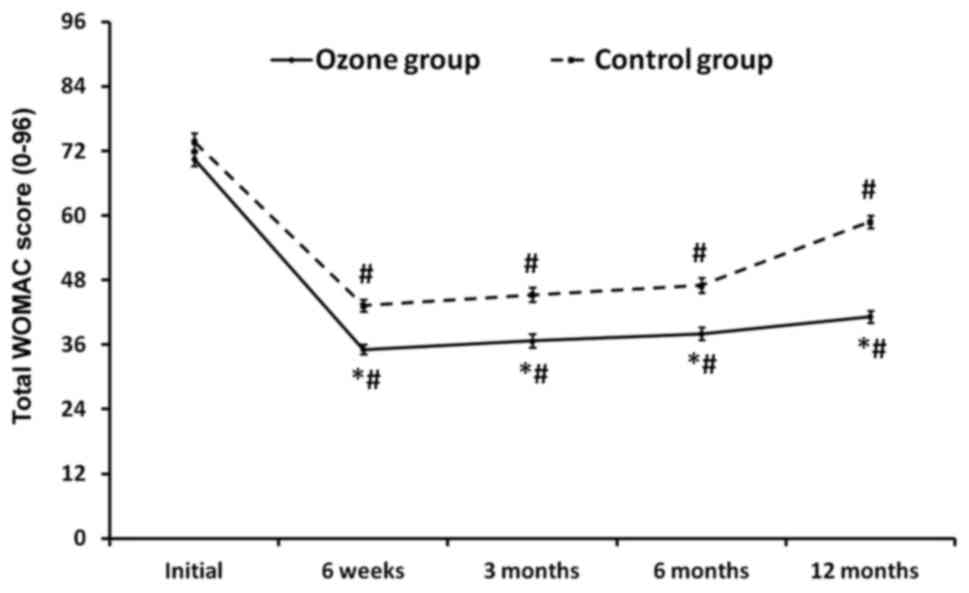
Although the two groups had comparable baseline
values, the VAS scores, Lequesne index scores, and the WOMAC-pain,
WOMAC-stiffness, WOMAC-function and total WOMAC scores were
significantly better in the ozone group than those in the control
group at all post-operative follow-up time-points (P<0.05;
Table II; Figs. 2–4).
The lower pain observed in the ozone group in the short term may be
due to injection of Lidocaine into the joint during ozone
administration. Of note, those differences were maintained even at
1 year post surgery. With regard to pain intensity, it was observed
that the VAS scores significantly decreased from 7.52 prior to
treatment to 5.17 at the 12-month follow-up in the ozone group,
whereas in the control group, the VAS scores decreased from 7.66 to
6.56 (Table II; Fig. 2). The Lequesne Index improved from
15.07 to 8.74 in the ozone group and from 14.26 to 10.08 in the
control group at the 12-month follow-up (Table II; Fig.
3). Furthermore, the WOMAC-pain, WOMAC-stiffness and
WOMAC-function scores for the ozone group were significantly
decreased from 12.36 to 6.71, 2.95 to 2.14 and 55.12 to 32.76,
respectively. In the control group, the same scores decreased from
15.9 to 4.4, 3.32 to 2.68 and 57.45 to 37.87, respectively. The
total WOMAC score decreased from 70.43 to 41.19 in the ozone group,
and from 73.68 to 58.84 in the control group at the 12-month
follow-up (Table II; Fig. 4). No significant difference in the
WOMAC-stiffness score was observed after surgery at the 6 and
12-month follow-up assessments compared with pretreatment in the
control group (Table II).
 | Table II.VAS, Lequesne and WOMAC scores in the
Ozone and Control groups at Baseline, at 6 weeks and at 3, 6 and 12
months after treatment. |
Table II.
VAS, Lequesne and WOMAC scores in the
Ozone and Control groups at Baseline, at 6 weeks and at 3, 6 and 12
months after treatment.
|
|
|
| WOMAC |
|---|
|
|
|
|
|
|---|
|
Time-point/group | VAS | Lequesne | Pain | Stiffness | Physical
function | Total |
|---|
| Baseline |
|
|
|
|
|
|
| Ozone
group | 7.52±1.57 | 15.07±3.82 | 12.36±2.79 | 2.95±1.75 | 55.12±6.99 | 70.43±8.37 |
| Control
group | 7.66±1.32 | 14.26±2.64 | 13.55±3.45 | 3.32±2.04 | 57.45±6.16 | 73.68±10.07 |
|
P-valuea | 0.682 | 0.280 | 0.091 | 0.394 | 0.120 | 0.119 |
| 6 weeks |
|
|
|
|
|
|
| Ozone
group | 3.69±1.14 | 5.86±2.40 | 4.90±2.25 | 1.67±1.12 | 28.55±5.00 | 35.12±6.23 |
| Control
group | 4.53±1.67 | 7.89±2.71 | 6.97±2.45 | 2.42±1.31 | 33.84±6.26 | 43.24±7.08 |
|
P-valuea | 0.010 | 0.001 | <0.001 | 0.008 | <0.001 | <0.001 |
|
P-valueb | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
|
P-valuec | <0.001 | <0.001 | <0.001 | 0.014 | <0.001 | <0.001 |
| 3 months |
|
|
|
|
|
|
| Ozone
group | 3.81±1.57 | 6.02±2.05 | 5.69±2.32 | 2.00±1.12 | 28.98±7.35 | 36.67±8.11 |
| Control
group | 4.74±1.54 | 8.97±2.14 | 7.71±2.04 | 2.61±1.33 | 34.82±7.61 | 45.29±8.51 |
|
P-valuea | 0.009 | 0.046 | <0.001 | 0.034 | <0.001 | <0.001 |
|
P-valueb | <0.001 | <0.001 | <0.001 | 0.002 | <0.001 | <0.001 |
|
P-valuec | <0.001 | <0.001 | <0.001 | 0.049 | <0.001 | <0.001 |
| 6 months |
|
|
|
|
|
|
| Ozone
group | 4.71±1.42 | 7.19±2.24 | 5.83±1.81 | 2.25±1.47 | 29.95±6.67 | 38.02±7.66 |
| Control
group | 5.97±1.23 | 9.21±2.04 | 7.95±1.90 | 2.76±1.56 | 36.50±8.77 | 47.00±8.70 |
|
P-valuea | <0.001 | 0.037 | <0.001 | 0.042 | <0.001 | <0.001 |
|
P-valueb | <0.001 | <0.001 | <0.001 | 0.021 | <0.001 | <0.001 |
|
P-valuec | <0.001 | <0.001 | <0.001 | 0.126 | <0.001 | <0.001 |
| 12 months |
|
|
|
|
|
|
| Ozone
group | 5.17±1.43 |
8.74±2.89 | 6.71±2.38 | 2.33±1.37 | 32.76±6.64 | 41.19±7.64 |
| Control
group | 6.76±1.45 | 10.08±3.03 | 8.55±2.44 | 2.68±1.47 | 37.87±6.96 | 58.84±7.48 |
|
P-valuea | <0.001 | 0.046 | <0.001 | 0.047 | 0.001 | <0.001 |
|
P-valueb | <0.001 | <0.001 | <0.001 | 0.032 | <0.001 | <0.001 |
|
P-valuec | 0.008 | <0.001 | <0.001 | 0.080 | <0.001 | <0.001 |
CGI scores
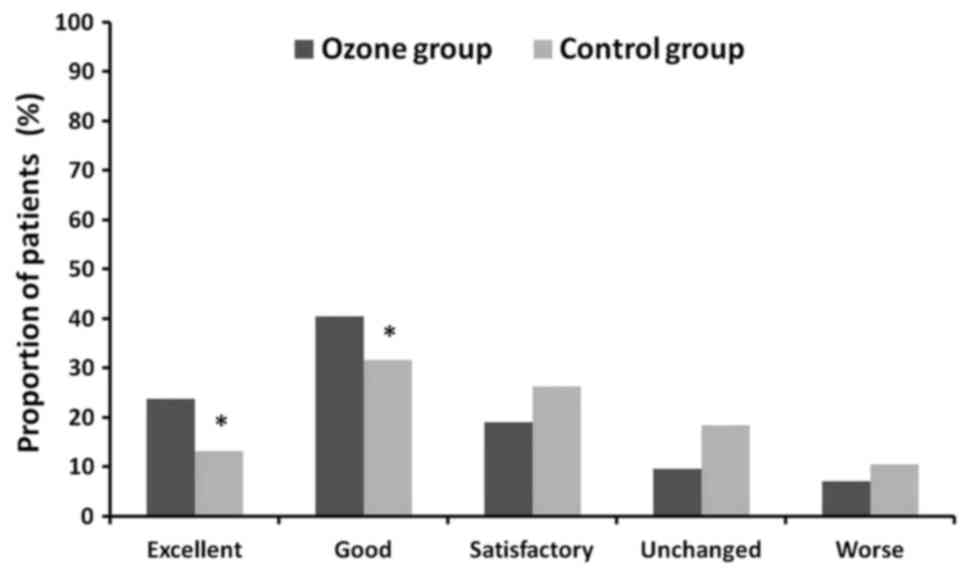
At the end of the follow-up of at least 12 months,
based on the CGI, the treatment outcome was rated as excellent in
10 (23.8%), good in 17 (40.5%), satisfactory in 8 (19.0%),
unchanged in 4 (9.5%) and worse in 3 (7.1%) patients in the ozone
group. In the control group, the treatment outcome was rated as
excellent in 5 (13.2%), good in 12 (31.6%), satisfactory in 10
(26.3%), unchanged in 7 (18.4%) and worse in 4 (10.5%) patients
(Fig. 5). Analysis of the
physician's CGI scores at the 12-month follow-up indicated that a
significantly higher number of patients in the ozone group had been
assigned better CGI grades (excellent and good) compared with that
in the control group (P<0.05).
Discussion
Knee OA is a degenerative disease that leads to
painful joints, articular stiffness and decreased function. At
present, no cure is available for knee OA, and the major objectives
of treatment are the relief of symptoms, including pain, stiffness
and swelling, improvement of function and limitation of joint
damage leading to the destruction of the joint. The pathophysiology
of knee OA is complex, and is characterized by the wearing of the
articular cartilage with subsequent damage to the bones and
increased matrix degradation. Most orthopedic surgeons include
arthroscopic surgery as a treatment modality for patients with mild
or moderate knee OA. Arthroscopic surgery for knee OA may delay
joint degeneration to maintain moderate activity and allow for
future reconstruction, particularly for patients with mild to
moderate OA (21,22). However, the treatment cannot reverse
or stop the pathological process of OA or prevent its continuous
development. Therefore, its long-term effects are less than ideal.
In the present study, it was also demonstrated that the efficacy of
arthroscopic treatment for patients with knee OA of
Kellgren-Lawrence Grade II or III had no obvious effect in joints
stiffness after 6 months of follow-up in the control group.
Treatment approaches combining arthroscopic surgery with
viscosupplementation have been trialed to improve the outcomes of
knee OA. For instance, treatment combining arthroscopic surgery and
hyaluronic acid has been widely used. Hempfling (8) reported that the post-arthroscopic
instillation of 0.5% sodium hyaluronate into the joint is a
suitable method for achieving long-term stabilization of the
treatment outcome. Mathies (7)
performed a study examining the outcomes of the use of 0.5% sodium
hyaluronate immediately after arthroscopic surgery. This study
indicated that the use of 0.5% sodium hyaluronate may be of benefit
in reducing post-operative pain and swelling. In addition, Huskin
et al (23) reported that
viscosupplementation with hylan G-F 20 had a favorable risk-benefit
profile in patients with symptomatic knee OA after arthroscopic
meniscectomy and/or debridement of the knee in a patient with
chondral disease.
Although ozone has been widely used for the
treatment of orthopedic diseases, at present there is no unanimous
protocol for ozone treatment in knee OA (12,14,24). It
is a gas that is highly soluble in biological fluids, where atomic
oxygen acts as a highly reactive species. After injection into a
joint capsule, ozone is able to reduce inflammation, improve
function and benefit the trophism, vascularization and repair of
articular and subchondral bone. The biological mechanism of action
of ozone therapy for knee OA is thought to be based on the
biological effects elicited by ozone, including reactive oxygen
species (ROS) and lipid oxidation products (LOPs) (12–14). It
is considered that ROS and LOPs may inhibit the release of
proteolytic enzymes or proinflammatory cytokines and stimulate the
proliferation of fibroblasts and chondrocytes with increased
synthesis of the matrix and articular cartilage (25). A randomized controlled trial
comparing intra-articular injection of platelet-rich plasma,
hyaluronic acid and ozone into the knee of OA patients indicated
comparable effects on pain reduction among the three approaches
after 1 month of treatment (26).
Hashemi et al (18) reported
that there was no significant difference in VAS and WOMAC scores
between intra-articular dextrose and ozone treatment in patients
with mild to moderate knee OA in the short term. Recently,
Chansoria et al (27)
indicated that in a randomized controlled trial, intra-articular
injection of a combination of ozone and steroids in patients with
primary knee OA resulted in a better outcome in terms of pain
relief and functional improvements than that achieved with ozone
alone. Several studies have indicated that intra-articular ozone
injection for knee OA is a safe and effective treatment with a low
risk of complications. In a single-blinded, controlled study
comprising 84 patients, Invernizzi et al (28) demonstrated that in terms of safety,
intra-articular ozone treatment is comparable to intra-articular
sodium hyaluronate in chronic knee OA. In the present study, no
serious complications occurred in the ozone treatment group. Only 5
patients felt a mild pain after the injection, which disappeared
within a few minutes. This side effect was also reported by Lopes
de Jesus et al (29).
The present study revealed that ozone treatment
reduced pain, as measured by the VAS. It also improved the quality
of life measured by the Lequesne Index score and total WOMAC score
in the ozone group. These significant changes demonstrate the
effectiveness of ozone therapy in reducing pain, and improving
function and quality of life of these patients post-surgery. The
positive results of intra-articular ozone injection for knee OA are
further supported the results of Lopes de Jesus et al
(29). Another recent study by
Fernández-Cuadros et al (30)
indicated that ozone treatment decreases the VAS, as well as the
WOMAC-pain, WOMAC-stiffness and WOMAC-function scores in patients
with knee OA. The present study also indicated that the ozone group
had a significantly greater improvement in pain and function than
the control group, according to the VAS, Lequesne index and WOMAC
function scores. Based on the CGI score at the 12-month follow-up,
64.3% of the patients obtained excellent or good results in the
ozone group. By contrast, only 42.1% of the patients obtained
excellent or good results in the control group. The reason for the
favorable long-term effects in the ozone group may be that ozone
promotes better vascularization in bones and cartilage, and
accelerating anabolism and recovery in osteoarticular diseases
(12). However, the exact mechanism
of action of ozone therapy in knee OA has remained to be fully
elucidated, and further studies are required to confirm the results
and the long-term outcome.
The present study had several limitations. First, it
was limited by the small sample size, and lidocaine was not
injected into the knee in the control group, which may have
affected the results. It will be necessary to expand the sample
size and perform rigorous prospective studies in the future.
Furthermore, the present study only recruited patients with
Kellgren-Lawrence grade II or III OA, so the results are difficult
to generalize to all OA populations that have different degrees of
radiographically evident severity. In addition, the present study
only investigated the clinical symptomatic changes, and no imaging
features of knee OA were studied.
In conclusion, the results of the present study
demonstrated the efficacy of intra-articular ozone injections after
arthroscopic surgery in relieving pain and improving physical
function in knee OA of Kellgren-Lawrence grade II or III. However,
the present results should be looked at with caution and require
further validation in larger cohorts.
Acknowledgements
The authors wish to thank Yingchao Han from the
Department of Orthopedics (Renji Hospital, Shanghai Jiao Tong
University School of Medicine, China) for performing the
statistical analysis.
Funding
This study was funded by the Sixth Affiliated
Hospital of Guangzhou Medical University (Guangzhou, China; grant
no. A2016222).
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
DC and XW conceived and designed the study. XW, GW
and CL performed the experiments. XW wrote the paper. DC, XW, GW
and CL reviewed and edited the manuscript. XW and CL analysed the
data. All authors read and approved the manuscript and agree to be
accountable for all aspects of the research in ensuring that the
accuracy or integrity of any part of the work are appropriately
investigated and resolved.
Ethical approval and consent to
participate
This study was approved by the Ethics Committee of
the Sixth Affiliated Hospital of Guangzhou Medical University
(Guangzhou, China) and performed in accordance with the provisions
of the World Medical Association Declaration of Helsinki 1995
(revised in Tokyo, 2004). Due to the retrospective nature of the
study, the Ethics Committee of the Sixth Affiliated Hospital of
Guangzhou Medical University (Guangzhou, China) waived the
requirement for study participants to provide informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hawamdeh M Z and Al-Ajlouni JM: The
clinical pattern of knee osteoarthritis in jordan: A hospital based
study. Int J Med Sci. 10:790–795. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pearse EO and Craig DM: Partial
meniscectomy in the presence of severe osteoarthritis does not
hasten the symptomatic progression of osteoarthritis. Arthroscopy.
19:963–968. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hunt SA, Jazrawi LM and Sherman OH:
Arthroscopic management of osteoarthritis of the knee. J Am Acad
Orthop Surg. 10:356–363. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jackson RW and Dieterichs C: The results
of arthroscopic lavage and debridement of osteoarthritic knees
based on the severity of degeneration: A 4- to 6-year symptomatic
follow-up. Arthroscopy. 19:13–20. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Figueroa D, Calvo R, Villalón IE, Meleán
P, Novoa F and Vaisman A: Clinical outcomes after arthroscopic
treatment of knee osteoarthritis. Knee. 20:591–594. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Forster MC and Straw R: A prospective
randomized trial comparing intra-articular hyalgan injection and
arthroscopic washout for knee osteoarthritis. Knee. 10:291–293.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mathies B: Effects of viscoseal, a
synovial fluid substitute, on recovery after arthroscopic partial
meniscectomy and joint lavage. Knee Surg Sports Traumatol Arthrosc.
14:32–39. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hempfling H: Intra-articular hyaluronic
acid after knee arthroscopy: A two-year study. Knee Surg Sports
Traumatol Arthrosc. 15:537–546. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ulucay C, Altintas F, Ugutmen E and Beksaç
B: The use of arthroscopic debridement and viscosupplementation in
knee osteoarthritis. Acta Orthop Traumatol Turc. 41:337–342.
2007.(In Turkish). PubMed/NCBI
|
|
10
|
Zietz PM and Selesnick H: The use of hylan
G-F 20 after knee arthroscopy in an active patient population with
knee osteoarthritis. Arthroscopy. 24:416–422. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bocci V: Ozone as Janus: This
controversial gas can be either toxic or medically useful.
Mediators Inflamm. 13:3–11. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fernandez-Cuadros ME, Perez-Moro OS and
Mirón-Canelo JA: Could ozone be used as a feasible future treatment
in osteoarthritis of the knee? Diversity Equal Health Care.
13:232–239. 2016.
|
|
13
|
Swapan ΚΜ, Rajesh P, Pallab D, Partha PD,
Asim KP, Jayanta R, Halder N and Rathindra NH: Role of
intra-articular ozone in osteo-arthritis of knee for functional and
symptomatic improvement. Ind J Phys Med Rehabil. 22:65–69.
2011.
|
|
14
|
Borrelli E, Alexandre A, Iliakis E,
Alexandre A and Bocci V: Disk herniation and knee arthritis as
chronic oxidative stress disieases: The therapeutic role of oxygen
ozone therapy. J Arthritis. 4:1612015.
|
|
15
|
Zhang JF, Zhan XQ, Hu HW, Yang Q and Wang
XH: Clinical results of medical ozone combined with sodium
hyaluronate for knee osteoarthritis. Orthop J China. 5:362–365.
2010.(In Chinese).
|
|
16
|
Kellgren JH and Lawrence JS: Radiological
assessment of osteo arthrosis. Ann Rheum Dis. 16:494–502. 1957.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Price DD, McGrath PA, Rafii A and
Buckingham B: The validation of visual analogue scales as ratio
scale measures for chronic and experimental pain. Pain. 17:45–56.
1983. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hashemi M, Jalili P, Mennati S, Koosha A,
Rohanifar R, Madadi F, Razavi SS and Taheri F: The effects of
prolotherapy with hypertonic dextrose versus prolozone
(intraarticular ozone) in patients with knee osteoarthritis. Anesth
Pain Med. 5:e275852015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lequesne MG: The algofunctional indices
for hip and knee osteoarthritis. J Rheumatol. 24:779–781.
1997.PubMed/NCBI
|
|
20
|
Bellamy N, Buchanan WW, Goldsmith CH,
Campbell J and Stitt LW: Validation study of WOMAC: a health status
instrument for measuring clinically important patient relevant
outcomes to antirheumatic drug therapy in patients with
osteoarthritis of the hip or knee. J Rheumatol. 15:1833–1840.
1988.PubMed/NCBI
|
|
21
|
Aaron RK, Skolnick AH, Reinert SE and
Ciombor DM: Arthroscopic debridement for osteoarthritis of the
knee. J Bone Joint Surg Am. 88:936–943. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shin CS and Lee JH: Arthroscopic treatment
for osteoarthritic knee. Knee Surg Relat Res. 24:187–192. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Huskin JP, Vandekerckhove B, Delincé P,
Verdonk R, Dubuc JE, Willems S, Hardy P, Blanco FJ, Charrois O and
Handelberg F: Multicentre, prospective, open study to evaluate the
safety and efficacy of hylan G-F 20 in knee osteoarthritis subjects
presenting with pain following arthroscopic meniscectomy. Knee Surg
Sports Traumatol Arthrosc. 16:747–752. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Calunga J L, Menéndez S, León R, Chang S,
Guanche D, Balbín A, Zayas J and García P: Application of ozone
therapy in patients withknee osteoarthritis. Ozone: Science &
Engineering. 34:469–475. 2012. View Article : Google Scholar
|
|
25
|
Bocci VA: Scientific and medical aspects
of ozone therapy. State of the art. Arch Med Res. 37:425–435. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Duymus TM, Mutlu S, Dernek B, Komur B,
Aydogmus S and Kesiktas FN: Choice of intra-articular injection in
treatment of knee osteoarthritis: Platelet-rich plasma, hyaluronic
acid or ozone options. Knee Surg Sports Traumatol Arthrosc.
25:485–492. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chansoria M, Upadhyay S, Panwar S,
Shivhare P and Vyas N: Comparative efficacy of intraarticular
injection of combination of ozone and steroid and ozone alone in
patients with primary knee osteoarthritis: A prospective,
randomized clinical analysis. J Recent Adv Pain. 2:11–14. 2016.
View Article : Google Scholar
|
|
28
|
Invernizzi M, Stagno D, Carda S, Grana E,
Picelli A, Smania N, Cisari C and Baricich A: Safety of
intra-articular oxygen-ozone therapy compared to intra-articular
sodium hyaluronate in knee osteoarthritis: A randomized single
blind pilot study. Int J Phys Med Rehabil. 5:3852017.
|
|
29
|
de Jesus Lopes CC, Dos Santos FC, de Jesus
LMOB, Monteiro I, Sant'Ana MSSC and Trevisani VFM: Comparison
between intra-articular ozone and placebo in the treatment of knee
osteoarthritis: A randomized, double-blinded, placebo-controlled
study. PLoS One. 12:e01791852017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fernández-Cuadros ME, Pérez-Moro OS,
Albaladejo-Florin MJ, et al: Ozone improves pain, function and
quality of life in patients with knee osteoarthritis: A prospective
quasi-experimental before-after study. Middle East J Rehabil
Health. 4:e418212017.
|