Introduction
Congenital cardiovascular abnormalities and
respiratory diseases are two tightly linked entities. Although
respiratory diseases, particularly infections, are common in
children, occasionally, they may be life-threatening if those
suffering from congenital cardiovascular abnormalities are affected
(1). Furthermore, ≥3% of children
with cardiac disease also exhibit airway issues, including
tracheobronchomalacia and airway narrowing, which are known to be
latent causes and aggravating factors of persistent and recurrent
lower respiratory infections (2,3). A rapid
and accurate diagnosis is essential for the initiation of
appropriate treatment in children presenting both pulmonary
diseases and congenital cardiovascular abnormalities (1). Determining whether these children
suffer from respiratory complications such as airway anomalies may
prove valuable for future preoperative planning and counseling of
their families (4).
Flexible bronchoscopy (FB) is a crucial and safe
technique for the evaluation of pulmonary diseases, allowing
assessment of anatomy, dynamics of airways, and determination of
pathogens via bronchoalveolar lavage (BAL) fluid (BALF)
examinations (3,5). With respect to certain airway
abnormalities, such as tracheomalacia and cartilage rings, FB
persists as the ‘gold standard’ method of diagnosis (6,7). In
addition, previous studies have demonstrated its potential in
evaluating patients with diseases of cardiovascular and
gastrointestinal systems (1,4,6,7).
Although FB has been performed in China for over 20
years, sufficient data describing the role of FB in evaluating lung
and airway diseases in children with congenital cardiovascular
abnormalities remains scarce. In 2009, a study solely focused on
airway compression complicated with excessive vessel abnormalities
was performed (7). Another study
summarized the bronchoscopy-associated diagnoses in children with
the congenital cardiac disease without an in-depth analysis
(4).
The present study aimed to investigate the features
of children with congenital cardiovascular abnormalities who
underwent FB due to pulmonary problems. The bronchoscopy findings,
and cellular and culture results are presented, and were analyzed
to assess the role of FB in guiding preoperative planning, and
evaluate the safety of the procedures in those children.
Materials and methods
Patients
The present study was carried out at West China
Second University Hospital, Sichuan University (Chengdu, China). A
review of medical records of all pediatric patients with congenital
cardiovascular abnormalities who underwent FB between November 1,
2013 and June 31, 2015 was conducted. A total of 57 patients
(male:female, 29:28; age, 9 days-9 years) were included. In order
to fulfill the inclusion criteria, patients should have suffered
from confirmed congenital cardiovascular abnormalities and
pulmonary diseases (as indicated in Table I and Fig.
1) that were indicated for FB. The exclusion criteria were as
follows: Patients with incomplete records and those whose parents
or guardians refused to allow participation in the study.
 | Table I.Characteristics of patients undergoing
bronchoscopy according to cardiovascular disorders. |
Table I.
Characteristics of patients undergoing
bronchoscopy according to cardiovascular disorders.
| Type of
cardiovascular disorders | Patients, n (%) | Median age,
years | Sex ratio,
male/female | Body weight, kg | Mechanically
ventilated, n |
|---|
| ASD | 24 (42.2) | 0.46 | 14/10 | 6.23±2.71 | 3 |
| VSD | 11 (19.3) | 0.25 | 5/6 | 4.65±1.73 | 2 |
| PDA | 8 (14.0) | 0.28 | 5/3 | 5.11±2.23 | 1 |
| VSD+ASD | 4 (7.0) | 0.17 | 0/4 | 9.35±11.12 | 1 |
| TOF | 2 (3.5) | 0.42 | 0/2 | 6.55±0.21 | 0 |
| Other | 8 (14.0) | 0.79 | 3/5 | 7.73±3.22 | 2 |
| Total | 57 (100.0) | 0.33 | 29/28 | 6.21±3.71 | 9 |
Cardiovascular abnormalities were evaluated via
transthoracic echocardiography (GE Vivid E9 Cardiovascular
Ultrasound System; GE Healthcare, Chicago, IL, USA). Magnetic
resonance angiography (MRA; Achieva 1.5T Magnetic Resonance
Diagnostic Device; Philips Medical Systems B.V., Eindhoven, The
Netherlands) indicated the suspected vessel abnormalities. Cardiac
diagnoses were made by pediatric cardiologists based on clinical,
transthoracic echocardiography, or MRA findings.
The Institutional Review Board/Ethics Committee
affiliated with West China Second University Hospital, Sichuan
University approved the current study, which was performed in
accordance with the ethical standards of the Declaration of
Helsinki. Parents or guardians of all patients provided written,
informed consent prior to the procedures.
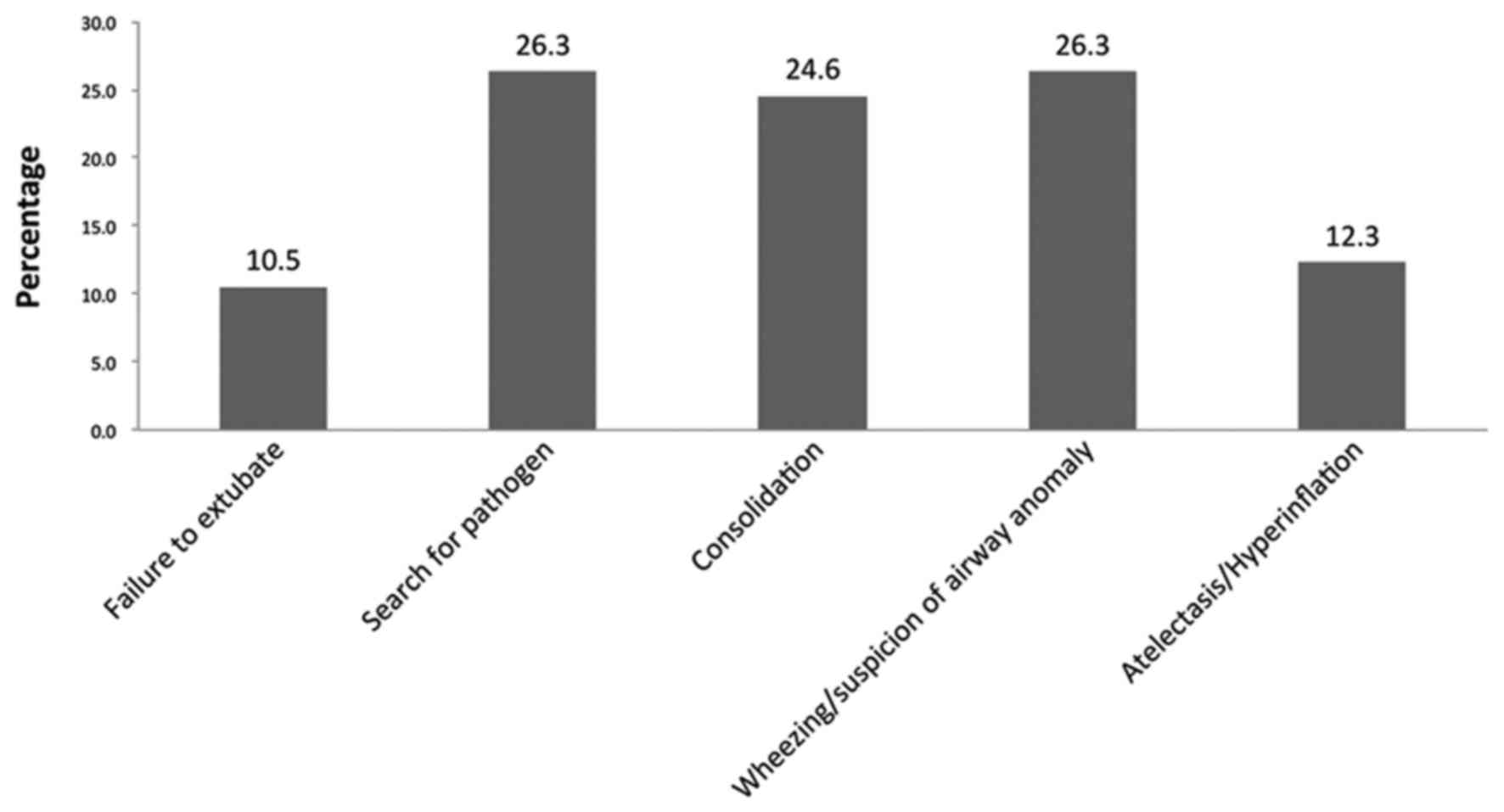
Indications for FB
All patients were hospitalized and exhibited
pneumonia. The indications for FB were as follows: Failure to
extubate in 6 patients, searching for pathogens in 15 patients,
consolidation in 14 patients, wheezing or suspicion of airway
anomaly in 15 patients, and persistent atelectasis or
hyperinflation in 7 patients (Fig.
1). Failure to extubate was defined as two or more failed
attempts to extubate or failing to meet the criteria for extubating
(2).
Procedure of FB and bronchoalveolar
lavage
All patients were evaluated by a pediatric
pulmonologist. FB was performed at the West China Second University
Hospital, Sichuan University by three experienced attending
pediatric pulmonologists using a bronchoscope (P260F or XP260F;
Olympus Corporation, Tokyo, Japan) in the Bronchoscopy Room, apart
from 8 patients who were supported by mechanical ventilation, who
underwent FB in the pediatric intensive care unit. Procedures were
performed in compliance with the Chinese Guide To Pediatric
Bronchoscopy (8). Patients were
sedated with intravenous midazolam (Jiangsu Nhwa Pharmaceutical
Co., Ltd., Jiangsu, China; 0.1–0.3 mg/kg). Topical anesthesia with
1% lidocaine (5–7 mg/kg) was administered via the nose, vocal
cords, trachea, and bronchus. The transnasal approach was used in
all patients who were not intubated, whereas the endotracheal
approach was utilized in those who were intubated and mechanically
ventilated (8).
During the procedure, vital signs and pulse oxygen
saturation of all patients were continuously monitored and recorded
as continuous oxygen was delivered. BAL was performed in the
abnormal region identified during physical examination, radiography
or chest computed tomography (CT) scan, or in the right middle or
left lingual lobe when no localization signs were present. Normal
saline solution (1 ml/kg, three times) was instilled followed by
immediate aspiration of the fluid into a sterile container. BALF
was further subjected to cellular analysis, Gram- and acid-fast
staining, bacterial culture, fungal smear, and culture as
previously described (9,10).
Data collection and outcome
measures
Data was obtained by reviewing the medical records,
managed with Microsoft Office Excel 2016 (Microsoft Corporation,
Redmond, WA, USA) and described as frequencies. The demographics,
results of radiography and transthoracic echocardiography,
bronchoscopy diagnoses, results of the cellular analysis, and
microbiology of BALF were recorded. Bronchoscopy diagnoses were
made by direct observation of airways by at least two of the
aforementioned experienced attending pediatric pulmonologists.
Disagreements between observers were resolved by consensus.
Clinically valuable contributions (defined as bronchoscopy
diagnosis leading to altered antimicrobial treatment, assistance in
preoperative planning and resolution of atelectasis) were analyzed.
The putative side effects of FB such as fever, hemorrhage,
arrhythmia, and sudden death were also recorded meticulously.
Results
Characteristics of patients
A total of 57 patients with congenital
cardiovascular abnormalities combined with pulmonary diseases were
enrolled in the present study and a bronchoscopy was performed on
each patient during the study period. The cohort comprised of 29
male and 28 female patients, and the median age was 4 months
(range, 9 days-9 years). The number of patients aged <29 days,
29 days-1 year, and >1 year were 4 (7.0%), 43 (75.4%), and 10
(17.6%), respectively. A total of 9 patients (15.8%) who were under
mechanical ventilation underwent FB through the endotracheal tube,
whereas the other 48 patients (84.2%) were examined via the
transnasal approach. The most common type of congenital
cardiovascular abnormality was atrial septal defect (ASD; 24/57,
42.2%), followed by ventricular septal defect (VSD; 11/57, 19.3%)
and patent ductus arteriosus (PDA; 8/57, 14.0%). In addition, 2
cases with Tetralogy of Fallot (TOF; 2/57, 3.5%) were enrolled.
Other types of cardiovascular disorders consisted of 1 case of
stenosis of aortic arch, 1 of dilated vena coronaria and a patent
foramen ovale, 2 of pulmonary slings and ASD, 2 of total anomalous
pulmonary venous connection (TAPVC), 1 of complete vascular ring,
and 1 of VSD combined with ASD and PDA. A total of 2 patients with
TAPVC and 1 with VSD plus ASD underwent open-chest surgery and
interventional operation, respectively, prior to FB. The
characteristics of patients who underwent FB according to the
cardiovascular abnormalities are presented in Table I.
Bronchoscopy findings
The primary findings of FB were signs of infection
(57/57, 100%) such as increased secretion, mucosal hyperemia, and
edema of airways, which coincided with that of pneumonia. In
addition, the second most common findings were disorders associated
with airway abnormalities, including 19 cases of external
compression of airways (33.3%), tracheobronchomalacia in 16 cases
(28.1%), and 12 cases of laryngomalacia and airway narrowing
(21.1%). A single case of mucosal bleeding was diagnosed in a
4-year-old Tibetan girl with pneumonia and ASD. Other diagnoses
comprised of 4 cases presenting bridging bronchus, 4 cases of
tracheal bronchus, and 1 case each of polyp of the vocal cord,
complete tracheal rings, neoplasm in the trachea, neoplasm in the
lingual root, and absence of the right upper lobe (Table II).
 | Table II.Diagnosis of flexible bronchoscopy
(n=57). |
Table II.
Diagnosis of flexible bronchoscopy
(n=57).
| Diagnosis | Patients, n (%) |
|---|
| Infection | 57 (100) |
| External compression
of airways | 19 (33.3) |
|
Tracheobronchomalacia | 16 (28.1) |
| Laryngomalacia | 12 (21.1) |
| Airway narrowing | 12 (21.1) |
| Others | 13 (22.8) |
| Bridging
bronchus | 4 (7.0) |
| Tracheal
bronchus | 4 (7.0) |
| Complete
tracheal rings | 1 (1.8) |
| Polyp of
vocal cord | 1 (1.8) |
| Neoplasm
in trachea | 1 (1.8) |
| Neoplasm
in the lingual root | 1 (1.8) |
| Absence
of right upper lobe | 1 (1.8) |
| Mucosal bleeding | 1 (1.8) |
Among 57 patients, only 14 (24.6%) presented
bronchoscopy findings in accordance with the infection. Thus, 43/57
(75.4%) patients exhibited ≥2 bronchoscopy diagnoses, among which
the infection combined with airway abnormality was most common
(Fig. 2).
Furthermore, different types of cardiovascular
abnormalities presented various airway abnormalities (Table III). Notably, the more complicated
the patients' cardiovascular abnormalities were, the more
complicated airway abnormalities they exhibited. Rare airway
abnormalities, including bridging trachea and complete tracheal
rings were present in patients with multiple congenital
cardiovascular abnormalities. Common airway anomalies, including
the external compression of airways, airway narrowing,
tracheobronchonmalacia and laryngomalacia were commonly observed in
patients with one cardiovascular anomaly such as ASD, VSD or
PDA.
 | Table III.Bronchoscopic diagnosis of airway
anomalies according to different type of cardiovascular disorders
(n=57). |
Table III.
Bronchoscopic diagnosis of airway
anomalies according to different type of cardiovascular disorders
(n=57).
| Type of
cardiovascular disorders | External compression
of airways |
Tracheobronchomalacia | Laryngomalacia | Airway narrowing | Tracheal
bronchus | Bridging trachea | Complete tracheal
rings |
|---|
| ASD | 4 (7.0) | 3 (5.3) | 6 (10.5) | 5 (8.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| VSD | 5 (8.8) | 4 (7.1) | 2 (3.5) | 1 (1.8) | 1 (1.8) | 0 (0.0) | 0 (0.0) |
| PDA | 2 (3.5) | 4 (7.1) | 2 (3.5) | 3 (5.3) | 0 (0.0) | 1 (1.8) | 0 (0.0) |
| VSD+ASD | 1 (1.8) | 1 (1.8) | 1 (1.8) | 1 (1.8) | 3 (5.3) | 0 (0.0) | 0 (0.0) |
| TOF | 2 (3.5) | 1 (1.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Other | 5 (8.8) | 3 (5.3) | 1 (1.8) | 2 (3.5) | 0 (0.0) | 3 (5.3) | 1 (1.8) |
| Stenosis of aortic
arch | 1 (1.8) | 0 (0.0) | 1 (1.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Pulmonary
sling+ASD | 2 (3.5) | 2 (3.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (3.5) | 0 (0.0) |
| TAPVC | 1 (1.8) | 0 (0.0) | 0 (0.0) | 1 (1.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Complete vascular
ring | 1 (1.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| VSD+ASD+PDA | 0 (0.0) | 1 (1.8) | 0 (0.0) | 1 (1.8) | 0 (0.0) | 1 (1.8) | 1 (1.8) |
| Total | 19 (33.3) | 16 (28.1) | 12 (21.1) | 12 (21.1) | 4 (7.1) | 4 (7.1) | 1 (1.8) |
BALF assessments
BALF cellularity analysis was performed in 50
patients. A total of 7 patients were excluded as they were too
young to tolerate repeated bronchoalveolar lavage, this meant the
amount of BALF gathered was not enough for cellularity analysis and
culture. The BALF cellularity analysis revealed an increased total
cell count (mean, 1631.3±497.2×106/ml), and the median
percentage of neutrophils and lymphocytes were 44.0 and 9.0%,
respectively. The increased total cell count and neutrophil
percentage were in accordance with the infection in these
patients.
Furthermore, 10/52 (19.2%) BALF specimens exhibited
a positive isolation of an etiological agent including 3 cases of
Klebsiella pneumoniae, 2 cases of acid-producing
Klebsiella and Bauman's Acinetobacter, and 1 case
each of Staphylococcus aureus, Haemophilus influenzae, and
Candida parapsilosis.
Clinically valuable contribution of
FB
FB findings contributed towards the clinically
valuable management of 15 patients (26.3%). A total of 2 patients
(3.5%) were treated with Vancomycin (10 mg/kg every 6 h),
Piperacillin and Tazobactam (30 mg/kg every 8 h) alternatively,
following positive isolation of Staphylococcus aureus and
Haemophilus influenzae from BALF. FB-based diagnoses
assisted in the preoperative planning for 8 patients (14.0%)
including bridging bronchus in 4 patients (7.0 %), complete
tracheal rings in 1 (1.8%), polyp of vocal cord in 1 (1.8%),
tracheal neoplasm in 1 (1.8%), and neoplasm in the lingual root in
1 (1.8%). Furthermore, atelectasis was resolved in 5 patients
(9.0%) following the FB procedure.
Complications
The procedure of FB was safe. The complications
observed were mild and easily corrected, including fever following
procedure in 1 patient and (1.8%) mild desaturation (peripheral
capillary oxygen saturation <92%) in 3 patients (5.3%) that were
resolved by supplemental oxygen. Mild bleeding was exhibited by 1
patient, which was ceased by administering 1–2 ml 1:10,000
epinephrine. The total incidence of complications was 8.8%. There
were 0 instances of mortality during or immediately following the
FB.
Discussion
Children with congenital cardiovascular
abnormalities are predisposed to respiratory diseases. As
cardiovascular abnormalities are associated with airway disorders,
occasionally, their respiratory symptoms are challenging to
resolve. FB presents a diagnostic and therapeutic role in the
evaluation of pulmonary diseases (2). In the present study, it was
demonstrated that FB is a clinically useful and safe technique for
the evaluation of pulmonary diseases in children with congenital
cardiovascular abnormalities.
FB confirmed that 75.4% of all patients enrolled in
the present study exhibited complications associated with airway
disorders. The spectrum of airway diseases observed is similar to
that described in previous studies (1,11,12).
Herein, the most common bronchoscopy diagnoses of airway
abnormalities consisted of external compression of airways,
tracheobronchomalacia, and airway narrowing, which are associated
with cardiovascular abnormalities such as ASD, VSD, and PDA. The
possible reasons why cardiovascular abnormalities are associated
with airway disorders have been discussed elsewhere (1,2,13,14).
Notably, a number of rare airway abnormalities such as bridging
bronchus, tracheal bronchus, and complete tracheal ring were also
presented, for which surgical correction was suggested. Although
certain diagnostic evaluations, such as MRI, are non-invasive and
are able to display the structure of the tracheobronchial tree, the
heart, and the ambient vessels, FB remains the technique of choice
for the evaluation of the airways in the event of tracheomalacia,
stenosis, complete tracheal rings, or aberrant bronchi (4). Furthermore, identification of these
airway abnormalities is useful in assisting preoperative planning
prior to cardiothoracic surgery. Surgeons may be more cautious in
airway management prior to and following cardiothoracic surgery to
decrease the incidence of airway-related complications, such as
airway stenosis following intubation and tracheostomy (15).
Congenital cardiovascular abnormalities accompanied
by airway disorders may result in various clinical manifestations,
such as recurrent lower respiratory infections, consolidation,
atelectasis, hyperinflation, and wheezing (1,2). As
mentioned in a previous study, the bronchoscopic procedure alone is
only seldom curative (1). However,
certain procedures during FB may initiate the relief of pulmonary
disease (1,2,5). For
example, the airway mucin and sputum plug may be aspirated out,
which is beneficial for the resolution of consolidation,
atelectasis, and hyperinflation of the lungs. A previous study
observed the effects of therapeutic BAL on refractory Mycoplasma
pneumoniae and demonstrated that the early application of BAL
shortened the duration of fever and hospitalization, improved
laboratory indices, and promoted the resolution of atelectasis
(16). In the present study, it was
observed that atelectasis was resolved in 5 patients (8.8%)
following FB. In addition, the airway abnormalities, including
narrowing and external compression of airways observed by FB, may
help identify cardiovascular abnormalities. These pieces of
evidence aid clinicians in revealing the underlying causes of
symptoms, such as wheezing, to determine the diagnosis and initiate
appropriate treatment as early as possible. In the present study, 2
patients exhibited airway narrowing; however, the chest CT failed
to provide additional details. Following the procedures, MRA was
arranged and pulmonary sling was confirmed as the cause of
wheezing.
FB not only allows the assessment of airway anatomy
and dynamics, but also provides information about infectious
etiological agents. Although the initial choice of antimicrobial
agents is empirical in the treatment of pulmonary infection,
persistent efforts are made to identify the etiology by sample
cultures (5,17). Obtaining the sputum samples from
children, particularly infants, is challenging as the majority are
unable to cough out sputum voluntarily (1,5). The
treatment depends primarily on cultures from oropharyngeal
specimens. FB and associated procedures (including BAL) allow the
collection of lower respiratory specimens from patients from whom
sputum samples are difficult to obtain. The cultures of
bronchoscopy specimens provide a higher yield of organisms as
compared to those from oropharyngeal specimens (17). In the present study, all patients
exhibited an elevated total cell count and neutrophil percentage,
which was similar to that of pneumonia. Furthermore, 10/52 patients
exhibited positive BALF culture, which guided the alteration in the
administration of antibiotics. The rate of pathogen recovery was
similar to that in a previously published study (1). An accurate and immediate isolation of
infectious agents is crucial for these patients, as the pulmonary
infection may aggravate the original cardiac diseases leading to
complications, such as cardiac failure, which may delay surgical
interventions. Hence, FB helps to treat pneumonia and cardiac
diseases.
FB is an invasive procedure and may have potentially
severe side effects. Complications are associated with an
individual patient's risk factors, medication used and ventilation
technique. Typical complications include trauma of nose and airway,
desaturation and hypoxemia, cough and bronchospasm, hemorrhage,
pneumothorax and fever and infection (18). Thus, safety is a priority prior to
performing FB, particularly in children. However, if patients and
evaluated cautiously and the potential complications are
considered, FB can be a safe technique. Although the majority of
the present patients were young infants (the youngest was
9-days-old), a surprisingly low rate of complications were
encountered: Only 5 patients exhibited mild complications, which
were resolved immediately following supportive therapies. No
mortality was recorded following FB.
However, there are a number of limitations to the
present study. First, the sample size is small, and the present
study was a single-center study, which may influence the strength
of the results. Second, the data were collected retrospectively,
which may result in bias. Furthermore, analysis corresponding to
the prognosis of the patients is absent, thereby necessitating
further studies.
In conclusion, the present study supplements the
literature describing the role of FB in the evaluation of pulmonary
diseases in Chinese children with congenital cardiovascular
abnormalities. In the present study, the majority of patients were
complicated with other airway disorders. The data presented FB as a
safe and effective tool for examining children with cardiovascular
abnormalities. Therefore, FB may be considered as an initial tool
in this specific group of children.
Acknowledgments
Not applicable.
Funding
The present study was partially supported by grants
from the Science & Technology department of Sichuan Province
(grant no. 2015SZ0152) and the National Natural Science Foundation
of China (grant no. 81200461).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TC was responsible for literature search, data
collection, study design, analysis of data, manuscript preparation
and review of manuscript. LQ was responsible for literature search,
data collection, study design, manuscript preparation and review of
manuscript. LZ was responsible for data collection, manuscript
preparation and review of manuscript. QT was responsible for data
collection and review of manuscript. HL was responsible for data
collection and review of manuscript. LC was responsible for study
design, literature search, data collection, analysis of data,
manuscript preparation and review of manuscript.
Ethics approval and consent to
participate
The present study has been approved by the
Institutional Review Board/Ethics Committee of West China Second
University Hospital, Sichuan University (Sichuan, China). Parents
or guardians of all patients provided written, informed consent
prior to the procedures.
Consent for publication
Parents or guardians of all patients provided
written, informed consent for the publication of the associated
data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Efrati O, Gonik U, Modan-Moses D, Bielorai
B, Barak A, Vardi A, Paret G, Mishaly D and Toren A: The role of
flexible fibreoptic bronchoscopy in evaluation of pulmonary
diseases in children with congenital cardiac disease. Cardiol
Young. 17:140–144. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Guillemaud JP, El-Hakim H, Richards S and
Chauhan N: Airway pathologic abnormalities in symptomatic children
with congenital cardiac and vascular disease. Arch Otolaryngol Head
Neck Surg. 133:672–676. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gokdemir Y, Cakir E, Kut A, Erdem E,
Karadag B, Ersu R and Karakoc F: Bronchoscopic evaluation of
unexplained recurrent and persistent pneumonia in children. J
Paediatr Child Health. 49:E204–E207. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li JB, Chen XX, Hu XY, Cui YQ, Hu CM, Li
FX and Chen JW: The application of flexible fiberoptic bronchoscope
in perioperative management of the patients with congenital cardiac
disease. Chin J Pediatr Surg. 34:173–175. 2013.(In Chinese).
|
|
5
|
Efrati O, Sadeh-Gornik U, Modan-Moses D,
Barak A, Szeinberg A, Vardi A, Paret G, Toren A, Vilozni D and
Yahav Y: Flexible bronchoscopy and bronchoalveolar lavage in
pediatric patients with lung disease. Pediatr Crit Care Med.
10:80–84. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nussbaum E: Pediatric fiberoptic
bronchoscopy: Clinical experience with 2,836 bronchoscopies.
Pediatr Crit Care Med. 3:171–176. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
He SR, Sun YX, Liu YM, Zhuang J, Zhong J,
Liang SX, Sun X and Lai JN: Airway obstruction caused by large
blood vessel anomalies: Assessment by flexible bronchoscopy.
Zhonghua Er Ke Za Zhi. 47:726–729. 2009.(In Chinese). PubMed/NCBI
|
|
8
|
Pediatric Bronchoscopy Collaborative
Group, . The Subspecialty Group of Respiratory Diseases, The
Society of Pediatrics, Chinese Medical Association. Guide to
pediatric bronchoscopy (2009 edition). Zhonghua Er Ke Za Zhi.
47:740–744. 2009.(In Chinese). PubMed/NCBI
|
|
9
|
Qun J, Zhou J and Yu Y: An official
Chinese Thoracic Society clinical pratice guideline: The etiologic
assessment of bronchoalveolar lavage in infectious lung disease.
Chin J Tuberc Respir Dis. 40:578–583. 2017.(In Chinese).
|
|
10
|
Baselski VS and Wunderink RG:
Bronchoscopic diagnosis of pneumonia. Clin Microbiol Rev.
7:533–558. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lee SL, Cheung YF, Leung MP, Ng YK and
Tsoi NS: Airway obstruction in children with congenital heart
disease: Assessment by flexible bronchoscopy. Pediatr Pulmonol.
34:304–311. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chapotte C, Monrigal JP, Pezard P, Jeudy
C, Subayi JB, De Brux JL, Cottineau C and Granry JC: Airway
compression in children due to congenital heart disease: Value of
flexible fiberoptic bronchoscopic assessment. J Cardiothorac Vasc
Anesth. 12:145–152. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Little AF, Phelan EM, Boldt DW and Brown
TC: Paediatric tracheobronchomalacia and its assessment by
tracheobronchography. Australas Radiol. 40:398–403. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kussman BD, Geva T and McGowan FX:
Cardiovascular causes of airway compression. Paediatr Anaesth.
14:60–74. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wilson MN, Bergeron LM, Kakade A, Simon
LM, Caspi J, Pettitt T and Kluka EA: Airway management following
pediatric cardiothoracic surgery. Otolaryngol Head Neck.
149:621–627. 2013. View Article : Google Scholar
|
|
16
|
Zhang Y, Chen Y, Chen Z, Zhou Y, Sheng Y,
Xu D and Wang Y: Effects of bronchoalveolar lavage on refractory
Mycoplasma pneumoniae pneumonia. Respir Care. 59:1433–1439. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jain K, Wainwright C and Smyth AR:
Bronchoscopy-guided antimicrobial therapy for cystic fibrosis.
Cochrane Database Syst Rev: Cd009530. 2013. View Article : Google Scholar
|
|
18
|
Paradis TJ, Dixon J and Tieu BH: The role
of bronchoscopy in the diagnosis of airway disease. J Thorac Dis.
8:3826–3837. 2016. View Article : Google Scholar : PubMed/NCBI
|