Introduction
Deep vein thrombosis is one of the common
complications of postpartum (1).
Maternal blood composition, exacerbated hypercoagulable state of
the blood caused by the changes in blood cell activity, pregnancy
uterine oppression, slow deep vein blood flow caused by postpartum
bed rest and breastfeeding while sitting, combined with birth
trauma activation of coagulation, has made women a high-risk
population for deep venous thrombosis. Deep vein thrombosis has
high morbidity and mortality, and is a serious threat to maternal
life and health (2).
Early identification and active intervention can
effectively reduce the incidence and mortality rates of deep vein
thrombosis. However, clinical methods for detecting deep vein
thrombosis cannot effectively identify the early changes of deep
vein thrombosis. Therefore, strengthening studies on the
development of laws and the pathogenesis of deep vein thrombosis
would contribute to the early identification of deep vein
thrombosis of lower extremity. Platelet aggregation is an important
part of thrombus formation (3). A
related study revealed that (4) the
PI3K/AKt signaling pathway can be involved in the regulation of
platelet adhesion and aggregation activity (5). However, changes in platelet aggregation
rate and the PI3K/AKt signaling pathway in postpartum deep venous
thrombosis patients needs to be further confirmed.
In the present study, platelet aggregation rate,
platelet activity indicators and PI3K expression level, and changes
in AKt phosphorylation were preliminarily analyzed in postpartum
deep vein thrombosis patients, in order to explore the platelet
aggregation activity changes and its possible mechanism in
postpartum deep vein thrombosis patients, with the aim to provide a
theoretical basis for the early diagnosis of patients with
postpartum deep vein thrombosis of lower extremity.
Materials and methods
Patients
A total of 23 patients with postpartum deep vein
thrombosis of lower extremity treated in the Department of
Obstetrics of Beijing Chaoyang Hospital (Beijing, China) from
January 2014 to January 2016 were selected for the study. The age
of these patients was 21–39 years, and the mean age was 28.75±6.72
years. Of the 23 patients, 14 patients had cesarean section, while
9 patients had vaginal delivery. These patients were assigned as
the observation group. The inclusion criteria were as follows: i)
Lower extremity swelling, pain, superficial varicose veins and
other clinical manifestations for deep vein thrombosis; and ii)
deep venous thrombosis diagnosed by ultrasound. During the same
period, 25 patients with normal recovery were assigned as the
control group. The age of these patients was 21–40 years, and the
mean age was 29.29±8.01 years. Of these patients, eight patients
had cesarean section, while 17 patients had vaginal delivery. The
inclusion criteria were as follows: i) No clinical manifestations
for deep venous thrombosis, and no history of thrombosis and ii) no
deep venous thrombosis detected by ultrasound. Exclusion criteria
for the two groups were: i) Patients who had pregnancy-induced
hypertension, gestational glucose, placental abruption and other
pregnancy disorders; ii) patients with severe heart, liver and
kidney dysfunction, or severe infection and iii) patients
associated with immune system diseases or active bleeding and other
diseases. In the present study, all the subjects or their families
provided signed informed consent. This study was approved by the
Ethics Committee of Beijing Chaoyang Hospital.
Methods
Groupings
Patients were diagnosed for postpartum deep venous
thrombosis according to the diagnostic and therapeutic criteria for
deep venous thrombosis (2015 revision) (6) were assigned as the observation group.
During the same period, 25 postpartum with normal recovery were
assigned as the control group.
Collection and processing of blood
samples
Since deep venous thrombosis occurred within 1–2
weeks postpartum (7), venous blood
samples at two weeks postpartum in the control group and venous
blood samples after diagnosis in the observation group were tested.
The collected venous blood was centrifuged for 30 min at 1,500 × g
at 4°C the plasma was drawn, and GPIb and platelet-activating
factor (PAF) content was determined. The specimens were centrifuged
for 10 min at 700 × g at 4°C to obtain the upper plasma, the
platelet rich plasma (PRP) was prepared, centrifuged again for 15
min at 700 × g at 4°C to draw the upper plasma, the platelet poor
plasma (PPP) was prepared and the number of platelets were measured
in five categories using a hemocytometer (Abbott Pharmaceutical Co.
Ltd., Lake Bluff, IL, USA). PPP was adjusted with PRP to a platelet
concentration of 3×108 cells/ml was counted, and these
were stored by cryopreservation.
Determination of platelet aggregation
rate
The adjusted PRP was placed into a four-channel
platelet aggregation instrument (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA) to determine the 5-min maximum platelet
aggregation rate with ADP as an inducer (at a final concentration
of 20 µmol/l).
Detection of platelet activity
indicators
The blood GPIb and PAF content of subjects were
determined using an ELISA kit purchased from a test company
(R&D Systems, Minneapolis, MN, USA), and the test procedure was
carried out in strict accordance with reagent instructions. Flow
cytometry was used to measure platelet membrane platelet P-selectin
(CD62p) and lysosomal membrane glycoprotein (CD63) positive rate.
After PRP was adjusted, 1% paraformaldehyde was added, fixed in
room temperature for 15 min, washed twice with PBS-EDTA solution,
centrifuged, and the supernatant was taken. Then, CD62p-FITC and
CD63-FITC, were added, mixed by blowing, allowed to react for 30
min in the dark at room temperature, washed twice, and suspended in
PBS solution. Then, flow cytometry (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA) was performed for detection. An excitation
wavelength of 490 nm was selected, the angular voltage was
adjusted, the target platelet community was divided, and the
positive rate of CD62p and CD63 was calculated.
Detection of PI3K and AKt
phosphorylation levels
The adjusted PRP was added to the lysate to lyse the
platelets, the protein concentration was measured using the BCA
method, the sample was run on the gel, transferred onto a membrane,
closed with milk, and incubated with primary rabbit anti-human AKt
polyclonal antibody (1:600; cat. no. LS-C183748-100),
phosphorylated AKt polyclonal antibody (1:1,000; cat. no.
LS-C122634-50), PI3Kp110β monoclonal antibody (1:1,000; cat. no.
3011) and β-actin monoclonal antibody (1:1,000; cat. no. LS-B1625).
Then it was incubated with goat anti-rabbit secondary polyclonal
antibody (1:1500; cat. no. LS-C56309). All antibodies were
purchased from LifeSpan BioSciences, Inc. (Seattle, WA, USA). The
PI3Kp110β antibody was purchased from Cell Signaling Technology,
Inc. (Danvers, MA, USA). Then, an ECL luminescent developer was
added, exposed and imaged.
Statistical analysis
SPSS 19.0 (SPSS, Inc., Chicago, IL, USA) software
was used to analyze the experimental data. The platelet aggregation
rate, platelet activity indicators and other measurement data were
presented as mean ± standard deviation (SD). The t-test was used to
compare the mean of two groups, and countable data by Chi-square
test were performed. The ROC curve was drawn to evaluate the value
of platelet aggregation in predicting the occurrence of postpartum
deep venous thrombosis of lower extremity. Pearson's correlation
was performed to analyze the platelet aggregation rate and the
plasma platelet activity factor content of subjects, and a
correlation analysis was performed on the expression level of
PI3K/AKt. P<0.05 was considered to indicate a statistically
significant difference.
Results
Comparison of the general information
and platelet aggregation rate between the two groups
A comparison of the age and 5-min maximum platelet
aggregation rate between the two groups is shown in Table I. The difference in age between the
two groups was not statistically significant (P>0.05). However,
compared with the control group, the cesarean section rate and
5-min maximum platelet aggregation rate of subjects in the
observation group was significantly increased (P<0.05).
 | Table I.Comparison of general data and the
platelet aggregation rate between the two groups. |
Table I.
Comparison of general data and the
platelet aggregation rate between the two groups.
| Groups | No. of cases | Age (years) | Cesarean section rate
(%) | Five-minute maximum
platelet aggregation rate (%) |
|---|
| Observation | 23 | 28.75±6.72 | 60.87 | 62.57±11.63 |
| Control | 25 | 29.29±8.01 | 20.00 |
49.06±10.74a |
|
t-test/χ2 |
| −0.252 | 8.367 | 4.184 |
| P-value |
| 0.802 | 0.004 | >0.05 |
Evaluation of the value of platelet
aggregation in predicting the occurrence of postpartum deep venous
thrombosis of lower extremity
Postpartum deep vein thrombosis patients with
illness in the observation group=1 and normal recovery subjects
without illness in the control group=0, and the ROC curve of the
5-min maximum platelet aggregation rate to predict the occurrence
of postpartum deep vein thrombosis was drawn (Fig. 1). The area under the ROC curve (AUC)
was 0.797 (P>0.05, 95% CI: 0.672–0.923).
Analysis of the platelet activity
indicators of subjects and its correlation with platelet
aggregation rate
The expression of PAF, CD62p and CD63 was detected
in subjects in the two groups, and the results were analyzed. The
expression levels of the three platelet activity indicators were
significantly higher in the observation than those in the control
group, (all P<0.05, Table II).
The correlation between the platelet activity indicators and
platelet aggregation rate in subjects was analyzed, and it was
found that the expression levels of PAF, CD62p and CD63 were
positively correlated with the platelet aggregation rate (r=0.389,
0.451 and 0.452; all P<0.05 (Table
III).
 | Table II.Comparison of platelet activity
indicators between the two groups. |
Table II.
Comparison of platelet activity
indicators between the two groups.
| Groups | No. of cases | PAF (pg/ml) | CD62p (%) | CD63 (%) |
|---|
| Observation | 23 | 13.40±2.34 | 31.07±6.37 | 36.00±9.63 |
| Control | 25 |
8.55±1.56a |
14.51±3.54a |
19.71±4.06a |
| t-test |
| 8.513 | 11.253 | 7.748 |
| P-value |
| <0.05 | <0.05 | <0.05 |
 | Table III.The correlation between platelet
activity indicators and the platelet aggregation rate. |
Table III.
The correlation between platelet
activity indicators and the platelet aggregation rate.
| Correlation
index | PAF | CD62p | CD63 |
|---|
| r-value | 0.389 | 0.451 | 0.452 |
| P-value | 0.006 | 0.001 | 0.001 |
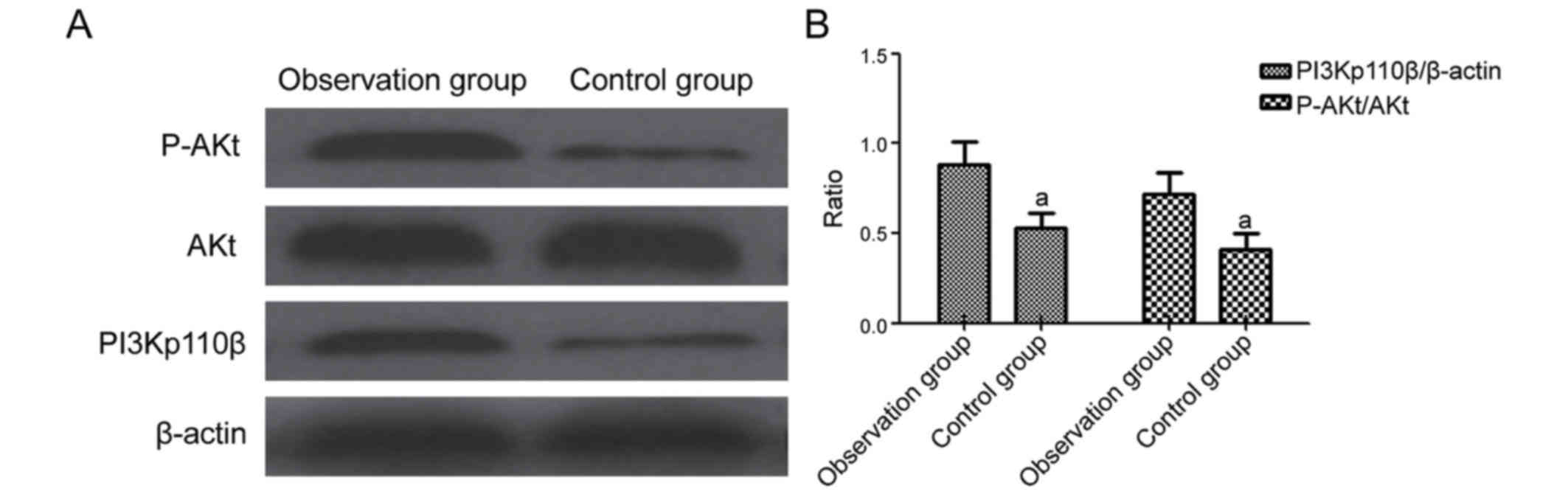
Change of PI3K and AKt expression in
platelets
Change of PI3K and AKt expression in platelets of
subjects in the two groups were detected by western blot analysis
to analyze the gray value of each band. In the observation group,
the PI3Kp110β/β-actin and p-AKt/AKt gray value ratios of subjects
were significantly higher than those in the control group (all
P<0.05; Fig. 2).
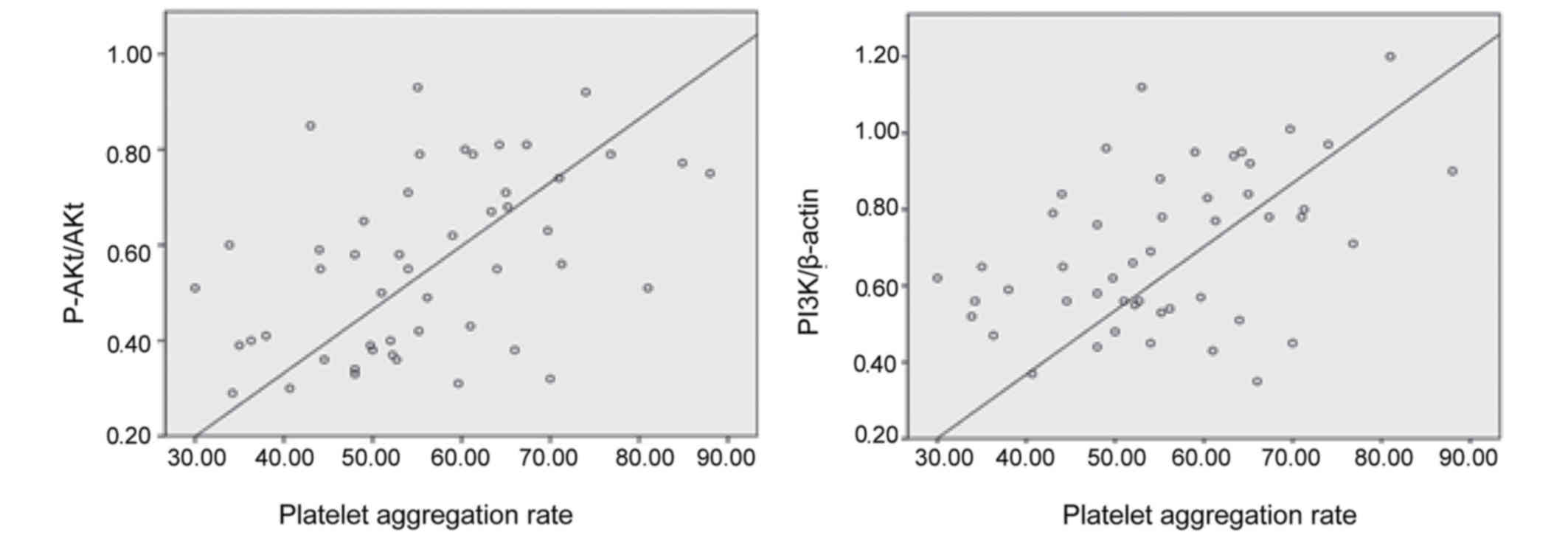
Analysis of the correlation between
the platelet aggregation rate of subjects and the change of PI3K
and AKt expression in platelets
The correlation between the platelet aggregation
rate of subjects and PI3K expression and AKt phosphorylation levels
in platelets were analyzed. Results revealed that the platelet
aggregation rate of subjects was positively correlated with PI3K
levels and p-AKt levels in platelets (r=0.441, 0.430; all
P<0.05; Fig. 3).
Discussion
Due to changes in maternal blood physiology and
anatomical structures, and the two risk factors of slow deep venous
blood flow and blood hypercoagulable state, postpartum deep venous
thrombosis has become a common postpartum complication (8). Strengthening the study of the mechanism
of deep venous thrombosis and determining effective diagnostic
indicators would contribute to the early prevention and treatment
of postpartum deep vein thrombosis. Platelets are important
components of thrombosis. They play a vital role in the formation
of thrombus, and activate platelet adhesion, aggregation and the
release of active substances that participate in the series of
changes in thrombosis formation. Hence, the platelet aggregation
rate is increased in patients with thrombosis, and the expression
of platelet-associated active substances is enhanced. In addition,
findings have shown that the expression of the PI3K/AKt pathway in
platelets was enhanced in thrombosis patients (9), the PI3K/AKt pathway participates in
cell activation, proliferation, apoptosis and other processes
(10), and platelet adhesion,
aggregation and release are closely related (11). Therefore, it could be considered that
the activation of the PI3K/AKt signaling pathway is one of the
mechanisms of platelet activation. The changes in platelet activity
and the PI3K/AKt signaling pathway in patients with postpartum deep
vein thrombosis remain to be confirmed. Therefore, in the present
study, 23 subjects with postpartum deep venous thrombosis were
assigned to the observation group and the 25 subjects with
postpartum normal recovery were assigned to the control group. The
platelet aggregation rate, PAF, CD62p, CD63, as well as the
platelet activity indicators and expression level of the PI3K/AKt
pathway, were analyzed to investigate platelet activity changes in
postpartum deep vein thrombosis patients, and the mechanism
involved.
Platelet adhesion aggregation is a key link in
thrombosis. Adhesion molecules in plasma bind to platelet surface
glycoprotein receptors to mediate platelet aggregation, blood
platelet aggregation substance expression in thrombus patients is
enhanced, platelets are activated under the action of a variety of
coagulation factors, the amount of platelet membrane glycoprotein
and plasma adhesive molecule expression becomes significantly
elevated, and a large number of procoagulant platelet factors are
released into the blood. Therefore, thrombosis may promote the
expression of PAF (12) and
significantly increase the platelet release of CD62p (13), CD63 and other (14) platelet activity markers. Thus, the
platelet aggregation rate of thrombosis patients is increased. In
the study conducted by Signorelli et al, it was suggested
that the platelet aggregation activity of patients with deep vein
thrombosis of lower extremity is enhanced (15). By analyzing the expression of the
three substances (PAF, CD62p, and CD63) in the two groups, it was
found that the expression levels of the three substances were
significantly higher in postpartum deep vein thrombosis patients
than in subjects with normal recovery. Similar results were
obtained in studies conducted by Gerdsen et al (16) and Malaponte et al (17). The analysis of the platelet
aggregation rate revealed that the 5-min maximum platelet
aggregation rate for postpartum deep vein thrombosis of lower
extremity was significantly higher than that for postpartum normal
recovery. Furthermore, the expression level of the three substances
was positively correlated with the platelet aggregation rate,
suggesting that platelet aggregation activity increased in
postpartum deep vein thrombosis patients. The ROC curve of
postpartum deep venous thrombosis was predicted through the 5-min
maximum platelets aggregation. The AUC obtained was 0.797
(P>0.05), and it was observed that the increased platelet
aggregation rate has a certain value in predicting postpartum deep
venous thrombosis. These results suggest that the platelet
aggregation activity of postpartum deep venous thrombosis of lower
extremity is significantly enhanced, and has a certain predictive
value for the occurrence of the disease.
The PI3K/AKt pathway intervenes with the platelet
adhesion process by mediating the GPIb-IX signal (18). PI3K can affect the activity of GPIb,
GPIIb/IIIa and GPIV (19), which
plays a role in controlling platelet aggregation and release; while
AKt platelets could promote the release of the active substance
(20). The study conducted by Chen
et al revealed that the tryptophan derivative CD-26 exerts
an anti-thrombotic effect by inhibiting the PI3K/Akt pathway in
platelets (9). Furthermore, the
study conducted by Hao et al suggested that lutein A may
inhibit platelet activation by inhibiting the PI3K/Akt pathway
(21). Thus, the PI3K/AKt pathway is
an important participant in the regulation of platelet activity.
Western blot analysis was used in this study to detect the
PI3Kp110β and p-AKt levels of platelets in subjects. The analysis
revealed that PI3Kp110β expression and AKt phosphorylation levels
were significantly higher in postpartum deep vein thrombosis
patients than in subjects in the control group, suggesting that the
expression of the PI3K/AKt pathway in postpartum deep vein
thrombosis patients was enhanced. A correlation analysis on
PI3Kp110β expression and AKt phosphorylation levels and the
platelet aggregation rates of subjects was conducted. It was found
that the platelet aggregation rate was positively correlated with
PI3Kp110β expression and AKt phosphorylation levels. The findings
suggests, that the enhancement of the PI3K/AKt signaling pathway in
postpartum deep vein thrombosis patients may be one of the
mechanisms of platelet aggregation.
Platelet is a key link in thrombosis. The study of
changes in platelet function and its mechanism for patients with
thrombosis would help to determine the early diagnostic indicators
of thrombosis, providing a theoretical basis for the early
prevention and treatment of thrombosis. Due to the limited amount
of experimental samples, the changes in platelet activation and
aggregation activity, and the expression level of the intracellular
PI3K/AKt signaling pathway in patients with postpartum deep vein
thrombosis remain to be further studied. It can only be speculated
that the enhancement of the expression of the PI3K/AKt pathway is
one of the mechanisms of platelet aggregation in postpartum deep
vein thrombosis patients. The intracellular signal transduction
process is very complex. Therefore, the specific mechanism of
platelet aggregation activity in patients with postpartum deep vein
thrombosis needs to be further confirmed. It is considered that the
mechanism of platelet activation can be elucidated through the
continuous study of platelet function changes in patients with
thrombosis, in order to develop new sensitive and specific
diagnostic indicators for early postpartum deep venous thrombosis.
In future research, we aim to analyze the changes of platelet
aggregation activity and PI3K/AKt expression before and after the
clinical intervention, to further clarify the predictive value of
platelet aggregation activity in postpartum deep venous thrombosis
and its mechanism.
In summary, the results of this study revealed that
platelet aggregation activity increased in postpartum deep vein
thrombosis patients, it has a certain predictive value for the
occurrence of postpartum deep venous thrombosis. Furthermore,
platelet PI3K expression and AKt phosphorylation levels increased,
suggesting that the PI3K/AKt signaling pathway may be one of the
mechanisms of platelet aggregation. This further elucidates the
changes in postpartum deep vein thrombosis patients and its
mechanism, and provide a theoretical basis for the early diagnosis
of deep vein thrombosis.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MS drafted the manuscript and collected the blood
samples. CL helped with platelet aggregation rate. NZ and KM
detected platelet activity indicators. ZZ detected PI3K and AKt
phosphorylation levels. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Beijing Chaoyang Hospital (Beijing, China). Written informed
consents were signed by the patients and/or guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Parunov LA, Soshitova NP, Ovanesov MV,
Panteleev MA and Serebriyskiy II: Epidemiology of venous
thromboembolism (VTE) associated with pregnancy. Birth Defects Res
C Embryo Today. 105:167–184. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Skuterud Wik H, Jacobsen Flem A and Morten
Sandset P: Long-term outcome after pregnancy-related venous
thrombosis. Thromb Res. 135:1–4. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shifrin MM and Widmar SB: Platelet
inhibitors. Nurs Clin North Am. 51:29–43. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim SD, Lee YJ, Baik JS, Han JY, Lee CG,
Heo K, Park YS, Kim JS, Ji HD, Park SI, et al: Baicalein inhibits
agonist-and tumor cell-induced platelet aggregation while
suppressing pulmonary tumor metastasis via cAMP-mediated VASP
phosphorylation along with impaired MAPKs and PI3K-Akt activation.
Biochem Pharmacol. 92:251–265. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Min SH and Abrams CS: Membrane grease
eases platelet maturation. Blood. 126:1055–1056. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Buller HR, Sohne M and Middeldorp S:
Treatment of venous thromboembolism. J Thromb Haemost. 3:1554–1560.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Konkle BA: Diagnosis and management of
thrombosis in pregnancy. Birth Defects Res C Embryo Today.
105:185–189. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Parent F, Jovan R and des Francs Colas V:
Venous thromboembolism during pregnancy. Rev Prat. 65:188–192.
2015.(In French). PubMed/NCBI
|
|
9
|
Chen Y, Wang Y, Xie Z, Ming X, Li Z and
Kong Y: A tryptophan derivative TD-26 attenuates thrombus formation
by inhibiting both PI3K/Akt signaling and binding of fibrinogen to
integrin αIIbβ3. Biochem Biophys Res Commun. 465:516–522. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Singhal R, Annarapu GK, Pandey A, Chawla
S, Ojha A, Gupta A, Cruz MA, Seth T and Guchhait P: Hemoglobin
interaction with GP1bα induces platelet activation and apoptosis: A
novel mechanism associated with intravascular hemolysis.
Haematologica. 100:1526–1533. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lopes-Pires ME, Naime AC, Cardelli Almeida
NJ, Anjos DJ, Antunes E and Marcondes S: PKC and AKT modulate
cGMP/PKG signaling pathway on platelet aggregation in experimental
sepsis. PLoS One. 10:e01379012015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Clark GD: Platelet-activating factor
acetylhydrolase and brain development. Enzymes. 38:37–42. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kuriyama N, Mizuno T, Yasuike H, Matsuno
H, Kawashita E, Tamura A, Ozaki E, Matsui D, Watanabe I, Koyama T,
et al: CD62-mediated activation of platelets in cerebral white
matter lesions in patients with cognitive decline. Arch Gerontol
Geriatr. 62:118–124. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pósfai É, Marton I, Kotosz B and Borbényi
Z: Contribution of cardiovascular risk factors in the thrombotic
complications of essential thrombocythaemia: A Hungarian
single-institute retrospective analysis. Eur Rev Med Pharmacol Sci.
19:1258–1263. 2015.PubMed/NCBI
|
|
15
|
Signorelli SS, Ferrante M, Gaudio A and
Fiore V: Deep vein thrombosis related to environment (Review). Mol
Med Rep. 15:3445–3448. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gerdsen F, Weber M, Langer F, Eifrig B and
Lindhoff-Last E: Platelet activation markers in patients with
venous thromboembolism without predisposing factors. Pathophysiol
Haemost Thromb. 34:1–5. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Malaponte G, Signorelli SS, Bevelacqua V,
Polesel J, Taborelli M, Guarneri C, Fenga C, Umezawa K and Libra M:
Increased levels of NF-kB-dependent markers in cancer-associated
deep venous thrombosis. PLoS One. 10:e01324962015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mu FT, Cranmer SL, Andrews RK and Berndt
MC: Functional association of phosphoinositide-3-kinase with
platelet glycoprotein Ibalpha, the major ligand-binding subunit of
the glycoprotein Ib-IX-V complex. J Thromb Haemost. 8:324–330.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim S, Mangin P, Dangelmaier C, Lillian R,
Jackson SP, Daniel JL and Kunapuli SP: Role of phosphoinositide
3-kinase beta in glycoprotein VI-mediated Akt activation in
platelets. J Biol Chem. 284:33763–33772. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim TH, Kim HM, Park SW and Jung YS:
Inhibitory effects of yuzu and its components on human platelet
aggregation. Biomol Ther (Seoul). 23:149–155. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hao HZ, He AD, Wang DC, Yin Z, Zhou YJ,
Liu G, Liang ML, Da XW, Yao GQ, Xie W, et al: Antiplatelet activity
of loureirin A by attenuating Akt phosphorylation: In vitro
studies. Eur J Pharmacol. 746:63–69. 2015. View Article : Google Scholar : PubMed/NCBI
|