Introduction
At present, more and more patients are clinically
treated with fixed orthodontic treatment for dental malformation,
and the effect is good. However, fixed orthodontic treatment also
has its common complications (1),
such as producing plaque to cause different degrees of irritation
to the gingiva of patients, and causing gingivitis, which can be
characterized by gingival swelling, pain or gingival irritating
bleeding (2). If the treatment of
gingivitis caused by fixed orthodontic treatment is not timely, it
will not only affect the effect of treatment, but also affect the
diet and quality of life of patients (3). Numerous studies have shown that a
variety of inflammatory factors are involved in the production of
fixed orthodontic gingivitis, thus effectively reducing the
inflammatory level in gingivitis gingival crevicular fluid, which
can effectively improve the condition, be helpful to fixed
orthodontic effect and remove dental plaque. Reducing the level of
inflammatory factors in gingival crevicular fluid is the main
treatment for fixed orthodontic gingivitis (4,5).
Kangfuxin solution is a traditional Chinese medicine
preparation, mainly consisting of ethanol extract from dried insect
body of Periplaneta americana. It has the function of
promoting blood circulation, nourishing yin and producing
muscle, and has a good curative effect on ulcers, burns, and
fistula. At present, it is increasingly used in the clinic
(6). In patients with fixed
orthodontic gingivitis, a polyol substance in Kangfuxin solution
can promote increased isosynthesis of gingival epidermal cell type
I isoelastic collagen, and generate new granulation tissues, so the
local cells of gingival inflammation proliferate (7). The treatment of patients with fixed
orthodontic gingivitis using Kangfuxin solution is gingivitis local
spraying, followed by sublingual administration, which increases
the direct contact time between the drug and gingivitis local
inflammatory mucosa, accelerate the healing of inflammation, and
improve the clinical effective rate (8).
Patients and methods
General data
A total of 78 patients diagnosed with fixed
orthodontic gingivitis in the Department of Stomatology in Weifang
People's Hospital (Weifang, China) from January, 2015 to March,
2017 were selected. The study was approved by the Ethics Committee
of Weifang People's Hospital (Weifang, China). Signed informed
consents were obtained from the patients or the guardians. Among
them, 39 patients were treated with gingival cleansing as control
group, and the other 39 patients were treated with gingival
cleansing plus spraying and sublingual administration with
Kangfuxin solution as treatment group. There were 41 males and 37
females, aged 13–28 years, with an average age of 16.07±1.86 years.
The course of disease was 3–10 months, and the average course of
disease was 6.23±0.91 months. All the included patients met the
following diagnostic criteria: Gingival swelling, pain, congested
mucosa, surface temperature rise, easily bleeding when stimulated,
swelling and pain levels of grade III, gingival sulcus bleeding
index (BI) >2, probing depth (PD) >4 mm, and all patients
undergoing straight wire appliance. Exclusion criteria: Patients
who had recently received antibiotic treatment or periodontal
related treatment, patients with severe oral and periodontal
diseases, severe heart, liver and kidney dysfunction, or poor
eating and chewing habits, and patients who refused to sign the
informed consent, those who quit midway or had incomplete clinical
data.
Methods
Therapeutic methods
All the included patients were treated with gingival
cleaning routine treatment, that is, gingival cleaners were used to
clean the plaque and periodontal stones, and gingival cleaning was
performed inside the periodontal pocket. In treatment group,
Kangfuxin solution was used on the basis of routine treatment. A 5
ml sterile disposable syringe was used to extract 5 ml Kangfuxin
solution at a time and spray it on the local mucosa of gingivitis
in patients in treatment group. The patients were told to take it
in the mouth for 5 min and then swallow it twice a day. Relevant
indexes of all patients were measured and recorded at 1 day before
treatment and 7 days after treatment.
Inflammatory factor detection
At 1 day before treatment and 7 days after
treatment, all the included patients gargled, and an air gun was
used to dry the tooth surface. A filter paper strip was inserted
into the gingival lateral sulcus of the patient, and it was taken
out when there was a slight sense of resistance. The filter paper
strip was observed, and if it had blood, the specimen was taken
again. The specimen was stored at 4°C and centrifuged at 3,000 × g,
and the supernatant was collected. The levels of interleukin
(IL)-1β, IL-6, IL-17 and tumor necrosis factor-α (TNF-α) in
gingival crevicular fluid were determined by enzyme-linked
immunosorbent assay (ELISA). The kit was provided by Shandong
Science and Technology Co., Ltd (Shandong, China).
Periodontal condition measurement
A coarse blunt gingival probe was put into the
lateral sulcus of the gingival, and BI and PD of the patient were
calculated. The grades are as follows: 0 point, no bleeding,
redness, or skin temperature rise after the probe touched the
gingiva; 1, bleeding or redness, etc, after the probe touched the
gingiva; 2, scattered point bleeding on the surface after the probe
touched the gingiva; 3, scattered bleeding after the probe touched
the gingiva; 4, larger amount of bleeding than that in gingival
sulcus after the probe touched the gingiva; and 5 points, bleeding
without the probe touching the gingiva.
Pain level
No obvious or slight pain, and normal life not
affected was grade I. Moderate or paroxysmal pain was grade II.
Intolerable pain and normal life affected was grade III.
Swelling level
No swelling or no periodontal pocket seen was grade
I. Visible redness and swelling, but no periodontal pocket was
grade II. Redness and swelling and periodontal pocket seen was
grade III.
Therapeutic effect
Markedly effective: Gingival color and appearance
are normal, PD<2 mm. Improved: Gingival color and appearance are
improved significantly, 2 mm<PD<3.0 mm. Ineffective: No
changes in gingival color and appearance, PD>3.0 mm.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
19.0 statistical software was used to process the data. Collection
data were represented as mean ± standard deviation (SD). Student's
t test was used for comparison of general data. ANOVA was used for
comparison of multiple groups and the post hoc test was SNK test.
Analysis of Pearson correlation between two factors was used.
P<0.05 indicates that the difference was statistically
significant.
Results
Comparison of general data before
treatment between treatment and control group
There were no statistically significant differences
in age, sex and the course of gingivitis between treatment and
control group, and the data were comparable (p>0.05, Table I).
 | Table I.Comparisons of general data between
treatment and control group by Student's t-test. |
Table I.
Comparisons of general data between
treatment and control group by Student's t-test.
| General data | Treatment group
(n=39) | Control group
(n=39) | P-value |
|---|
| Age (years) | 15.94±1.77 | 16.22±1.08 | 0.719 |
| Sex
(male/female) | 20/19 | 21/18 | 0.908 |
| Course of gingivitis
(months) | 5.99±0.87 | 6.32±1.01 | 0.779 |
| BMI
(kg/m2) | 21.73±4.62 | 20.64±3.91 | 0.813 |
Comparison of inflammatory factors in
gingival crevicular fluid before and after treatment between
treatment and control group
There were no significant differences in the levels
of IL-1β, IL-6, IL-17 and TNF-α before treatment between treatment
and control group (p>0.05). After treatment, the levels of
IL-1β, IL-6, IL-17 and TNF-α in both groups were lower than those
before treatment. Moreover, the curative effect of the treatment
group was lower than that of the control group, and the difference
was statistically significant (p<0.05, Table II).
 | Table II.Comparison of levels of inflammatory
factors before and after treatment between treatment and control
group by Student's t-test. |
Table II.
Comparison of levels of inflammatory
factors before and after treatment between treatment and control
group by Student's t-test.
| Groups | No. | Time | IL-1β (ng/l) | IL-17 (ng/ml) | IL-6 (ng/l) | TNF-α (pg/ml) |
|---|
| Control | 39 | Before treatment | 14.23±1.76 | 3.26±0.71 | 16.34±2.23 | 13.29±4.18 |
|
|
| After treatment | 10.97±1.78 | 1.87±0.33 | 10.41±1.16 | 9.45±1.44 |
| Treatment | 39 | Before treatment | 14.38±1.91 | 3.31±0.96 | 16.44±2.29 | 13.66±3.91 |
|
|
| After treatment | 8.79±1.83 | 0.97±0.42 | 8.16±1.68 | 7.08±1.16 |
Comparison of periodontal condition
before and after treatment between the treatment and the control
group
There were no significant differences in gingival BI
and PD before treatment between the treatment and the control
group. After treatment, gingival BI and PD in both groups were
lower than those before treatment. The curative effect in the
treatment group was better than that in the control group, and the
difference was statistically significant (p<0.05, Table III).
 | Table III.Comparison of periodontal conditions
before and after treatment between treatment and control group by
Student's t-test. |
Table III.
Comparison of periodontal conditions
before and after treatment between treatment and control group by
Student's t-test.
| Groups | No. | Time | BI | PD (mm) |
|---|
| Control | 39 | Before treatment | 3.93±0.41 | 4.79±0.45 |
|
|
| After treatment | 2.77±0.38 | 3.33±0.41 |
| Treatment | 39 | Before treatment | 3.89±0.37 | 4.81±0.49 |
|
|
| After treatment | 1.54±0.49 | 2.36±0.37 |
Comparison of swelling and pain levels
after treatment between the treatment and control the group
The levels of gingival pain and swelling in the
treatment group were mainly in grade I, which were 89.74 and
92.31%, respectively. The levels of gingival pain and swelling
after treatment in the control group were mainly in grade II and
III, and the difference was statistically significant (p<0.05,
Table IV).
 | Table IV.Comparison of swelling and pain levels
after treatment between treatment and control group by ANOVA. |
Table IV.
Comparison of swelling and pain levels
after treatment between treatment and control group by ANOVA.
|
|
| Pain level (n,
%) | Swelling level (n,
%) |
|---|
|
|
|
|
|
|---|
| Groups | No. | Grade I | Grade II | Grade III | Grade I | Grade II | Grade III |
|---|
| Control | 39 | 13 (33.33) | 17 (43.59) | 9 (23.08) | 13 (33.33) | 16 (41.03) | 10 (25.64) |
| Treatment | 39 | 35 (89.74) | 3
(7.69) | 1 (2.56) | 36 (92.31) | 2
(5.13) | 1
(2.56) |
Comparison of therapeutic effects
between the treatment and control group
After treatment, the total effective rate of the
control group was 76.92% and that of the treatment group was
97.44%. The difference was statistically significant (p<0.05,
Table V).
 | Table V.Comparison of therapeutic effects
between treatment and control group by ANOVA. |
Table V.
Comparison of therapeutic effects
between treatment and control group by ANOVA.
| Groups | No. | Markedly effective
(n, %) | Improved (n, %) | Ineffective (n,
%) | Effective (n, %) |
|---|
| Control | 39 | 17 (43.59) | 13 (33.33) | 9 (23.08) | 30 (76.92) |
| Treatment | 39 | 34 (87.18) | 4 (10.26) | 1 (2.56) | 38 (97.44) |
| P-value |
|
|
|
| 0.001 |
Analysis of correlation of
inflammatory factors with periodontal conditions
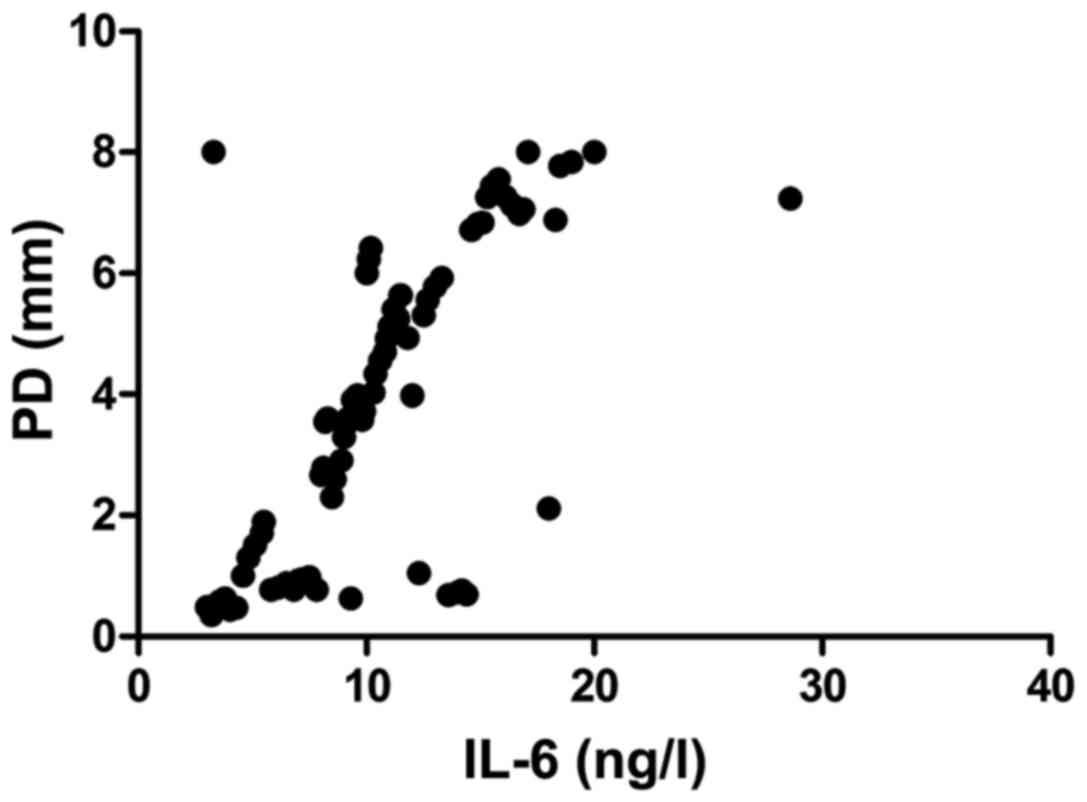
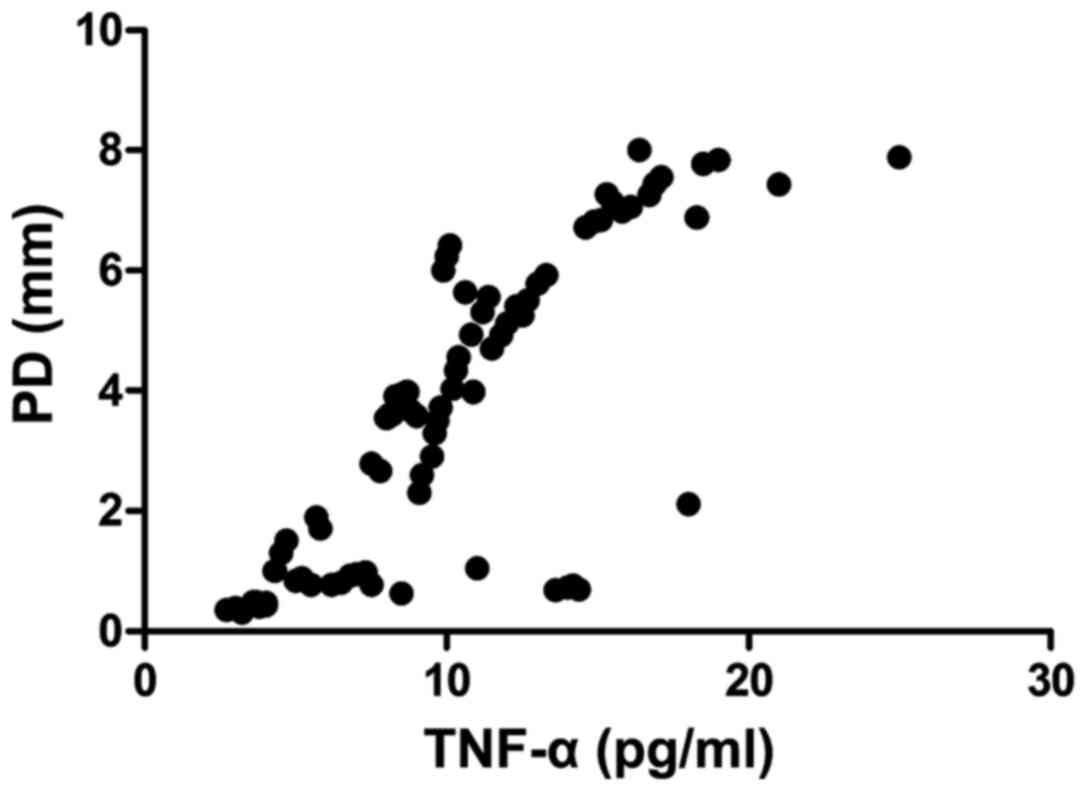
The levels of IL-6 (r=0.793, p<0.001) and TNF-α
(r=0.667, p<0.001) in gingival crevicular fluid were positively
correlated with PD, and the differences were statistically
significant (Figs. 1 and 2).
Discussion
A membrane formed by plaque adheres to tooth
surface, resulting in inflammation of gingiva, which is known as
gingivitis. Gingivitis is more common in patients with fixed
orthodontic teeth. During the formation of gingivitis in fixed
orthodontic patients, many inflammatory factors in gingival
crevicular fluid promote the occurrence and development of
gingivitis (9). It has been reported
that the levels of IL-1β, IL-6, IL-17 and TNF-α in gingival
crevicular fluid are closely related to the occurrence of
gingivitis in fixed orthodontic patients (10). Inflammatory factors contribute to the
increase of synthesis and secretion of gingival proteinase, the
decrease of collagen content and the weakening of cell
proliferation, so the healing of the wound is slow (11). Numerous data indicate that in fixed
orthodontic patients without gingivitis, the levels of inflammatory
factors in gingival crevicular fluid are significantly decreased,
and the higher the inflammatory level, the more severe the
condition of gingivitis is (12).
Fixed orthodontic patients with gingivitis generally manifest local
gingival mucosal swelling, redness, increased skin temperature and
bleeding, affecting the diet, and quality of life (13). However, if the treatment is not
timely, it may develop into periodontitis, and bacteria may enter
the body's blood circulation through the wound, leading to systemic
inflammation, fever, and other organ infections (14,15). For
gingivitis occurring in fixed orthodontic patients, gingival
cleaning was used as the main treatment in the past. However,
gingival cleaning is often unable to cure gingivitis, which can
easily lead to recurrence and affect the quality of life of
patients (16). If the drug can
prolong the contact time with the local mucosal tissues of
gingivitis, it is better for gingivitis, and Kangfuxin solution has
this advantage (17). Kangfuxin
solution in the treatment of gingivitis in fixed orthodontic
patients has more advantages, such as improving the immune function
of patients, increasing the activity of lysozyme in serum, and
speeding up the clearance of necrotic cell tissues (18). Secondly, the local blood circulation
is accelerated, the speed of capillary proliferation is
accelerated, new granulation tissues are generated, and the healing
of inflammation is accelerated (19).
It was found in this study that the levels of
inflammatory factors in gingival crevicular fluid after treatment
in the treatment and control groups were lower than those before
treatment, and they were more obvious in treatment group than those
in control group (p<0.05). Moreover, the periodontal conditions
in treatment group were also improved significantly after
treatment, and the overall effective rate was higher. Gingival
crevicular fluid is the metabolite of epithelial cells, and cell
fluid. The cytokine components in gingival crevicular fluid can
represent the periodontal conditions. If the inflammatory level in
gingival crevicular fluid is increased, the periodontal conditions
are poor, and the condition of gingivitis is more serious (20). A positive correlation between
inflammatory factors and periodontal conditions was found in this
study (p<0.001), which was consistent with the above conclusion.
Therefore, Kangfuxin solution effectively reduces the levels of
inflammatory factors in gingival crevicular fluid, and improves the
periodontal conditions at the same time, and it is more helpful in
the treatment of fixed orthodontic patients complicated by
gingivitis, thus improving the overall effective rate.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YL drafted this manuscript. YL and FM were
responsible for the conception and design of the study. FM
collected the patient data, and revised the manuscript critically
for important intellectual content. LL and CS analyzed and
interpreted the data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Weifang People's Hospital (Weifang, China). Signed informed
consents were obtained from the patients or the guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lakschevitz F, Aboodi G, Tenenbaum H and
Glogauer M: Diabetes and periodontal diseases: Interplay and links.
Curr Diabetes Rev. 7:433–439. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Duarte PM, Bezerra JP, Miranda TS, Feres
M, Chambrone L and Shaddox LM: Local levels of inflammatory
mediators in uncontrolled type 2 diabetic subjects with chronic
periodontitis. J Clin Periodontol. 41:11–18. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kossack C and Jost-Brinkmann PG: Plaque
and gingivitis reduction in patients undergoing orthodontic
treatment with fixed appliances-comparison of toothbrushes and
interdental cleaning aids. A 6-month clinical single-blind trial. J
Orofac Orthop. 66:20–38. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sánchez GA, Miozza VA, Delgado A and Busch
L: Salivary IL-1β and PGE2 as biomarkers of periodontal status,
before and after periodontal treatment. J Clin Periodontol.
40:1112–1117. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Persson GR and Persson RE: Cardiovascular
disease and periodontitis: An update on the associations and risk.
J Clin Periodontol. 35 Suppl:362–379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Luke R, Khan SN, Iqbal PS, Soman RR,
Chakkarayan J and Krishnan V: Estimation of specific salivary
enzymatic biomarkers in individuals with gingivitis and chronic
periodontitis: A clinical and biochemical study. J Int Oral Health.
7:54–57. 2015.PubMed/NCBI
|
|
7
|
Abhishek KN, Supreetha S, Sam G, Khan SN,
Chaithanya KH and Abdul N: Effect of neem containing toothpaste on
plaque and gingivitis - a randomized double blind clinical trial. J
Contemp Dent Pract. 16:880–883. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kirschneck C, Christl JJ, Reicheneder C
and Proff P: Efficacy of fluoride varnish for preventing white spot
lesions and gingivitis during orthodontic treatment with fixed
appliances - a prospective randomized controlled trial. Clin Oral
Investig. 20:2371–2378. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sedighrahimabadi M, Shams M, Fani M and
Chijan MR: Gingivitis from the viewpoint of traditional Persian
medicine. Iran J Med Sci. 41:S352016.
|
|
10
|
Gopinath VK, Rahman B and Awad MA:
Assessment of gingival health among school children in Sharjah,
United Arab Emirates. Eur J Dent. 9:36–40. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Santos MT, Ferreira MC, Guaré RO, Diniz
MB, Rösing CK, Rodrigues JA and Duarte DA: Gingivitis and salivary
osmolality in children with cerebral palsy. Int J Paediatr Dent.
26:463–470. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Azodo CC and Agbor AM: Gingival health and
oral hygiene practices of school children in the North West region
of Cameroon. BMC Res Notes. 8:3852015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jovito VC, Freires IA, Ferreira DA, Paulo
MQ and Castro RD: Eugenia uniflora dentifrice for treating
gingivitis in children: Antibacterial assay and randomized clinical
trial. Braz Dent J. 27:387–392. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ravikumar R, Manohar R, Latha SM and Scott
JX: Gingival hypertrophy in a child: Expect the unexpected. Indian
J Dent. 7:112–114. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Detert J, Pischon N, Burmester GR and
Buttgereit F: The association between rheumatoid arthritis and
periodontal disease. Arthritis Res Ther. 12:218–225. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gurav A and Jadhav V: Periodontitis and
risk of diabetes mellitus. J Diabetes. 3:21–28. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Covani U, Marconcini S, Derchi G, Barone A
and Giacomelli L: Relationship between human periodontitis and type
2 diabetes at a genomic level: A data-mining study. J Periodontol.
80:1265–1273. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gamonal J, Acevedo A, Bascones A, Jorge O
and Silva A: Levels of interleukin-1 beta, −8, and −10 and RANTES
in gingival crevicular fluid and cell populations in adult
periodontitis patients and the effect of periodontal treatment. J
Periodontol. 71:1535–1545. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Acharya AB, Thakur S and Muddapur MV:
Evaluation of serum interleukin-10 levels as a predictor of
glycemic alteration in chronic periodontitis and type 2 diabetes
mellitus. J Indian Soc Periodontol. 19:388–392. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pradeep AR, Martande SS, Singh SP, Suke
DK, Raju AP and Naik SB: Correlation of human S100A12 (EN-RAGE) and
high-sensitivity C-reactive protein as gingival crevicular fluid
and serum markers of inflammation in chronic periodontitis and type
2 diabetes. Inflamm Res. 63:317–323. 2014. View Article : Google Scholar : PubMed/NCBI
|