Introduction
Myocardial infarction (MI), also known as myocardial
infarct, refers to local myocardial necrosis due to ischemia after
interruption of blood flow caused by coronary occlusion, and it is
a kind of heart disease seriously threatening human healthy, which
can lead to such complications as arrhythmia, heart failure or
shock (1,2). The traditional treatment methods of MI
include drug therapy, interventional therapy and coronary artery
bypass grafting. However, these treatment methods bring different
degrees of physical or psychological burden to patients due to poor
efficacy or complications (3–6). Poulos
(7)studied and showed that stem cell
transplantation can promote the regeneration of myocardial cells in
the local infarct region, thereby repairing the heart and improving
the cardiac function. At present, the main stem cells applied
include bone marrow mesenchymal, hematopoietic, embryonic and
cardiac stem cells (CSCs) (8–11), among
which CSC, with strong proliferation and differentiation
capacities, is an innate undifferentiated cell derived from the
heart (12). CSCs possess the
regenerative potential and appear in the myocardial ischemic region
in animal model experiment, which can be directionally
differentiated into myocardial, vascular smooth muscle and vascular
endothelial cells and fibroblasts, thereby participating in
repairing the cardiac function (5,9). CSCs
are characterized by low tissue specificity and immunogenicity, so
their therapeutic effect in transplantation is better than those of
other stem cells (9,10,13).
Integrin-linked kinase (ILK) is a kind of serine/threonine protein
kinase (14), which is highly
expressed in the heart and involved in various pathophysiological
processes, such as myocardial proliferation, contraction and
hypertrophy, and plays an important role in cardiac transplantation
and repair (15–17).
In this study, the rat model of MI was established,
CSCs in rats were transfected with green fluorescent protein (GFP)
adenovirus vector overexpressing ILK, and the effects of
transplantation of CSCs overexpressing ILK on cardiac function,
exercise capacity and myocardial cell proliferation of rats with
acute MI were investigated, so as to provide a certain basis for
the new therapeutic direction of acute MI.
Materials and methods
Experimental animals and reagents
Male Sprague-Dawley (SD) rats of clean grade, aged
49–56 days old and weighing 250–300 g, were purchased from the
Laboratory Animal Center of Guangzhou University of Traditional
Chinese Medicine (Guangzhou, China). ILK complementary
deoxyribonucleic acid (cDNA) adenovirus vector was purchased from
Invitrogen (Invitrogen; Thermo Fisher Scientific, Inc., Waltham,
MA, USA). Lipofectamine 2000, phosphate-buffered saline (PBS), type
II collagenase, trypsin, Dulbecco's modified Eagle's medium
(DMEM)/Ham's F12 medium, and Iscove's modified Dulbecco's medium
(IMDM) were bought from Gibco (Gibco; Thermo Fisher Scientific,
Inc.). Rabbit anti-rat ILK, rat Ki-67 and P-H3 antibodies, and
horseradish peroxidase-labeled goat anti-rat immunoglobulin G (IgG)
were bought from Abcam (Cambridge, MA, USA).
The study was approved by the Ethics Committee of
Weifang People's Hospital (Weifang, China).
Isolation, culture and adenovirus
transfection of CSCs
Male SD rats (aged 49–56 days) were anesthetized by
an intraperitoneal injection of 3% sodium pentobarbital (at a dose
of 30 mg/kg), and sacrificed via cervical dislocation. The rats
were housed in pairs in a temperature-controlled room (21–22°C)
with 40–50% humidity under a 12-h light/dark cycle and were allowed
free access to food and water. The large artery was removed from
the heart under sterile conditions, and the heart was placed in a
petri dish, cut into pieces and rinsed with PBS. Then 0.2% trypsin
and type II collagenase were added at 37°C for 5 min, and the
operation was repeated 3 times. After trypsin was removed, the
pieces were washed twice with complete culture solution (IMDM
containing 10% fetal bovine serum, 100 U/ml penicillin, 100 µg/ml
streptomycin, 2 mmol/l glutamine and 0.1 mmol/l 3-mercaptoethanol).
The above culture solution was added into a culture flask for
culture. After 1 week, the pieces were rinsed twice with PBS, and
the exfoliated cells were collected and inoculated into the culture
flask at a density of 1×105 cells/ml, followed by
culture using the mixed culture solution (35% IMDM, 65% DMEM and
Ham's F-12). When 80% CSCs were fused, the medium was replaced, and
Ad-ILK (GFP adenovirus overexpressing ILK) or Ad-null (empty GFP
adenovirus) was added at 37°C for 2 h. Finally, the cells were
collected after 48 h of culture.
Construction of rat model of MI and
cell transplantation
A total of 60 SD rats were randomly divided into MI
+ normal saline group (NS group, n=20), MI + CSC transfected with
empty vector group (GFP-CSC group, n=20) and MI + CSC transfected
with ILK group (ILK-CSC group, n=20). The rat model of MI was
constructed via ligation of the left anterior descending coronary
artery. At 15 min after successful modeling, 30 µl NS, GFP-CSC
(1×105 cells/30 µl) and ILK-CSC (1×105
cells/30 µl) were injected into the MI region at three different
points. Then muscles and skin were sutured, and penicillin was
intramuscularly injected to prevent infection at 1 week after
operation.
Echocardiography method
Four weeks after modeling, all rats underwent
echocardiography using the Philips SONOS 5500 color ultrasonic
apparatus. After rats were anesthetized via intraperitoneal
injection of 3% sodium pentobarbital (30 mg/kg), the chest hair was
shaved off under a supine position, and then left ventricular
end-systolic diameter (LVESD), left ventricular end-diastolic
diameter (LVEDD) and left ventricular ejection fraction (LVEF) of
rats in each group were measured. The measurement was repeated for
3 times and the average was taken.
Exhaustive swimming experiment
Four weeks after transplantation, exhaustive
swimming experiment was performed for all rats to detect the
exercise capacity. The rat tails were loaded with the weights
weighing 5% of its weight for weight-bearing swimming in a water
tank [45 cm (depth) × 1 m (length) × 1 m (width)]. The sinking of
rats in swimming was the main focus, and the swimming time of rats
was recorded.
Observation of the survival of
transplanted cells
Three days and 4 weeks after transplantation, 5 rats
were sacrificed, respectively, and heart specimens were frozen and
stored. The specific method is as follows: the heart tissues were
rewarmed to −20°C. The left and right ventricles were separated
along the ventricular wall, the myocardial tissues in the infarct
region and marginal infarct region of 3 rats in each group were
collected, fixed in 4% paraformaldehyde solution, and embedded in
paraffin. The paraffin-embedded tissue was sliced into 5 µm-thick
sections. The GFP expression was observed under a fluorescence
microscope (BX53; Olympus, Tokyo, Japan) and analyzed using
SigmaScan software.
Detection of Ki-67 and P-H3 protein
expressions in myocardial tissues of rats via
immunohistochemistry
After echocardiography and exhaustive swimming
experiment, 5 rats were sacrificed in each group, respectively.
After heart tissues were prepared into paraffin-embedded sections,
they were dewaxed, incubated with 3% H2O2 for
10 min, washed with PBS for 3 times (3 min/time). After treatment
with 0.5% Triton X-100 for 30 min, sections were washed with PBS
for 3 times (3 min/time) and sealed in 10% goat serum for 30 min.
After the serum was removed, rabbit polyclonal Ki-67 antibody
(diluted at 1:100; ab833), rabbit polyclonal Histone H3 (phospho
S28) antibody (diluted at 1:100; ab5168), and goat anti-rabbit IgG
H&L (Biotin) (ab6720) (dilution: 1:500) (all purchased from
Abcam), were added dropwise, and the sections were placed in a wet
box at 4°C overnight and washed again with PBS for 3 times (3
min/time). After the secondary antibody horseradish
peroxidase-labeled goat anti-rat immunoglobulin G (IgG) was added
for incubation at room temperature for 2 h, the sections were
washed with PBS for 3 times (3 min/time), followed by color
development via diaminobenzidine and hematoxylin counterstaining.
Finally, the sections were rinsed with PBS and deionized water and
sealed, and the brown-yellow particles with positive protein
expression in myocardial cells were observed under the fluorescence
microscope (BX53; Olympus). The optical density value was measured
using Image-Pro Plus 6.0 software.
Statistical analysis
Statistical analysis was performed using Statistical
Product and Service Solutions (SPSS) 13.0 software (SPSS, Inc.,
Chicago, IL, USA). Analysis of variance or t-test was used for
quantitative data in line with normal distribution, and
Student-Newman-Keuls (SNK)-Q test was used for the pairwise
comparison after analysis of variance. ANOVA followed by post hoc
test (Dunnetts test) was used to evaluate the quantitative data.
All P-values indicated the two-tailed probability, and the
inspection level α=0.05.
Results
Four weeks after transplantation of the myocardial
cells, 5 rats died of heart failure, including 3 rats in the NS
group, 1 rat in the GFP-CSC group and 1 rat in the ILK-CSC group.
Finally, 17 rats in the NS group, 14 rats in the GFP-CSC group and
14 rats in the ILK-CSC group were analyzed.
Detection results of cardiac function
of rats
Four weeks after transplantation, LVESD and LVEDD of
rats in the ILK-CSC group were smaller than those in the GFP-CSC
group (P<0.05), but LVEF was higher than that in the GFP-CSC
group (P<0.05). In addition, LVESD and LVEDD of rats in the
GEP-CSC group were smaller than those in the NS group (P<0.05),
but LVEF was higher than that in the NS group (P<0.05) (Table I).
 | Table I.Detection results of cardiac function
of rats in each group mean ± standard deviation (SD). |
Table I.
Detection results of cardiac function
of rats in each group mean ± standard deviation (SD).
| Groups | Rats (n) | LVESD (mm) | LVEDD (mm) | LVEF (%) |
|---|
| NS | 17 | 7.01±0.48 | 11.19±0.52 | 50.17±4.08 |
| GFP-CSC | 14 |
5.85±0.21a |
8.96±0.57a |
56.70±4.25a |
| ILK-CSC | 14 |
4.11±0.28a,
b |
7.16±0.44a,
b |
69.88±5.61a, b |
| F value |
| 6.899 | 12.561 | 18.108 |
| P-value |
| 0.012 | <0.001 | <0.001 |
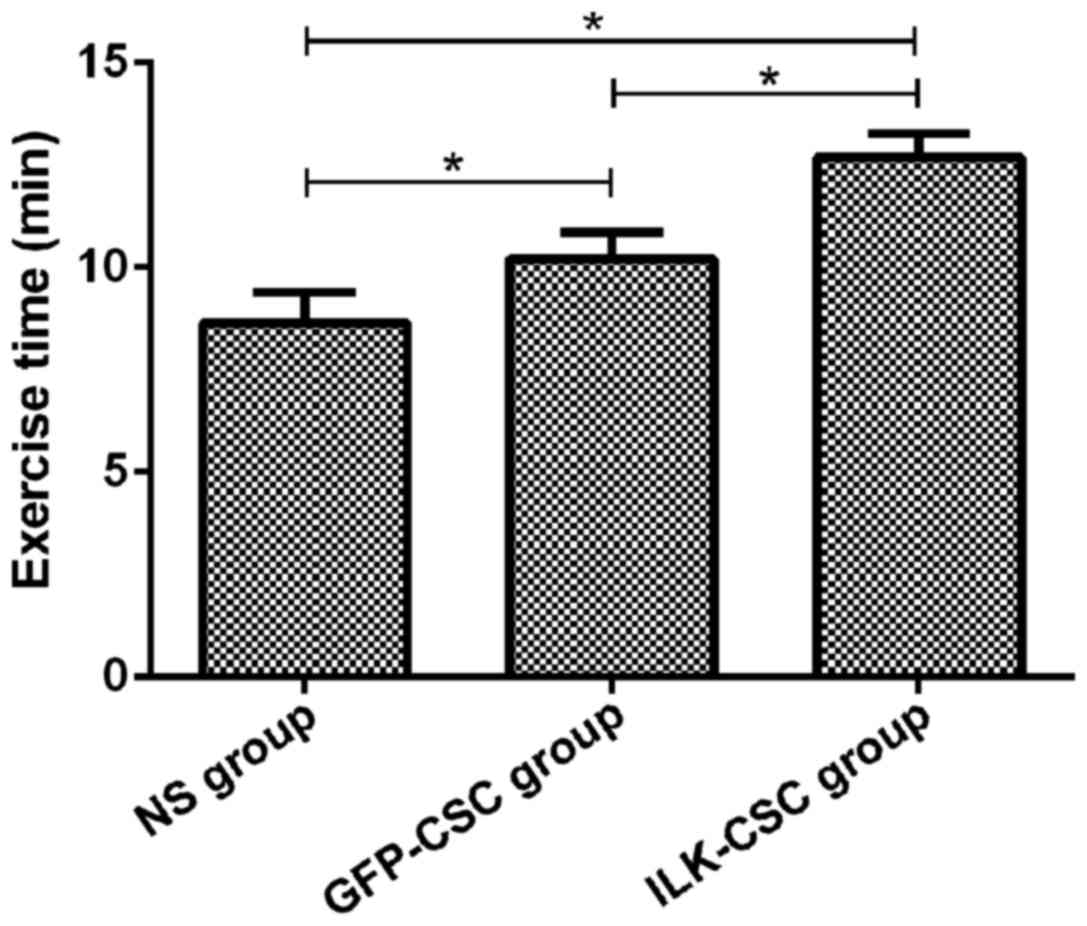
Measurement results of exercise
capacity of rats in each group
Results of the swimming experiment showed that the
exercise time in the ILK-CSC group (12.69±0.58 min) was longer than
that in the GFP-CSC (10.21±0.65 min) and NS (9.65±0.73 min) groups,
and differences were statistically significant (P<0.05). In
addition, the exercise time in the GFP-CSC group was longer than
that in the NS group (P<0.05) (Fig.
1).
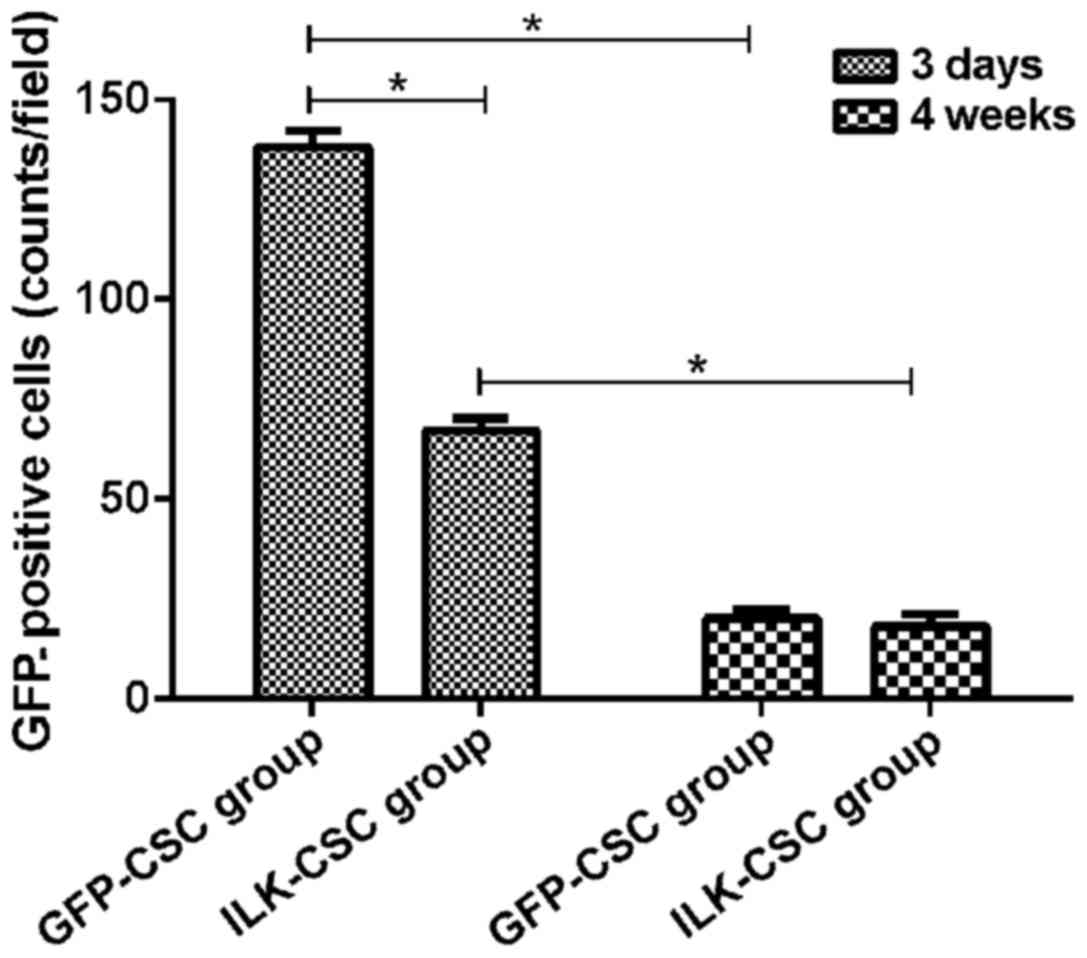
GFP expression in the myocardial
tissues in the GFP-CSC and ILK-CSC groups
GFP protein was expressed in the peripheral infarct
region in both the GFP-CSC and ILK-CSC groups at 3 days after
transplantation, and the expression of the GFP protein in the
GFP-CSC group (138±4 counts/field) was higher than that in the
ILK-CSC group (67±3 counts/field), and there was a statistically
significant difference (P<0.05). The GFP protein expression in
the ILK-CSC (20±5 counts/field) and GFP-CSC (18±4 counts/field)
groups 4 weeks after transplantation was lower than those 3 days
after transplantation (P<0.05), and there was no statistically
significant difference between the two groups (P>0.05) (Fig. 2).
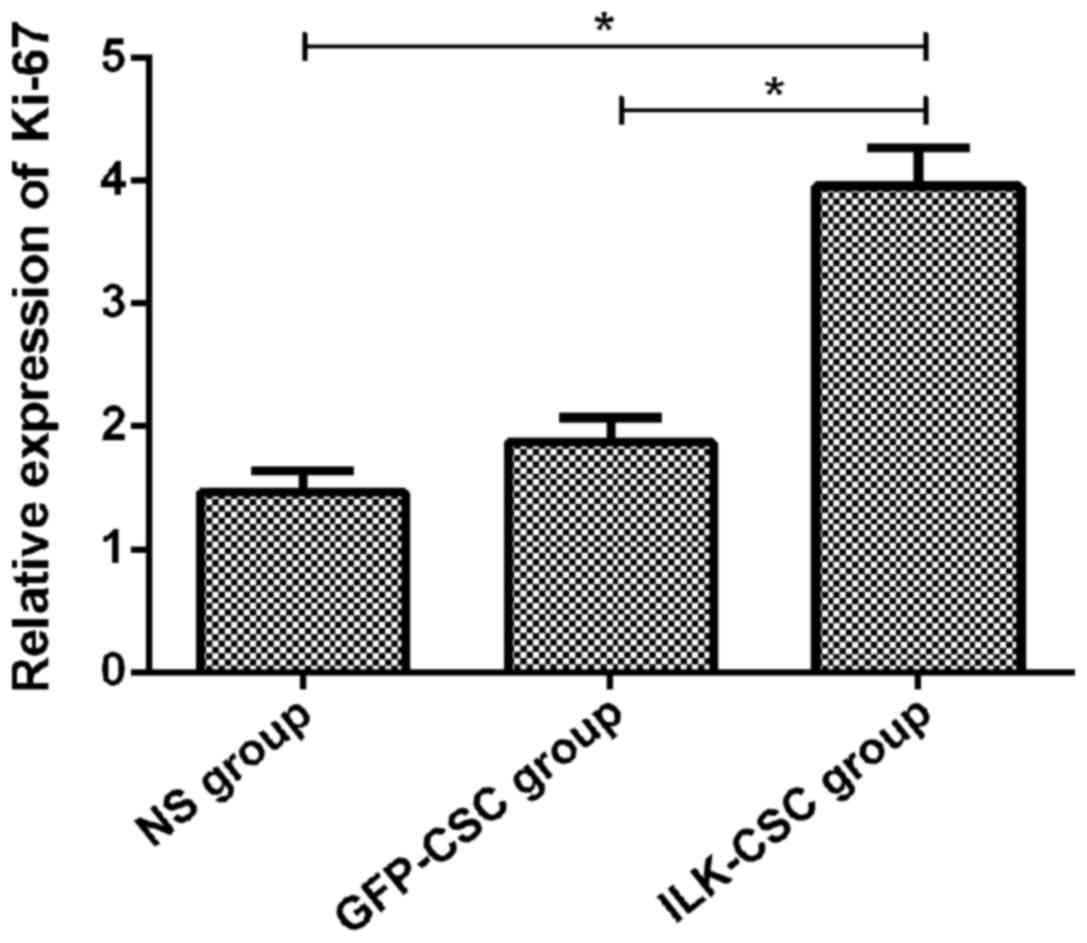
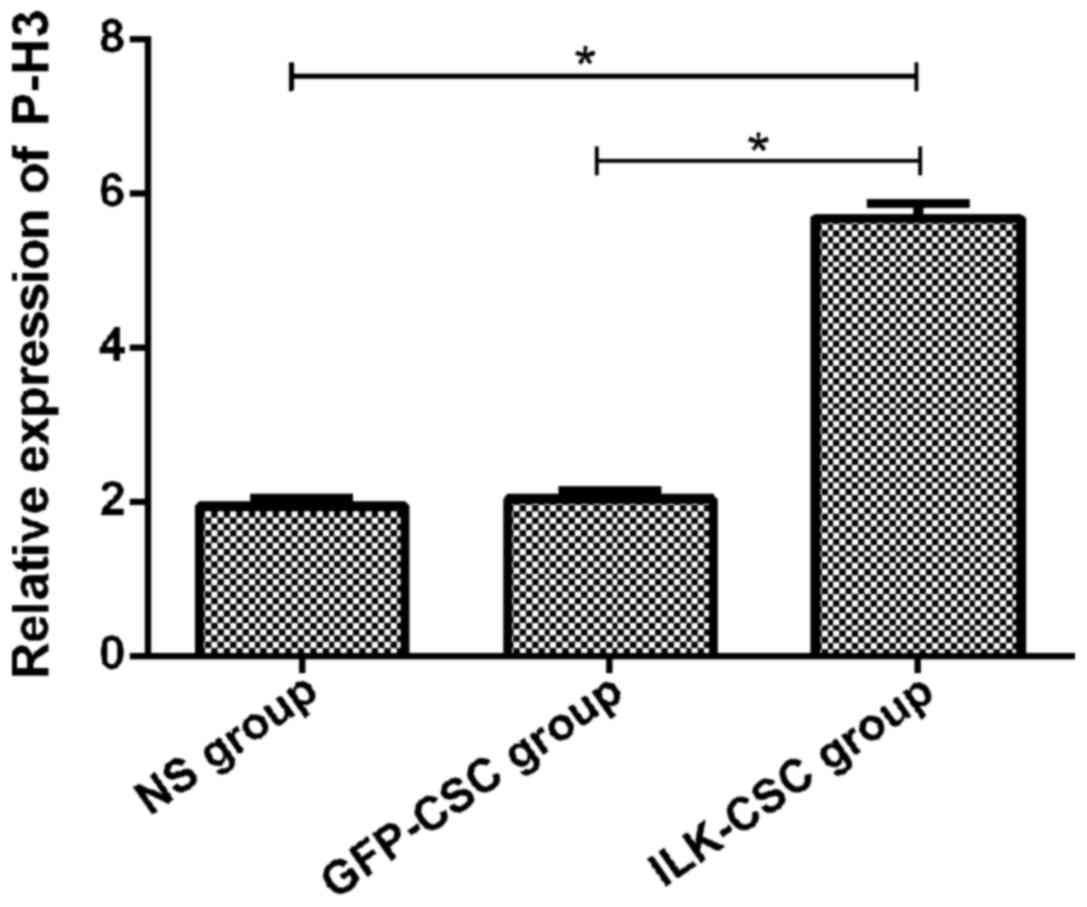
Expression of proliferation-related
proteins in myocardial tissues of left ventricle of rats in each
group
Immunohistochemical staining was performed for
proliferation-related proteins (Ki-67 and P-H3), and results
manifested that the optical density values of Ki-67 (3.95±0.31) and
P-H3 (5.68±0.19) proteins in the myocardial tissues of rats in the
ILK-CSC group were higher than those in the GFP-CSC (1.87±0.20,
2.03±0.11) and NS (1.46±0.18, 1.94±0.09) groups, and differences
were statistically significant (P<0.05). The optical density
values of the two kinds of proteins had no statistically
significant differences between the GFP-CSC and NS groups
(P>0.05) (Figs. 3 and 4).
Discussion
MI is an issue seriously threatening public health
and safety, as well as a global health problem. After MI,
irreversible death occurs in myocardial cells, leading to cardiac
dysfunction, such as decline in local cardiac contractility, and
even heart failure (2). Traditional
treatment methods, such as percutaneous transluminal coronary
angioplasty, myocardial reperfusion therapy or coronary artery
bypass grafting, can improve patients' cardiac function to some
extent, but the prognosis is poor (5). CSCs have superior performance of
directional differentiation, which can be directionally
differentiated into myocardial cells, providing a new choice for
cardiac cell transplantation therapy after MI (8). Zhong and Rao (18) studied and showed that after the
treatment of ischemic cardiomyopathy with CSC transplantation
therapy, the migration and proliferation capabilities of CSCs are
superior, there are many new cells and blood vessels in the MI
region, and cardiac function recovery is better. ILK can regulate
intracellular signaling pathways and transmit extracellular signals
into cells, thereby promoting cell survival, reducing apoptosis and
promoting cell proliferation and differentiation (3,19,20).
In this study, CSCs in rats were transfected with
GFP adenovirus vector overexpressing ILK to investigate the effects
of transplantation of CSCs overexpressing ILK on cardiac function,
exercise capacity and myocardial cell proliferation of rats with
acute MI. During the experimental process, the experimental
procedures were strictly implemented, and the scientific,
standardized and strict internal quality control was also adopted,
so experimental results had high accuracy and reliability.
Echocardiography results demonstrated that LVESD and LVEDD of rats
in the ILK-CSC group 4 weeks after transplantation were smaller
than those in the GFP-CSC group, but LVEF was higher than that in
the GFP-CSC group, suggesting that transplantation of CSCs
overexpressing ILK can improve cardiac function, and its efficacy
is better than that of ordinary CSCs. Moreover, results of the
exhaustive swimming experiment revealed that the exercise time in
the ILK-CSC group was longer than those in the GFP-CSC and NS
groups, indicating that the transplantation of CSCs overexpressing
ILK can improve the rats exercise capacity. Hannigan et al
(20) studied and showed that
injecting adenovirus overexpressing ILK around the infarct region
in rats after acute MI can improve cardiac function, increase
myocardial cell proliferation and reduce apoptosis. ILK can protect
the myocardial cells of neonatal rats from apoptosis, increase the
survival rate of myocardial cells, and improve cardiac function,
thereby improving the exercise capacity of rats after
transplantation (21,22).
Rats were sacrificed 3 days and 4 weeks after
transplantation, and frozen sections were observed under the
fluorescence microscope to detect the GFP expression in myocardial
tissues in the infarct region. Results demonstrated that the GFP
expression was observed in the peripheral infarct region of rats in
the IKL-CSC and GFP-CSC groups at 3 days after transplantation, and
it was significantly increased in the ILK-CSC group compared with
that in the GFP-CSC group, indicating that the high expression of
ILK can promote the survival ability of transplanted cells in the
peripheral infarct region after MI. Ki-67 is a cell cycle marker
that is specifically expressed in proliferating cells (23), and P-H3 is a kind of phosphorylated
histone that is a marker of cell mitosis, both of which exist in
the process of cell DNA synthesis and can reflect the cell
proliferation (24). Results of
immunohistochemical staining manifested that the expression levels
of Ki-67 and P-H3 proteins in the myocardial cells of rats in the
ILK-CSC group were higher than those in the GFP-CSC and NS groups,
indicating that ILK-CSC transplantation has a stronger effect on
activating the proliferation of myocardial cells. In a word,
results of this study were basically consistent with those in other
studies (25,26). The possible reason for the enhanced
proliferation of myocardial cells is that the ILK overexpression
contributes to the survival of CSCs in the myocardium, and then
CSCs are differentiated into myocardial cells with proliferation
capacity, or myocardial cells secrete regulatory factors after the
ILK-CSC transplantation, which is beneficial to the survival and
proliferation of original myocardial cells (27).
In conclusion, a rat model of MI was established,
and the experiment was carried out on rats transplanted with
ILK-CSC in this study. Results indicated that transplantation of
CSCs overexpressing ILK can promote proliferation of myocardial
cells and restore cardiac function and exercise capacity.
Therefore, transplantation of CSCs overexpressing ILK can be used
as a new direction in the treatment of MI.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
FZ drafted this manuscript. FZ and FG contributed to
the construction of the rat model of MI and cell transplantation,
The exhaustive swimming experiment was performed by both authors.
Both authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Weifang People's Hospital (Weifang, China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Desai R, Patel U, Sharma S, Amin P, Bhuva
R, Patel MS, Sharma N, Shah M, Patel S, Savani S, et al:
Recreational marijuana use and acute myocardial infarction:
Insights from nationwide inpatient sample in the United States.
Cureus. 9:e18162017.PubMed/NCBI
|
|
2
|
Andreadou I, Efentakis P, Balafas E,
Togliatto G, Davos CH, Varela A, Dimitriou CA, Nikolaou PE, Maratou
EV, et al: Empagliflozin limits myocardial infarction in vivo and
cell death in vitro: Role of STAT3, Mitochondria, and Redox
Aspects. Front Physiol. 8:10772017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dinser L, Meisinger C, Amann U, Heier M,
Thilo C, Kuch B, Peters A and Kirchberger I: Peripheral arterial
disease is associated with higher mortality in patients with
incident acute myocardial infarction. Eur J Intern Med.
18:30007–30004. 2018.
|
|
4
|
Clemens KK, Shariff SZ, McArthur E and
Hegele RA: Ezetimibe prescriptions in older Canadian adults after
an acute myocardial infarction: A population-based cohort study.
Lipids Health Dis. 17:82018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cimmino G, D'Andrea D, Mauro C, Morisco C
and Cirillo P: Treatment of acute myocardial infarction in 2017. G
Ital Cardiol (Rome). 18:3–10. 2017.(In Italian).
|
|
6
|
Noble S and Roffi M: Routine beta-blocker
administration following acute myocardial infarction: Why still an
unsolved issue? J Thorac Dis. 9:4191–4194. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Poulos J: The limited application of stem
cells in medicine: A review. Stem Cell Res Ther. 9:12018.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Husby S and Grønbæk K: Mature lymphoid
malignancies: Origin, stem cells, and chronicity. Blood Adv.
1:2444–2455. 2017.PubMed/NCBI
|
|
9
|
Li JJ, Liu Y, Zhao J, Li AY and Wang DM:
Transplantation of cardiac stem cells overexpressing
integrin-linked kinase improves cardiac function in a rat model of
acute myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi.
45:880–886. 2017.(In Chinese). PubMed/NCBI
|
|
10
|
Sussman MA: Cardiac stem cells: Working
independently together. J Am Coll Cardiol. 70:742–744. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Leong YY, Ng WH, Ellison-Hughes GM and Tan
JJ: Cardiac stem cells for myocardial regeneration: They are not
alone. Front Cardiovasc Med. 4:472017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lader J, Stachel M and Bu L: Cardiac stem
cells for myocardial regeneration: Promising but not ready for
prime time. Curr Opin Biotechnol. 47:30–35. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jackson R, Mount S, Ye B, Mayfield AE,
Chan V, Boodhwani M, Davies RA, Haddad H and Davis DR: Isolation of
human explant derived cardiac stem cells from cryopreserved heart
tissue. PLoS One. 12:e01760002017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao J, Liu N, Hao X, Que L, Liu J and
Tang X: Association between integrin-linked kinase and hyperthermia
in oral squamous cell carcinoma. Oncol Lett. 14:7705–7714.
2017.PubMed/NCBI
|
|
15
|
Olmos G, López-Ongil S and Ruiz Torres MP:
Integrin-linked kinase: A new actor in the ageing process? Exp
Gerontol. 100:87–90. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lu W, Xie J, Gu R and Xu B: Expression of
integrin-linked kinase improves cardiac function in a swine model
of myocardial infarction. Exp Ther Med. 13:1868–1874. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bai J, Gu R, Wang B, Zhang N, Kang L and
Xu B: Overexpression of integrin-linked kinase improves cardiac
function in a rat model of doxorubicin-induced chronic heart
failure. Zhonghua Xin Xue Guan Bing Za Zhi. 42:225–229. 2014.(In
Chinese). PubMed/NCBI
|
|
18
|
Zhong Y and Rao L: Atrioventricular block
after reperfusion: A reflection on early beta-blocker therapy for
acute myocardial infarction. Anatol J Cardiol. 18:438–439.
2017.PubMed/NCBI
|
|
19
|
Yin Z, Yu B, Liu W and Lan K: Blood
transfusion and mortality in myocardial infarction: An updated
meta-analysis. Oncotarget. 8:102254–102262. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hannigan GE, Coles JG and Dedhar S:
Integrin-linked kinase at the heart of cardiac contractility,
repair, and disease. Circ Res. 100:1408–1414. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bock-Marquette I, Saxena A, White MD,
Dimaio JM and Srivastava D: Thymosin beta4 activates
integrin-linked kinase and promotes cardiac cell migration,
survival and cardiac repair. Nature. 432:466–472. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bendig G, Grimmler M, Huttner IG, Wessels
G, Dahme T, Just S, Trano N, Katus HA, Fishman MC and Rottbauer W:
Integrin-linked kinase, a novel component of the cardiac mechanical
stretch sensor, controls contractility in the zebrafish heart.
Genes Dev. 20:2361–2372. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Raynov AM, Moon SK, Choung YH, Hong SP and
Park K: Nucleoplasm staining patterns and cell cycle-associated
expression of Ki-67 in middle ear cholesteatoma. Am J Otolaryngol.
26:296–301. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
López-Sánchez N, Müller U and Frade JM:
Lengthening of G2/mitosis in cortical precursors from mice lacking
β-amyloid precursor protein. Neuroscience. 130:51–60. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mu D, Zhang XL, Xie J, Yuan HH, Wang K,
Huang W, Li GN, Lu JR, Mao LJ, Wang L, et al: Intracoronary
transplantation of mesenchymal stem cells with overexpressed
integrin-linked kinase improves cardiac function in porcine
myocardial infarction. Sci Rep. 6:191552016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mao Q, Lin C, Gao J, Liang X, Gao W, Shen
L, Kang L and Xu B: Mesenchymal stem cells overexpressing
integrin-linked kinase attenuate left ventricular remodeling and
improve cardiac function after myocardial infarction. Mol Cell
Biochem. 397:203–214. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ding L, Dong L, Chen X, Zhang L, Xu X,
Ferro A and Xu B: Increased expression of integrin-linked kinase
attenuates left ventricular remodeling and improves cardiac
function after myocardial infarction. Circulation. 120:764–773.
2009. View Article : Google Scholar : PubMed/NCBI
|