Introduction
Clinically common left heart diseases (LHD) that
cause pulmonary hypertension (PH) include the following: i) Heart
failure: Left ventricular (LV) systolic dysfunction (e.g., dilated
cardiomyopathy and ischemic cardiomyopathy) and LV diastolic
dysfunction (e.g., hypertension, coronary heart disease,
hypertrophic cardiomyopathy); and ii) valvular heart disease and
other diseases, including left atrial disease (e.g., left atrial
myxoma or thrombosis), as well as certain types of congenital heart
disease. Left heart disease is one of the most common causes of PH
in the clinic. Data of a previous study suggest that 2/3 of chronic
heart failure cases may be associated with PH (1). An estimate of 60% of patients with
severe LV systolic dysfunction and 70% of patients with isolated LV
diastolic dysfunction may have PH (2). The diagnosis of PH due to LHD (PH-LHD)
is based on a mean pulmonary artery pressure (mPAP) of ≥25 mmHg
determined by a right heart catheter in the resting condition, or
of >30 mmHg in the active state. Furthermore, the simultaneous
determination of a left atrial pressure and pulmonary capillary
wedge pressure (PCWP) of >15 mmHg is required for the clinical
diagnosis. PH-LHD may occur due to an increased LV filling
pressure, and with the pulmonary arterial pressure progressively
increasing, the pulmonary artery may contract irreversible damage
and pulmonary vascular structural and functional remodeling,
resulting in right ventricular dysfunction or failure. Although the
study of the mechanisms of PH-LHD has achieved certain progress in
recent years, no specific treatment is currently available. The
efficacy and safety of targeted therapies for pulmonary artery
hypertension (PAH) in patients with PH-LHD remain to be determined.
As the results of clinical trials of targeted drugs for PH-LHD are
mostly negative or neutral, it is required to explore alternative
drugs that are effective against PH-LHD and to prove their
effectiveness. Milrinone is a commonly used drug for the treatment
of heart failure, and has been reported to also have an effect on
PH. In 2012, Guo (3) reported that
the phenomenon of secondary PH was more common in patients with
severe left heart valvular disease compared with other types of
PH-LHD. Inhalation of milrinone significantly reduces the pulmonary
artery pressure and pulmonary vascular resistance (PVR), increases
the cardiac index, while not having any significant effect on the
patients' heart rate (HR) and systemic vascular resistance;
inhalation of milrinone was efficient in reducing the PH and PVR,
and its effect was stronger than that on the systemic circulation,
reflecting a good selectivity to pulmonary vessels (3). In 2012, Yu and Shi (4) indicated that milrinone effectively
reduces PH, improves oxygenation and is a safe and effective drug
for reducing PH in patients with congenital heart disease. In 2013,
a study by Xu et al (5),
including 20 patients with moderate PH after cardiac surgery,
indicated that milrinone has a synergistic effect with dopamine on
increasing myocardial contractility and cardiac output to decrease
pulmonary artery pressure. In 2014, Yao et al (6) reported that milrinone improves the
heart function and effectively reduces PH in patients with PH due
to congenital heart disease following operation of the plateau
area; patients with congenital heart disease in the study came from
altitude of 2,100–3,800 m; PH formation and progression were
accelerated by hypoxia and low air pressure. As a specific
phosphodiesterase inhibitor, milrinone inhibits the cleavage of
AMP, and increases intracellular concentrations of cAMP and the
influx of Ca2+ to increase myocardial contractility. At
the same time, milrinone highly selectively increases the
concentration of cGMP in the pulmonary vascular smooth muscle via
activation of protein kinase G, increased opening of potassium ion
channels, hyperpolarization of the cell membrane and inhibition of
Ca2+ influx, resulting in a decrease in the
intracellular Ca2+ concentration, relaxation of smooth
muscle cells and vasodilation, and reduction of pulmonary arterial
pressure. In the present study, PH-LHD patients were treated with
milrinone injection, and differences in ultrasound indexes and
biochemical indexes were observed and analyzed prior to and
following treatment to evaluate its efficacy and safety. The
innovation of the present study lies in the following points: i)
Single primary disease. The cases included in the present study are
of coronary heart disease, but previous studies have assessed cases
with multiple primary diseases. Due to differences in the
pathogenesis of different primary diseases, there are also
differences in the mechanisms leading to PH. ii) Different doses.
To observe the efficacy and safety of milrinone, different doses
were administered to patients with PH-LHD. iii) Different severity.
The efficacy of milrinone was assessed in patients with different
severities of PH-LHD. iv) Evaluation of right ventricular function.
Only few previous studies have assessed the effects of milrinone on
right ventricular function in patients with PH-LHD.
Patients and methods
Patients
A total of 60 coronary heart disease patients with
PH-LHD hospitalized between May 2016 and May 2017 were enrolled in
the present study. The patients were randomly divided into three
groups: Group A and group B as the treatment groups, and group C as
the control group (n=20 in each group). Among them, group A
comprised 9 male and 11 female cases (age, 60.2±3.3 years), group B
included 12 male and 8 female cases (age, 59.9±4.2 years) and group
C comprised 10 male and 10 female cases (age, 60.8±6.0 years).
There was no significant difference between the three groups in
terms of sex, age, supine systolic pressure, supine diastolic
pressure, mean arterial pressure and supine HR. All of the
participants of the present study provided written informed consent
and volunteered to join the study. The study was approved by the
Ethics Committee of the Sixth People's Hospital of Jinan (Jinan,
China).
Inclusion criteria
The criteria for inclusion were systolic heart
failure (left heart failure or total heart failure), LV ejection
fraction (LVEF) ≤50%. Referring to the 2009 European guidelines for
Pulmonary Hypertension, PASP <37 mmHg under resting condition in
normal subjects (7). If PASP is
>50 mmHg, it can be used to diagnose PH (7). When 37<PASP<50 mmHg, further
cardiac catheterization should be performed for diagnosis (7). In the current study, PASP >50 mmHg
was used as diagnostic criteria for PH-LHD. According to the
severity of pulmonary hypertension, patients in each group were
divided into a mild group (PASP, 51–60 mmHg), a moderate group
(PASP, 61–70 mmHg) and a severe group (PASP, >70 mmHg).
Exclusion criteria
i) PH associated with chronic obstructive pulmonary
disease, interstitial lung disease, pulmonary disease and hypoxemia
caused by sleep apnea, as well as idiopathic, familial and other
underlying factors (collagen, portal hypertension, infection,
drugs/toxins), and PH caused by chronic thrombosis, embolism or
diseases including sarcoidosis and histiocytosis. ii) Acute
myocardial infarction, severe arrhythmia, dilated cardiomyopathy,
hypertrophic cardiomyopathy, restrictive cardiomyopathy, valvular
heart disease or constrictive pericarditis. iii) Cardiogenic shock
with insufficient blood volume or vasodilator. iv) Supine systolic
pressure <90 or >180 mmHg. v) Pulmonary vascular
malformation. vi) Cerebrovascular accident. vii) Malignant tumor.
viii) Severe hepatic dysfunction (elevated transaminase exceeding
the normal limit by 3-fold) and renal failure. ix) Serious
infectious diseases. x) Uncontrolled thyroid disease. xi)
Cyclophilin drugs and endothelin receptor antagonists have been
used in the past and other targeted drugs for pulmonary
hypertension. xii) Participation in other clinical studies in the
previous 3 months. xiii) A history of allergies to specific
phosphodiesterase inhibitors or contraindications for the use of
such drugs, including hypotension and arrhythmias. xiv) Cardiac
resynchronization pacemaker. xv) Mental sickness.
Research drug use
The research drug was milrinone injection, whose
commodity name is Lunan Li Kang, produced by Nonan Bate
Pharmaceuticals Co., Ltd (Linyi, China; approval no. H10970051). A
volume of 5 ml of the formulation was equivalent to 5 mg
milrinone.
Equipment and preparations
A Philips CX-50 type color Doppler ultrasound
(Philips Medical Co., Eindhoven, the Netherlands) was used in the
present study. NT-proBNP was detected by a Roche Cobas-e601
automatic biochemical analyzer (Roche Diagnostics, Basel,
Switzerland). Determination of NT-proBNP was performed with a
chemiluminescent immunoassay provided by Roche Diagnostics (cat.
nos. 14129204, 16899201 and 16899203). HsCRP was detected by a
Siemens BN II specific protein analyzer (Siemens AG, Munich,
Germany). The hsCRP kit was provided by Siemens AG (cat. nos.
167551C and 167553C).
Treatment
The same conventional treatment was used in the
three groups, including digitalis, angiotensin-converting enzyme
inhibitor/angiotensin II receptor antagonist, β receptor blocker
and diuretics. First, group A and group B were given intravenous
milrinone for 10 min at rate 5 µg/kg/min. The maintenance dose for
group A and B were 0.25 and 0.5 µg/kg/min of milrinone,
respectively, administered by continuous application for 5 days.
Group C was not treated with milrinone. Echocardiography was
performed prior and following milrinone treatment and blood samples
were taken to determine the biochemical parameters. HR, blood
pressure (BP) and various examination results were monitored prior
to and following treatment.
Observation indexes
General observation indexes
The following indicators were determined prior to
treatment: BP, HR, blood routine, urine routine, stool routine,
liver function, renal function, blood glucose, blood lipids, blood
electrolytes and electrocardiogram examination.
Echocardiography
Echocardiography was performed prior and following
milrinone treatment. The ultrasonic instrument was a Philips CX-50
type color Doppler ultrasound, equipped with a S51 heart
two-dimensional probe, a frequency of 1–5 MHz and a frame frequency
of 60–90 frames/s. The patient was placed in the left lateral
decubitus position. M-mode echocardiography was used on the long
axial of sternum side to measure the left atrial diameter (LAD), LV
end diastolic diameter (LVEDd) and LVEF. The apical four chamber
was viewed and the tricuspid annular plane systolic excursion
(TAPSE) was measured. The right ventricular end-diastolic area and
end-systole area was measured, and the right ventricular fractional
area change (RVFAC) was calculated. PASP was measured by tricuspid
regurgitation estimation, with PASP equaling the right ventricular
systolic pressure (RVSP). The RVSP was calculated according to the
modified formula of Bernoulli (RVSP=4Vmax2 + RAP), where
Vmax is the maximum tricuspid regurgitation velocity (m/sec) and
RAP is the right atrial pressure (8). The RAP may be estimated based on the
size of the right atrium and the extent of the tricuspid
regurgitation. The right atrium diameter was normal, mild tricuspid
regurgitation was observed and the RAP was 5 mmHg. The right atrium
was slightly enlarged, moderate three tricuspid regurgitation
occurred and the RAP was 10 mmHg. The right atrium was markedly
enlarged, severe three tricuspid regurgitation was observed and the
RAP was 15 mmHg. The above indicators were measured by two
ultrasound attending physicians with 5 years of experience who were
blinded to the grouping. All records were stored on a computer for
data analysis.
Detection of NT-proBNP
Blood (5 ml) was drawn from the elbow vein prior to
and following pre-therapy, collected in EDTA anticoagulant vacuum
tubes, and after standing for 30 min at room temperature, serum was
separated by centrifugation at 1,000 × g for 15 min at room
temperature. The concentration of NT-proBNP was determined with a
Roche Cobas-e601 automatic biochemical analyzer with an
electrochemiluminescence immunoassay. The range of measurements
covered by the assay was 5–35,000 pg/ml. The determination
principle is the double antibody clamp method and the protocol was
as follows: First, 20 µl specimen, biotinylated monoclonal
NT-proBNP-specific antibody and monoclonal NT-proBNP-specific
antibody labeled with ruthenium complex were reacted to form a
Sandwich complex. Subsequently, magnetic beads coated with
streptavidin were added, and through the interaction between biotin
and streptavidin, the sandwich complex was bound to the magnetic
beads. The reaction mixture was added to a measuring tank, where
magnetic particles were adsorbed to the electrode surface by
electromagnetic action. Voltage was added to the electrode to
produce electrochemiluminescence and light signals were measured
using photomultiplier tubes. Specific curves were obtained by
two-point calibration and the major curve provided by the reagent
bar code was used to determine the results.
Detection of hsCRP
The concentration of hsCRP in the serum was
determined by a Siemens BN II specific protein analyzer via an
immunoturbidimetric test (normal value, 0–3 mg/ml). Its
determination principle was as follows: The CRP in the sample is
reacted with the CRP-specific antibody coated on latex particles
contained in the reagent to form an immunoprecipitated, whose
amount is proportional to the concentration of CRP in the
specimen.
Observation of adverse events
By clinical observation, type, time, duration,
severity, process and outcome of adverse events that occurred
following administration were recorded. The safety of the drug was
evaluated objectively by recording whether the drug administration
was terminated and whether any measures to treat the adverse events
were taken. The adverse events were then classified into five
levels of relevance: Definitely relevant, probably relevant,
possibly relevant, possibly irrelevant and irrelevant. The items in
the first three levels were classified as adverse reactions and
their incidence was determined. Once an adverse reaction occurred,
the necessary treatment measures were taken according to the
condition, which included adjustment of the dose, temporary
interruption of drug use and decision to terminate the
administration. Patients with severe adverse reactions were
discontinued.
Statistical analysis
In the present study, SPSS 22.0 statistical software
(IBM Corp., Armonk, NY, USA) was applied for statistical analysis.
The measurement data were expressed as the mean ± standard
deviation. The differences in measurement data among the groups
were analyzed by a homogeneity test of variances (least-significant
difference method). Analysis of variance followed by Tukey's honest
significant differences test was applied to make pairwise
comparisons. For the above, P<0.05 was considered to indicate a
statistically significant difference. The paired t-test was used to
compare differences between the pre-therapy and post-treatment
groups, and P<0.05 was considered to indicate a statistically
significant difference. Pearson's correlation coefficient was
determined to assess the correlation between PASP and LAD, LVEDd,
LVEF, TAPSE, RVFAC, NT-proBNP and hsCRP, with 0.8<x≤1.0,
extremely strong correlation; 0.6<x≤0.8, strong correlation;
0.4<x≤0.6, medium correlation; 0.2<x≤0.4, weak correlation;
0.0–0.2, very weak or no correlation. P<0.01 was considered to
indicate a statistically significant difference.
Results
Experimental results prior to
treatment
The treatment groups (groups A and B) and the
control group C exhibited no statistically significant differences
in the measurement indexes (LAD, LVEDd, LVEF, PASP, TAPSE, RVFAC,
NT-proBNP and hsCRP) prior to treatment (P>0.05; Table I).
 | Table I.Comparison of general data,
echocardiography results and biochemical markers levels of three
groups of patients with pulmonary hypertension due to left heart
disease prior to treatment. |
Table I.
Comparison of general data,
echocardiography results and biochemical markers levels of three
groups of patients with pulmonary hypertension due to left heart
disease prior to treatment.
| Parameter | Group A (n=20) | Group B (n=20) | Group C (n=20) | F | P-value |
|---|
| Age (years) | 60.2±3.3 | 59.9±4.2 | 60.8±6.0 | 0.035 | 0.965 |
| Male sex [cases
(%)] | 9 (45) | 12 (60) | 10 (50) | 1.262 | 0.291 |
| SBP (mmHg) | 132.2±4.8 | 133.8±9.1 | 128.2±8.0 | 0.039 | 0.962 |
| NBP (mmHg) | 86.8±5.2 | 84.7±5.4 | 85.3±4.0 | 0.053 | 0.948 |
| MAP (mmHg) | 101.9±4.7 | 101.4±6.4 | 99.6±5.1 | 0.034 | 0.967 |
| HR (per min) | 80.6±10.3 | 83.6±8.0 | 81.1±8.9 | 0.042 | 0.959 |
| LAD (mm) | 46.4±4.1 | 46.5±4.8 | 46.2±4.7 | 0.015 | 0.985 |
| LVEDd (mm) | 61.7±5.4 | 62.0±6.6 | 61.9±4.6 | 0.015 | 0.985 |
| LVEF (%) | 39.1±6.2 | 39.6±7.3 | 38.1±6.1 | 0.269 | 0.765 |
| PASP (mmHg) | 62.3±6.9 | 62.1±6.3 | 62.4±7.4 | 0.009 | 0.991 |
| TAPSE (mm) | 15.0±3.6 | 15.1±3.4 | 15.1±2.8 | 0.011 | 0.989 |
| RVFAC (%) | 35.1±4.1 | 35.2±4.2 | 35.0±4.7 | 0.011 | 0.989 |
| NT-proBNP
(pg/ml) |
5,153.4±1,821.2 |
5,176.3±1,675.4 |
5,157.3±1,924.5 | 0.001 | 0.999 |
| hsCRP (mg/l) | 6.5±2.9 | 6.3±3.6 | 5.5±2.9 | 0.566 | 0.571 |
Comparison of echocardiographic
results and levels of biochemical markers between the three groups
of PH-LHD patients prior to and following treatment
In group A, the RVFAC following treatment was
significantly higher compared with prior to treatment (P<0.01;
Table II). The LVEF and TAPSE
following treatment were significantly higher compared with prior
to treatment (P<0.05; Table II).
The LVEDd, PASP, NT-proBNP and hsCRP following treatment were
significantly lower compared with prior to treatment (P<0.01;
Table II). The LAD following
treatment was significantly lower compared with prior to treatment
(P<0.05; Table II).
 | Table II.Comparison of echocardiographic
results and levels of biochemical markers between the three groups
of patients with pulmonary hypertension due to left heart disease
prior to and following treatment. |
Table II.
Comparison of echocardiographic
results and levels of biochemical markers between the three groups
of patients with pulmonary hypertension due to left heart disease
prior to and following treatment.
|
| Group A (n=20) | Group B (n=20) | Group C (n=20) |
|---|
|
|
|
|
|
|---|
| Parameter | Pre-treatment | Post-treatment | P-value | Pre-treatment | Post-treatment | P-value | Pre-treatment | Post-treatment | P-value |
|---|
| LAD (mm) | 46.4±4.1 | 43.0±4.9 | 0.024 | 46.5±4.8 | 39.7±5.9 | <0.001 | 46.2±4.7 | 44.5±5.5 | 0.286 |
| LVEDd (mm) | 61.7±5.4 | 56.7±4.7 | 0.004 | 62.0±6.6 | 54.5±5.6 | <0.001 | 61.9±4.6 | 59.7±5.0 | 0.166 |
| LVEF (%) | 39.1±6.2 | 44.0±6.6 | 0.022 | 39.6±7.3 | 49.4±8.2 | <0.001 | 38.1±6.1 | 40.4±6.3 | 0.250 |
| PASP (mmHg) | 62.3±6.9 | 52.9±7.4 | <0.001 | 62.1±6.3 | 47.3±7.6 | <0.001 | 62.4±7.4 | 59.4±8.7 | 0.242 |
| TAPSE (mm) | 15.0±3.6 | 17.4±4.0 | 0.017 | 15.1±3.4 | 18.4±4.0 | <0.001 | 15.1±2.8 | 15.8±3.2 | 0.510 |
| RVFAC (%) | 35.1±4.1 | 40.7±5.0 | <0.001 | 35.2±4.2 | 44.2±5.7 | <0.001 | 35.0±4.7 | 36.9±4.9 | 0.218 |
| NT-proBNP
(pg/ml) |
5,153.4±1,821.2 |
3,526.6±1,333.3 | <0.001 |
5,176.3±1,675.4 |
2,863.2±1,098.8 | <0.001 |
5,157.3±1,924.5 |
4,581.0±1,850.8 | <0.001 |
| hsCRP (mg/l) | 6.5±2.9 | 3.3±1.8 | <0.001 | 6.3±3.6 | 2.8±1.6 | <0.001 | 5.5±2.9 | 5.1±3.0 | 0.681 |
In group B, the LVEF, TAPSE and RVFAC following
treatment were higher than those prior to treatment, and the
difference was statistically significant (P<0.01; Table II). The LAD, LVEDd, PASP, NT-proBNP
and hsCRP following treatment were lower than those prior to
treatment, and the difference was statistically significant
(P<0.01; Table II).
In group C, the NT-proBNP following treatment was
lower than that prior to treatment, and the difference was
statistically significant (P<0.01; Table II). The LVEF, TAPSE and RVFAC
following treatment were higher than those prior to treatment, the
difference was not statistically significant (P>0.05; Table II). The LAD, LVEDd, PASP and hsCRP
following treatment were lower than those prior to treatment, the
difference was not statistically significant (P>0.05; Table II).
Comparison of echocardiography results
and levels of biochemical markers in patients of the different
groups following treatment
Following treatment, the LVEF in group B was higher
compared with that in group A, the difference was not statistically
significant (P>0.05; Table
III). The TAPSE and RVFAC of group B were higher than those of
group A, and the difference was statistically significant
(P<0.05; Table III). The PASP
of group B was lower than that of group A, and the difference was
statistically significant (P<0.05; Table III). The LAD, LVEDd, NT-proBNP and
hsCRP of group B were lower than those of group A; the difference
was not statistically significant (P>0.05; Table III).
 | Table III.Comparison of echocardiography
results and levels of biochemical markers between the three groups
following treatment. |
Table III.
Comparison of echocardiography
results and levels of biochemical markers between the three groups
following treatment.
|
|
|
|
|
|
|
| ANOVA |
|---|
|
|
|
|
|
|
|
|
|
|---|
| Parameter | Group A (n=20) | Group B (n=20) | Group C (n=20) | P1 | P2 | P3 | F | P |
|---|
| LAD (mm) | 43.0±4.9 | 39.7±5.9 | 44.5±5.5 | 0.061 | 0.012 | 0.381 | 4.032 | 0.023 |
| LVEDd (mm) | 56.7±4.7 | 54.5±5.6 | 59.7±5.0 | 0.187 | 0.014 | 0.154 | 3.712 | 0.031 |
| LVEF (%) | 44.0±6.6 | 49.4±8.2 | 40.4±6.3 | 0.064 | 0.001 | 0.112 | 6.195 | 0.004 |
| PASP (mmHg) | 52.9±7.4 | 47.3±7.6 | 59.4±8.7 | 0.025 | 0.000 | 0.015 | 11.547 | 0.000 |
| TAPSE (mm) | 17.4±4.0 | 18.4±4.0 | 15.8±3.2 | 0.037 | 0.000 | 0.043 | 9.119 | 0.000 |
| RVFAC (%) | 40.7±5.0 | 44.2±5.7 | 36.9±4.9 | 0.046 | 0.000 | 0.022 | 9.663 | 0.000 |
| NT-proBNP
(pg/ml) |
3,526.6±1,333.3 |
2,863.2±1,098.8 |
4,581.0±1,850.8 | 0.094 | 0.001 | 0.046 | 7.024 | 0.000 |
| hsCRP (mg/l) | 3.3±1.8 | 2.8±1.6 | 5.1±3.0 | 0.375 | 0.005 | 0.029 | 5.768 | 0.005 |
Following treatment, the TAPSE and RVFAC of group A
were higher than those of group C, and the difference was
statistically significant (P<0.05; Table III). The PASP, NT-proBNP and hsCRP
of group A were lower than those of group C, and the difference was
statistically significant (P<0.05; Table III). The LVEF of group A was higher
than that of group C; the difference was not statistically
significant (P>0.05; Table
III). The LAD and LVEDd of group A were lower than those of
group C; the difference was not statistically significant
(P>0.05; Table III).
Following treatment, the LVEF, TAPSE and RVFAC of
group B were higher than those of group C, and the difference was
statistically significant (P<0.05; Table III). The LAD, LVEDd, PASP,
NT-proBNP and hsCRP of group B were lower than those of group C,
and the difference was also statistically significant (P<0.05;
Table III).
Comparison of echocardiographic
results and biochemical markers levels between patients with
different severities of PH-LHD prior to and following
treatment
In group A, the LVEF, TAPSE and RVFAC in patients
with mild (n=10) and moderate (n=8) PH-LHD following treatment were
higher than those prior to treatment, and the difference was
statistically significant (P<0.01; Table IV). The LAD, LVEDd, PASP, NT-proBNP
and hsCRP in patients with mild and moderate PH-LHD following
treatment were lower than those prior to treatment, and the
difference was statistically significant (P<0.01; Table IV).
 | Table IV.Comparison of echocardiographic
results and levels of biochemical markers between patients with
different severities of PH due to left heart disease in group A
prior to and following treatment. |
Table IV.
Comparison of echocardiographic
results and levels of biochemical markers between patients with
different severities of PH due to left heart disease in group A
prior to and following treatment.
|
| Mild PH (n=10) | Moderate PH
(n=8) |
|---|
|
|
|
|
|---|
| Parameter | Pre-treatment | Post-treatment | P-value | Pre-treatment | Post-treatment | P-value |
|---|
| LAD (mm) | 43.5±3.0 | 39.5±3.5 | <0.001 | 48.0±1.3 | 45.1±1.5 | <0.001 |
| LVEDd (mm) | 58.2±3.4 | 53.6±2.4 | <0.001 | 63.4±3.3 | 58.1±2.6 | <0.001 |
| LVEF (%) | 44.1±2.8 | 49.1±3.1 | <0.001 | 35.8±2.6 | 40.6±3.3 | <0.001 |
| PASP (mmHg) | 56.5±2.6 | 46.8±3.6 | <0.001 | 66.0±2.1 | 56.9±2.0 | <0.001 |
| TAPSE (mm) | 17.4±1.4 | 21.2±1.8 | <0.001 | 14.4±1.7 | 18.0±3.1 | <0.001 |
| RVFAC (%) | 38.1±2.0 | 46.5±2.5 | <0.001 | 33.7±2.9 | 40.6±3.5 | <0.001 |
| NT-proBNP
(pg/ml) | 3,918.6±283.3 | 2,580.0±104.8 | <0.001 | 5,622.9±681.9 | 3,903.5±603.9 | <0.001 |
| hsCRP (mg/l) | 4.4±1.0 | 1.9±0.5 | <0.001 | 7.3±0.9 | 3.95±0.7 | <0.001 |
In group B, the LVEF, TAPSE and RVFAC in patients
with mild (n=10) and moderate (n=8) PH-LHD following treatment were
higher than those prior to treatment, and the difference was
statistically significant (P<0.01; Table V). The LAD, LVEDd, PASP, NT-proBNP
and hsCRP in the patients with mild and moderate PH-LHD following
treatment were lower than those prior to treatment, and the
difference was statistically significant (P<0.01; Table V).
 | Table V.Comparison of echocardiographic
results and levels of biochemical markers between patients with
different severities of PH due to left heart disease in group B
prior to and following treatment. |
Table V.
Comparison of echocardiographic
results and levels of biochemical markers between patients with
different severities of PH due to left heart disease in group B
prior to and following treatment.
|
| Mild PH (n=10) | Moderate PH
(n=8) |
|---|
|
|
|
|
|---|
| Parameter | Pre-treatment | Post-treatment | P-value | Pre-treatment | Post-treatment | P-value |
|---|
| LAD (mm) | 43.2±4.0 | 35.6±4.1 | <0.001 | 47.7±1.4 | 41.2±2.4 | <0.001 |
| LVEDd (mm) | 58.3±2.6 | 51.0±1.7 | <0.001 | 62.4±5.4 | 55.2±4.2 | <0.001 |
| LVEF (%) | 44.7±2.8 | 55.0±3.9 | <0.001 | 38.0±6.4 | 47.8±6.5 | <0.001 |
| PASP (mmHg) | 56.2±2.9 | 40.4±3.3 | <0.001 | 65.6±1.9 | 50.8±0.7 | <0.001 |
| TAPSE (mm) | 17.7±0.7 | 25.4±1.2 | <0.001 | 14.0±1.3 | 19.5±2.6 | <0.001 |
| RVFAC (%) | 37.7±2.0 | 48.4±1.4 | <0.001 | 33.9±2.6 | 42.1±2.4 | <0.001 |
| NT-proBNP
(pg/ml) | 3,911.7±288.1 | 2,022.2±137.9 | <0.001 | 5,576.7±789.2 | 3,197.3±680.1 | <0.001 |
| hsCRP (mg/l) | 3.8±1.2 | 1.6±0.4 | <0.001 | 6.9±1.5 | 3.2±0.6 | <0.001 |
In group C, the RVFAC in patients with mild (n=11)
and moderate (n=8) PH-LHD following treatment was higher than that
prior to treatment and the difference was statistically significant
(P<0.01; Table VI). The TAPSE in
patients with mild PH-LHD following treatment was higher than that
prior to treatment, and the difference was statistically
significant (P<0.05; Table VI).
The TAPSE in patients with moderate PH-LHD following treatment was
higher than that prior to treatment, and the difference was not
statistically significant (P>0.05; Table VI). The LVEF in patients with mild
and moderate PH-LHD following treatment was higher than that prior
to treatment, and the difference was statistically significant
(P<0.01 and P<0.05; Table
VI). The LAD, LVEDd, PASP and NT-proBNP in the patients with
mild and moderate PH-LHD following treatment were lower than those
prior to treatment, and the difference was statistically
significant (P<0.01; Table VI).
The hsCRP in the patients with mild PH-LHD following treatment was
lower than that prior to treatment, and the difference was
statistically significant (P<0.01; Table VI). The hsCRP in the patients with
moderate PH-LHD following treatment was lower than that prior to
treatment, and the difference was not statistically significant
(P>0.05; Table VI).
 | Table VI.Comparison of echocardiographic
results and levels of biochemical markers between patients with
different severities PH due to left heart disease in group C prior
to and following treatment. |
Table VI.
Comparison of echocardiographic
results and levels of biochemical markers between patients with
different severities PH due to left heart disease in group C prior
to and following treatment.
|
| Mild group PH
(n=11) | Moderate group PH
(n=8) |
|---|
|
|
|
|
|---|
| Parameter | Pre-treatment | Post-treatment | P-value | Pre-treatment | Post-treatment | P-value |
|---|
| LAD (mm) | 43.0±3.2 | 40.8±3.7 | <0.001 | 49.4±2.2 | 48.0±2.7 | 0.001 |
| LVEDd (mm) | 58.8±2.6 | 56.3±2.4 | <0.001 | 64.6±2.4 | 62.8±2.4 | <0.001 |
| LVEF (%) | 42.6±1.7 | 44.6±2.4 | 0.001 | 33.9±2.9 | 36.6±4.1 | 0.019 |
| PASP (mmHg) | 56.8±2.3 | 52.8±3.8 | <0.001 | 67.5±1.9 | 65.5±1.9 | <0.001 |
| TAPSE (mm) | 16.8±0.8 | 17.6±0.9 | 0.011 | 13.4±2.1 | 13.9±2.7 | 0.170 |
| RVFAC (%) | 38.7±1.3 | 40.6±1.3 | <0.001 | 31.3±1.5 | 33.3±2.3 | 0.001 |
| NT-proBNP
(pg/ml) | 4,008.5±183.0 | 3,525.5±182.0 | <0.001 |
5,908.5±1,017.4 |
5,223.4±1,024.0 | <0.001 |
| hsCRP (mg/l) | 3.3±0.6 | 2.8±0.8 | 0.003 | 7.7±1.9 | 7.4±1.8 | 0.186 |
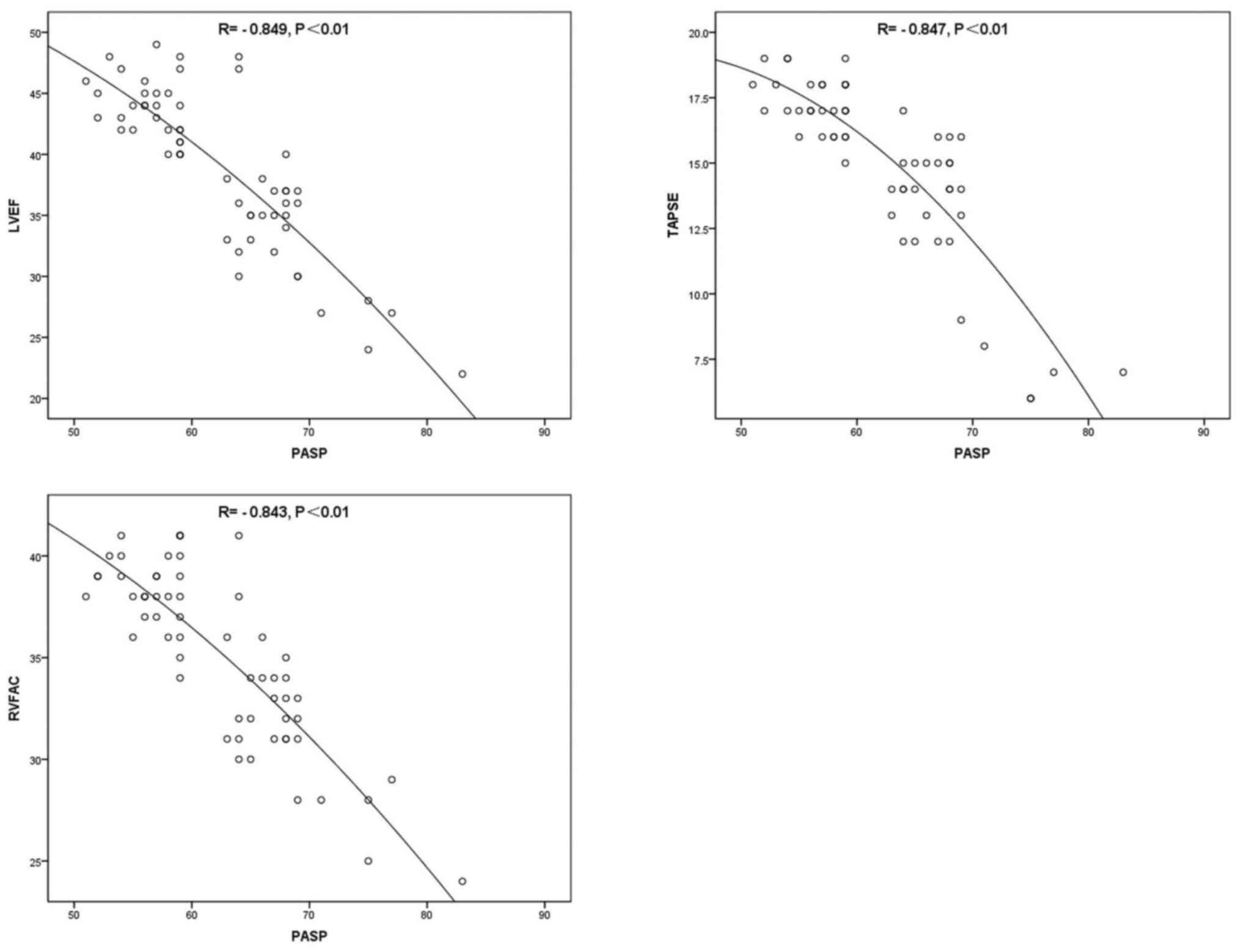
Correlation between PASP and other
indicators
PASP was positively correlated with LAD, LVEDd,
NT-proBNP and hsCRP (P<0.01; Fig.
1; Table VII), and negatively
correlated with LVEF, TAPSE and RVFAC (P<0.01; Fig. 2; Table
VII).
 | Figure 1.Scatter plots for the correlations
between PASP+LAD (R=0.835, P<0.01), PASP+LVEDd (R=0.760,
P<0.01), PASP+NT-proBNP (R=0.862, P<0.01) and PASP+hsCRP
(R=0.825, P<0.01) prior to therapy. PASP, pulmonary artery
systolic pressure; LAD, left atrial diameter; LVEDd, left ventricle
end diastolic diameter; NT-proBNP, N-terminal pro-B-type
natriuretic peptide; hsCRP, hypersensitive C-reactive protein. |
 | Table VII.Correlation between PASP and LAD,
LVEDd, LVEF, TAPSE, RVFAC, NT-proBNP and hsCRP prior to
treatment. |
Table VII.
Correlation between PASP and LAD,
LVEDd, LVEF, TAPSE, RVFAC, NT-proBNP and hsCRP prior to
treatment.
| Parameter | R | P-value |
|---|
| LAD | 0.835 | <0.01 |
| LVEDd | 0.760 | <0.01 |
| LVEF | −0.849 | <0.01 |
| TAPSE | −0.847 | <0.01 |
| RVFAC | −0.843 | <0.01 |
| NT-proBNP | 0.862 | <0.01 |
| hsCRP | 0.825 | <0.01 |
Comparison of adverse reactions in the
three groups of patients with PH-LHD
In group A (n=20), 2 cases of headache (10%), 2
cases of asthenia (10%), 1 case of HR increase (5%) and 1 case of
hypotension (5%) were encountered. Group B (n=20) included 1 case
of headache (5%), 2 cases of asthenia (10%), 1 case of HR increase
(5%) and 3 cases of hypotension (15%). In group C (n=20), 1 case of
headache (5%), 1 case of asthenia (5%) and 1 cases of HR increase
(5%) were encountered (Table
VIII). The maintenance dose of milrinone did not cause any
significant adverse reactions during the course of treatment.
 | Table VIII.Comparison of adverse reactions in
the three groups of patients with pulmonary hypertension due to
left heart disease, n (%). |
Table VIII.
Comparison of adverse reactions in
the three groups of patients with pulmonary hypertension due to
left heart disease, n (%).
|
| Group A (n=20) | Group B (n=20) | Group C (n=20) |
|---|
|
|
|
|
|
|---|
| Adverse
reaction | Cases incidence
(%) | Cases incidence
(%) | Cases incidence
(%) |
|---|
| Headache | 2 (10) | 1 (5) | 1 (5) |
| Asthenia | 2 (10) | 2 (10) | 1 (5) |
| Increased heat
rate | 1 (5) | 1 (5) | 1 (5) |
| Hypopiesia | 1 (5) | 3 (15) | 0 |
Discussion
A retrospective review from the US indicated that
77% of the centers used PAH targeted drugs for patients with PH-LHD
(9). Clinical trials on targeted
drugs for PH mostly provided negative or neutral results, and the
choice of the test population had a decisive role in the outcome,
it is also possible that the effective dose of PAH and PH-LHD is
different. Furthermore, the mechanism of pulmonary vascular
remodeling in PH-LHD requires further elucidation. In 2015, a study
by Li et al (10) reported on
the efficacy of the combined use of atorvastatin and sodium
ferulate in the treatment to PH-LHD based on routine treatment and
the safety was good, the PASP decreased and the Tei index (ratio of
isovolumic contraction time and isovolumic relaxation time to
ejection time.) of the right ventricle decreased (P<0.05). In
2013, Lian et al (11)
indicated that the LVEF was increased in patients with chronic
heart failure and PH treated with levosimendan combined with
sildenafil compared with that in the control group; the PAH
decreased and the 6-min walking distance improved.
Milrinone is an inhibitor of phosphodiesterase III
(PDE III). PDE III is distributed and dominant in pulmonary airway
smooth muscle, vascular smooth muscle and endothelial cells.
Milrinone is highly selective in inhibiting PDE III in myocardial
cells and vascular smooth muscle cells, reduces the degradation of
cAMP, increases the levels of cAMP in cardiac myocytes, acts on a
series of intracellular protein kinases, opens the calcium channel
on the sarcoplasmic reticulum causing large amounts of calcium ions
to enter the cytoplasm, and improves the contractility of
myocardium by stimulating contraction coupling mechanisms.
Milrinone increases the level of cGMP in vascular smooth muscle
cells, inhibits the phosphorylation of myosin light chain kinase
and calcium reabsorption in the sarcoplasmic reticulum, resulting
in a decrease in cytosolic calcium levels, while the contraction
and coupling process of smooth muscle is inhibited, finally leading
to arterial and venous dilatation (12). Therefore, milrinone increases
myocardial contractility and reduces the ventricular load. Various
experimental studies have indicated that milrinone reduces the
concentration of inflammatory factors, reduces the adhesion between
inflammatory cells and vascular endothelial cells, and also reduces
the damage caused by the inflammatory response to vascular
endothelium by increasing the intracellular concentration of cAMP
(13–17). Milrinone antagonizes intracellular
calcium overload and maintains tight junctions between endothelial
and stromal cells. Activation of cyclase and restrainment of
phosphodiesterase may reduce the gap formation between cells and
decrease vascular permeability (18). Milrinone has a short plasma
half-life, and 80% of the drug is excreted by the kidneys within 24
h. It has been indicated that following 2 h of milrinone
withdrawal, the hemodynamic indexes and cardiac function indexes
may be restored to the level prior to treatment, so the current
recommendation is administration for 24 h, which requires a
maintenance dose to maintain the effective concentration at the
loading dose after the vein, and the treatment efficacy is
positively correlated with the dosage (19). Milrinone is a commonly used drug for
the treatment of heart failure, and its effect on PH was also
reported (3–6). Various studies have also assessed the
inhalation of milrinone. In 2005, Lamarche et al (20) reported the effects of inhaled and
intravenous milrinone on the function of pulmonary vascular
endothelial cells in pigs following extracorporeal circulation. In
2012, Guo (3) reported that
inhalation of milrinone significantly reduces the PAH and PVR, and
increases the cardiac index in patients with severe left heart
valvular disease, while the patients' HR and systemic vascular
resistance were not significantly affected, which reflects good
selectivity for pulmonary vessels.
The results of the present study indicate that
conventional treatment improved the cardiac systolic function, but
the improvement was not obvious. Instructions for the
administration of milrinone currently only contain recommended
doses for heart failure and not for PH. The dose chosen in the
present study was in accordance with the dose reported for heart
failure in the drug instructions, which describes a loading dose of
25–75 µg/kg injected intravenously over 5–10 min and a maintenance
dose of 0.25-1 µg/kg/min. A small dose of milrinone (0.25
µg/kg/min) had no significant superiority compared with the
conventional treatment group in improving LV structure and LV
systolic function. Following doubling the dose of milrinone to 0.5
µg/kg/min, LV structure and function are obviously improved
compared with the conventional treatment group. The double dose of
milrinone improved the left heart ventricular systolic function and
structure compared with the small dose of milrinone, but the extent
of improvement was not significant. The small dose (0.25 µg/kg/min)
and the double dose (0.5 µg/kg/min) of milrinone significantly
improved the left heart structure and LV systolic function in
patients with mild and moderate PH-LHD. As there were only 2
patients with severe PH-LHD in group A and group B, the number of
samples was small and not suitable for comparison by statistical
methods. The mechanism by which milrinone reduces LAD and LVEDd is
as follows: Milrinone inhibits PDE III, increases cAMP in vascular
smooth muscle cells, reduces the intracellular calcium
concentration, inhibits excitatory contraction coupling, and
dilates arteries and veins, which reduces the front and back load
of the heart. The reduction in the volume of blood returning to the
heart reduces the pressure in the heart and the inner diameter of
the atrium and ventricle.
Right heart catheterization has been used to
evaluate and diagnose PH. However, the tests are invasive, costly
and use radioactivity, and it is therefore difficult to accept by
clinicians and patients. PASP may be estimated by tricuspid
regurgitation velocity and exhibits a good correlation with
pulmonary arterial pressure measured by right cardiac
catheterization (21,22). The present study demonstrates that
milrinone significantly improves the PASP in patients with PH-LHD,
while the improvement of the PASP was not obvious in the
conventional treatment group. Milrinone significantly improved the
PASP in patients with PH-LHD compared with that in the conventional
treatment group, and the double dose of milrinone caused the PASP
to further reduce. Milrinone significantly improved the PASP of
patients with mild and moderate PH-LHD. In future studies, a
statistical analysis should be performed by increasing the number
of samples with severe PH-LHD.
According to the Pearson correlation analysis, PASP
was strongly positively correlated with LAD, LVEDd, NT-proBNP and
hsCRP, and strongly negatively correlated with LVEF, TAPSE and
RVFAC. Therefore, the severity of PH in PH-LHD patients may be
estimated according to the above indexes.
The present study demonstrated that conventional
treatment does not significantly improve the right ventricular
function. Milrinone significantly improved the right heart function
of PH-LHD patients compared with the conventional treatment. The
small dose of milrinone (0.25 µg/kg/min) and the double dose of
milrinone (0.5 µg/kg/min) significantly improved the right heart
function. Milrinone significantly improved the right heart function
in in patients with mild and moderate HP-LHD. However, in the
routine treatment group, TAPSE was significantly improved but RVFAC
has not significantly changed following treatment in patients with
mild and moderate HP-LHD. Multiple measures, including
three-dimensional echocardiography and cardiac magnetic resonance,
will be used to assess whether the right ventricular function may
be significantly improved in future research for patients with
PH-LHD. Since there were only 2 patients with severe PH-LHD in
group A or group B, and 1 patient with severe PH-LHD in group C,
statistical analysis may be performed in future studies by
increasing the number of samples.
The latest guidelines for PH of The European Heart
Association from 2015 recommended BNP as the only biomarker for PAH
risk assessment (23). NT-proBNP has
a good prognostic value in pediatric and adult patients with PAH
(24). Andreassen et al
(25) confirmed that the elevated
levels of NT-proBNP in PAH patients are associated with
hemodynamics. Kolditz et al (26) suggested that different biomarkers
respond to different aspects of the pathogenesis of PH and
NT-proBNP was significantly correlated with hemodynamics. The
present study indicated that milrinone significantly reduces
NT-proBNP and hsCRP in patients with PH-LHD. In the routine
treatment group C, NT-proBNP was significantly decreased, while the
decrease of hsCRP was not significant. The small dose (0.25
µg/kg/min) and the double dose (0.5 µg/kg/min) of milrinone
significantly decreased NT-proBNP and hsCRP compared with those in
the conventional treatment group. However, by comparing the results
of group A and B following treatment, it was revealed that
following increasing the dose of milrinone, the decrease of
NT-proBNP and hsCRP was not significant. In future studies, the
dose of milrinone may be further increased to observe whether these
indexes may be further reduced. The present study indicated that
the small dose (0.25 µg/kg/min) and the double dose (0.5 µg/kg/min)
of milrinone significantly decrease NT-proBNP and hsCRP in patients
with mild and moderate PH-LHD. The present study suggested that
PASP was strongly positively correlated with NT-proBNP and hsCRP
(P<0.01). The degree of pulmonary artery pressure, and the
degree of improvement may be evaluated according to the NT-proBNP
and hsCRP. The following mechanism of NT-proBNP reduction following
the application of milrinone is suggested: i) Milrinone
significantly enhances cardiac contractility, increases the
ejection fraction, increases cardiac output per beat, and reduces
the volume load of the ventricle, thus reducing the secretion of
NT-proBNP. ii) Milrinone improves diastolic ventricular compliance
and ventricular diastolic function, so that the LV end-diastolic
filling pressure is reduced, thus reducing the secretion of
NT-proBNP.
In the present study, 4 cases of hypotension
occurred when patients were given an intravenous milrinone load
dose (BP <90/60 mmHg). Following intravenous infusion of
dopamine, the BP rose to >90/60 mmHg. The adverse effects of
fatigue and HR increase also occurred when the load dose was given,
but the symptoms disappeared following the maintenance dose was
given. No adverse effects of arrhythmia and thrombocytopenia were
encountered in the present study. Milrinone has been reported to
affect platelets in a dose-dependent manner (27), and Kikura et al (28) demonstrated that long-term oral
administration of amrinone caused thrombocytopenia; however, the
short-term use of milrinone had no significant effect on platelet
count and function.
The major causative factors of adverse reactions to
milrinone are as follows: i) Pharmacological action. Competitive
inhibition of PDE III by milrinone increases cGMP in vascular
smooth muscle cells and reduces the BP (12). ii) Pathological factors. Based on the
findings of the current study, milrinone opens the calcium channel
in the myocardial cell membrane during myocardial depolarization
and the influx of calcium ions increases the concentration of
calcium ions in the cells. The rate of depolarization of sinus node
pacemaker cells was accelerated during the diastolic phase. As a
result, the P-R interval is shortened and the atrioventricular node
conduction is accelerated. Milrinone increases the intracellular
calcium concentration by increasing the concentration of protein
kinase A (PKA) (12). PKA also
further activates the slow potassium channel and L-type calcium
channel in the heart, which in turn shortens the refractory period
of the atrium (12). The adverse
effects of milrinone on long-term use are arrhythmia, such as
atrial fibrillation and frequent ventricular premature beats, so it
should be used for a short time (19). iii) Drug concentration. Based on
current research, when a single dose is too large or the
intravenous drip is too fast, this may lead to high local
concentrations in the body in a short period of time, which may
cause adverse reactions. iv) Combination of milrinone with potent
diuretics. As heart failure is a complex clinical syndrome, it
frequently requires a combination of multiple drugs. In the present
study, 4 cases of hypotension occurred following the use of
milrinone on the basis of strong diuretics. It was suggested that
the vasodilator effect of milrinone was enhanced upon decreasing
the blood volume, resulting in a sharp decrease in BP.
In the present study, the maintenance dose of
milrinone did not cause any significant adverse reactions during
the course of the treatment. The results of Baruch et al
(29) demonstrated that if no load,
at 25–75 µg/kg intravenously over 5–10 min, was administered in
advance and milrinone was injected over 30 min at 0.5 µg/kg/min, a
hemodynamic effect is evident. The PCWP was similar to that of
application load following 2 h of continuous infusion and cardiac
index and plasma concentration of milrinone were similar following
3 h of continuous infusion (29).
However, 3 cases of hypotension and 2 cases of arrhythmia were
observed in the load dose group, which was associated to the short
injection time and fast injection speed (29). A previous study suggested that if
milrinone is not administered at a load dose, it may not affect
clinical outcomes and reduce adverse events (29). Through injection via a micropump, the
input speed of the drug may be accurately controlled, and at the
same time, the dose may be adjusted according to the hemodynamic
changes of the patients to avoid large increases in the local
concentration within a short period of time. Due to the short
plasma half-life of milrinone, 80% of the drug is excreted by the
kidneys following 24 h of treatment. It has been reported that
following milrinone withdrawal for 2 h, the hemodynamic and cardiac
function indices were restored to the level of that prior to
treatment; therefore, it is recommended that the drug be
administered over 24 h (30).
Following the loading dose, the maintenance dose must be
administered by infusion to maintain an effective plasma
concentration, and a positive correlation between the dosage and
efficacy has been reported (30).
Monitoring should be performed during the course of medication, and
the dynamic changes of BP, HR and other clinical symptoms must be
closely monitored; first aid should be provided immediately in case
of hypotension. If atrial flutter/atrial fibrillation occurs,
milrinone may in theory slightly increase atrioventricular node
conduction and the ventricular rate. Therefore, it is suggested
that digitalis preparation is used to control the ventricular rate
in advance.
Based on the present results, the following may be
concluded: i) Milrinone reduces PASP in patients with PH-LHD, and
improves the cardiac structure, cardiac function and biochemical
indexes; ii) a small dose of milrinone may significantly reduce
PASP in patients with mild and moderate PH-LHD, and significantly
improve the cardiac structure, cardiac function and biochemical
indexes; iii) increasing the dose of milrinone may further improve
PASP in patients with mild and moderate PH-LHD, but the cardiac
structure and cardiac function are not significantly improved in
comparison with low-dose milrinone; iv) PASP was positively
correlated with LAD, LVEDd, NT-proBNP and hsCRP, and negatively
correlated with LVEF, TAPSE and RVFAC; v) the maintenance dose of
milrinone did not cause any significant adverse reactions during
the course of the treatment. Therefore, it needs to be investigated
whether the use of milrinone with no load dose may reduce adverse
reactions without affecting its clinical efficacy.
In the present study, the number of patients with
severe PH-LHD was small, so that no statistical analysis could be
performed, and further studies are required to increase the number
of patients with severe PH-LHD to provide meaningful clinical
results. In the present study, only PASP was used to assess PAH. In
future studies, ultrasound and right heart catheterization may be
combined to evaluate PAH and increase the accuracy of its
determination. In future studies, the milrinone maintenance dose
may be increased within the specified dose range, to see if heart
function and structure, PASP and test indicators of patients with
PH-LHD may be improved, and whether adverse events increase with
higher doses.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BH contributed to the conception and design of the
study, the acquisition, analysis and interpretation of data and
drafting and revising of the manuscript. QW contributed to the
acquisition, analysis and interpretation of data. The final version
of the manuscript has been read and approved by all authors.
Ethical approval and consent to
participate
All of the participants of this study provided
written informed consent and volunteered to join the study. The
study was approved by the Ethics Committee of The Sixth People's
Hospital of Jinan (Jinan, China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bursi F, McNallan SM, Redfield MM, Nkomo
VT, Lam CS, Weston SA, Jiang R and Roger VL: Pulmonary pressures
and death in heart failure: A community study. J Am Coll Cardiol.
59:222–231. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Barst RJ, Ertel SI, Beghetti M and Ivy DD:
Pulmonary arterial hypertension: A comparison between children and
adults. Eur Respir J. 37:665–677. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Guo H: Applied research of specific
phosphodiesterase inhibitor during perioperative period of
rheumatic valvular disease combining with pulmonary hypertension
(unpublished PhD thesis). Southern Medical University. 2012.
|
|
4
|
Yu Y and Shi J: Effect of milrinone on
pulmonary function and dynamics of congenital heart disease with
pulmonary hypertension in patients with pulmonary oxygen. J
Practical Med. 28:469–470. 2012.
|
|
5
|
Xu D: Effect of milrinone on pulmonary
hypertension after cardiac surgery. Guide Chin Med. 11:200–202.
2013.(In Chinese).
|
|
6
|
Yao B, Da G, Li Y, Wu J, Li Z, Yang Y, Zhu
J, Wang W and Yang J: The protective effect of milrinone on heart
function in plateau region in children with congenital heart
disease and pulmonary hypertension after operation. Shandong Med J.
54:49–51. 2014.(In Chinese).
|
|
7
|
Galiè N, Hoeper MM, Humbert M, Torbicki A,
Vachiery JL, Barbera JA, Beghetti M, Corris P, Gaine S, Gibbs JS,
et al: Guidelines for the diagnosis and treatment of pulmonary
hypertension: The Task force for the diagnosis and treatment of
pulmonary hypertension of the European society of cardiology (ESC)
and the European Respiratory Society (ERS), endorsed by the
International society of heart and lung transplantation (ISHLT).
Eur Heart J. 30:2493–2537. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yock PG and Popp RL: Noninvasive
estimation of right ventricular systolic pressure by Doppler
ultrasound in patients with tricuspid regurgitation. Circulation.
70:657–662. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Trammell AW, Pugh ME, Newman JH, Hemnes AR
and Robbins IM: Use of pulmonary arterial hypertension-approved
therapy in the treatment of non-group 1 pulmonary hypertension at
US referral centers. Pulm Circ. 5:356–363. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li A, Xue C, Song M, MA S and Jia W: The
clinical efficacy and safety of oral administration of atorvastatin
in patients with pulmonary hypertension with left heart disease.
Ningxia Med J. 37:319–321. 2015.(In Chinese).
|
|
11
|
Lian X, Yang G and Wang E: Efficacy of
levosimendan combined with sildenafil in the treatment of chronic
heart failure with pulmonary hypertension. Practical J. 40:14–16.
2013.
|
|
12
|
Shipley JB, Tolman D, Hastillo A and Hess
ML: Milrilone: Basic and clinical pharmacology and acute and
chronic management. Am J Med Sci. 311:286–291. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schudt C, Winder S, Forderkunz S,
Hatzelmann A and Ullrich V: Influence of selective
phosphodiesterase inhibitors on human neutrophil functions and
levels of cAMP and Cai. Naunyn Schmiedebergs Arch Pharmacol.
344:682–690. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kume M, Banafsche R, Yamamoto Y, Yamaoka
Y, Nobiling R, Gebhard MM and Klar E: Dynamic changes of
post-ischemic hepatic microcirculation improved by a pre-treatment
of phosphodiesterase-3 inhibitor, milrinone. J Surg Res.
136:209–218. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Endres S, Sinba B and Fulle HJ: Amrinone
suppresses the synthesis of tumor necrosis factor-alpha in human
mononuclear cells. Shock. 1:377–380. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kawamura A, Yoshikawa T, Takahashi T,
Hayashi T, Takahashi E, Anzai T, Sato T and Ogawa S: Randomized
trial of phosphodiesterase inhibitors versus catecholamines in
patient with acutely decompensated heart failure. Jpn Circ J.
65:858–862. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lanfear DE, Hasan R, Gupta RC, Williams C,
Czerska B, Tita C, Bazari R and Sabbah HN: Short term effects of
milrinone on biomarkers of necrosis, apoptosis, and inflammation in
patients with severe heart failure. J Transl Med. 29:672009.
View Article : Google Scholar
|
|
18
|
Siflinger-Bimboim A, Bode DC and Malik AB:
Adenosine 3′,5′-cyclic monophosphate attenuates neutrophil-mediated
increase in endothelial permeability. Am J Physiol. 264:H370–H375.
1993.PubMed/NCBI
|
|
19
|
Fleming GA, Murray KT, Yu C, Byrne JG,
Greelish JP, Petracek MR, Hoff SJ, Ball SK, Brown NJ and Pretorius
M: Milrinone use is associated with post-operative atrial
fibrillation after cardiac surgery. Circulation. 118:1619–1625.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lamarche Y, Malo O, Thorin E, Denault A,
Carrier M, Roy J and Perrault LP: Inhaled but not intravenous
milrinone prevents pulmonary endothelial dysfunction after
cardiopumonary bypass. J Thorac Cardiovasc Surg. 130:83–92. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Burgess MI, Mogulkoc N, Bright-Thomas RJ,
Bishop P, Egan JJ and Ray SG: Comparison of echocardiographic
markers of right ventricular function in determining prognosis in
chronic pulmonary disease. J Am Soc Echocardiogr. 15:633–639. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li Y, Wang Y, Zhai Z, Guo X, Yang Y and Lu
X: Real-time three-dimensional echocardiography to assess right
ventricle function in patients with pulmonary hypertension. PLoS
One. 10:e01295572015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Galiè N, Humbert M, Vachiery JL, Gibbs S,
Lang I, Torbicki A, Simonneau G, Peacock A, Noordegraaf Vonk A,
Beghetti M, et al: 2015 ESC/ERS Guidelines for the diagnosis and
treatment of pulmonary hypertension: The joint task force for the
diagnosis and treatment of pulmonary hypertension of the European
Society of Cardiology (ESC) and the European Respiratory Society
(ERS): Endorsed by: Association for European Paediatric and
Congenital Cardiology (AEPC), International Society for Heart and
Lung Transplantation (ISHLT). Eur Heart J. 37:67–119. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Harbaum L, Hennigs JK, Baumann HJ,
Lüneburg N, Griesch E, Bokemeyer C, Grünig E and Klose H:
N-terminal pro-brain natriuretic peptide is a useful prognostic
marker in patients with pre-capillary pulmonary hypertension and
renal insufficiency. PLoS One. 9:e942632014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Andreassen AK, Wergeland R, Simonsen S,
Geiran O, Guevara C and Ueland T: N-terminal pro-B-type natriuretic
peptide as an indicator of disease severity in a heterogeneous
group of patients with chronic precapillary pulmonary hypertension.
Am J Cardiol. 98:525–529. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kolditz M, Seyfarth HJ, Wilkens H, Ewert
R, Bollmann T, Dinter C, Hertel S, Klose H, Opitz C, Grünig E, et
al: MR-proADM predicts exercise capacity and survival superior to
other biomarkers in PH. Lung. 193:901–910. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wesley MC, McGowan FX, Castro RA,
Dissanayake S, Zurakowski D and Dinardo JA: The effect of milrinone
on platelet activation as determined by TEG platelet mapping.
Anesth Analg. 108:1425–1429. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kikura M, Lee MK, Safon RA, Bailey JM and
Levy JH: The effects of milrinone on platelets in patients
undergoing cardiac surgery. Anesth Analg. 81:44–48. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Baruch L, Patacsil P, Hameed A, Pina I and
Loh E: Pharmacodynamic effects of milrinone with and without a
bolus loading infusion. Am Heart J. 141:266–273. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Huang LY and Yang Y: Clinical study of
milrinone in the treatment of neonatal persistent pulmonary
hypertension. Straits Sci. 8:111–113. 2012.(In Chinese).
|